Gyn- Intro & Menstrual Physiology
1/106
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
107 Terms
The study of women and diseases that affect them is known as _____
gynecology
The management of women during pregnancy, childbirth, and the puerperium is known as ______
obstetrics
What bones form the border of the true pelvis?
3 innominate bones of hip (ilium, ischium, pubis), sacrum, and coccyx
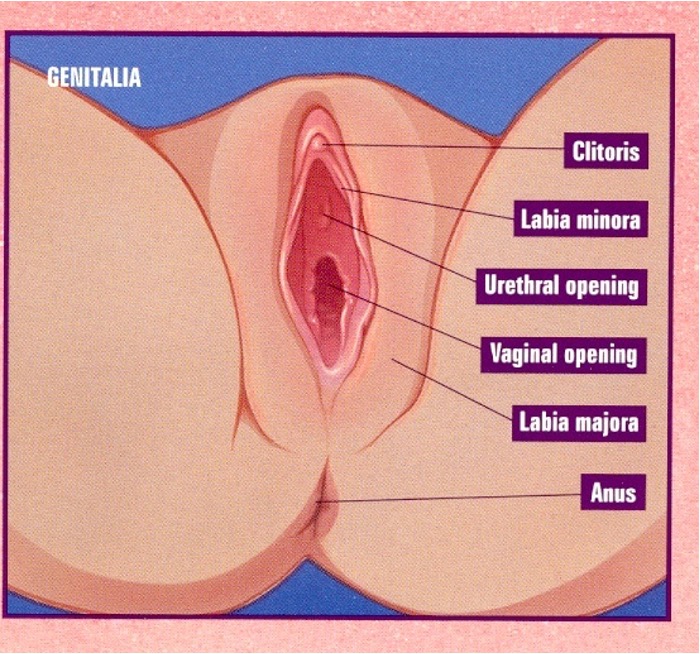
What is between the vestibule and the anus?
perineum
the muscular tube that is a potential space (not sitting open, collapsed) and extremely distensible is the _____
vagina
What regions is the area surrounding the uterine cervix divided into?
anterior fornix, posterior fornix, 2 lateral fornices
The area where fallopian tubes enter the uterus is known as the _____
cornu
The major divisions of the uterus, body and cervix, is separated by the ____
isthmus
How does the uterus normally appear?
pear shaped, thick walled, muscular organ
What are the layers of the uterine wall?
serial layer → outer
myometrium → firm, thick, intermediate coat of smooth muscle
endometrium → inner mucosal lining
The uterus is supported by ______
ligaments
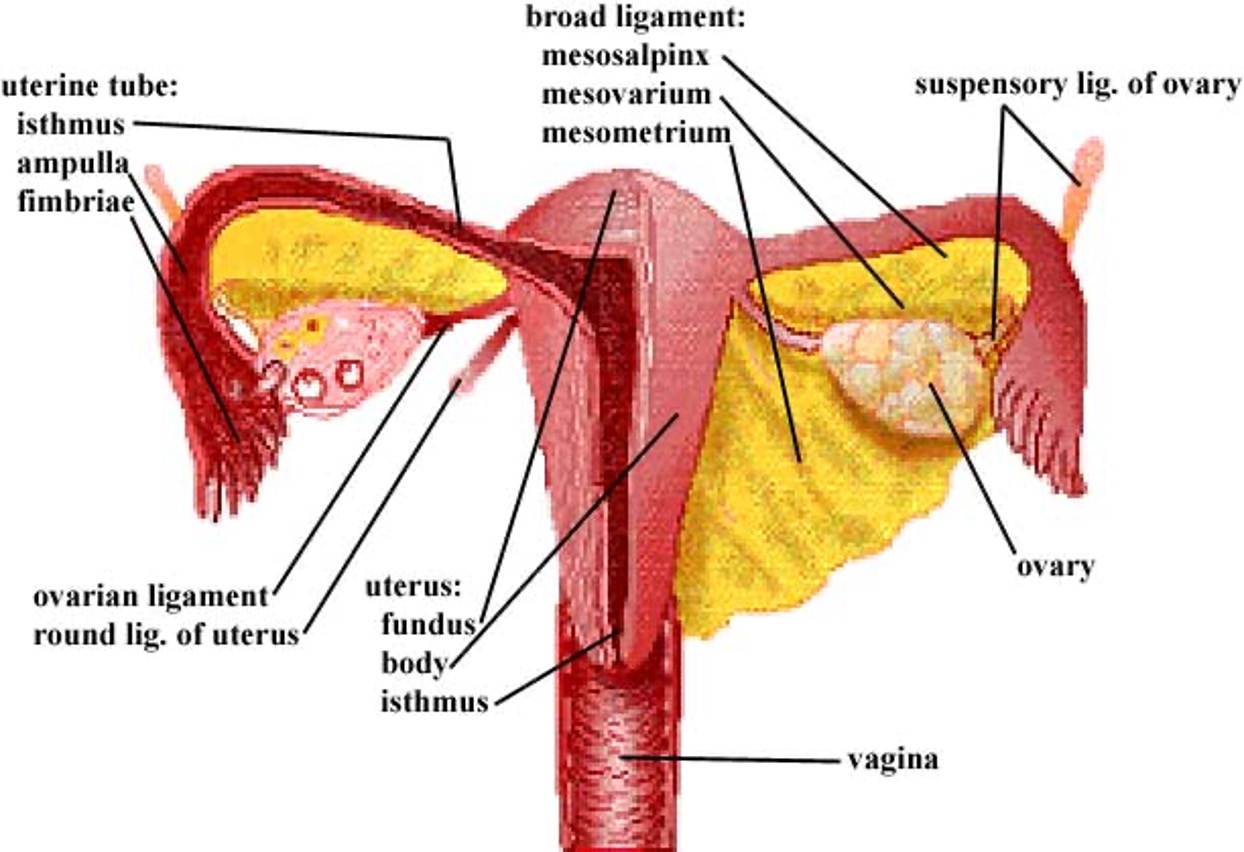
The neck of the uterus, aka the lower, narrow portion of the uterus where it joins w/ the top end of the vagina (fusion of mullerian ducts); and is cylindrical/conical in shape and protrudes through the upper anterior vaginal wall is known as the _____
cervix / cervix uteri
The purpose of which organ is egg transport and site of fertilization to form a zygote?
fallopian tubes
The purpose of which organ is gametogenesis- egg/ova/gamete production?
ovary

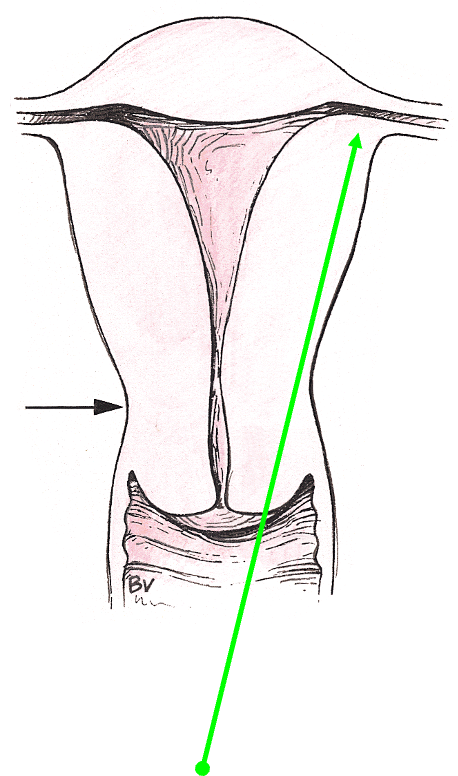
what type of cervical os?
nonparous / nulliparous

what kind of cervical os?
parous / multiparous or instrumentation
when would the ovaries be palpable?
reproductive years 50/50- based on timing in menstrual cycle (less often if on BCPS)
postmenopausal - variable; enlargement = alarm
The fallopian tubes, uterus, cervix, and upper 2/3s of the vagina develop from ______
2 paired mullerian ducts
What is derived from germ cells?
ovaries
What arises from the sinovaginal bulb?
lower vagina
Mullerian defects are often discovered due to _____
infertility
What kind of abnormalities commonly accompany Müllerian duct defects due to the close proximity of development?
renal
When one or both Müllerian ducts don’t develop fully, producing abnormalities such as uterine agenesis or hypoplasia (b/l) or unicornuate uterus (u/l), this is known as ______
organogenesis
The process during which the lower segments of paired Müllerian ducts fuse to form the uterus, cervix, and upper vagina, this is known as _____
lateral fusion
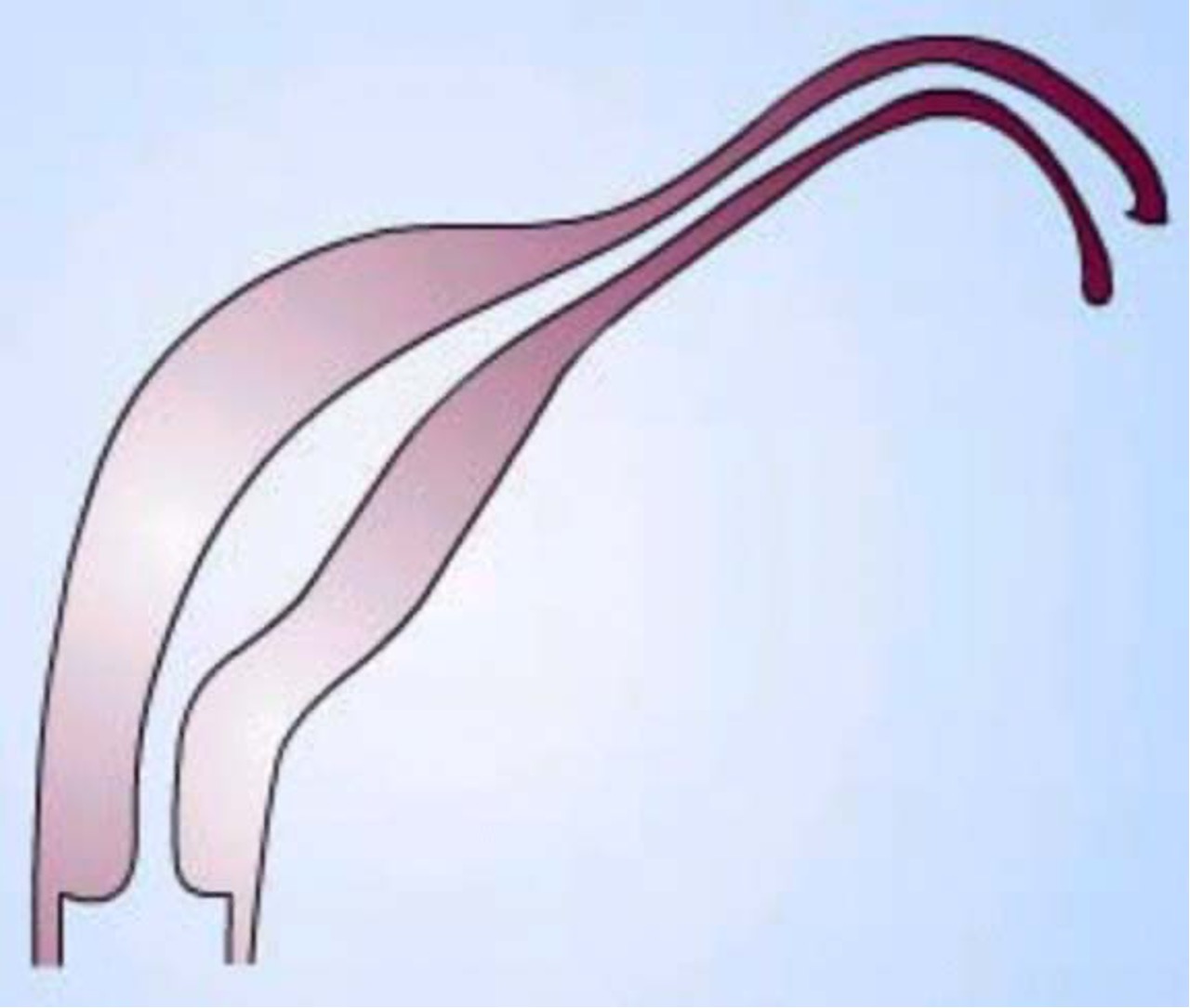
Fusion of the ascending sinovaginal bulb with the descending mullerian system, resulting in a patent vagina, is referred to as ____
vertical fusion
incomplete vertical fusion results in _____
imperforate hymen
failure of lateral fusion results in _____
bicornuate or didelphys uterus
After the lower Müllerian ducts fuse, a central septum is present, referred to as _____
septal reportion
failure of septal resorption results in ____
septate uterus
What are the 3 phases of development of complete formation and differentiation of the mullerian defects?
organogenesis, fusion, septal resorption
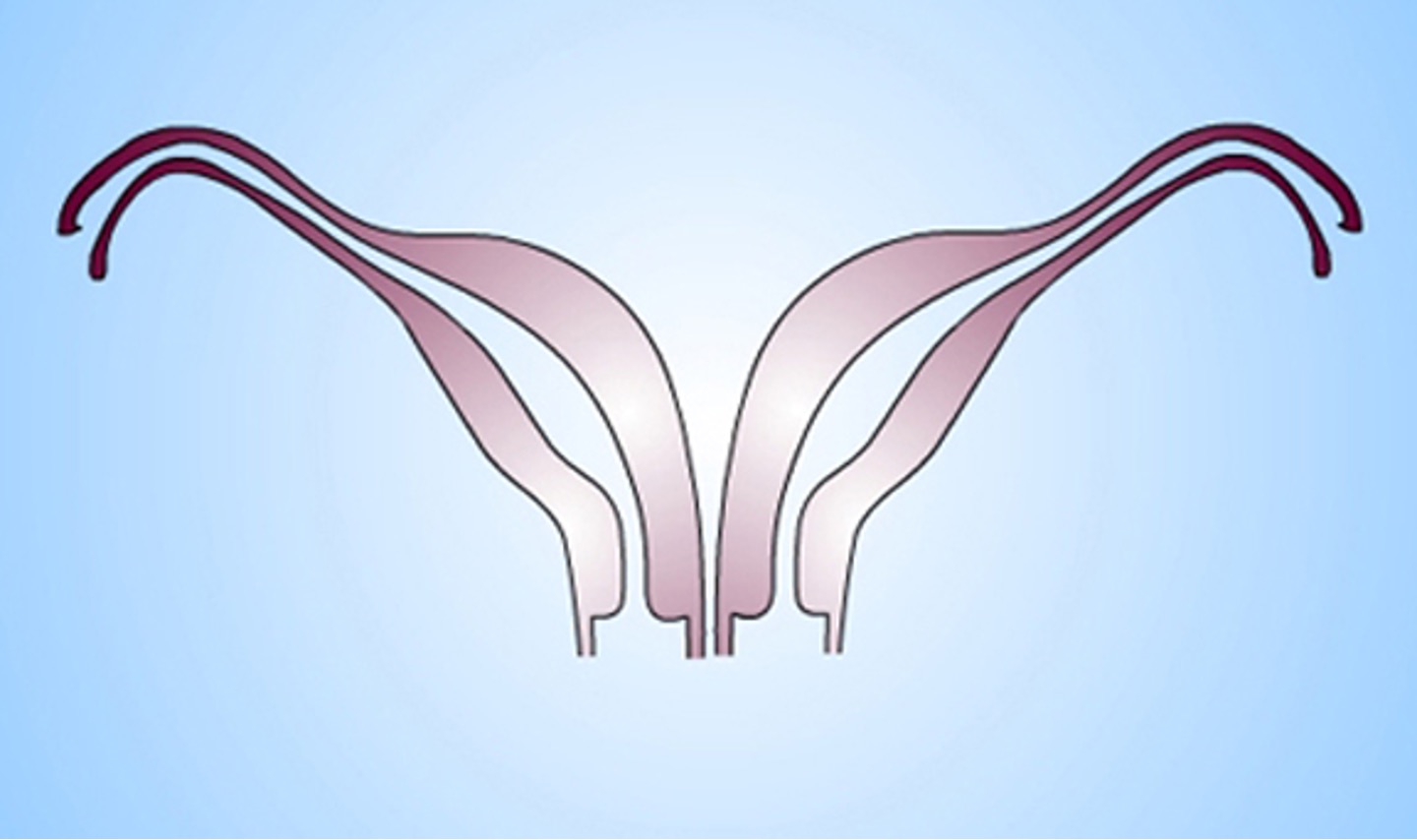
What class mullerian defect is this?
hypoplasia / agenesis → no reproductive potential aside from IVF of harvested ova and implantation in a host
class I
What class mullerian defect is this?
unicornuate uterus → result of complete/almost complete arrest of development of 1 Müllerian duct
incomplete arrest (MC) → rudimentary horn w/ or w/o functioning endometrium
if horn obstructed, may need surgery, enlarging pelvic mass
if contralateral healthy horn is almost fully developed, a full term pregnancy is believed to be possible
class II
What class mullerian defect is this?
didelphys uterus → results from complete confusion of both ducts
individual horns are fully developed and almost normal in size
2 cervices inevitably present
longitudinal or transverse vaginal septum possible
consider metroplasty (removing septum & fusing both)
can carry pregnancy to full term since each horn is almost a fully developed uterus
class III
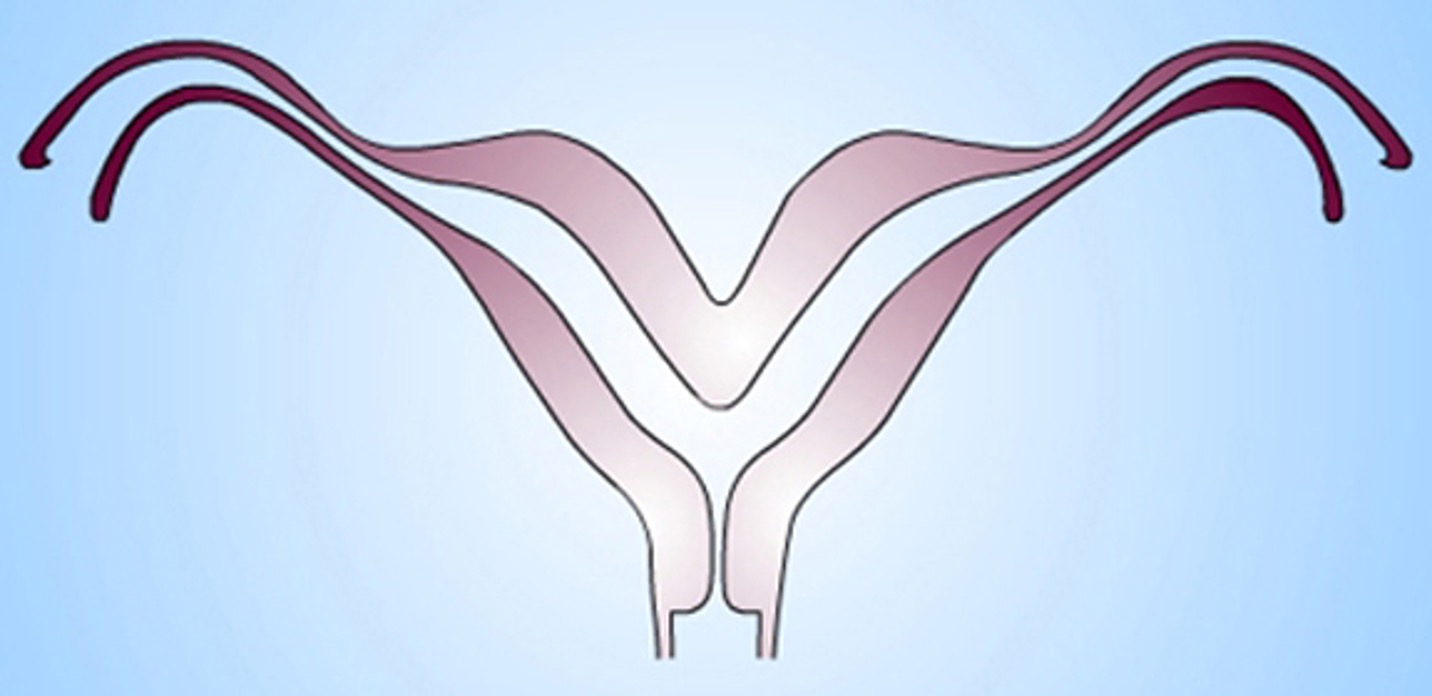
What class mullerian defect?
bicornuate uterus → results from partial confusion of ducts
demonstrates some degree of fusion b/t the 2 horns
horns not fully developed, typically smaller
some pts are candidates for metroplasty
class IV
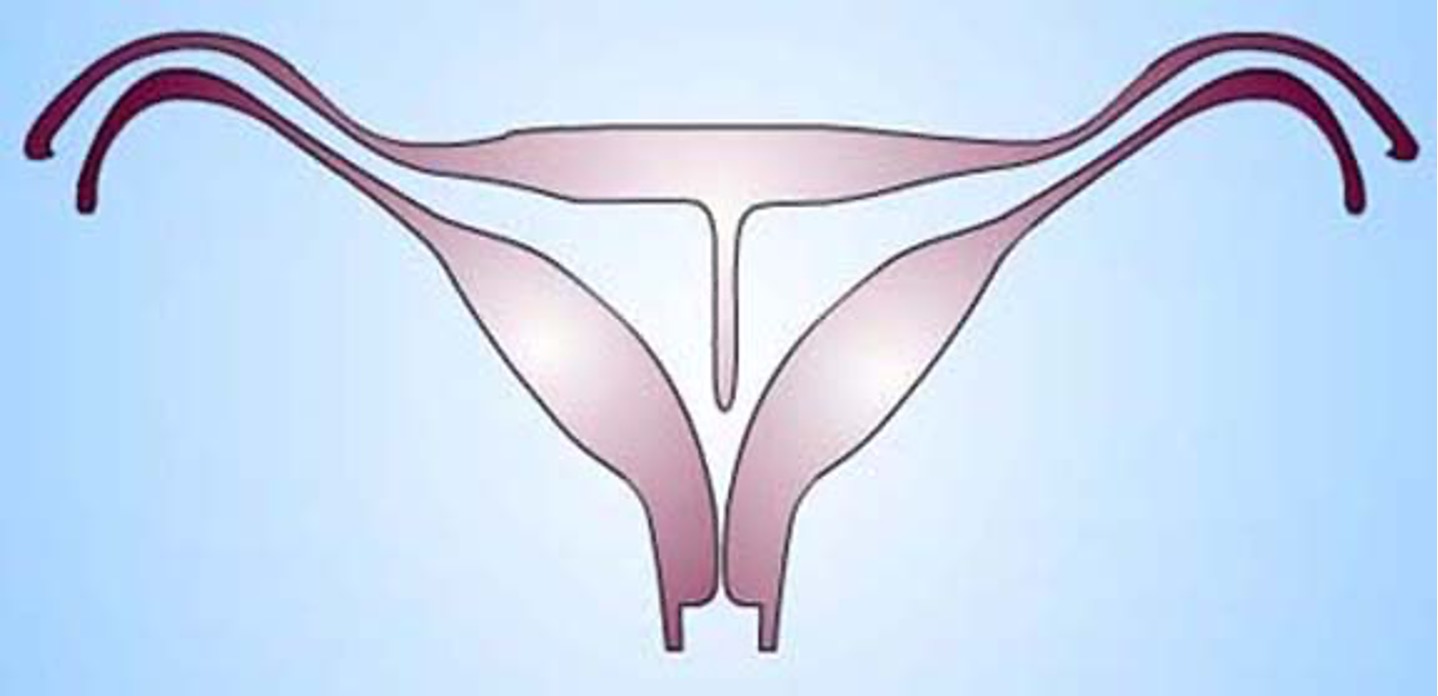
What class mullerian defect?
septate uterus → results from failure of resorption of septum b/t 2 uterine horns
septum can be partial or complete
uterine fundus is typically convex but may be flat or slightly concave
highest incidence of reproductive complications
treated by using transvaginal hysteroscopic resection of septum
class V
What class mullerian defect?
arcuate uterus → variant of normal, no adverse impact on fertility and pregnancy outcomes
has slight midline septum w/ minimal and often broad fundal cavity indentation
variously classified as septate, bicornuate, or normal variant
class VI
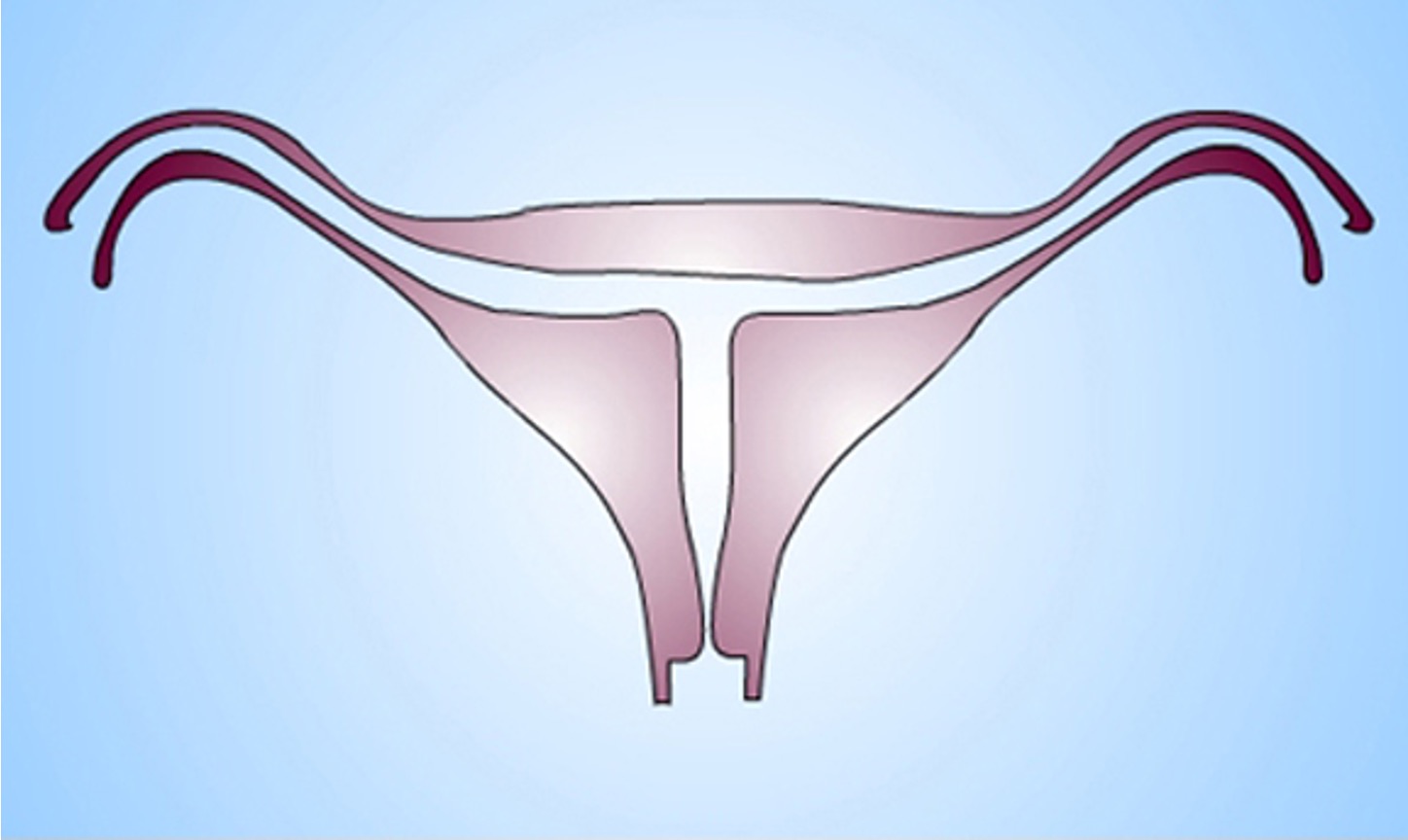
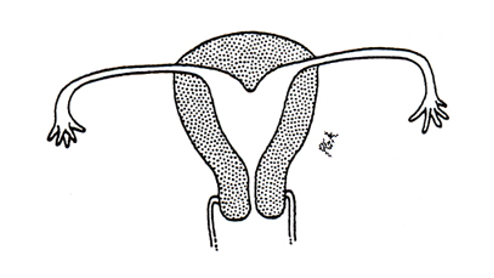
What class mullerian defect?
diethylstilbestrol (DES) related anomaly → synthetic form of estrogen prescribe to pregnant women to prevent pregnancy complications from 1945-1971
seen in female offspring in 15% women exposed to DES during pregnancy
variety of abnormal findings- uterine hypoplasia and t shaped uterine cavity; inc risk vaginal clear cell carcinoma
class VII
When an individual is physiologically capable of reproduction, this is known as _____
puberty
The development of breasts is _____
thelarche
The development of hair in the axilla and on the pubis is _____
pubarche
The first menstrual period is ______
menarche
An increase of adrenal androgens, early in sexual maturation and precursor to puberty, is ______
adrenarche
The stages of physical and sexual development in children, adolescents, and adults based on external primary and secondary sex characteristics is referred to as _____
sexual maturity rating (SMR) - tanner stages
Which Tanner Stage?
prepubertal
height inc at basal rate; 5-6 cm/yr
breast → papilla elevation only
pubic hair → villus hair only, no coarse pigmented hair
Tanner Stage 1
Which Tanner Stage?
height increases at accelerated rate: 7-8 cm/yr
breast → buds palpable and areolae enlarge; ~ age 10.9 (8.9-12.9)
pubic hair → minimal coarse pigmented hair mainly on labia; ~ age 11.2 (9-13.4)
modifications based on increasingly earlier puberty
white: may appear 1 year earlier
black: may appear 2 years earlier
Tanner Stage 2
Which Tanner Stage?
height increases at peak rate: 8cm/yr (age 12.5)
breast → elevation of contour, areolae enlarge; ~ age 11.9 (9.9-13.9)
pubic hair → dark, coarse, curly hair spreads over mons pubis; ~ age 11.9 (9.6-14.1)
axillary hair develops (13.1)
acne vulgaris develops (13.2)
Tanner Stage 3
Which Tanner Stage?
height increases 7 cm/yr
breast → areolae forms secondary mound on the breast; ~ age 12.9 (10.5-15.3)
pubic hair → hair of adult quality, no spread to junction of medial thigh w/ perineum; ~ age 12.6 (10.4-14.8)
Tanner Stage 4
Which Tanner Stage?
no further height increases after age 16
breast → adult contour, areola recesses to general contour of breast
pubic hair → adult distribution of hair, spreads to medial thigh, does not extend up linea alba
Tanner Stage 5
The onset of secondary sexual development before the age of 8 in girls and 9 in boys is referred to as _____
precocious puberty
What are the signs of precocious puberty in girls?
breast development and/or pubic hair→ white before age 7, black before age 6
menarche before age 10
**refer if 2 signs under 8 years old
What might suggest a pathological cause of precocious puberty?
premature puberty in very young children, contrasexual development, peripheral cause (asynchronous development), visual field deficit suggesting pituitary mass
What kind of precocious puberty?
caused by early maturation of hypothalamic pituitary-gonadal -axis
sequential maturation of breasts and pubic hair in girls, and testicular enlargement and pubic hair in boys
sex characteristics appropriate for gender (isosexual)
idiopathic in most cases
gonadotropin-dependent (GDPP) / central / true precocious puberty
What kind of precocious puberty?
caused by excess secretion of estrogens/androgens (derived from adrenal glands or gonads), exogenous sources of sex steroids, or ectopic production of gonadotropin from GCT
may be appropriate for child’s gender (isosexual) or inappropriate (contrasexual)
gonadotropin-independent (GIPP) precocious puberty / peripheral precocity / pseudo-precocious puberty
What kind of precocious puberty?
isolated breast development in girls (premature thelarche) or
isolated male hormone mediated sex characteristics in boys or girls that result from inc adrenal androgen production (premature adrenarche)
can be variant of normal puberty
should be monitored bc may progress to precocious puberty
tx: GnRH agonists
incomplete precocious puberty
Most cases of premature thelarche are ____
idiopathic and present around age 2 with serum estradiol in prepubertal range
What are the key features of premature thelarche?
isolated breast development; either u/l or b/l
absence of other secondary sex characteristics
normal linear growth & bone age
Premature thelarche occurs in what two peaks?
first 2 years of life & 6-8 years of age
When would a consultation with an endocrinologist be warrnet for premature thelarche?
progressive secondary sexual development, increasing growth velocity, or accelerated bone maturation present
What population is premature adrenarche most common in?
girls (black > white) & individuals w/ obesity and insulin resistance
Premature adrenarche is a risk factor for ______
PCOS
What is the diagnosis of premature adrenarche best supported by?
elevated DHEA-sulfate concentration in pubic hair stage
17-hydroxyprogesterone and testosterone levels in age appropriate normal ranges
Initial periods are usually ______
anovulatory (regular ovulation begins ab 1 yr later
The USA average age of menarche (12.5) has _____
decreased
What is the normal length of a menstrual cycle?
28 days +/- 7
What is the normal duration of menses?
5 days +/- 2
What Is the average blood loss per day in normal menses?
8 or fewer soaked pads / 35-150 ml (usually no more than 2 heavy days)
What is the average loss of iron in normal menses?
13 mg
What are the 3 primary components of the menstrual cycle?
HPA axis (hypothalamus, pituitary gland, & anterior pituitary )
______ secretes LH and FSH to stimulate ovarian function.
anterior pituitary
Which cycle?
follicular phase
ovulation
luteal phase; pregnancy
ovarian
Which cycle?
proliferative phase
secretory phse
menses
uterine
What is the control center that responds to hormones and neurotransmitters and secretes GnRH every 90 minutes, pulsatile to the anterior pituitary via portal circulation?
hypothalamus
What hormones does the anterior pituitary produce?
FSH & LH → ovary
prolactin → breast
What hormone?
produced in gonads, pituitary gland, placenta, etc
increases FSH binding and FSH induced aromatization in the ovarian follicle
participates in androgen synthesis enhancing LH action in the ovary
activin
Which hormone?
inhibits FSH production
produced in gonads, pituitary gland, placenta, corpus luteum, etc
secretion from the granulose cells of ovarian follicles is stimulated by FSH
secretion is diminished by GnRH and enhanced by IGF-1
inhibin
What phase of the ovarian cycle?
initiated by lack of estrogen at end of menses
FSH from ant pit stimulates follicle to grow & produce estrogen
Graafian follicle chosen by day 7
as estrogen inc, it inhibits release of FSH
LH from ant pit in small amounts prior to ovulation, surges mid cycle in response to peak amounts of estrogen from mature follicle, stimulates ovary to produce progesterone after ovulation
10-14 days
follicular / phase I
Which phase of the ovarian cycle?
estrogen peaks at 200-300 pg/ml
GnRH inhibited by high estrogen & amt of FSH being secreted drops off
ant pit releases LH surge ahead of ovulation
one egg released 36-42 hours from onset of surge
corpus luteum formed at site of follicle that hs matured and released ovum
secretes progesterone to ready uterus for pregnancy
if not fertilized, becomes inactive after 10-14 days, involutes and becomes corpus albicans (fibrous scar tissue) and menstruation occurs
ovulatory / phase II
what phase of the ovarian cycle?
progesterone dominant (secreted by corpus luteum)
relatively constant in length (12-14 days)
progesterone increases and peaks (day 20 of the cycle - 6 days post ovulation)
estrogen levels off
corpus luteum involutes after 14 days, resulting in drop of progesterone levels
if implantation, progesterone levels stay up due to production of hCG, progesterone would then further inhibit FSH and new follicular recruitment
luteal / phase III
What phase of the uterine cycle?
roughly corresponds with follicular phase of ovarian cycle
influenced by estrogen
thickness of endometrium rapidly increases by the drawing out of the uterine glands
dont consulte or secrete in this phase
proliferative phase
What phase of the uterine cycle?
roughly corresponds with luteal phase of ovarian cycle
progesterone influence from corpus luteum
lining becomes highly vascularized, slightly edematous, glands become coiled and tortuous and begin to secrete clear fluid
secretory phase
What process occurs when the corpus luteum involutes, progesterone & estrogen dec,, PG inc & smooth muscle contraction, & endometrium loses its blood supply and sloughs its functional layer?
menstruation
The stage of a woman’s reproductive life that begins up to 10 years before menopause (~40s) when the ovaries gradually begin to produce less estrogen in known as _____
perimenopause
What is the average length of perimenopause?
4 years; ends after 12 consecutive months w/p a menstrual cycle (menopause)
The following symptoms are associated with what condition?
change in periods - shorter or longer, lighter or heavier, more/less time in between
hot flashes, night sweats, trouble sleeping
vaginal dryness
mood swings, trouble focusing
less hair on head, more on face and breasts
Perimenopause
What marks the permanent end of fertility with reduced functionaling of the ovaries, confirmed with the absence of menses for 12 consecutive months?
menopause
what is the average age of menopause in the US?
52
T/F: ovulation can still sporadically occur during menopause.
true
What condition might happen during menopause due to the increased loss of estrogen?
osteoporosis
what is the most common cause of secondary amenorrhea?
pregnancy
what type of amenorrhea?
never menstruated
eti: gonadal failure, congenital absence of vagina, constitutional delay
primary
What kind of amenorrhea?
menstruated but failed to menstruate again for more than 3 cycles or w/in 6 mos
eti: chronic anovulation, hypothyroidism/hyperprolactinemia, wt loss/anorexia
secondary
when should a work up be initiated for amenorrhea?
no period by age 14 w/ absent secondary sex characteristics
no period by a ge 16 regardless of secondary sex characteristics
in menstruating women w/o menses for 6 mos
obvious cases- turners appearance, genital anomalies, etc
What is the treatment for amenorrhea?
must treat to avoid prolonged uterine exposure to unopposed estrogen or anovulation if fertility desired
OC’s are good for younger pts; otherwise regular progesterone withdrawal
ovulation induction for desired conception
HRT or OC’s if perimenopausal
What is the most common Ullrich turner syndrome?
chromosomal monosomy X (45XO)
The following symptoms are associated with what condition?
characteristic physical abnormalities → short stature, lymphedema, broad chest, low hairline, low set ears, webbed neck
gonadal dysfunction (amenorrhea & infertility)
CHD, hypothyroidism, ophthalmologic problems, etc
Ullrich turner syndrome
Severe uterine pain/cramps during menstruation that are severe enough to limit normal activities or require medication is known as _____
dysmenorrhea
Excessively heavy blood loss is known as ____
menorrhagia
what is the treatment for primary dysmenorrhea?
OCPs- suppress ovulation, lighter/regular flow
NSAIDS- ibuprofen, mefenamic acid, naproxen sodium
low level topical heat
When ectopic tissue similar to the lining of the uterus is found elsewhere in the body, this is _____
endometriosis
What is the most common symptom of endometriosis?
pelvic pain