Ch 2: Liver
1/113
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
114 Terms
Is the liver intraperitoneal or retroperitoneal?
Mostly intraperitoneal, except for the bare area (which is retroperitoneal).
What is the normal size of the liver (craniocaudal at mid-clavicular line)?
Approximately 13–15 cm (varies slightly by source). >15.5 cm = suspicious for hepatomegaly
What is the normal sonographic appearance of the liver parenchyma?
Homogeneous, medium-level echogenicity; slightly hyperechoic or isoechoic to the renal cortex. Slightly hypoechoic or isoechoic to the spleen. Hypoechoic to the pancreas.
What is the name of the fibrous capsule that surrounds the liver?
Glisson’s capsule.
What structures separate the right and left lobes of the liver?
The main hepatic vein (MHV) within the main lobar fissure, and functionally also the gallbladder fossa.
What divides the right lobe into anterior and posterior segments?
The right hepatic vein (RHV).
What divides the left lobe into medial and lateral segments?
The left hepatic vein (LHV); also functionally the falciform ligament and ligamentum teres.
What is another name for the medial segment of the left lobe?
The quadrate lobe.
What is unique about the caudate lobe’s blood supply?
It has a separate/independent blood supply.
What structure bounds the caudate lobe anteriorly and posteriorly?
Anterior: ligamentum venosum
Posterior: IVC
Compare portal veins vs hepatic veins in direction of flow and waveform.
Portal veins = hepatopetal, monophasic.
Hepatic veins = hepatofugal, triphasic.
Compare portal veins vs hepatic veins in segmental anatomy and size changes toward the diaphragm.
Portal veins = intrasegmental, decrease toward diaphragm.
Hepatic veins = intersegmental/interlobar, increase toward diaphragm.
What is the sonographic appearance of portal vein walls?
Hyperechoic walls.
What is the liver’s dual blood supply percentage (PV vs HA)?
Portal vein ~75%, hepatic artery ~25%.
What is the normal MPV diameter, and what does enlargement suggest?
<13 mm; enlargement → portal hypertension.
How do the portal veins branch within the liver?
Main portal → right & left.
Right portal → anterior & posterior.
Left portal → medial & lateral.
Hepatic vein occlusion or narrowing is associated with what condition?
Budd–Chiari syndrome.
What is the Doppler characteristic of the hepatic artery?
Low-resistance flow.
What structures form the “Mickey Mouse sign”?
Portal vein, hepatic artery, common bile duct.
What is the fetal origin and adult remnant of the left umbilical vein, and what clinical finding may occur here in portal hypertension?
The left umbilical vein connects to the left portal vein (LPV) in utero. After birth it becomes the ligamentum teres.
In portal hypertension, recanalization of the paraumbilical vein may occur in this liagment.
What is the fetal origin and adult remnant of the ductus venosus, and where is its remnant located sonographically?
The ductus venosus (right umbilical vein) shunts blood from the umbilical vein directly to the IVC. Postnatally it becomes the ligamentum venosum, which lies anterior to the caudate lobe.
What landmarks help identify the main lobar fissure on ultrasound?
It lies between the right portal vein (RPV) and the gallbladder.
What is Riedel’s lobe, and why does it matter clinically?
An anatomical variant of the liver which is a inferior tongue-like extension of the right lobe that can mimic hepatomegaly. More often seen in women
What is the difference between unconjugated and conjugated bilirubin?
Unconjugated (indirect): Not water-soluble, before liver processing.
Conjugated (direct): Water-soluble, liver-processed, excreted into bile.
What is the cause and key lab pattern of prehepatic jaundice?
Excess RBC breakdown → ↑ unconjugated bilirubin (ex: sickle cell disease: too much RBC breakdown, liver is overloaded and cannot process all of the unconjugated bilirubin)
What is the cause and typical lab pattern of hepatic jaundice?
Liver dysfunction (e.g., hepatitis, cirrhosis) → ↑ either conjugated or unconjugated bilirubin (liver either can’t process or secrete)
What is the cause and key lab pattern of posthepatic jaundice?
Biliary obstruction (e.g., stones, mass, stricture) → ↑ conjugated bilirubin.
Which bilirubin type rises with obstruction (gallstones or pancreatic head mass) and why?
Conjugated bilirubin — leaks into the bloodstream when bile flow is blocked.
Which bilirubin type rises with excessive hemolysis and why?
Unconjugated bilirubin — excessive RBC breakdown overwhelms the liver and builds up in the bloodstream.
Which liver enzymes are most associated with cholestasis/obstruction?
ALP and GGT (disproportionately elevated compared to AST/ALT).
Which lab pattern suggests hepatocellular injury rather than obstruction?
Marked ↑ AST + ALT, with only mild–moderate ↑ ALP/GGT.
What is the most common liver disorder?
Hepatic steatosis
What is hepatic steatosis?
Fat accumulation within hepatocytes
What are the most common causes of hepatic steatosis?
Obesity, diabetes, metabolic syndromes, alcohol, and certain medications.
What is the classic sonographic hallmark of hepatic steatosis?
Increased echogenicity with decreased penetration and poor visualization of vessels/diaphragm.
What is “focal fatty sparing”?
Areas of normal liver within a fatty liver that appear hypoechoic, typically in the GB fossa, porta hepatis, and adjacent to the left portal vein.
What is “focal fatty infiltration”?
Localized regions of increased echogenicity fatty liver within a diffusely normal liver, often segmental or wedge-shaped.
How can focal fatty infiltration be differentiated from a mass?
Fatty sparing/focal infiltration preserves vascular architecture and shows no mass effect.
What condition can severe hepatic steatosis progress into?
NASH (nonalcoholic steatohepatitis) → fibrosis → cirrhosis.

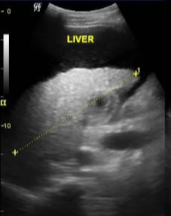
Diffuse fatty liver (increased echogenicity and attenuation, poor visualization of diaphragm and vasculature)

The hyperechoic area represents?
Focal fatty infiltration (differentiation from hyperechoic mass=no distortion of hepatic vasculature)

The hypoechoic area represents?
Focal fatty sparing (differentiation from hypoechoic mass=no distortion of hepatic vasculature)
What is hepatitis, and what major complications can it progress to?
Inflammation of the liver that can progress to cirrhosis, portal hypertension, and hepatocellular carcinoma (HCC).
How long must inflammation persist to be considered acute vs chronic hepatitis?
Acute: resolves within <4 months.
Chronic: persists >6 months.
How are the major viral hepatitis types transmitted (A, B, C)?
A: fecal–oral (contaminated food/water).
B: body fluids (blood, unsafe sex, perinatal mom to baby).
C: blood exposure — needlesticks, tattoos/piercings, high-risk sex; major risk for healthcare workers.
What non-viral conditions can cause chronic hepatitis?
Wilson disease (↑ copper), hemochromatosis (↑ iron), autoimmune disorders, and drug-induced hepatitis.
What are key clinical findings in hepatitis?
Fatigue, fever, nausea/vomiting, dark urine, jaundice (hepatic), elevated LFTs, chills, hepatosplenomegaly.
What is the sonographic appearance of early vs later hepatitis?
Early: liver may appear normal.
Later: hepatosplenomegaly, hypoechoic liver, portal triad echogenicity (periportal cuffing) = “starry sky” sign; possible GB wall thickening.
What is the “starry sky” sign, and what does it represent?
Hypoechoic liver with bright periportal triads, representing periportal cuffing in acute hepatitis.
Compare and contrast Wilson disease and hemochromatosis.
Wilson disease: Excessive copper accumulation
Hemochromatosis: Excessive iron accumulation
Both are inherited disorders that can lead to chronic hepatitis, cirrhosis, and HCC risk.
What is cirrhosis, and what structural changes define it?
A chronic liver disorder marked by hepatocyte death, fibrosis, necrosis, and regenerating nodules.
What are the major complications (sequelae) of cirrhosis?
Portal hypertension, varices, portal vein thrombosis, HCC, and hepatorenal syndrome.
What is the most common cause of cirrhosis, and what is the classic disease progression pathway?
Alcoholism.
Pathway: Fatty liver → steatohepatitis → cirrhosis → portal HTN → PVT → HCC.
What conditions (besides alcohol) can lead to cirrhosis?
Hepatitis, cholangitis, Wilson disease, hemochromatosis, and primary biliary cirrhosis.
What lab abnormalities are typical in cirrhosis?
Elevated AST, ALT, LDH, and bilirubin.
What is the hallmark clinical picture of cirrhosis?
Jaundice, ascites, fatigue, hepatosplenomegaly, varices, and signs of portal HTN.
What are the hallmark sonographic findings of cirrhosis?
Early: hepatomegaly.
Later: shrunken echogenic right lobe, enlarged caudate/left lobes, nodular surface, coarse texture, splenomegaly, ascites.
Doppler: monophasic hepatic veins, hepatofugal portal flow.
When cirrhosis is suspected, what must always be assessed?
Portal hypertension, portal vein thrombosis, and HCC.
What is hepatic encephalopathy?
confusion from buildup of toxins
Define caput medusae.
engorged abdominal veins from portal HTN
Cirrhotic liver with nodular changes
What does liver elastography evaluate, and what does increased stiffness indicate?
Elastography measures the stiffness of liver tissue; increased stiffness corresponds to more liver fibrosis.
What is portal hypertension, and what is the most common cause?
Elevated pressure in the portal venous system; most commonly caused by cirrhosis.
Besides cirrhosis, what other conditions can cause portal hypertension?
Portal vein thrombosis, hepatic vein thrombosis, IVC thrombosis, or tumor compression of the liver or adjacent organs.
Explain the hemodynamic changes in portal hypertension related to cirrhosis.
Fibrosis increases intrahepatic resistance, making the liver difficult to perfuse → portal pressure rises, hepatic artery enlarges, and portal vein flow may reverse (hepatofugal).
Why do portosystemic collaterals and varices develop in portal hypertension?
The body reroutes blood away from the high-resistance liver through collateral pathways to reduce portal pressure.
What is the most common sonographically identifiable collateral in portal hypertension, and what syndrome does it represent?
Recanalization of the paraumbilical vein (left umbilical vein in the ligamentum teres), shunting blood to epigastric veins — Cruveilhier-Baumgarten syndrome.
What is the difference between portal vein compression and portal vein thrombosis?
Compression: External narrowing, most often from adjacent tumors or lymphadenopathy.
Thrombosis: Intraluminal clot within the portal vein
What conditions are commonly associated with portal vein thrombosis (PVT)?
HCC, portal hypertension, pancreatitis, cholecystitis, pregnancy, oral contraceptive use, and post-surgical states.
What is cavernous transformation of the portal vein, and what does it look like sonographically?
A chronic sequela of portal vein thrombosis characterized by multiple serpiginous/tortuous collateral vessels in the porta hepatis.
What are common clinical findings of portal vein thrombosis?
Abdominal pain, elevated LFTs, leukocytosis, low-grade fever, nausea/vomiting, and hypovolemia.
What is portal venous gas, and why is it clinically important?
Gas within the portal or mesenteric veins, most classically from ischemic bowel disease (often fatal), though it can also be seen with inflammatory, obstructive, malignant, or iatrogenic bowel conditions.
What is the sonographic appearance of portal venous gas?
Small, bright echogenic reflectors moving within the portal vein blood flow.
What is Budd–Chiari syndrome, and what are its key clinical findings?
Occlusion of the hepatic veins (± IVC).
Clinical findings: ascites, elevated LFTs, hepatomegaly, splenomegaly, upper abdominal pain.
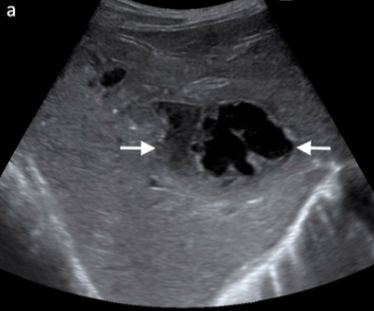
What are the hallmark sonographic findings of Budd–Chiari syndrome?
Absent or reduced visualization of hepatic veins, thrombus in hepatic veins, absent flow on color Doppler, enlarged caudate lobe, and possible IVC narrowing.
What is hepatorenal syndrome, and how does it appear clinically and sonographically?
Renal failure secondary to chronic liver disease.
Clinical: history of cirrhosis, ↓ GFR, ↑ creatinine, ↓ urine output.
Sonographic: cirrhotic liver findings; kidneys may appear normal.

What is the vascular disease in this liver?
Budd-chiari syndrome
What are true hepatic cysts, and when are they typically encountered?
Benign, fluid-filled cysts, often solitary and idiopathic, usually discovered in middle age.
With what systemic disease are multiple hepatic cysts commonly associated?
Autosomal dominant polycystic kidney disease (ADPKD).
What are the typical clinical findings of hepatic cysts?
Usually asymptomatic with normal LFTs; large or hemorrhagic cysts may cause RUQ pain
What are the classic sonographic features of hepatic cysts?
Anechoic, well-defined lesions with posterior acoustic enhancement; may be multiple or clustered in ADPKD.
What causes a hydatid (echinococcal) liver cyst and how is it transmitted?
Caused by Echinococcus granulosus (tapeworm); humans ingest food contaminated with dog feces, parasite travels via portal vein to liver; common in sheep/cattle-raising regions.
What are the classic sonographic findings of a hydatid liver cyst?
Anechoic cyst with internal debris, daughter cysts within a mother cyst, and the water lily sign (floating endocyst within the pericyst).

Benign liver lesion
Hydatid liver cyst (water lily sign)

Benign liver lesion
Hydatid liver cyst (daughter cysts within mother cyst)
What causes an amebic liver abscess and what clinical clue is most important?
Entamoeba histolytica, transmitted via contaminated water; key clue is recent travel and dysentery (bloody diarrhea).
What are the sonographic features of an amebic abscess and how is it confirmed?
Round hypoechoic/anechoic lesion with debris, often right lobe near capsule; indistinguishable from pyogenic abscess → requires serology.
What is schistosomiasis and why is it globally important?
A flatworm (schistosoma) infection transmitted through snail-contaminated freshwater; one of the most common causes of hepatic fibrosis worldwide.
What are the characteristic sonographic findings of schistosomiasis?
Periportal thickening, possible bulls-eye lesions; chronic disease shows turtleback sign (calcified septa/fibrosis).
What is the most common source of a pyogenic liver abscess?
Spread from intra-abdominal infection (appendicitis, diverticulitis, cholecystitis, cholangitis) via portal vein, biliary tree, or HA.
What are the sonographic findings of a pyogenic liver abscess?
Complex cystic mass with thick walls, debris, septations, and possibly gas.
Who is at highest risk for hepatic candidiasis and how does it spread?
Immunocompromised patients (cancer, transplant, HIV); spreads via the bloodstream.
What is the classic sonographic appearance of hepatic candidiasis?
Multiple tiny (<1 cm) target/halo/bulls-eye lesions with hyperechoic centers and hypoechoic rims; may calcify over time.
How can you differentiate the major infectious liver lesions based on transmission, key clinical clues, and sonographic appearance?
Hydatid (Echinococcal) Cyst
Source: Dog feces → sheep/cattle → humans (portal vein spread)
Clue: Travel to sheep-raising regions
US: Daughter cysts, water lily sign, anechoic cyst with debris
Amebic Abscess (Entamoeba histolytica)
Source: Contaminated water (portal vein spread)
Clue: Travel + dysentery (bloody diarrhea)
US: Round hypoechoic/anechoic lesion with debris, often right lobe near capsule; indistinguishable from pyogenic
Schistosomiasis
Source: Snail-contaminated freshwater (skin penetration)
Clue: Africa/Asia + fibrosis
US: Periportal thickening, bulls-eye lesions, chronic turtleback sign
Pyogenic Abscess
Source: Appendicitis, diverticulitis, biliary infection, surgery
Clue: Fever + leukocytosis + abdominal infection history
US: Complex cyst, thick walls, septations, possible gas
Hepatic Candidiasis
Source: Bloodstream fungal spread
Clue: Immunocompromised patient
US: Multiple tiny (<1 cm) target/halo lesions, may calcify

Benign liver lesion
Liver abscess
Benign liver lesion
Liver abscess

Fungal disease, typically in immunocompromised patients
Hepatic candidiasis
What is the most common benign liver tumor, and who is it most commonly found in?
Cavernous hemangioma; more commonly discovered in women.
How do hepatic hemangiomas typically present clinically?
Incidental and asymptomatic.
What is the most common location and classic size/appearance of a hepatic hemangioma?
Right lobe; typically a small (<3 cm), well-defined hyperechoic mass (larger ones are giant hemangiomas).