Acid-Base Fluid & General Fluid | Chapter 25 | BIOL117
1/131
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
132 Terms
rank the liquid requirement of these group from highest to lowest: children, young & middle-aged adult, elderly, infant
infant
children, young anf middle aged adult
elderly
true or false body fluid increases with age
false: body fluid decreases with age
where is most of the body water stored?
75% of skeletal is water
20% of adipose tissue is water
5% at other places around the body
true or false: males have more skeletal muscles so slightly higher percentage of body fluid
true
the percentage of body fluid decreases as body fat __________
increases
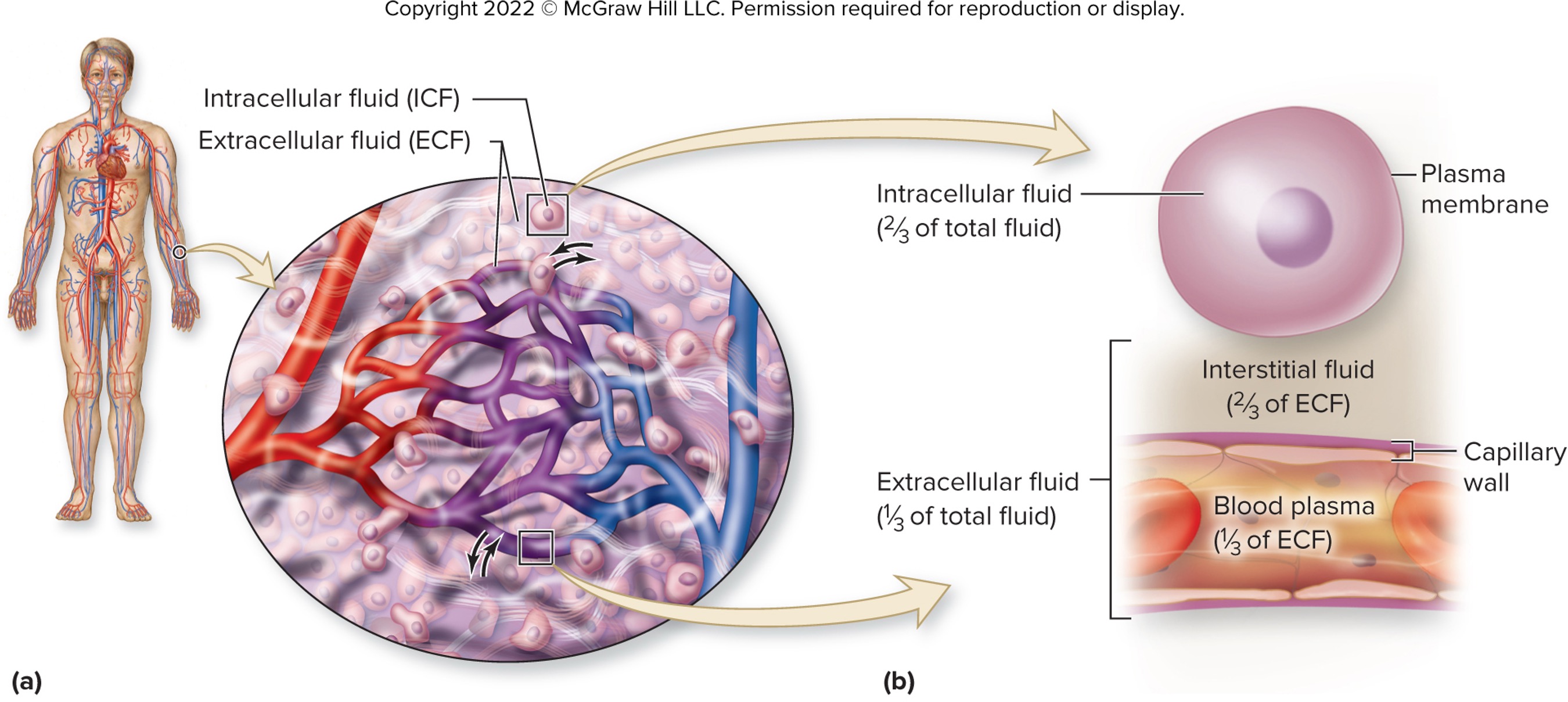
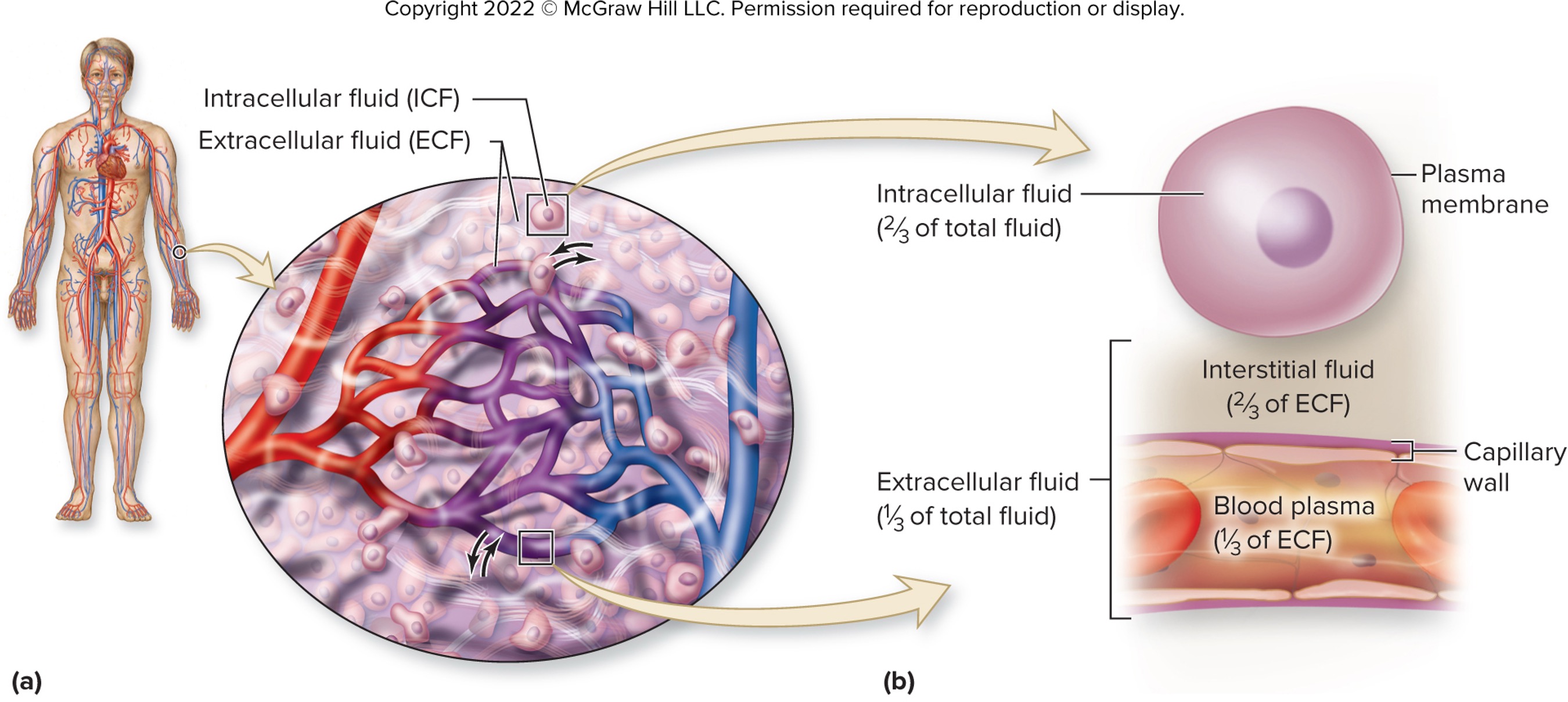
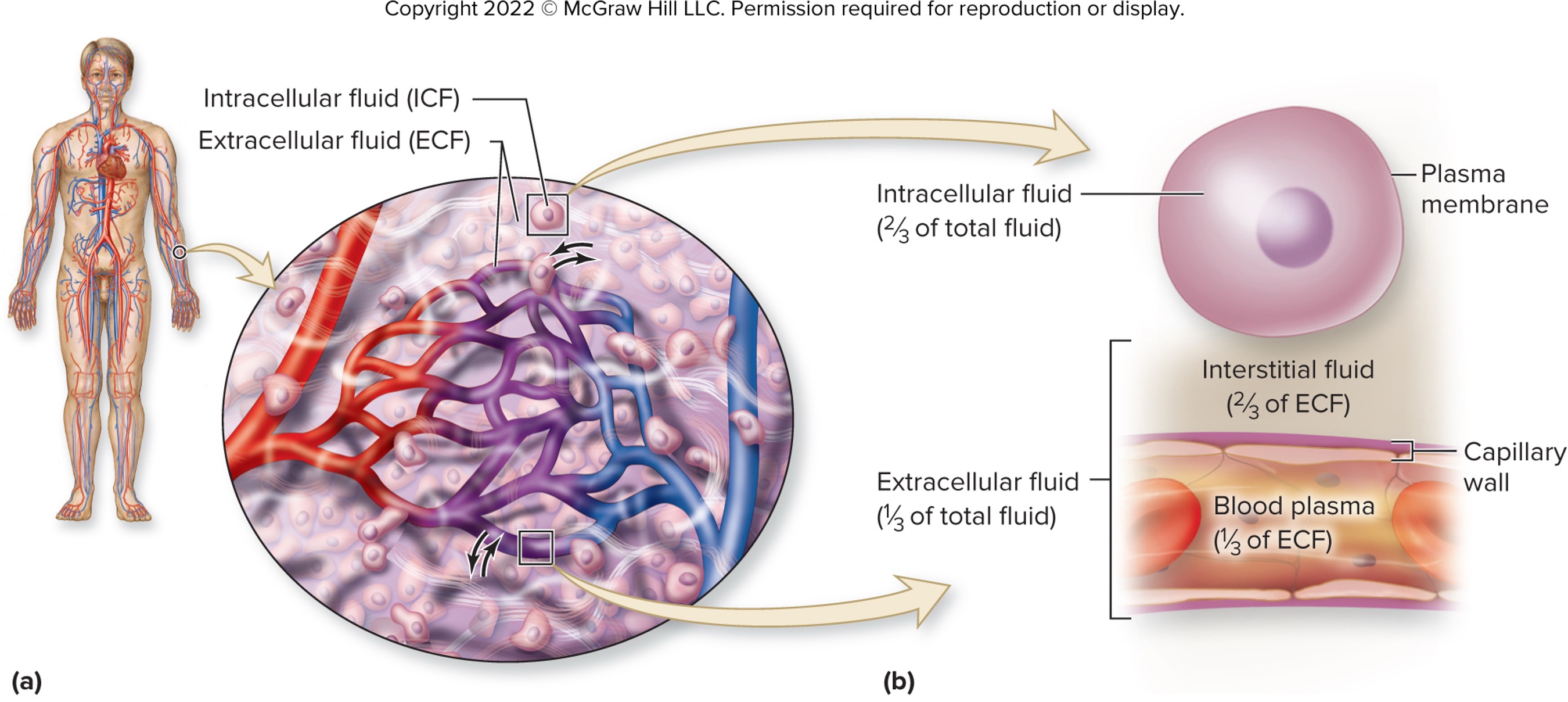
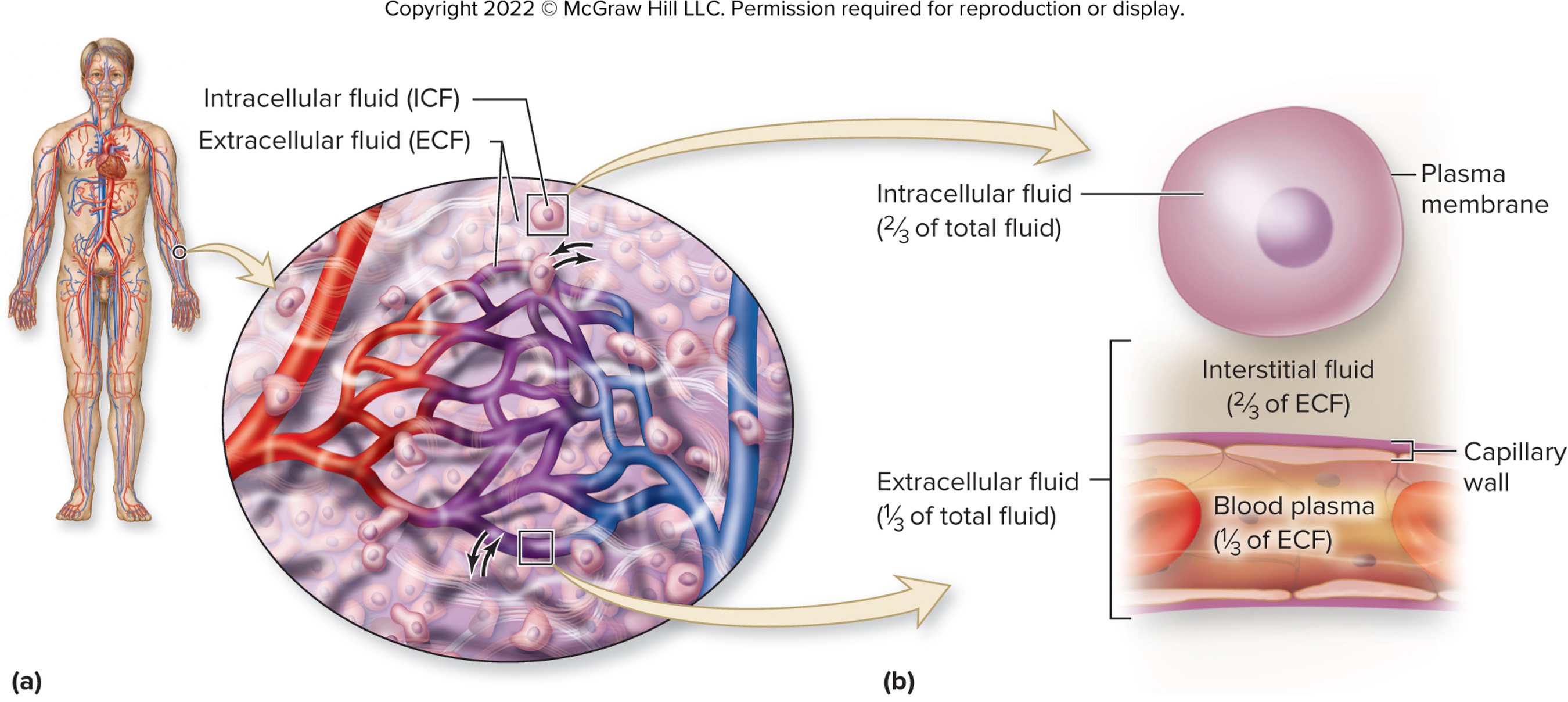
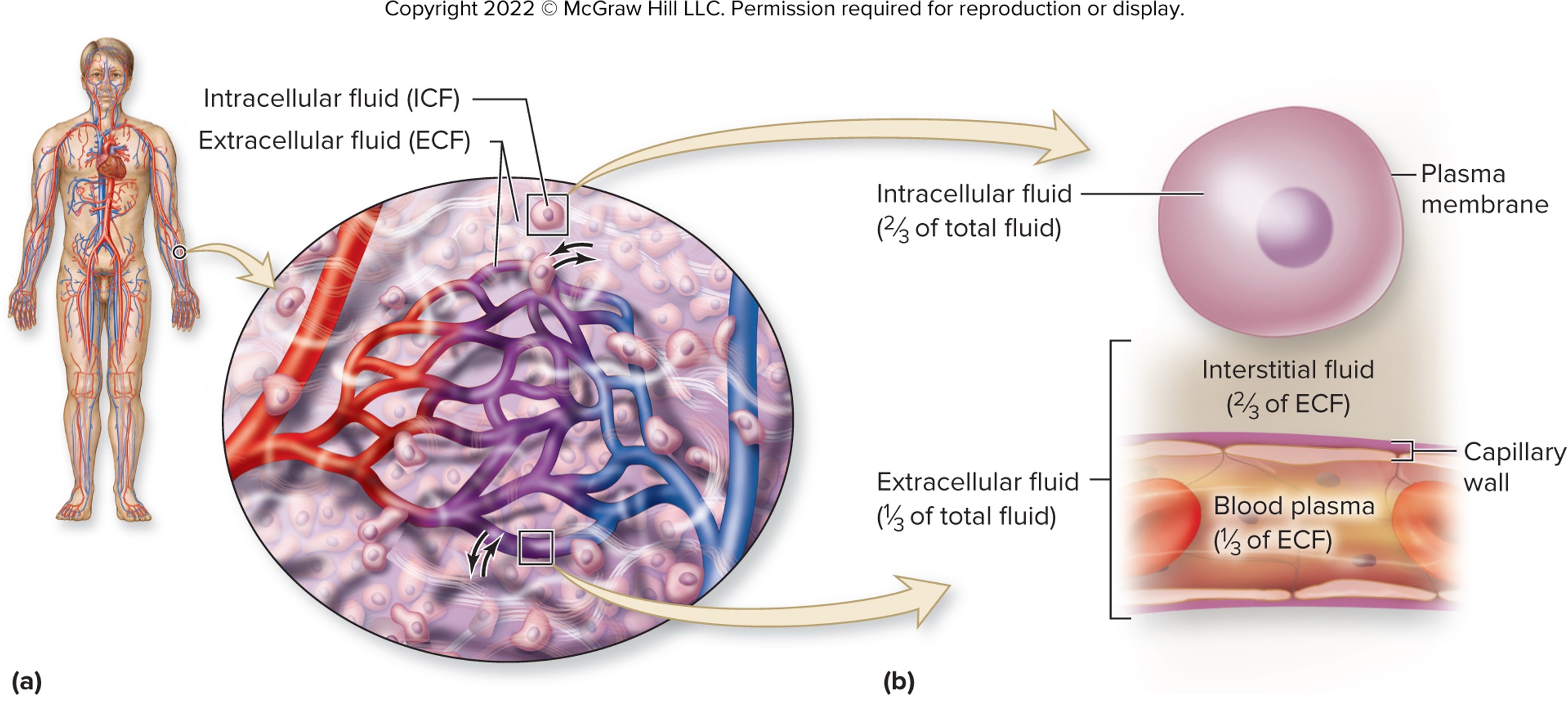
intracellular fluid (ICF)
fluid within our cells
comprised of 2/3 of total body fluid
enclosed by plasma membrane
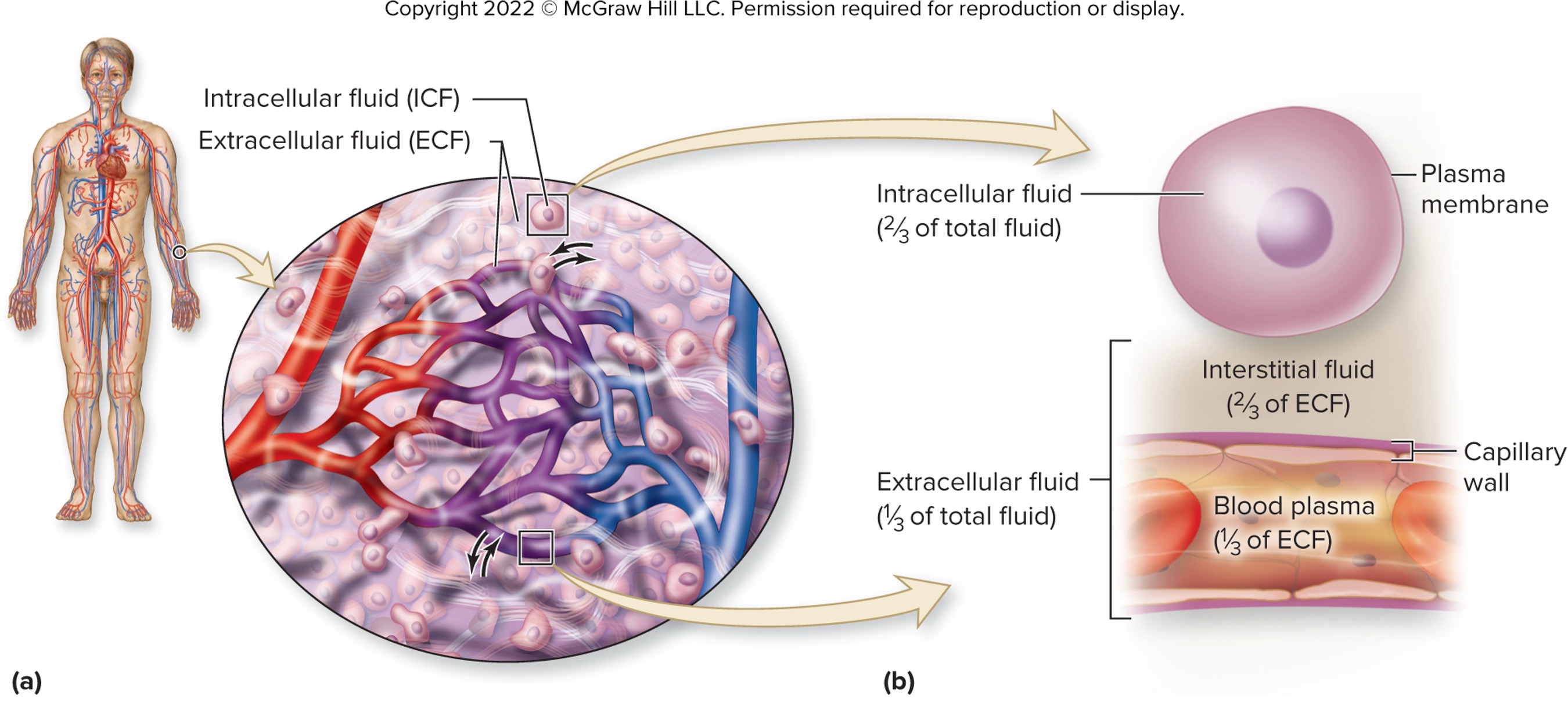
extracellular fluid (ECF)
fluid outside our cells
comprised of two types: interstitial and blood plasma
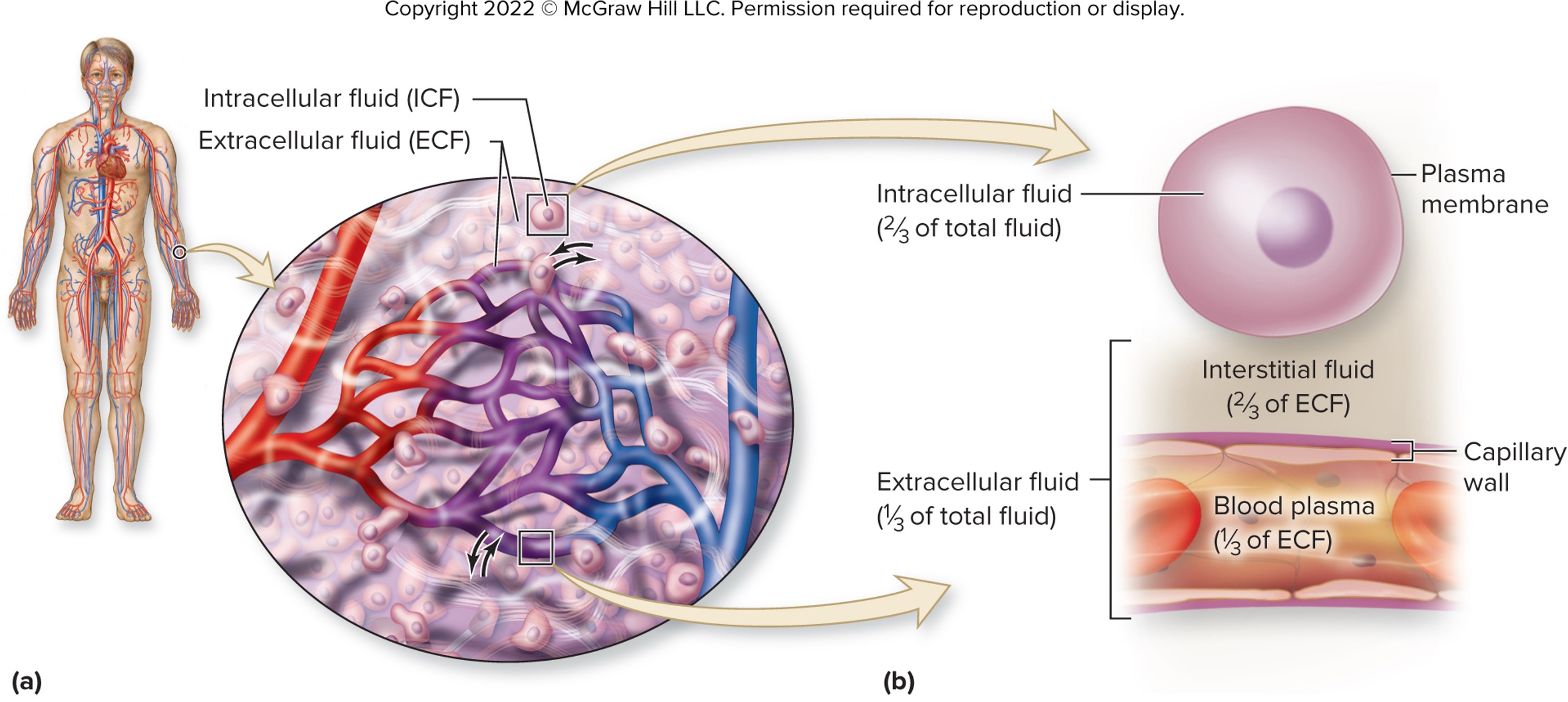
interstitial fluid
extracellular fluid surrounding the cells (like right outside of the cell)
composes 2/3 of extracellular fluid
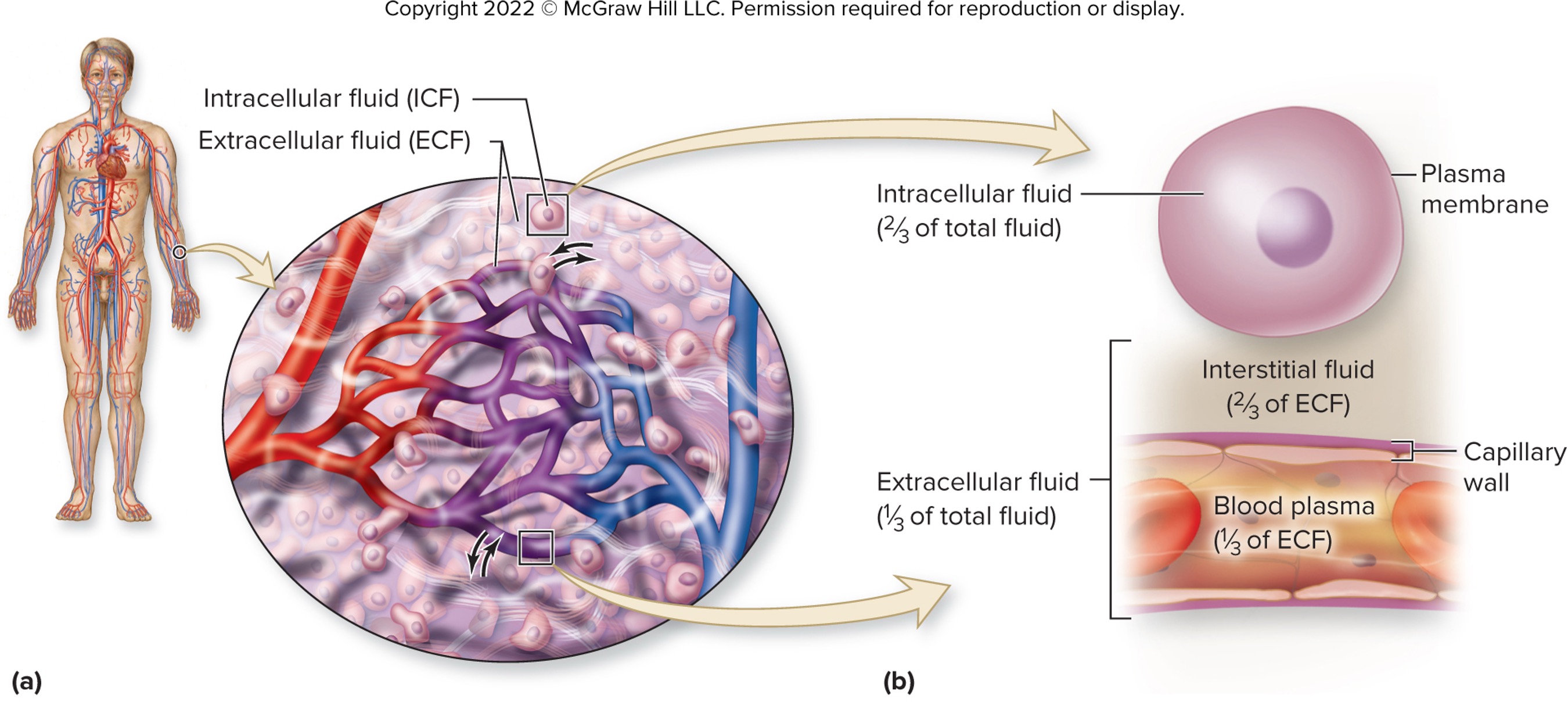
blood plasma
extracellular fluid within the blood vessels
seperated from interstitial fluid by capillary vessel wall (more permeable than plasma membrane)
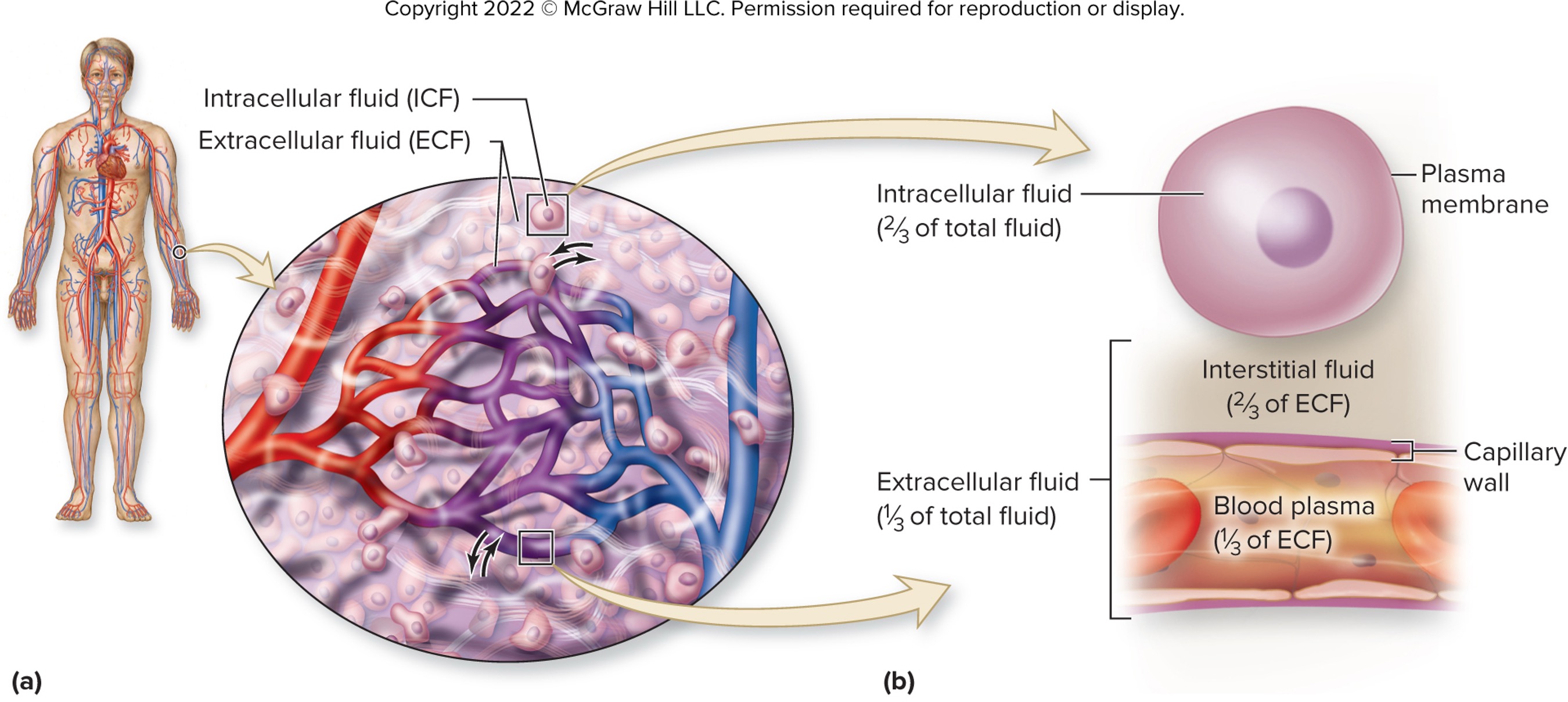
true or false: the capillary vessels are more permeable than plasma membrane
true
interstitial fluid and blood plasma membrane are _______ in composition
similar
review the different type of extracellular fluid existing in the body….
cerebrospinal fluid
synovial joint fluid
aqueous and vitreous humor of the eye
fluids of the inner ear
serous fluids within body cavity
____________ fluid has more K+, Mg2+, PO43- and negatively charged proteins
intracellular
____________ fluid has more Na+, Ca2+, Cl-, HCO3-
extracellular
what is the main difference between interstitial fluid and blood plasma?
proteins is present in blood plasma but very little in interstitial fluid
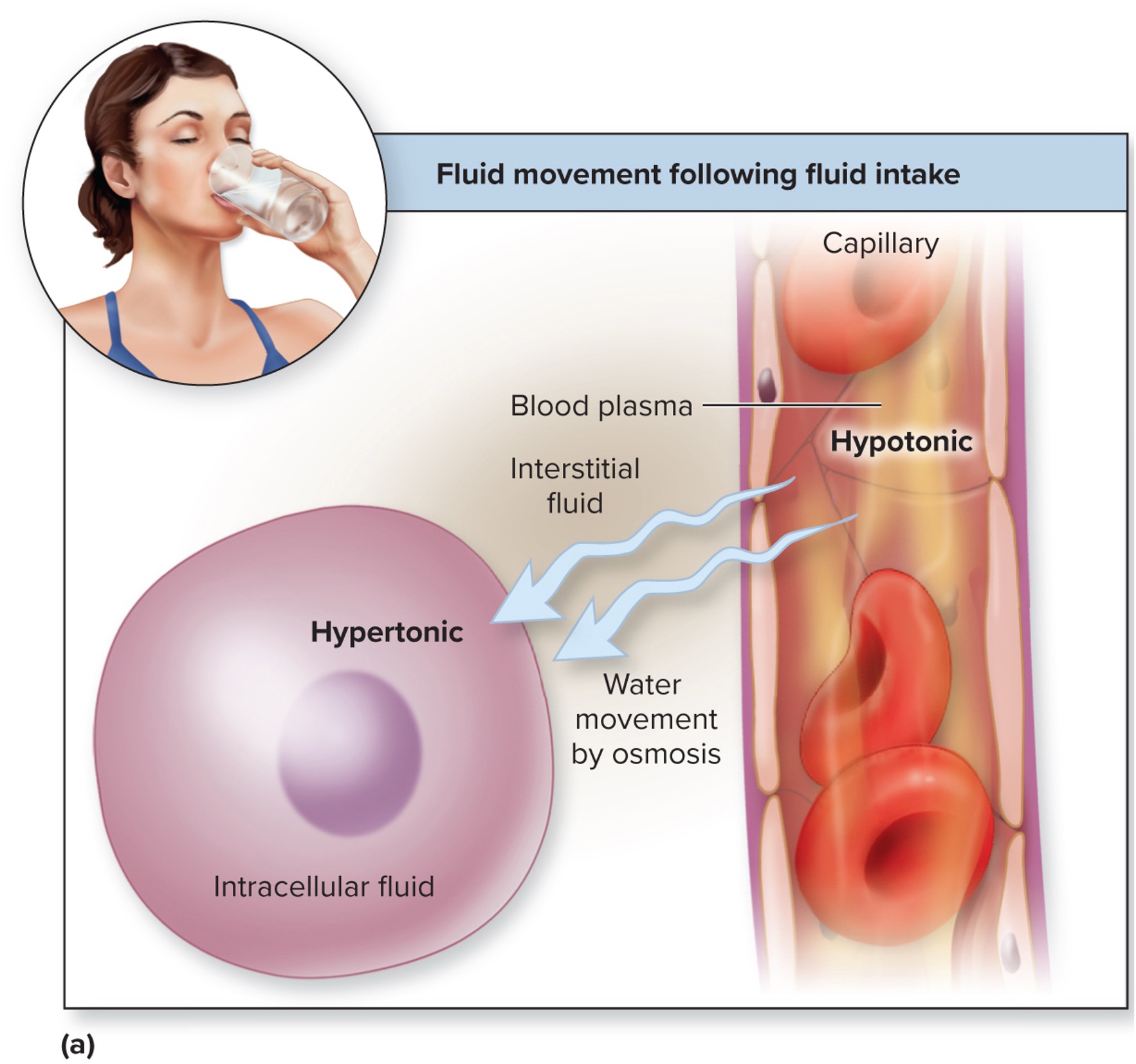
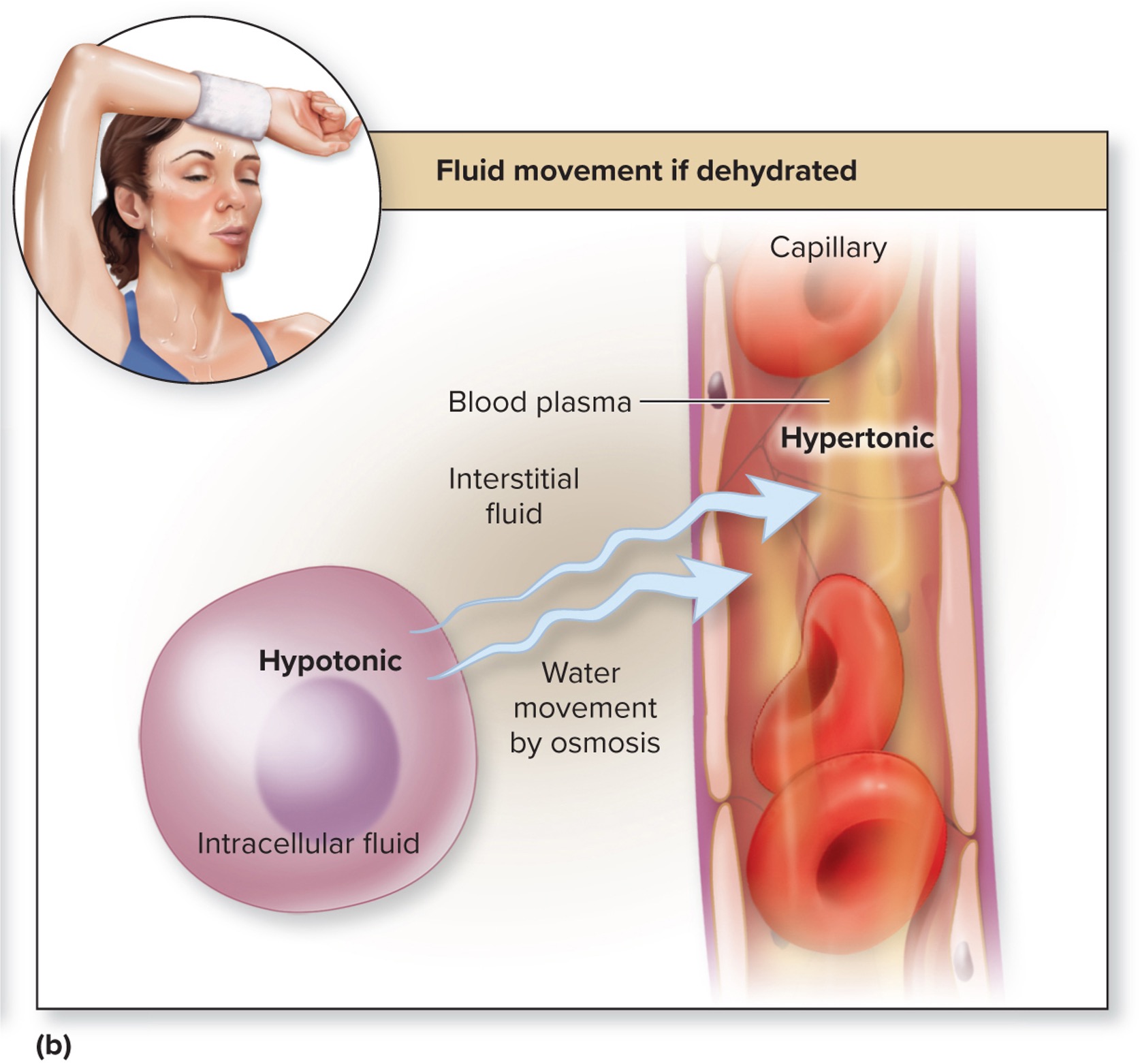
there is a ____________ movement of fluid between compartment (extra - intra) in response to changes in osmolarity (concentration of solutes)
continuous
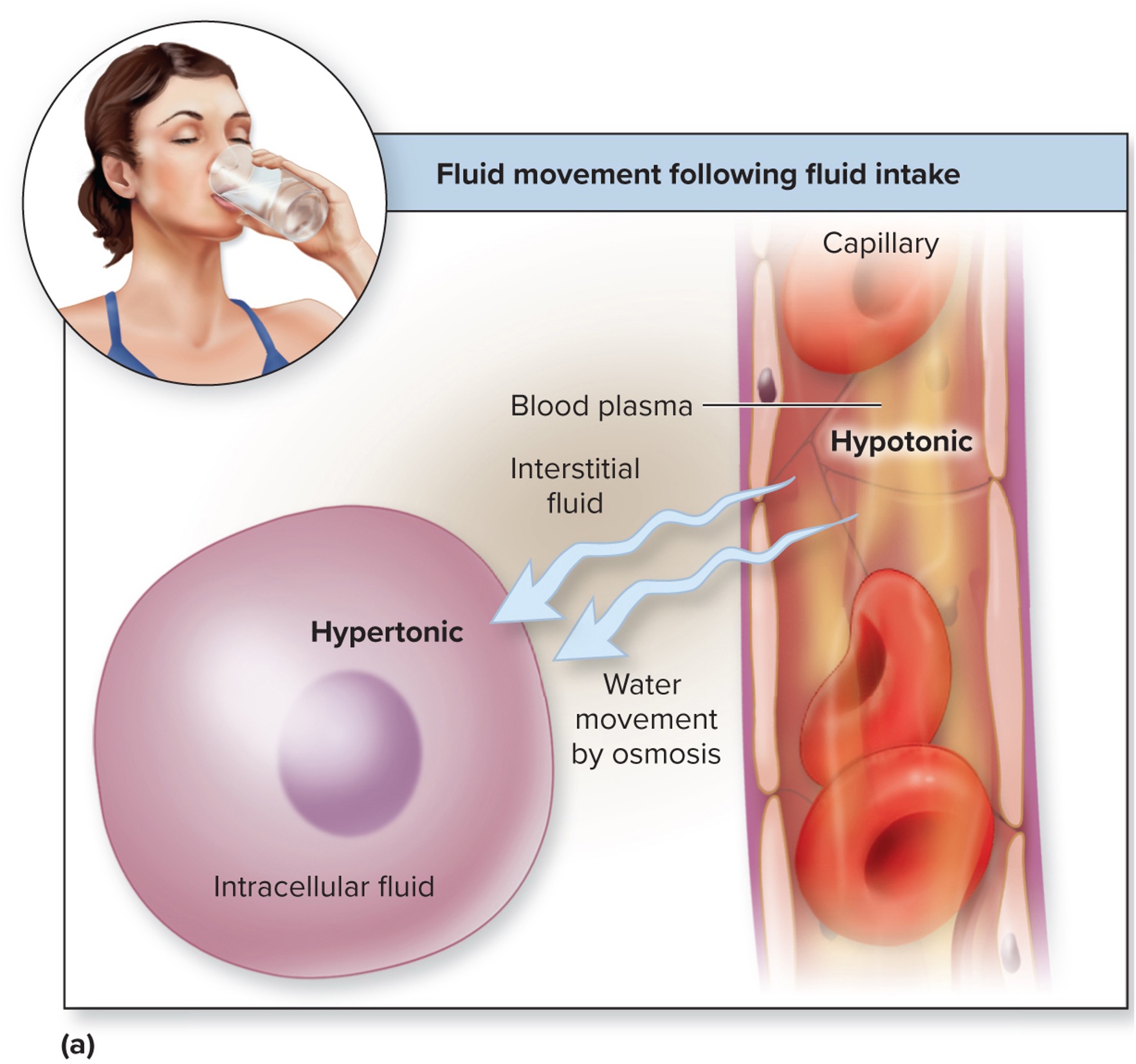
water moves by osmosis from __________ solution to ____________ solution
hypotonic; hypertonic
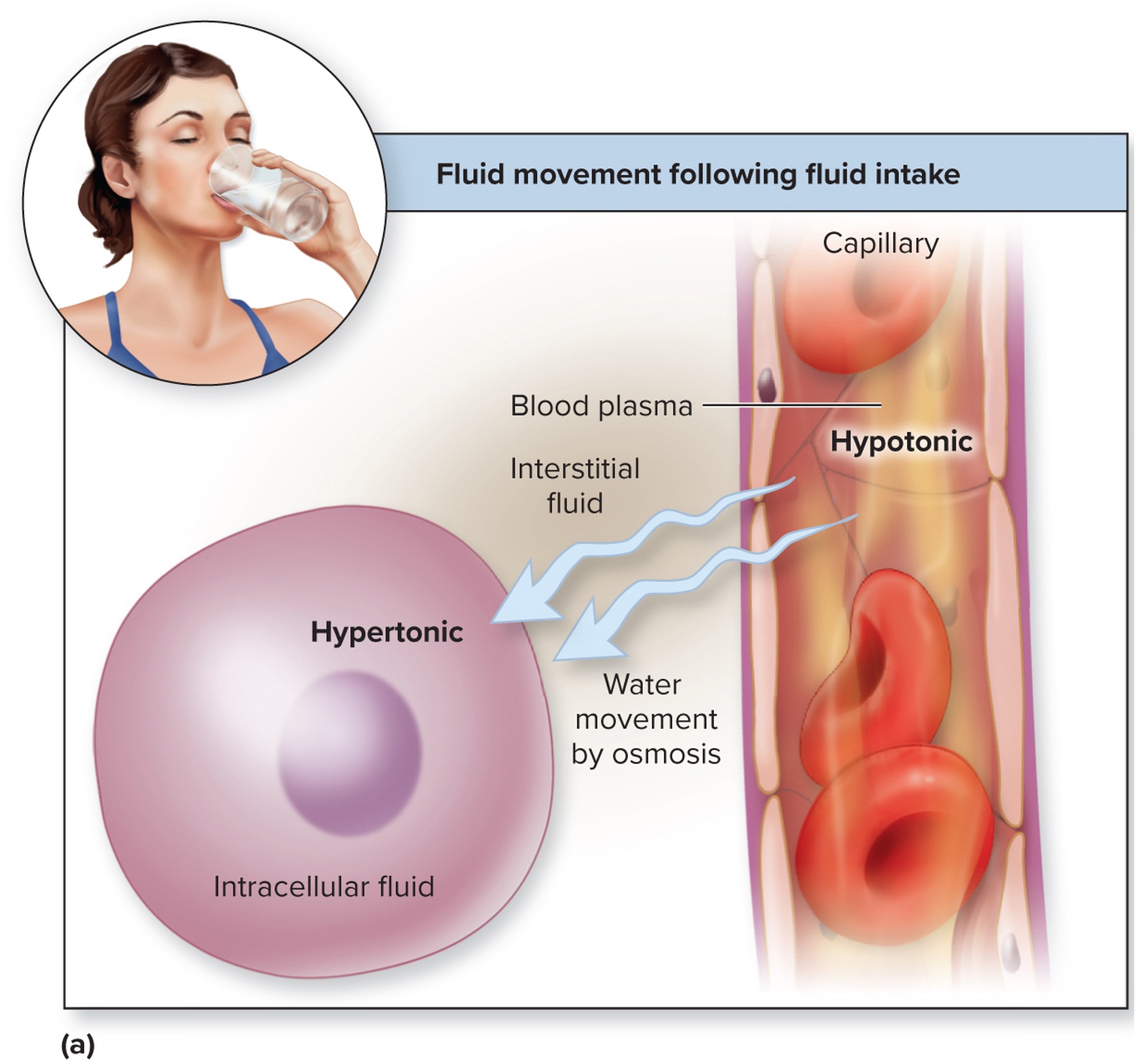
when water enter the body, does the plasma osmolarity decreases or increases?
decreases; because the water dilute the solute concentration (e.g., sodium, chlorides) within the blood
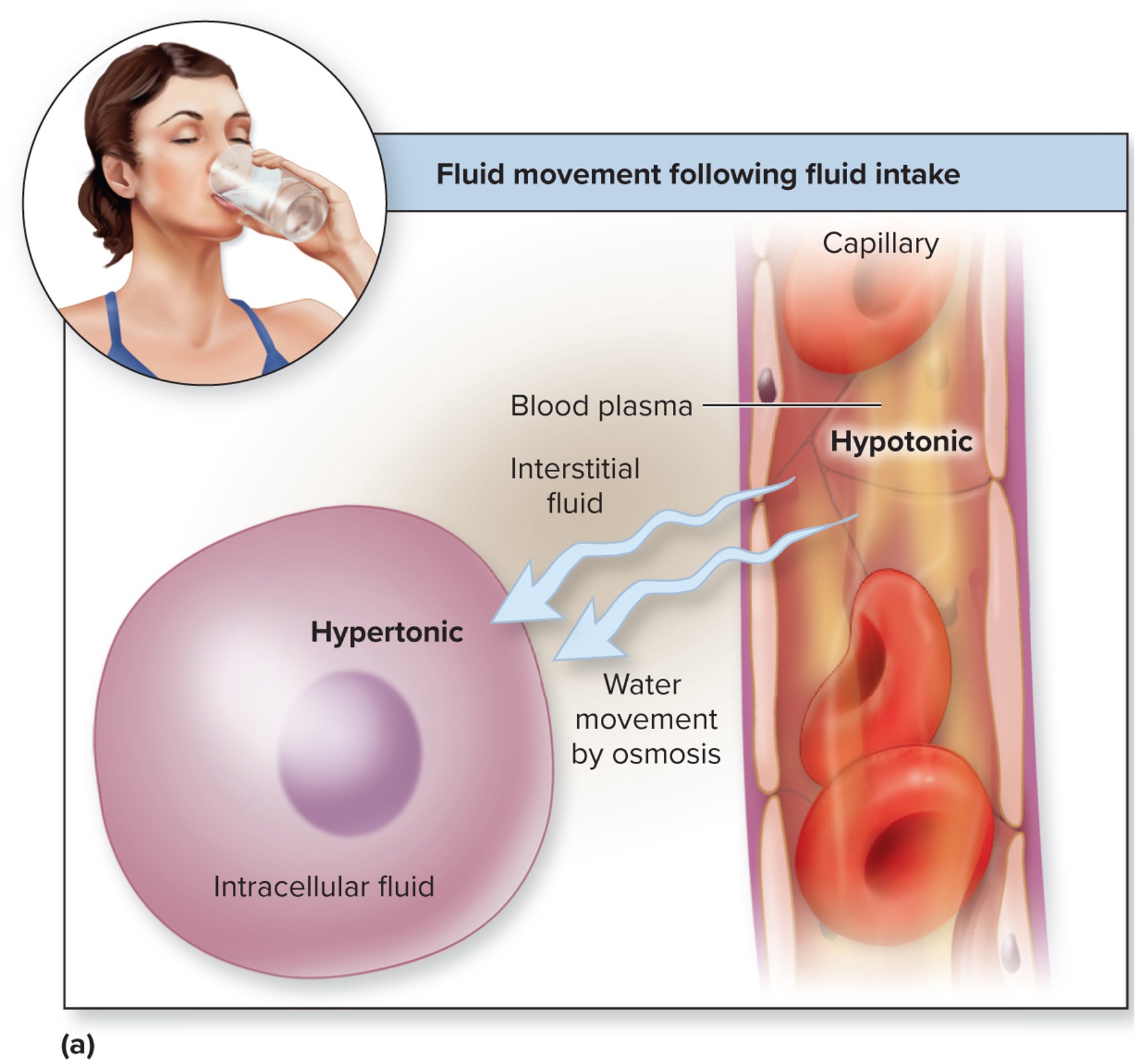
hypotonic
when the solute concentration outside the cell is lower compared to inside the cells, thus water moves into the cells and potentially burst it
hypertonic
when the solute concentration outsde the cell is higher compared to inside the cells, thus mwater move out of the cells and potentially shrink it
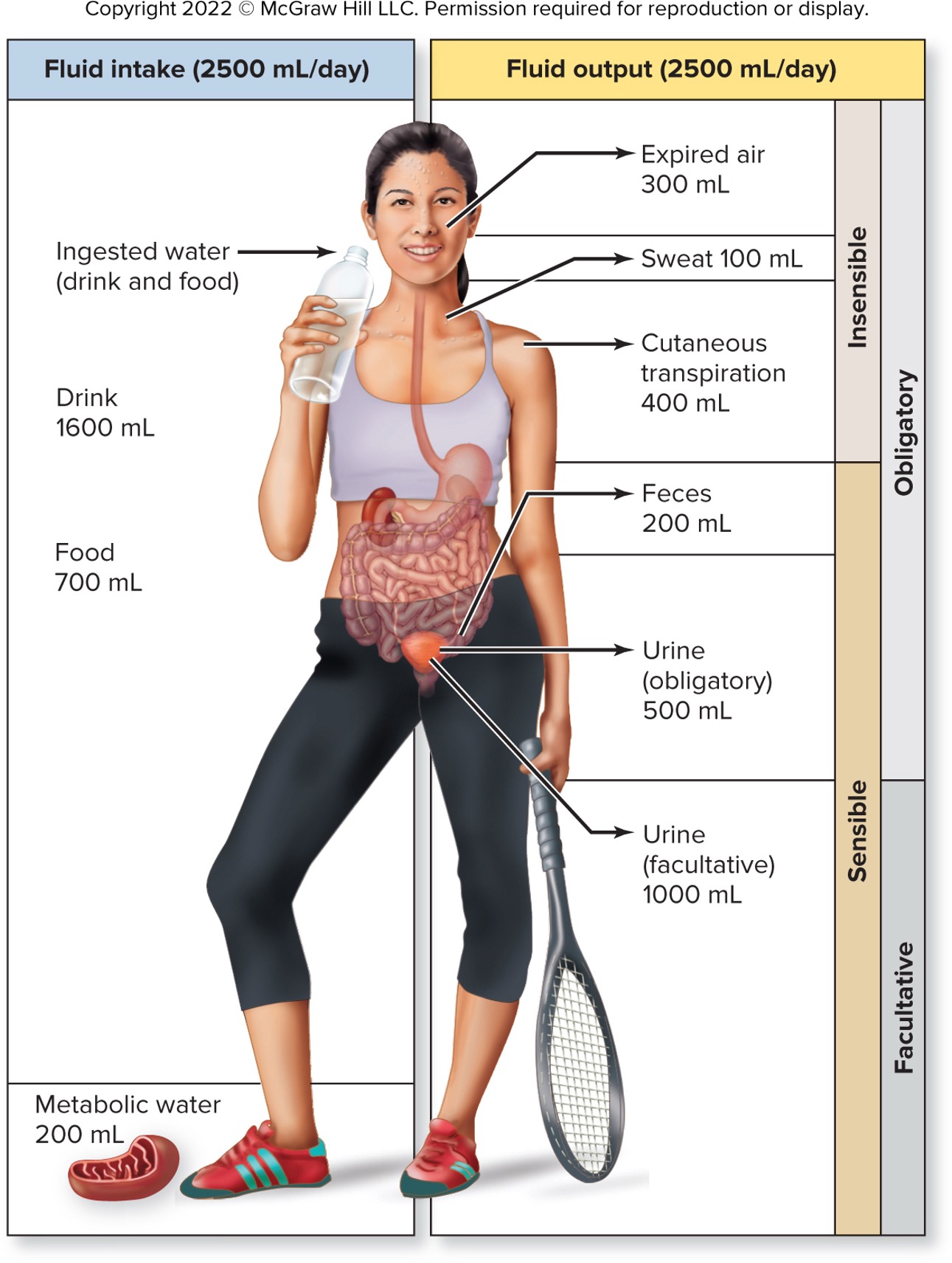
fluid intake is ___________ to fluid output
equal
ingested water
water absorbed from food and drink; about 2300 mL per day
metabolic water
water produced from aerobic cellular respiration and dehydration synthesis; about 200 mL per day
what is the average loss of water from the body per day and some of the ways the water is lost?
2500 mL per day; breathing, sweating, evaporation of water through skin (cutaneous transpiration), defecation, urination
what are the ways that water loss can be described as?
sensible/insensible
obligatory/ facultative
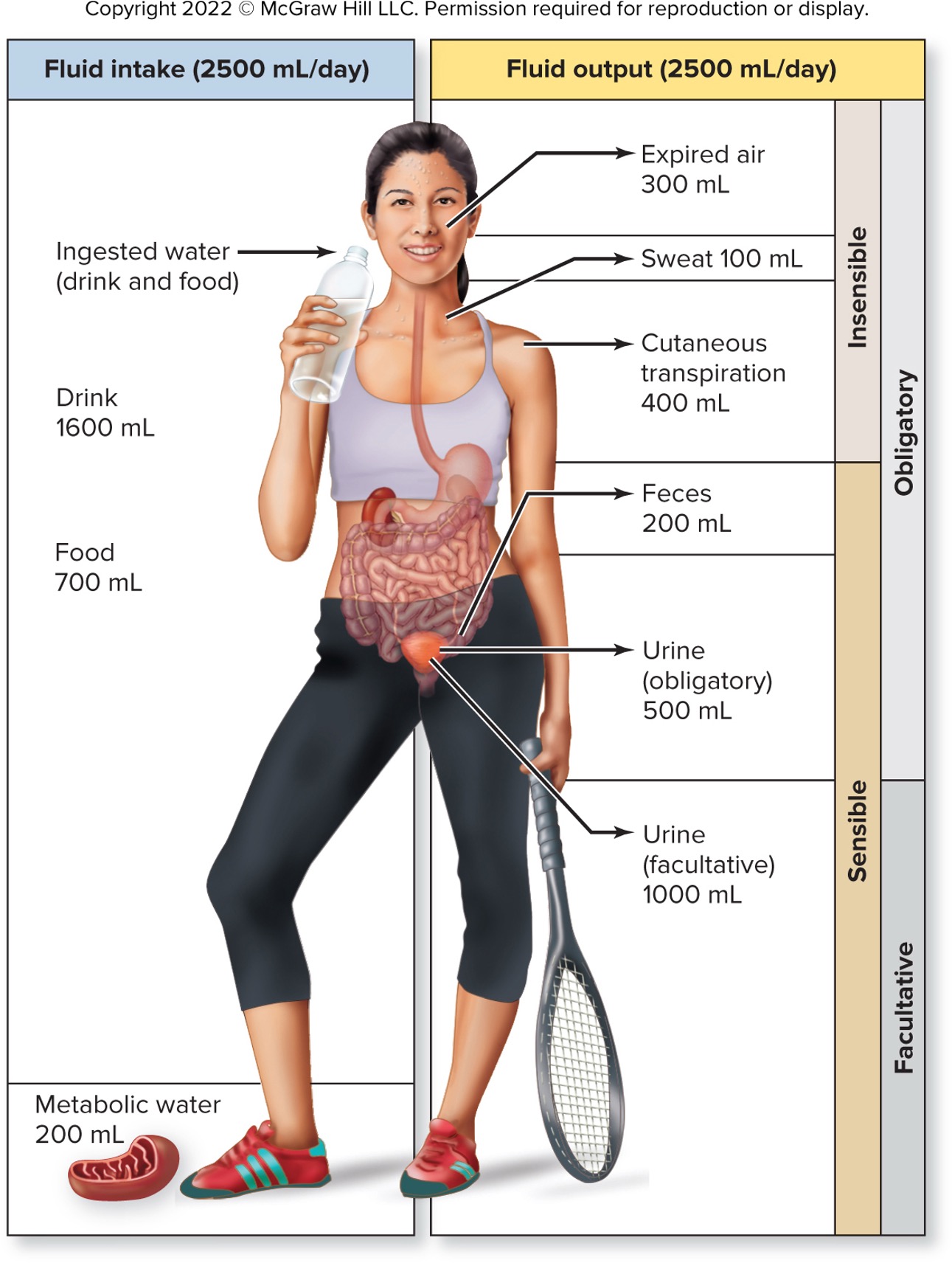
sensible water loss
measureable
include fluid lost through feces and urine
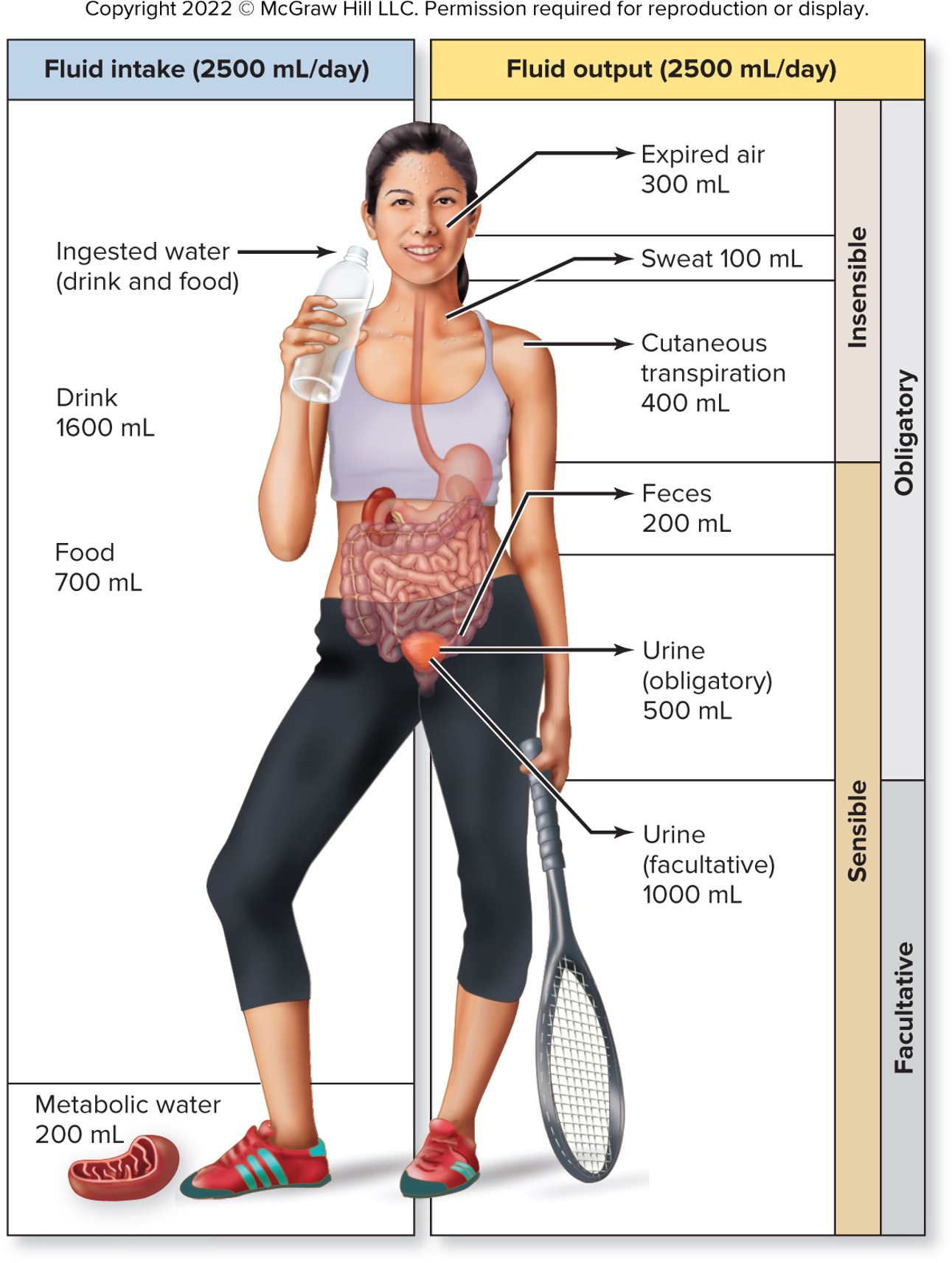
insensible water loss
not measreuable
fluid lost in expired air
fluid lost from skin through sweat and cutaneous transpiration
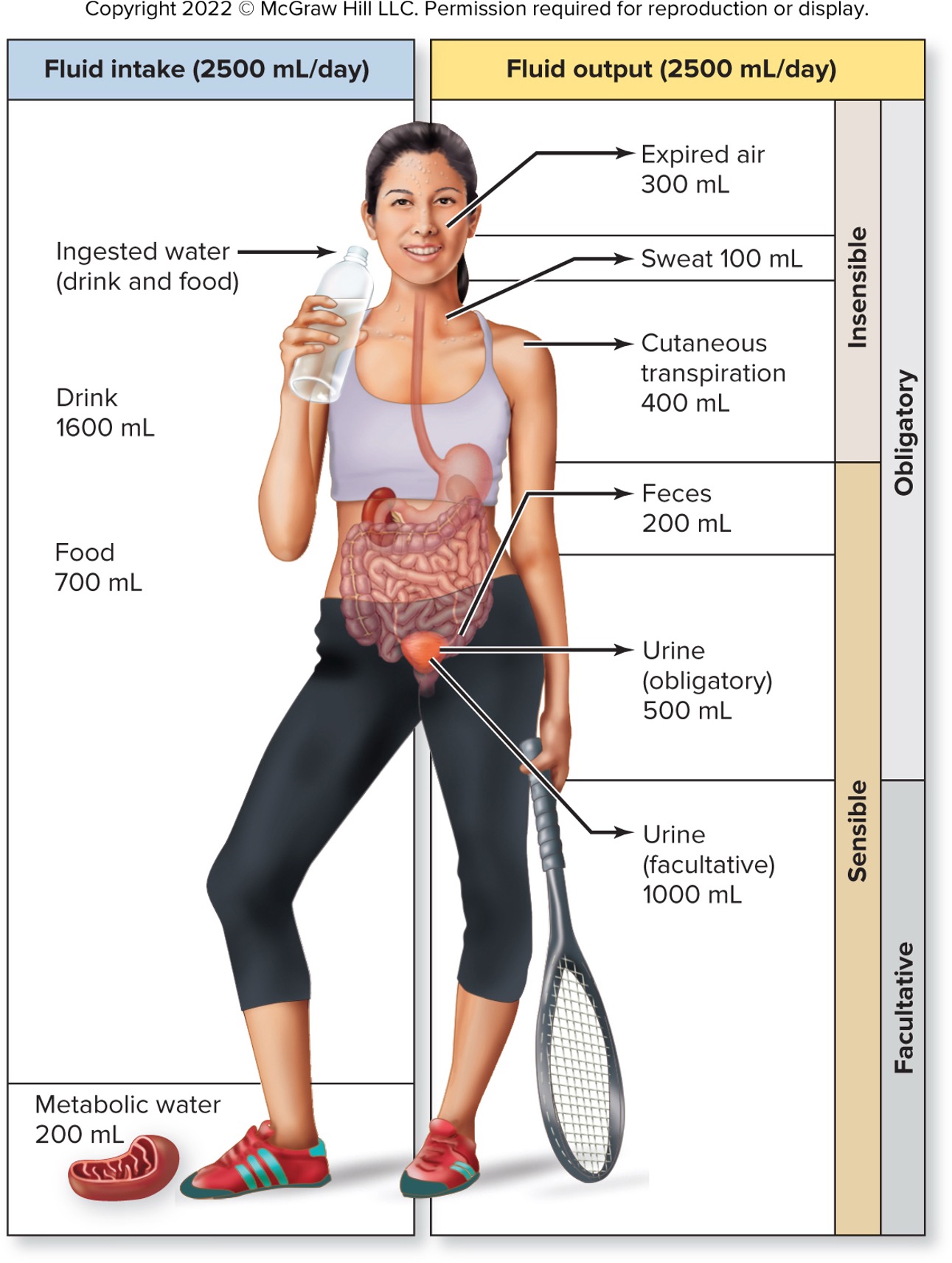
obligatory water loss
loss of water that always occur
water lost through breathing adn through the skin
water lsot through feces and minimal urine needed to eliminate waste
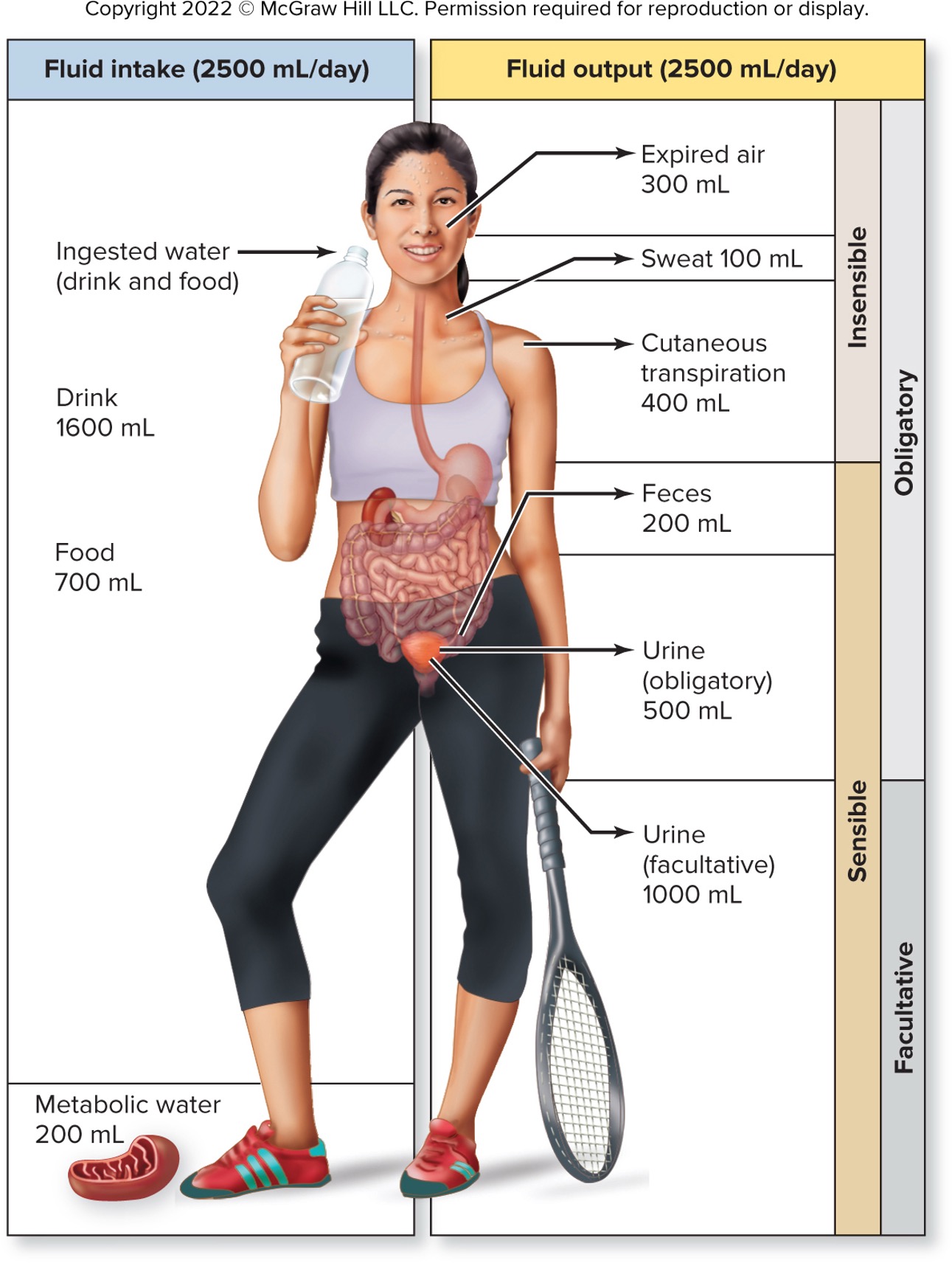
facultative water loss
controlled water loss
dependent on hydration of the body
hormonally regulated in kidney nephrons (only mechanism to control fluid output and can decrease fluid loss if the body is dehydrated)
what are the different type of fluid imbalance with constant osmolarity?
volume depletion
volume excess
volume depletion
fluid imbalance with constant osmolarity
occurs when isotonic fluid loss is greater than isotonic fluid gain
e.g., hemorrhage, severe burns, chronic vomiting, diarrhea, hyposecretion of aldosterone
volume excess
fluid imbalance with constant osmolarity
isotonic fluid gain is greater than isotonic fluid loss
fluid intake normal but decreased fluid loss through kidneys
Caused by kidney/heart failure or hormonal excess (e.g., aldosterone).
what are the different type of fluid imbalance with changing osmolarity?
dehydration
hypotonic hydration
dehydration
fluid imbalance with changes in osmolarity
water loss greater than loss of solutes
result from profuse sweating, diabetes, intake of alcohol, hyposecretion of ADH, insufficient water intake, overexposure to cold weather
water shifts from cells into interstitial fluid and blood plasma
possible dehydration of body cells
hypotonic hydration
fluid imbalance with changes in osmolarity
water intoxication
can result from ADH hypersecretion
usually from drinking large amount of plain water
Both Na+ and water lost during sweating
plasma becomes hypotonic
fluid moving from blood plasma into interstitial fluid and into cells
possible swelling of cells
fluid sequestration
total body fluid is normal but distributed abnormally
edema
puffiness with fluid accumulation in interstitial space
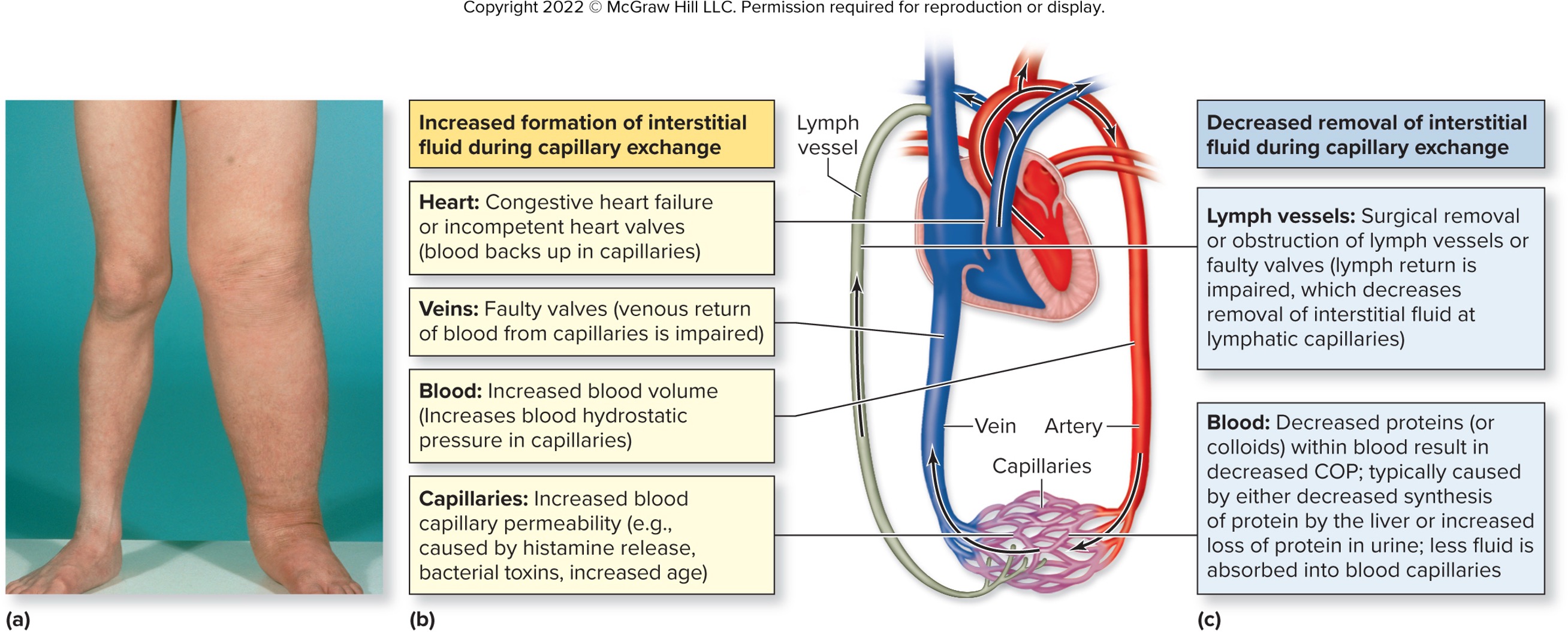
ascites
accumulation of fluid within the peritoneal cavity
pericardial effusion
accumulation of fluid in pericardial cavity
pleural effusion
accumulation of fluid in pleural cavity
regulting fluid balance is important at regulating _______________, ___________, and ______________
blood volume
blood pressure
blood plasma osmolarity
what happen to blood pressure, blood volume, and blood osmolarity when fluid intake is less than output?
decreases blood pressure and blood volume
increases blood osmolarity if more water is lost than solutes
what happen to blood pressure, blood volume, and blood osmolarity when fluid intake is greater than output?
increases blood pressure and blood volume
decreases blood osmolarity if water gain exceeds solute gains
what are the stimuli that activate the thirst center?
decreased blood volume and blood pressure (renin → angiotensin II → activate thirst center0
increased blood osmolarity (trigger hypothalamus to release ADH)
decreases salivary secretions (from mucous membrane)
what are the stimuli that inhibits the thirst center?
increased blood volume and blood pressure (inhibited released of renin → decreased angiotensin II)
decreased blood osmolarity (decreased secretion of ADH)
increased salivary secretions
distention of stomach (stretch caused by fluid entering)
Nonelectrolytes
molecules that do not dissoacite in solutions
most covalently bonded organic molecules
electrolytes
dissociates in solution to form cations and anions
have the abilityt to conduct electrical current when dissolved
each have unique osmotic functions
concentration given as milliequivalents/L (mEq/L)
28-37
99% of sodium ion is presented in ___________ fluid
extracellular
what are the hormones that regulate concentration of sodium in the body through urine?
aldosterone
ADH
ANP
which ions exert the greatest osmotic pressure?
sodium
what is the most important electrolyte in determining blood plasma osmolarity and regulating fluid balance?
sodium
ECF is ___________ if Na_ concentration increased
hypertonic
ECF is ___________ if Na+ concentration decreased
hypotonic
where is the most abundant source of calcium?
bone and teeth
retention of Na+ and water causes _________ in blood volume and blood pressure
increase
hypernatremia
above normal level sodium
hyponatremia
below normal level sodium
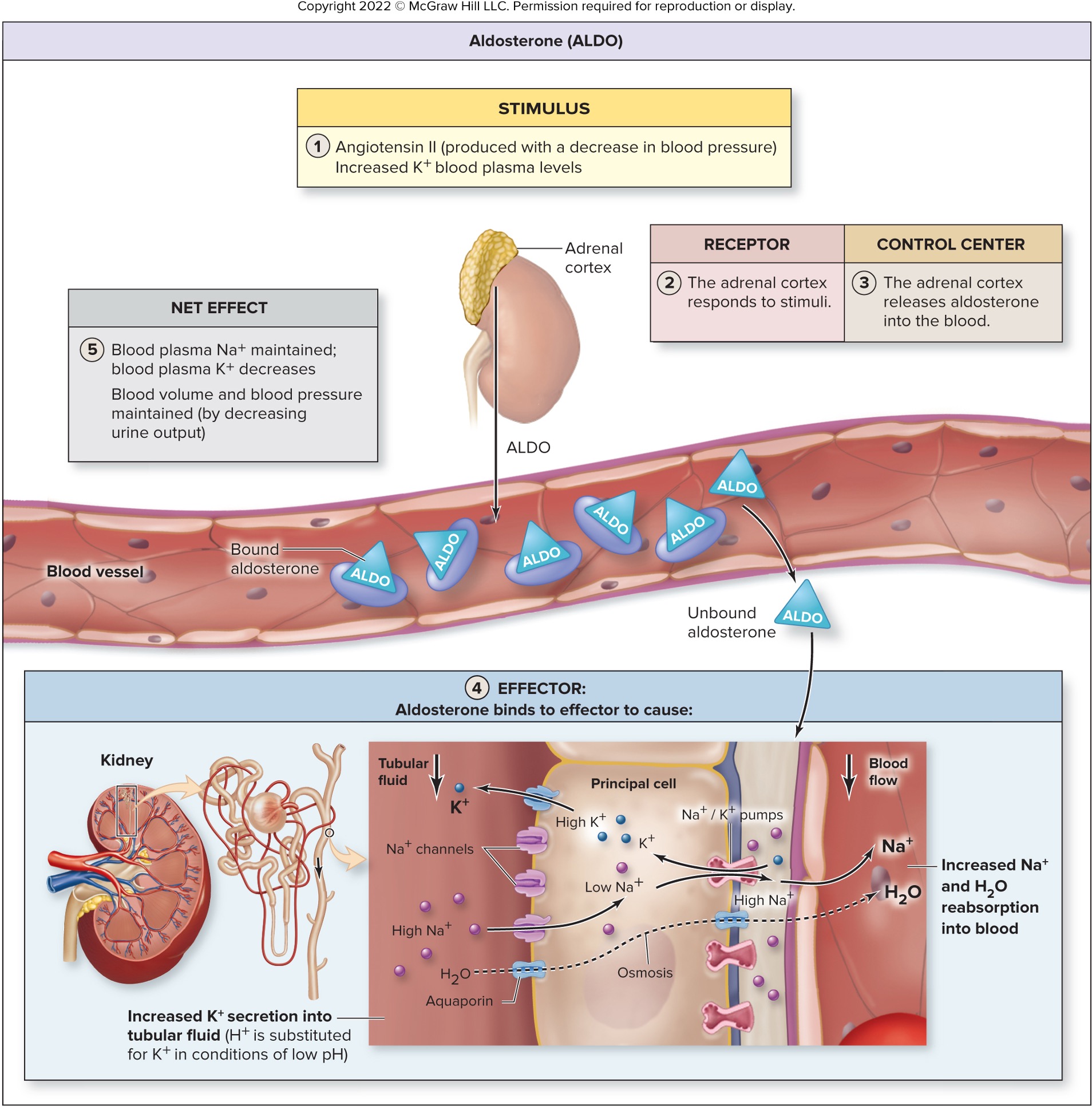
how does aldosterone regulate fluid balance?
retain Na+ and water
maintain Na+ blood plasma concentration
how does ADH regulate fluid balance?
retains water
decreases Na+ blood plasma concentration
how does ANP regulate fluid balance?
increases excretion of Na+ and H2O
decreases Na+ blood plasma concentration
which ions is essential in exerting intracellular osmotic pressure?
potassium (K+)
potassium is extremely important for ________ activities and controlling _______ rhythm
neuromuscular; heart
which ions have the most lethal of electrolyte imbalances?
potassium → cardiac or respiratory arrest
hyperkalemia
above normal level potassium
hypokalemia
below normal level potassium
functions of calcium
muscle contraction
nerve impulse
true or false: sodium is the most common type of electrolyte imbalance
true
where is phosphate most abundant in?
ICF but can also be found in DNA, RNA, and phospholipids
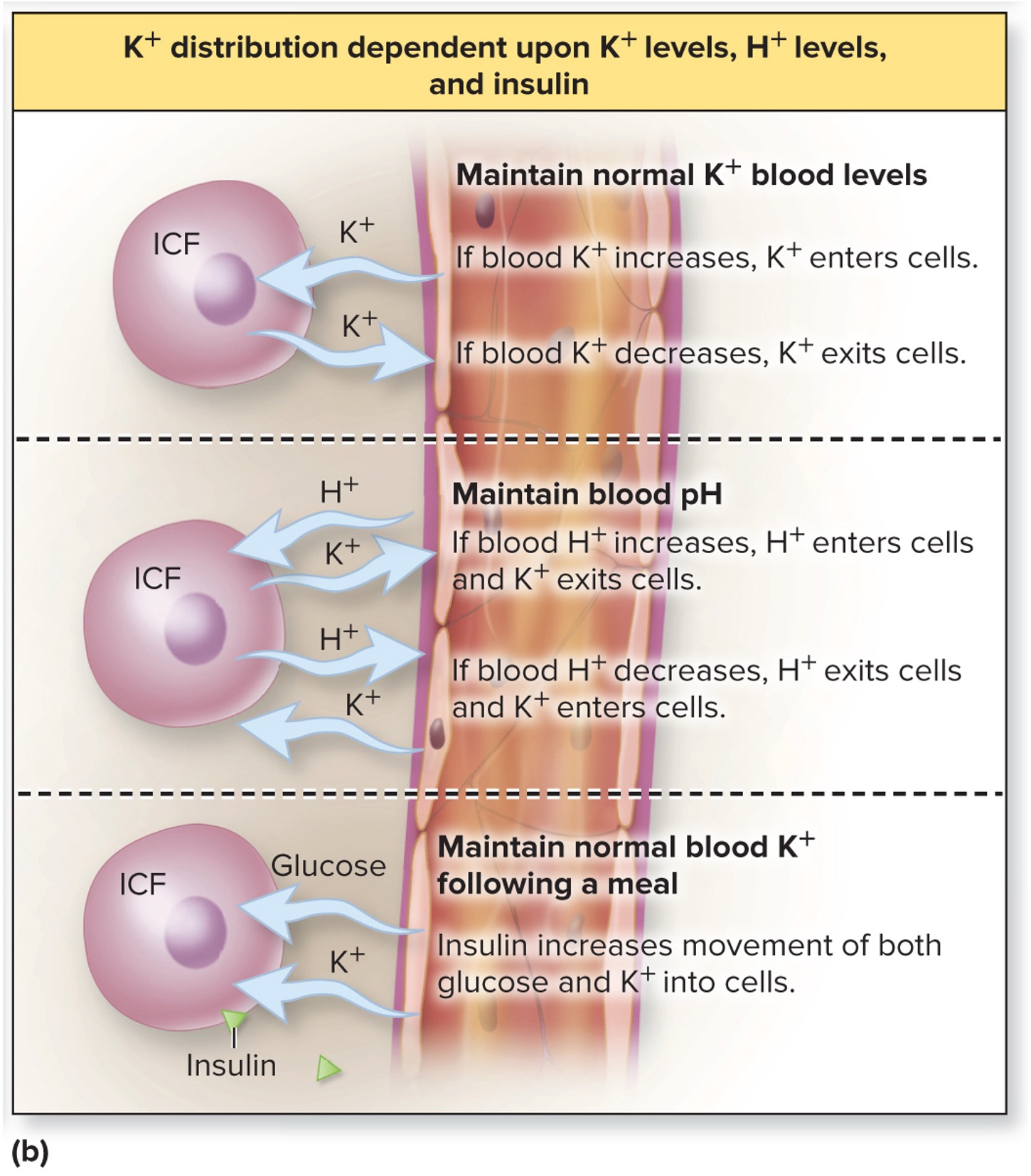
changes in blood plasma K+ and H+ concentration can cause __________ shift
potassium
how does aldosterone regulate potassium balance?
cause K+ secretion by kidneys (and excretion in urine)
decreases K+ blood plasma concentration
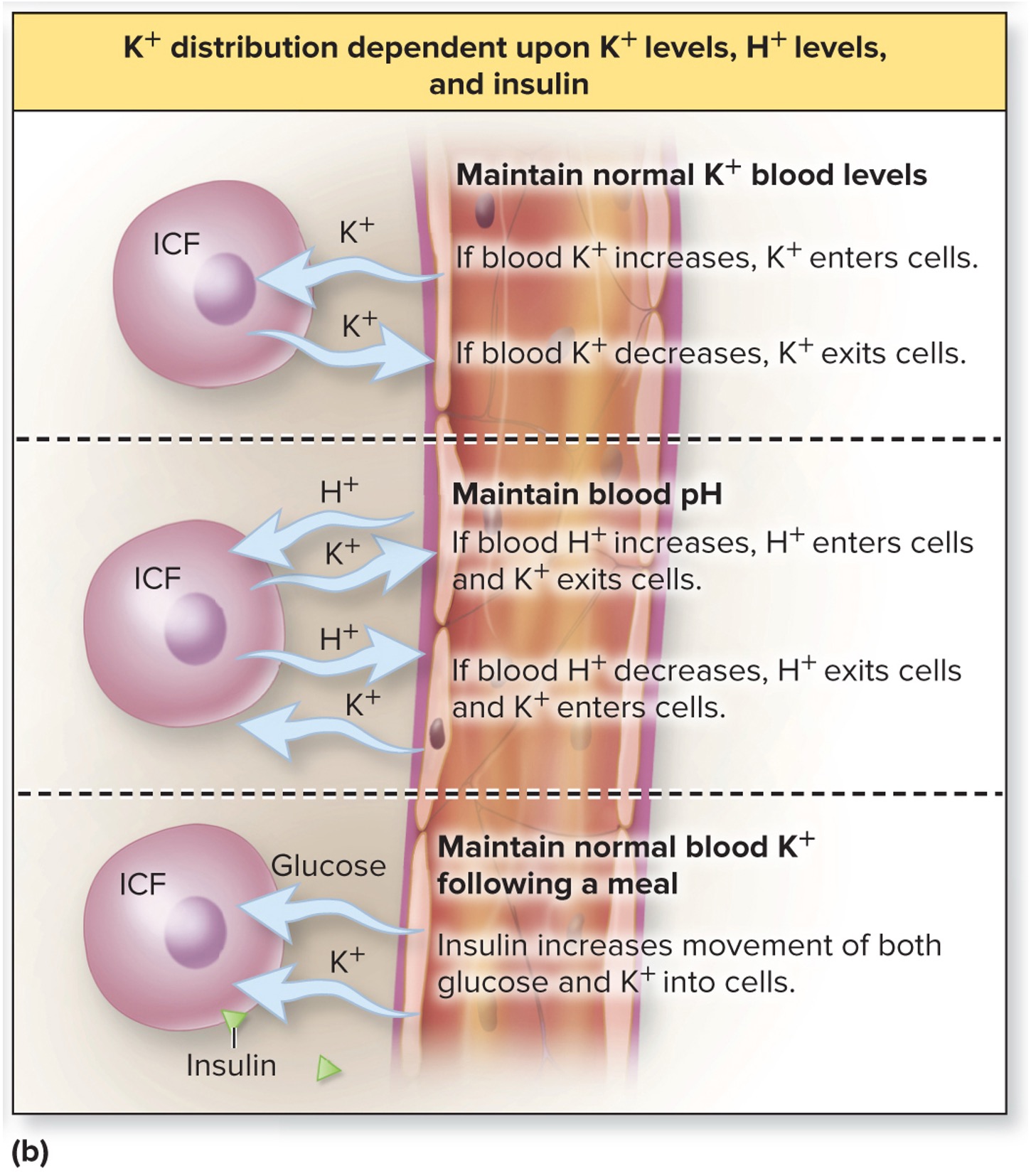
K+ distribution is dependent upon __________, ___________, and __________
K+ levels, H+ levels, insulin
what is the most abundant anion in ECF?
chloride
hyperchloremia
above normal level chloride
hypochloremia
below normal level chloride
which ions follows Na+ by electrostatic interaction with amount lost in urine dependent upon blood plasma Na+
chloride
what is the most abundant electrolytes in the bone and teeth?
calcium
what is the function of calcium?
muscle concentration
neurotransmitter release
serves as a second messenger and participates in blood clotting
hypercalcemia
above normal level calcium
hypocalcemia
below normal level calcium
what is the most abundant anion in ICF?
phosphate (PO43-)
what is the function of phosphate ions?
component of DNA, RNA and phospholipids
intracellular buffer and urine buffer
what is the second most abundant cation in ICF?
magnesium
what is the functions of magnesium?
muscle relaxation
enzymatic reactions
bone rigidity
magnesium ions is regulated through the ____________
kidneys
how does angiotensin II, antidiuretic hormone (ADH) and aldosterone regulate fluid balance?
decrease urine output to increase blood volume and pressure
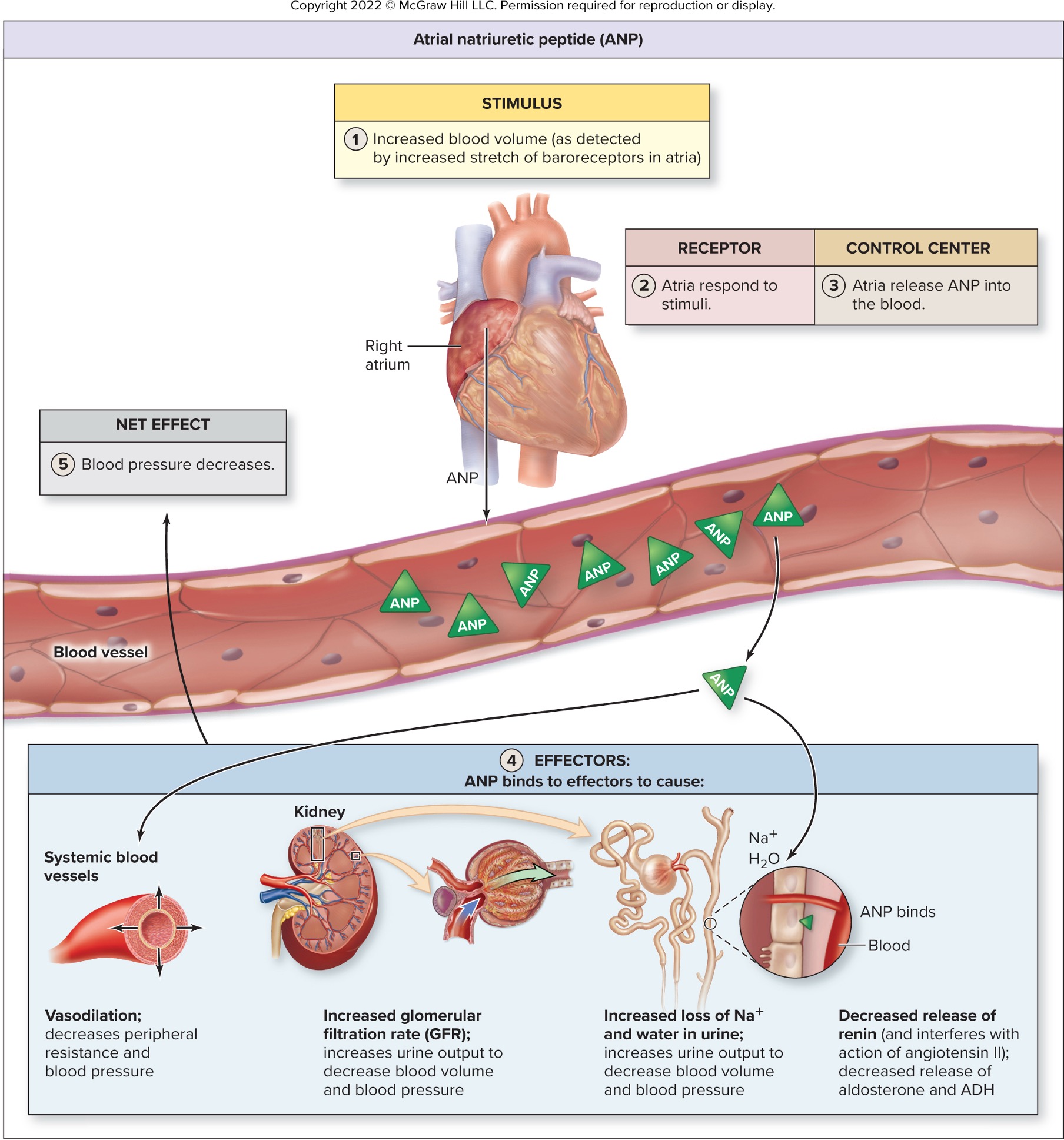
how does atrial natriuretic peptide (ANP) regulate fluid balance?
increases urine output to decrease blood volume and pressure
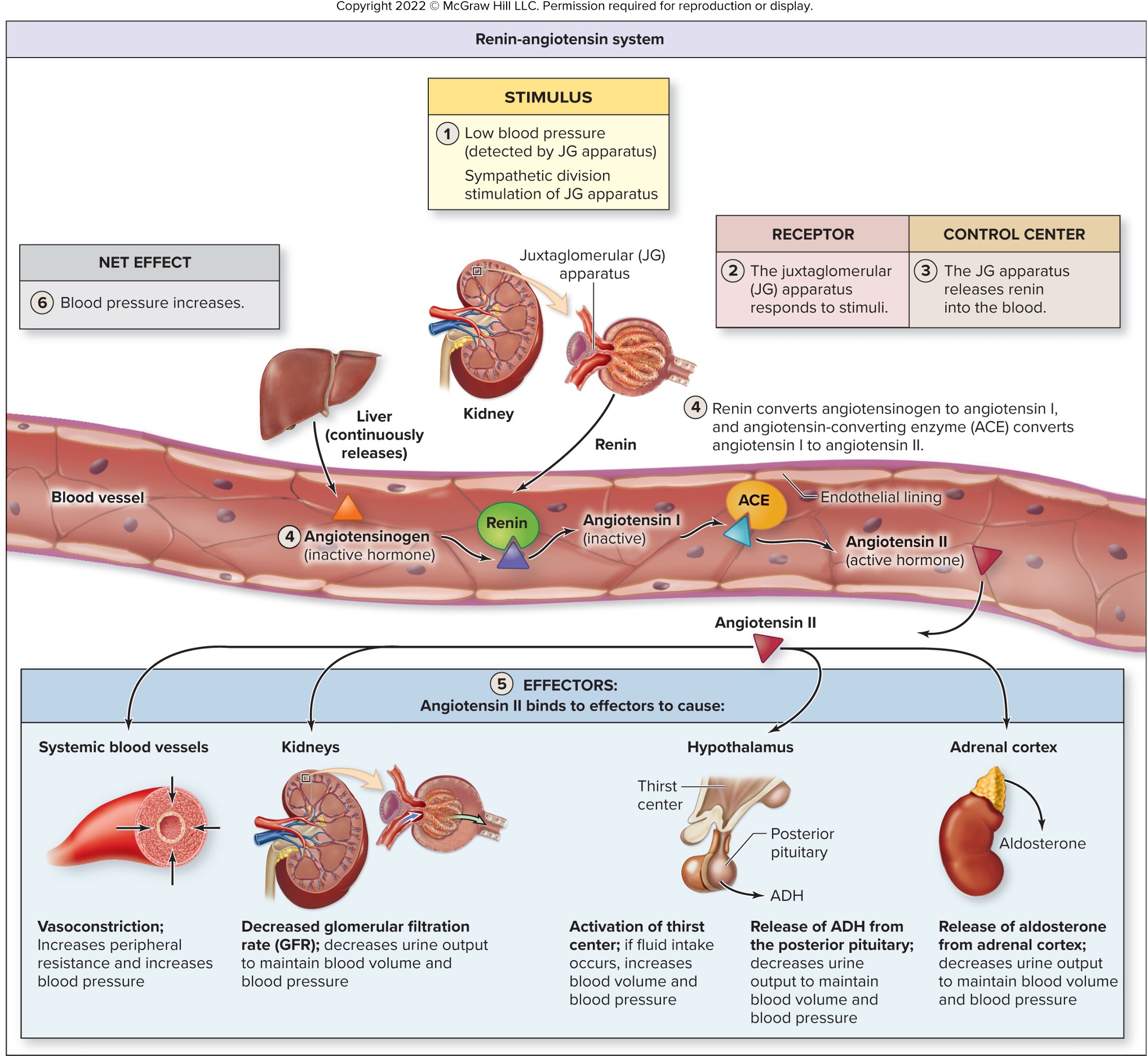
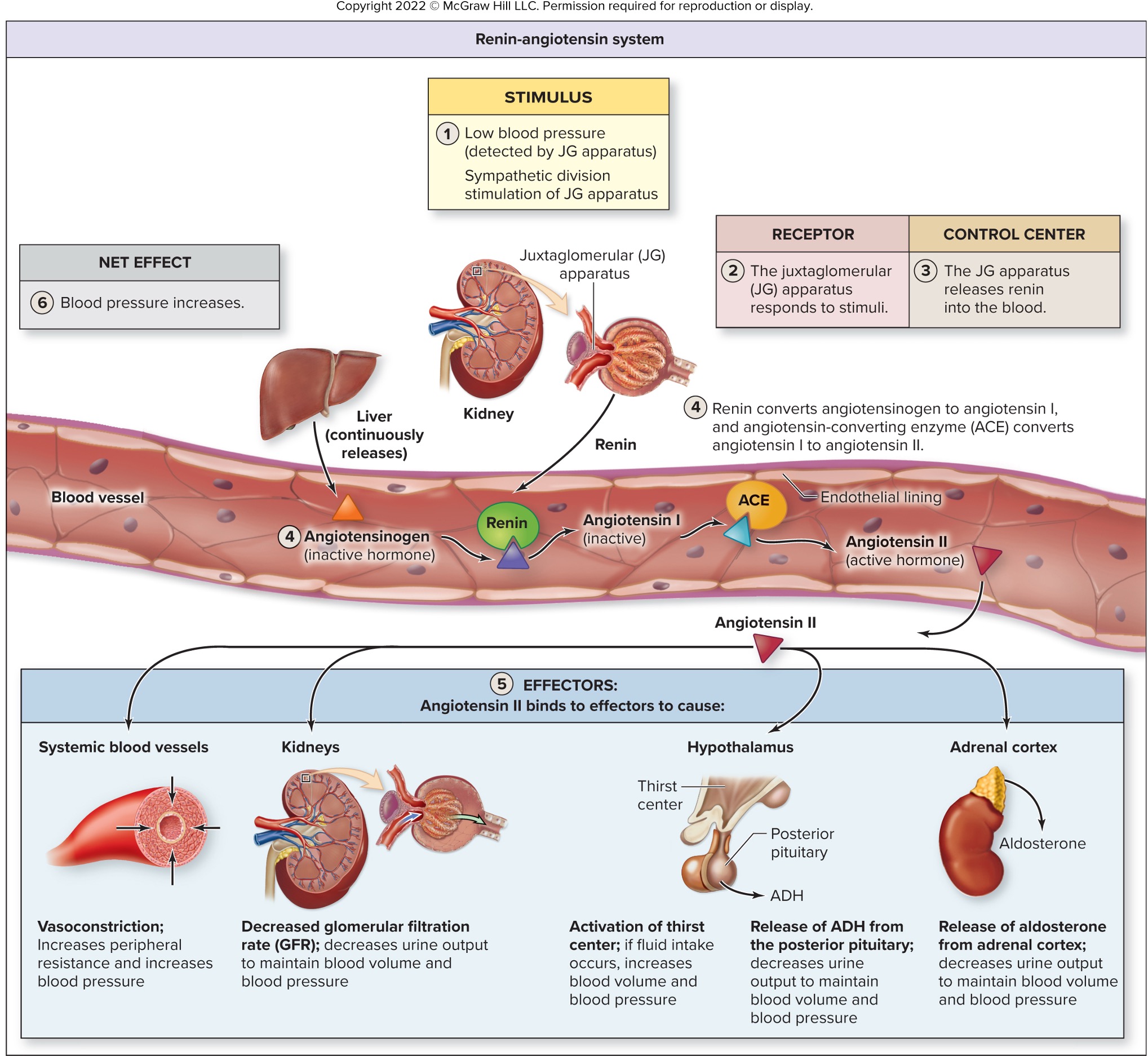
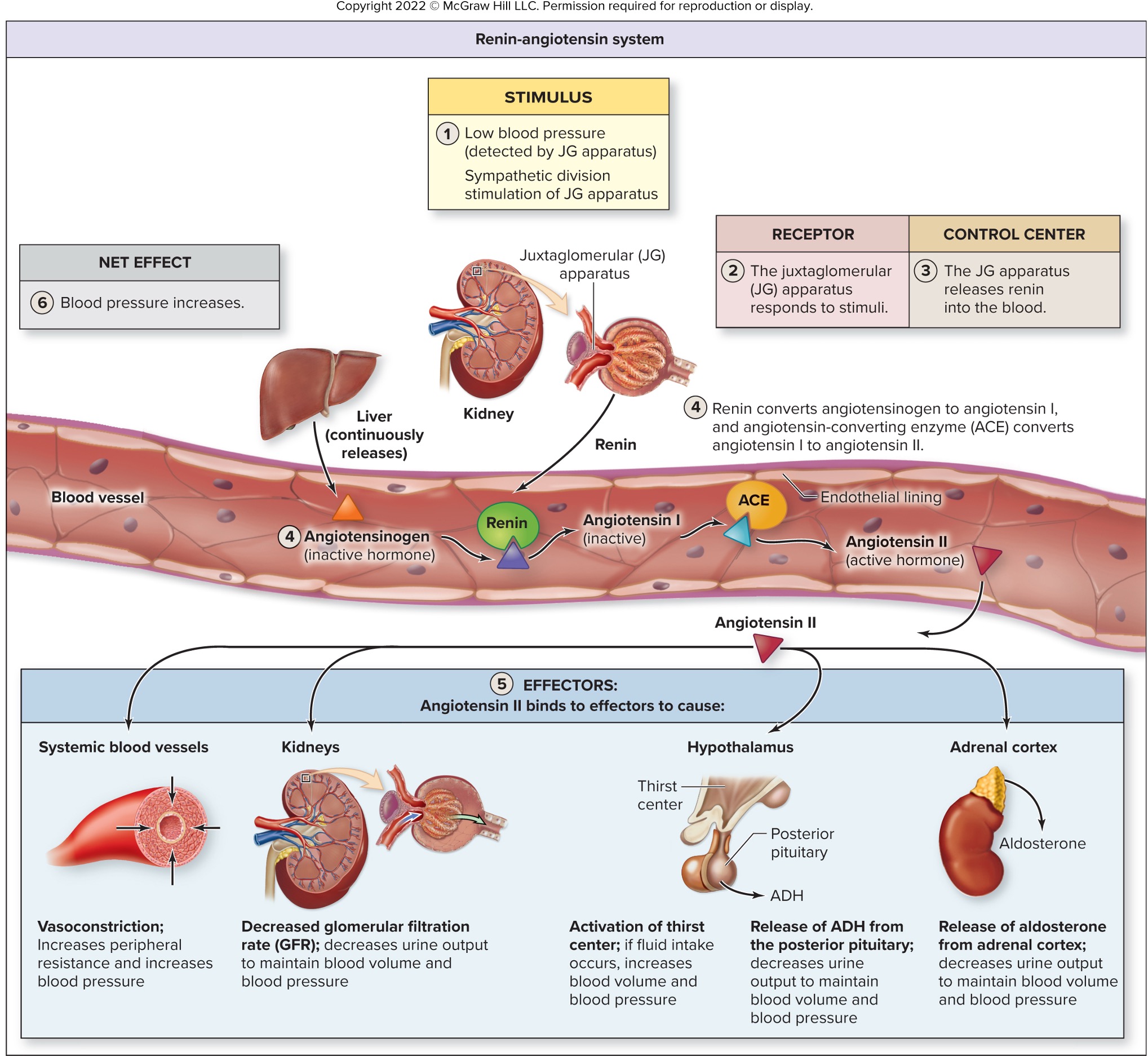
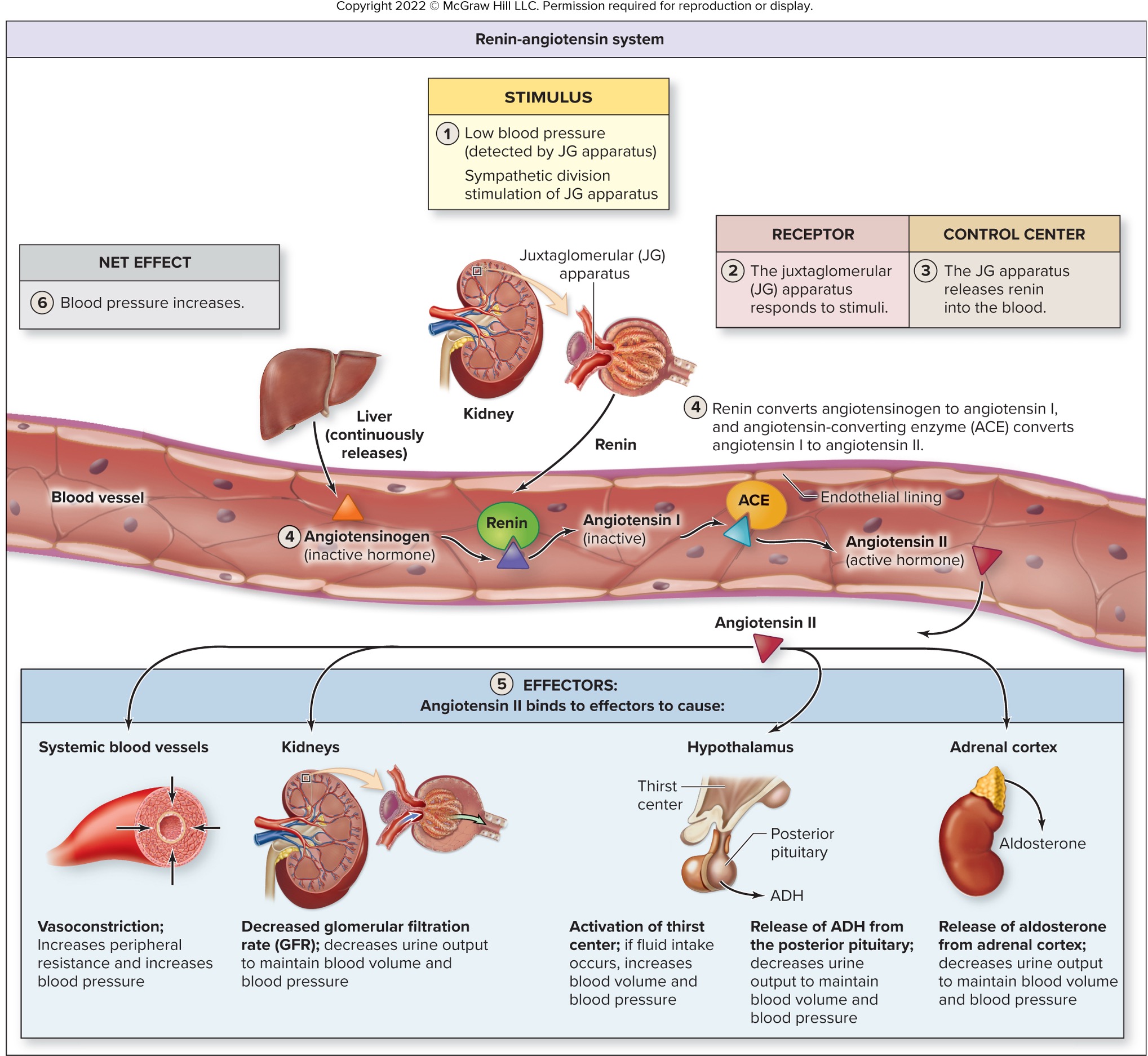
what is the pathway of blood pressure decreasing and Angiotensin, ADH, and Aldosterone at work?
BP falls → kidneys release enzyme renin into the bloodstream
renin splits angiotensin into Angiotensin I
Angiotensin I flows through the bloodstream and split into pieces, Angiotensin II, by angiontensin-converting enzyme (ACE) in the lungs and kidneys
Angiotensin cause muscular walls of small arteries (arterioles) to constrict → increasing blood pressure
Angiotensin II trigger the adrenal glands to release aldosterone and posterior pituitary gland to release ADH
ADH and aldosterone cause kidney to retain sodium, release potassium into the urine, and decrease urine output
increased sodium cause wate retention → increased blood volume and blood pressure
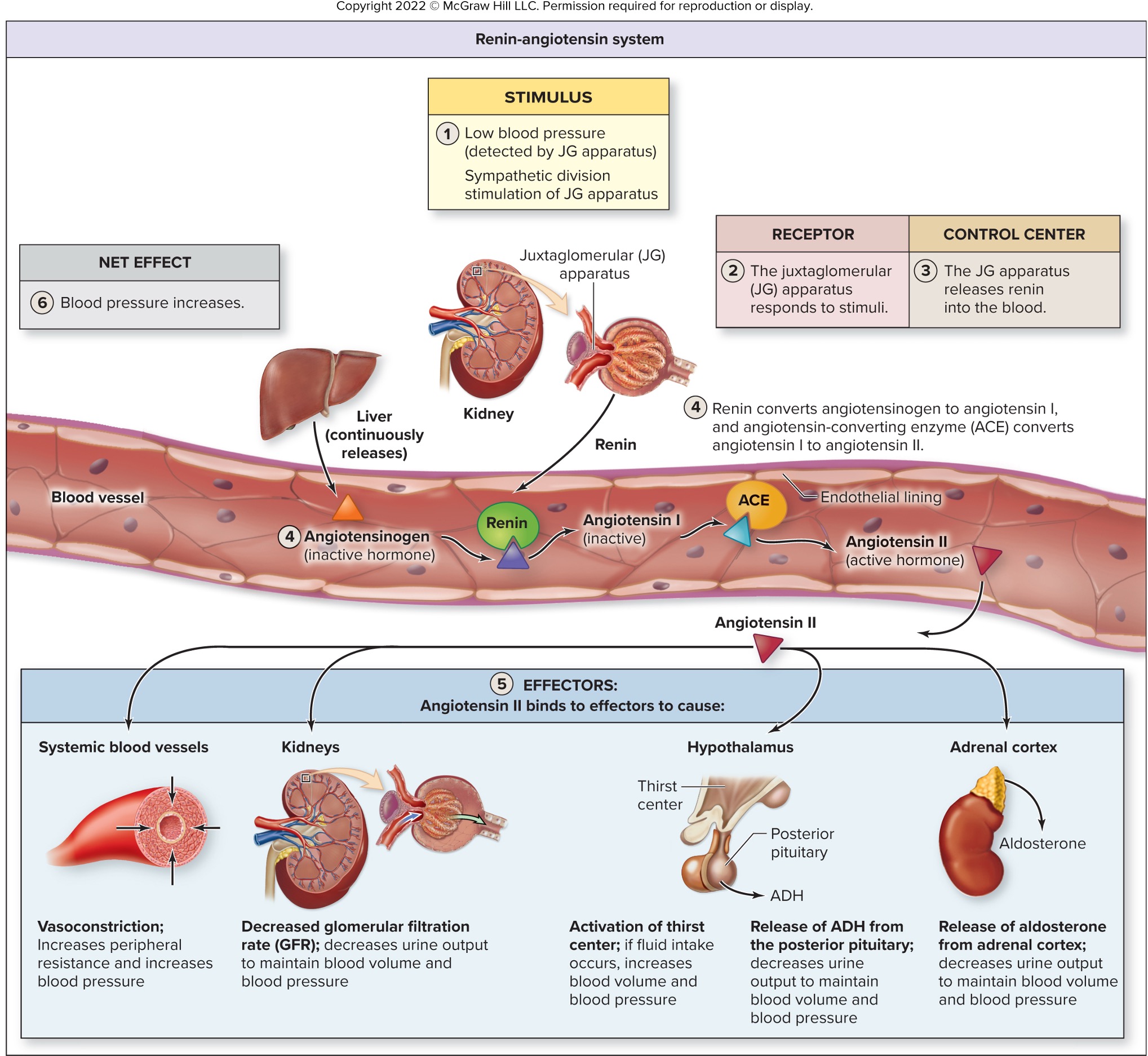
renin is released from the juxtaglomerular apparatus of the kidney in response to _________ or __________
low blood pressure (constrict the efferent now afferent); sympathetic stimulation
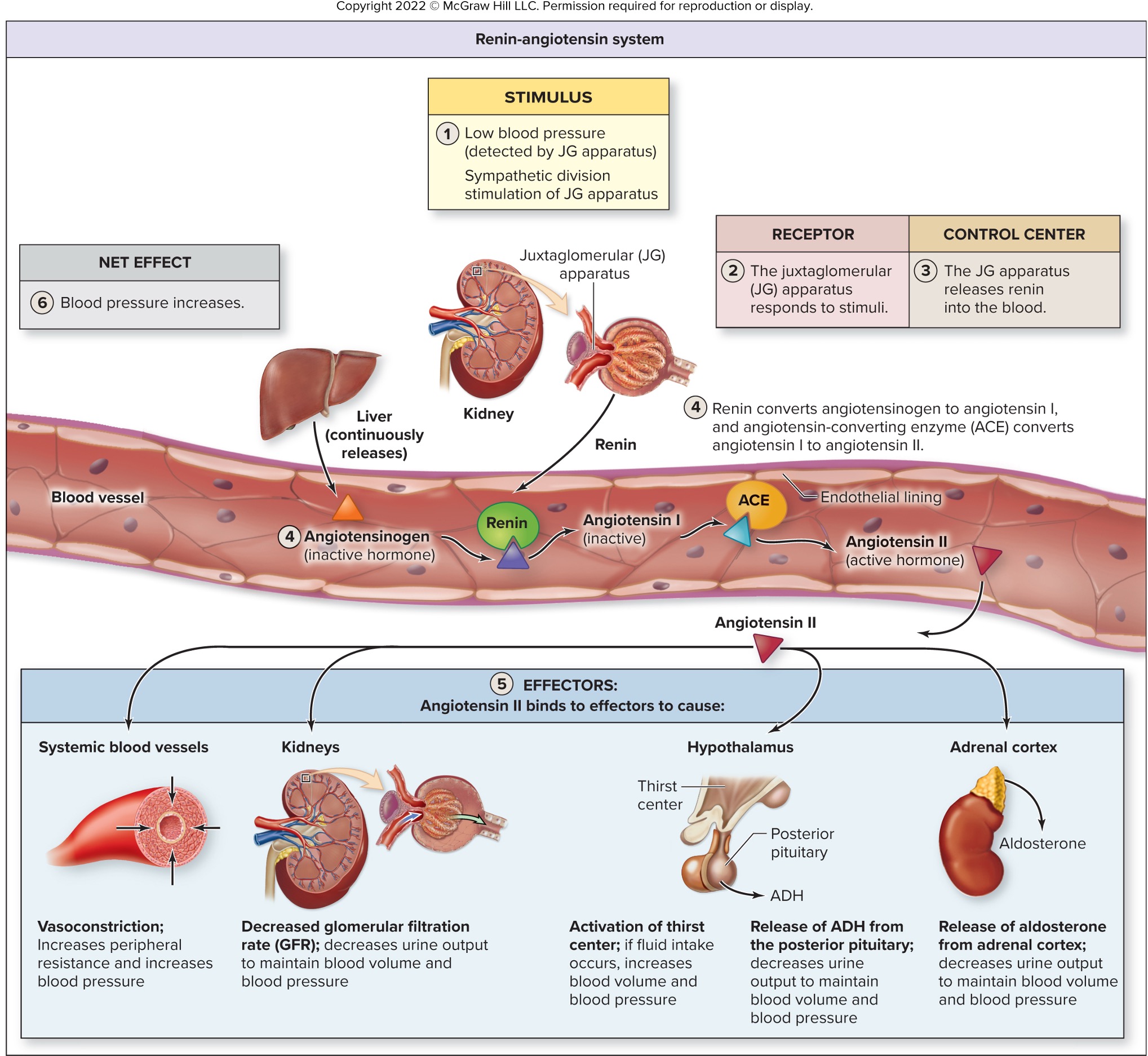
_________ and _______ cause formation of angiotensin II
renin; ACE
Low blood pressure (hypotension) and low salt/water concentration (low blood volume/effective circulating volume) trigger the formation of angiotensin II, a key hormone in the renin-angiotensin-aldosterone system (RAAS)
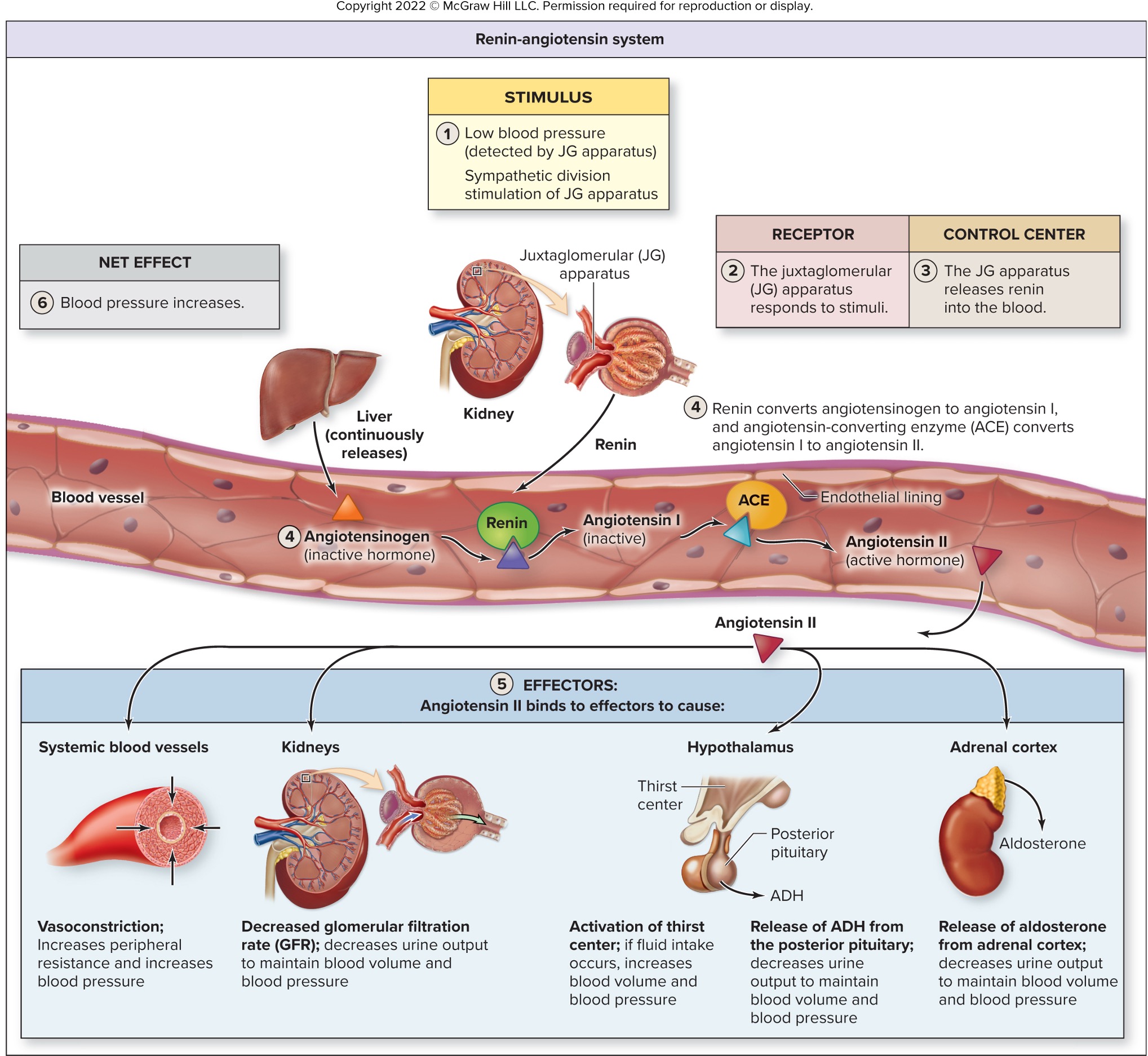
what effects does angiotensin II got on the blood vessels and kidneys?
blood vessels = vasoconstriction which increase peripheral resistance and blood pressure
kidneys = decreases urine output to hel maintain blood volume and blood pressure
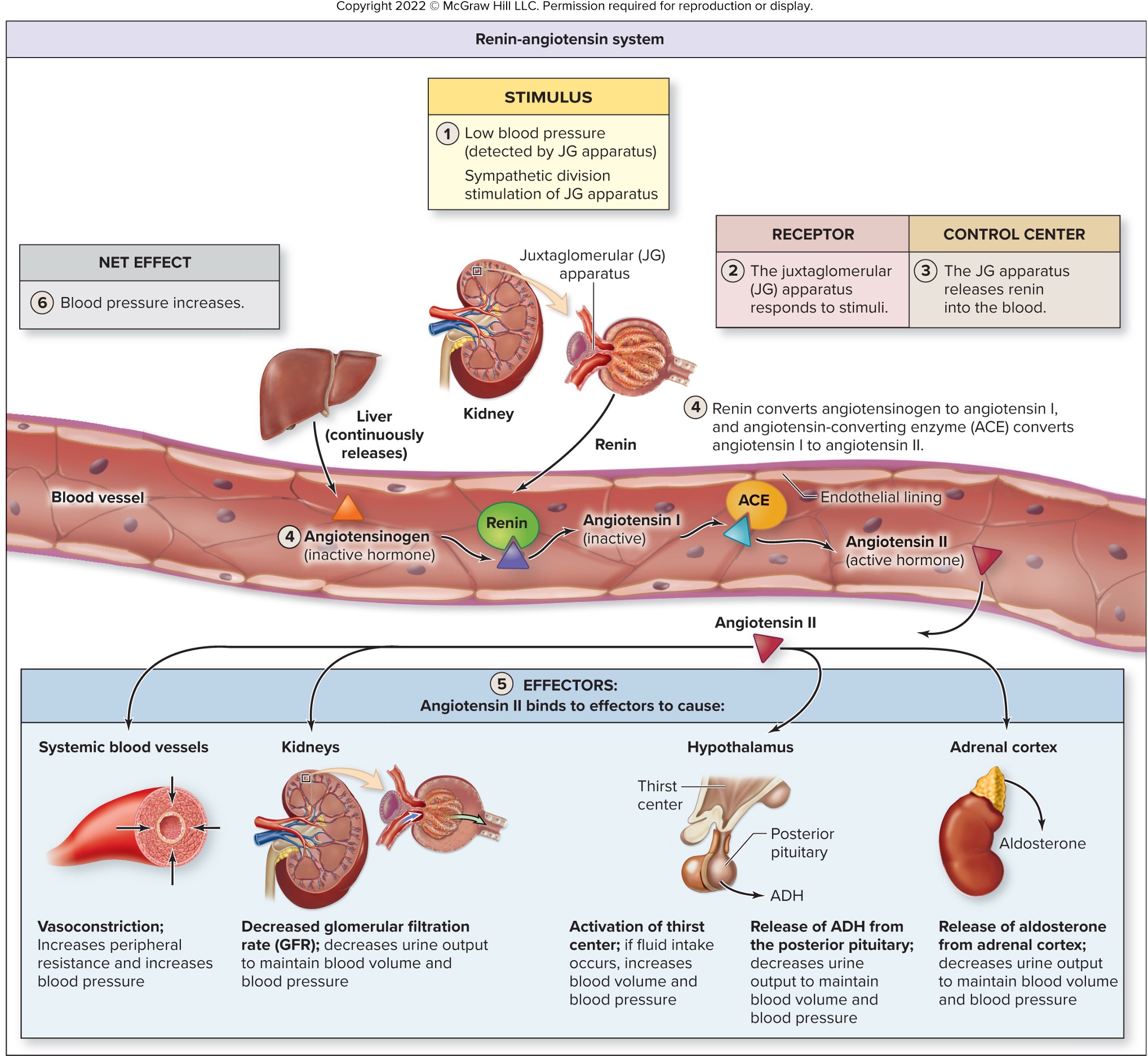
what effects does angiotensin got on the thirst center, hypothalamus, and adrenal cortex?
thirst center - increased fluid intake → increased blood volume and pressure
hypothalamus = stimulate posterior pituitary to release ADH
adrenal cortex = release aldosterone
true or false: the body would rather have low blood pressure than high
FALSE: the brian is a greedy “bastard” and want to have as much blood oxygen as possible!!!! but in all seriousness that brain dn heart need the blood supply to keep a person alive
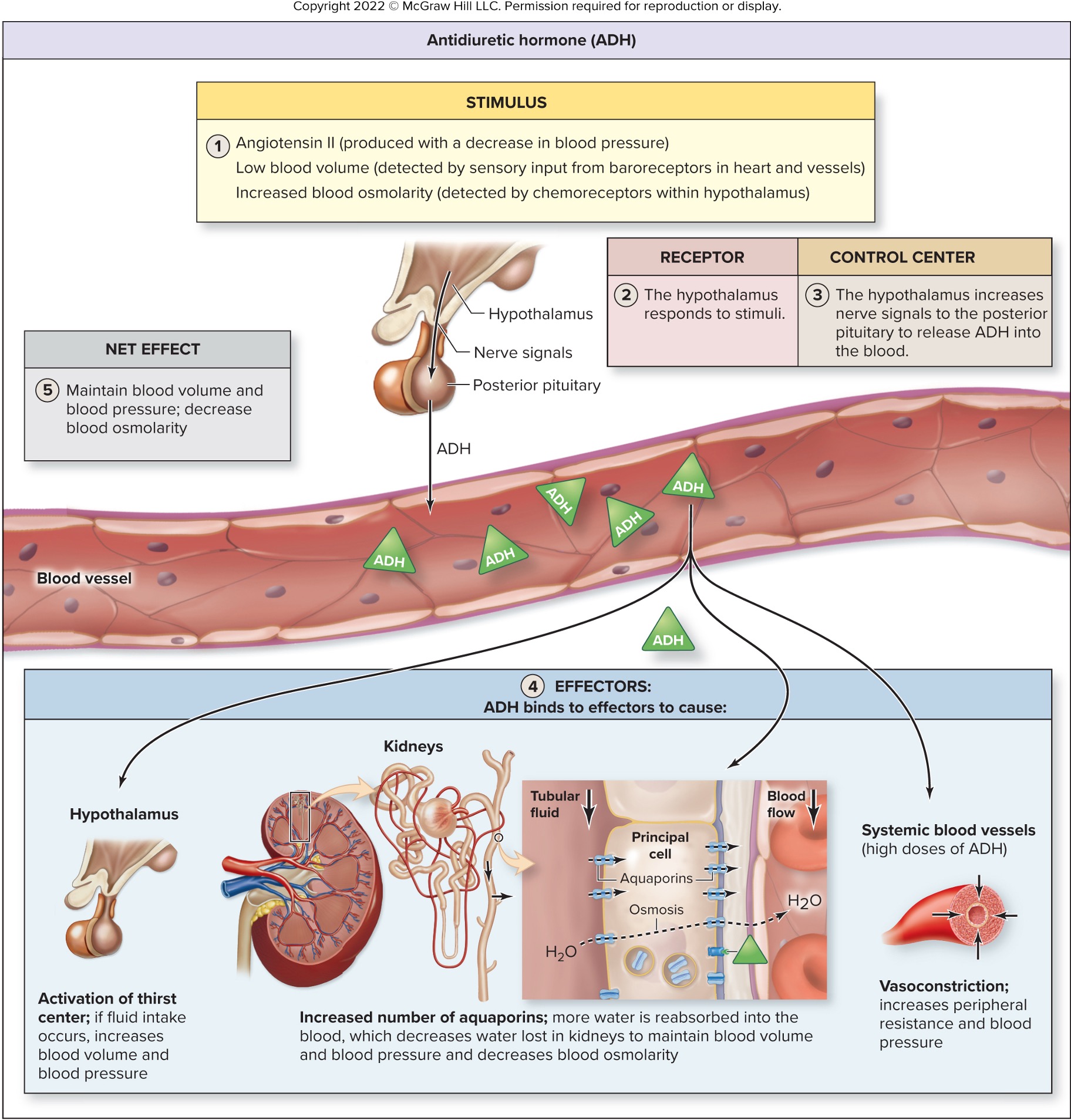
what is the primary stimulus for ADH release beside form angiotensin II?
increased blood osmolarity - detected by hypothalmic chemoreceptors
what are the changes initiated by ADH?
stimulates thirst center in the hypothalamus - fluid intake increases → increased blood volume
increases water reabsorption in the kidneys
stimulates principals cells to increase number of aquaporins (more water channels to let more water in)
vasoconstriction of systemic blood vessels → increase peripheral resistance and systemic blood pressure
aldosterone is a ________ hormone
steroid
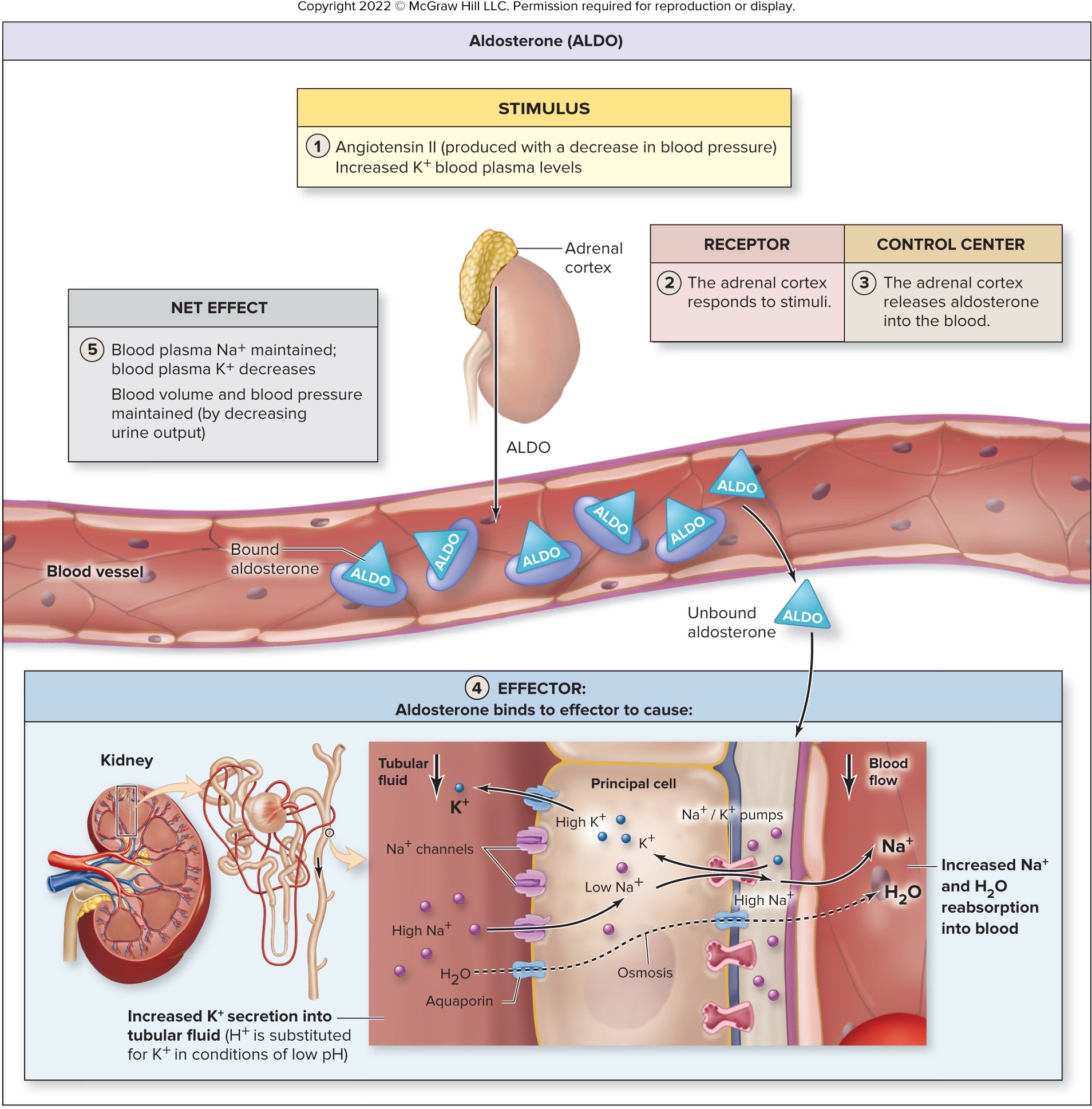
aldosterone respond to ___________, ____________, ___________
angiotensin II
decreased blood plasma Na+ levels (decreased water retention)
increased blood plasma K+ (decreased water retention)
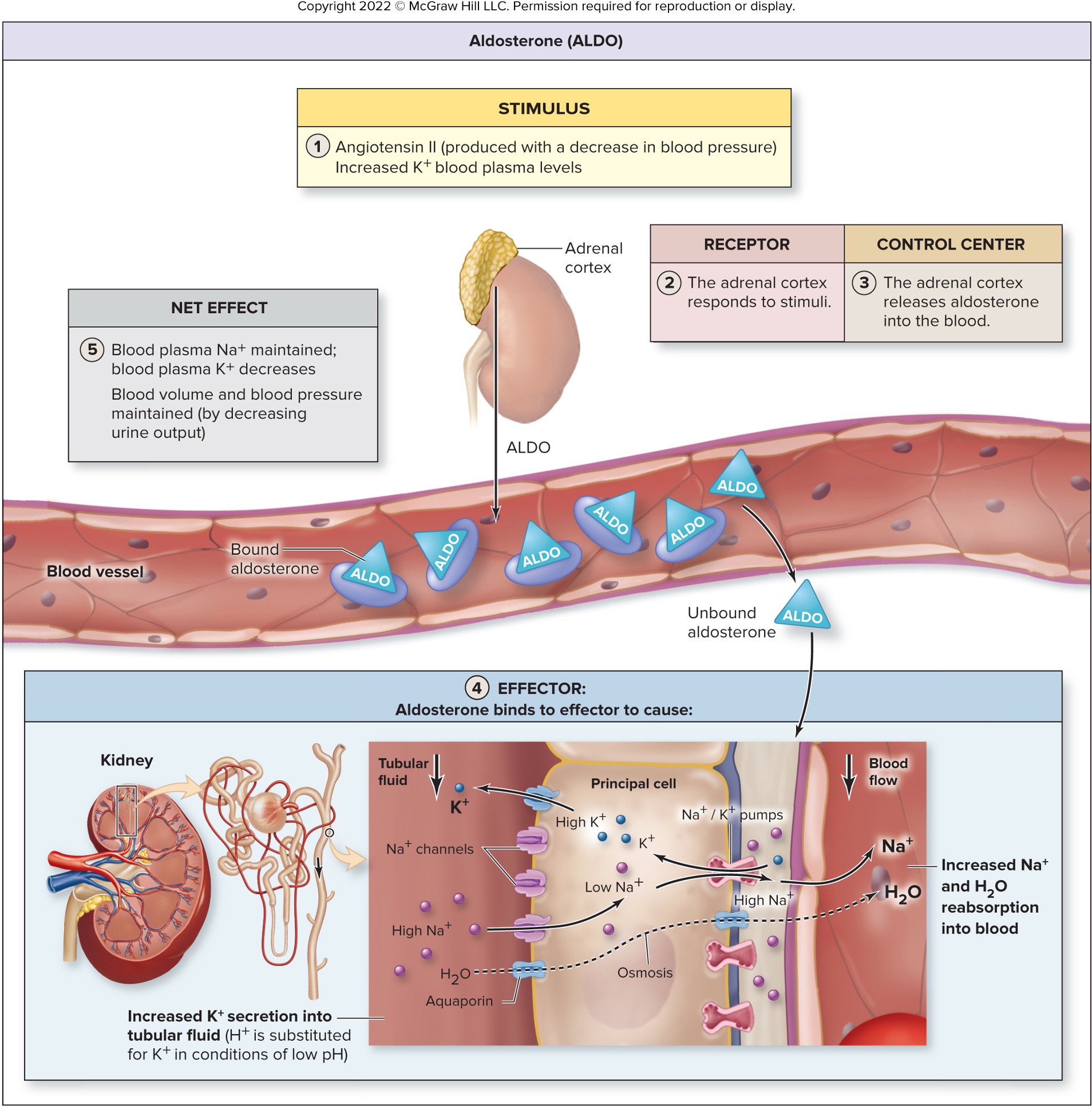
what are the changes initiated by aldosterone?
increased reabsorption of Na+ and water
increased secretion of K+
decreases urine output
maintains blood osmolarity
what is atrial natriuretic peptide (ANP) and what does it respond to?
peptide hormone
released from the heart atria
response to stretch of the heart (increased blood volume and pressure to the heart)
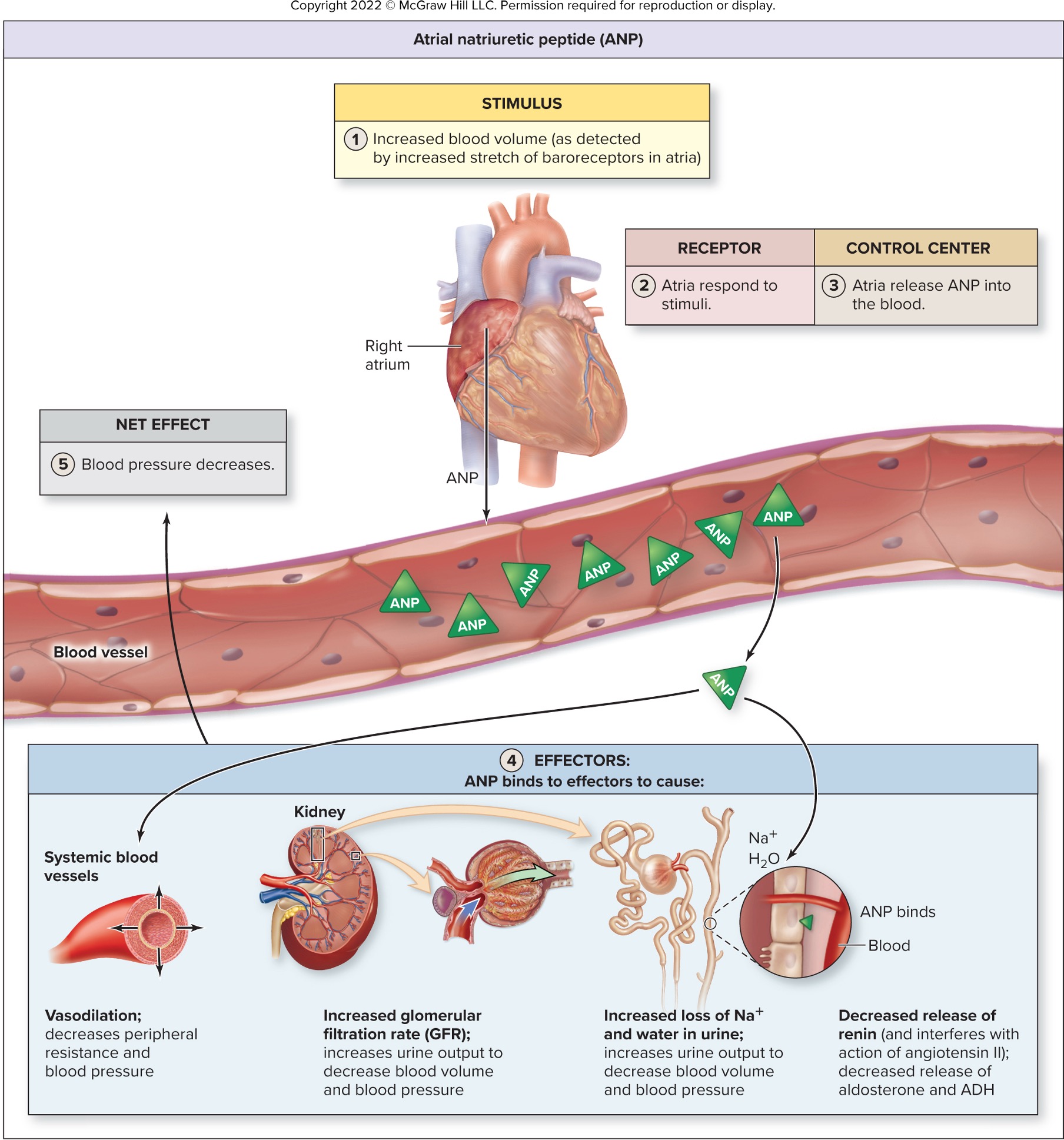
what are the changes initiated by atrial natriuretic peptide (ANP)?
decreases blood volume and pressure by binding to target organs
dilate systemic vessels (cause dilation of afferent arterioles in the kidneys) → relaxes mesangial cells → increase GFR and urine output
inhibits Na+ and water reabsorption by nephron tubules
increases urine output, decreasing blood volume and blood pressure
inhibit the release of renin, ADHD, and action of aldosterone