Module 16: Psychotic Disorders and SZ (1)
1/56
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
57 Terms
Psychosis
A collection of symptoms that can form part of a disease
It is an abnormality of the mind and can involve:
Delusions e.g. thoughts of persecution
Hallucinations – seeing/hearing/feeling/smelling things that aren’t there
Disordered thoughts
Catatonia
Active Psychosis
A highly disabling condition
It is more disabling than blindness and paraplegia, but less so than dementia and quadriplegia
Causes of Psychosis
It can occur as part of various conditions and external factors:
Mental health conditions:
Affective disorders (e.g., Bipolar Disorder, Major Depressive Disorder) – with psychotic specifiers
Anxiety disorders – e.g., PTSD
Alzheimer’s Disease and other neurodegenerative conditions
Non-illness-related causes:
Illegal drugs (e.g., stimulants, hallucinogens)
Prescription medications
Sleep deprivation
Caffeine intoxication
First Episode Psychosis
Often occurs unexpectedly and can't be immediately linked to a specific mental health condition.
A person may be diagnosed with Brief Psychotic Disorder, which is:
A period of psychosis not caused by conditions like schizophrenia, BPD, or MDD.
A more definitive diagnosis typically comes later, once the condition develops further.
Prodromal Phase
The period before acute psychosis, marked by behavioural changes such as:
Irritability, difficulty concentrating, memory issues
Anxiety and depression
This phase can last months or years and is often hard to recognise, especially if symptoms mimic other mental health disorders (e.g., depression).
Importance of Early Intervention For Psychosis
Delays in treatment are common because:
The person may not realize they are ill
Friends/family might not understand what's happening
Delayed treatment is linked to worse outcomes
If psychosis is part of an ongoing/ underlying condition (e.g., schizophrenia), future episodes are likely
Recognising prodromal symptoms can help intervene earlier in future episodes
Diagnosis of Schizophrenia
Uses the DSM-5 criteria
Two or more of the following symptoms must be present for at least 1 month, and one must be a positive symptom (1–3 below):
Hallucinations
Delusions
Disorganized speech
Disorganized or catatonic behavior
Negative symptoms
There must be significant impairment in functioning.
Continuous signs of disturbance in behaviour must be present for 6+ months.
Symptoms must not be better explained by another condition.
ICD-10 diagnostic criteria are similar to DSM-5.
Positive Symptoms of Schizophrenia
Symptoms are behaviours or experiences added/ in addition to normal functioning.
Heavily emphasised in DSM-5.
Include:
Hallucinations (e.g., hearing voices)
Delusions (false beliefs)
Disorganised speech
Disorganised or catatonic behaviour
These are not present in healthy individuals, hence considered “positive.”
Negative Symptoms of SZ
Symptoms are behaviours or responses that a person with SZ has that normal individuals doesn’t have → represents deficits in normal emotional or behavioural functions:
Flat affect (loss of emotional expression)
Anhedonia (inability to feel pleasure)
Apathy (lack of motivation or interest)
Cognitive Symptoms of SZ
Include:
Difficulty processing information
Impaired attention or memory
Schizoaffective Disorder
A hybrid of SZ with a mood disorder (BPD and MDD)
Meets criteria for schizophrenia AND there is also a major mood episode (mania or depression)
manic and depressive episodes: SZA with bipolar type
depressive only: depressive type
mixed (manic and depressed simultaneously)
Name Some Features of Schizoaffective Disorder (Katie 35 y/o Female Case Study)
Suffered psychotic symptoms for 8 years previously. Usually very well controlled.
Relapsed and began experiencing hallucinations
Voices: constant commentary on actions, life choices
Tactile hallucinations
Visual hallucinations
Delusions that food was being poisoned -> anorexia
Delusions that husband was conspiring with family
Delusions that people were trying to harm her son
These symptoms are characteristic of SZ
Mania: high level of activity directed at delusions
Social withdrawal culminating in virtual catatonia
Sectioned 4 times in 3-year period.
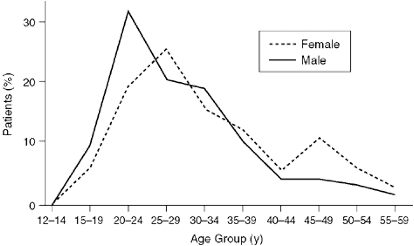
Epidemiology of Schizophrenia
Common - Around 1% of the population
Males 1.4x female – more common in males
Strikes at an early age
Males: late teens
Females: late twenties; second peak at menopause
Highly disabling – causes major disability with no cure
Myths Vs Facts of SZ
Myth: People with schizophrenia have split personalities.
➤ Fact: This confuses SZ with dissociative identity disorder. "Schizo" refers to a split from reality, not identity.Myth: People with schizophrenia are dangerous.
➤ Fact: Most are not dangerous to others. A small minority may show violence, but they’re more likely to harm themselves (e.g., high suicide risk).Myth: People with schizophrenia will never recover.
➤ Fact: Many experience partial or full recovery and can lead productive lives with appropriate treatment.
Additional Clinical Features of SZ
Psychiatrists may look for associated symptoms:
Sleep disturbances
Anxiety
Cognitive difficulties
These don't form part of the core diagnostic criteria but may support the diagnosis.
Neurological soft signs may also be present:
Motor abnormalities
Difficulty distinguishing right from left
Other subtle neurological deficits
Schizophrenia and Suicide
Higher rate of suicide with SZ rather than depression
Estimated that ~5% of those with SZ take their own lives – double the rate of those with depression
BPD type 1 has a higher rate of 10-15%
Patterns of Care: Bedlam (1700s and Earlier)
Inmates of the bedlam lunatic asylum were subject to terrible conditions with no effective treatment → were treated as entertainers for wealthy visitors
Patterns of Care: Joint Counties Asylum - Abergavenny (1850)
Legislations resulted in the building of public lunatic asylums, inspected by government conditions still brutal and more like a prison then a hospital
Beginning of a more humanitarian approach – led by the Quaker Tuke Family
Patterns of Care: Norther Michigan Asylum (Late 19th, Early 20th Century)
Improvement in conditions, with psychiatry recognised as a medical speciality
Treatments confined to psychical approaches e.g. surgery, ECT, fever therapy and insulin shock
Hospital ward: communal wards where SZ were often housed alongside elderly patients with senile dementia – violence between patients was common, with staff having to use physical restraints used
Communal wards are still present, but conditions are much better
Inpatient explosion decline – peak in mental hospital numbers occurred in the US with 6 in 1000 adults being inmates in an institution
Decline in numbers in 1955 following the introduction of the first antipsychotic, Thorazine
Patterns of Care: Norther Michigan Asylum: 1970s onwards
Many older psychiatric hospitals like Barrow Hospital were closed
Emphasis moved from institutional care to care in the community
Unity centre provided ‘hall of residence’ style facilities rather than traditional psych hospitals
Today few people are residents in psychiatric hospitals
Some people do need residential care to either protect them from themselves or to protect society
Mental Health Act legislation allows people to be detained in psychiatric hospitals against their will
Mental Health Act 1983
"Sectioning" refers to legal detention of an individual under this act
Allows compulsory hospitalisation and treatment for individuals with serious mental health conditions.
Used only if the person is a danger to themselves or others.
Includes safeguards and legal checks to prevent its misuse and abuse
Powers granted to medical professionals, social workers, and police.
Section 2 and Section 3 of the Mental Health Act 1983
Section 2: 28-day assessment and treatment order.
Section 3: 6-month treatment order (can be renewed).
Typically used for ongoing mental illness where a diagnosis already exists.
Sectioning
Application to ‘detain an individual’ is made by a near relative or “approved mental health professional”
The patient must be seen by two doctors (one must be a psychiatrist) and an Approved Mental Health Professional
Cannot refuse treatment (except ECT)
Used in SZ, MDD, and BPD where an individual is a danger to themselves or others
Risk Factors for Schizophrenia
Its origin is unknown but both genetics and environmental and social factors can increase an individual risk
Environmental and social factors can cause epigenetic changes → early child hood trauma can causes changes in the HPA axis which can increase the risk of mood disorders in later life
Schizophrenia: Genetic Risk Factors
Rate of 1% in the general population
The rate increases to 8-10% if near relative affected
A concordance rate of 50% in twin studies
unlikely a single gene, probably many “tendency” genes that have a small impact individually but collectively more profound
e.g. DISC1
tendency genes may require environmental impact too
Schizophrenia: Environmental Risk Factors
Winter birth (controversial risk factor – myth?)
May be maternal exposure to viruses
Substance abuse may be involved
amphetamine -> psychosis and worsen psychosis in SZ/ cause relapse
cannabis? increases risk
BUT schizophrenics have a high risk for substance abuse (cause or effect?)
AKT1
A gene that codes for a kinase that inactivates glycogen synthase kinase (GSK).
GSK is implicated in BPD and is a target of lithium treatment.
GSK also plays a role in dopamine (D2) receptor signaling, linking it to SZ (schizophrenia).
This suggests AKT1 impacts dopamine-related pathways, relevant to both BPD and SZ.
How does AKT1 genotype influence schizophrenia (SZ) risk with cannabis use
A study used odds ratios to assess SZ risk in different AKT1 genotypes:
T/T (Homozygous wild-type): No increased SZ risk, regardless of cannabis use.
C/T (Heterozygous): Also no change in SZ risk.
C/C (Homozygous mutant): Heavy cannabis users had a 7-fold increased risk of SZ.
Shows genetic risk (AKT1) interacts with environmental factors (cannabis) in SZ development.
Schizophrenia: Social Risk Factors:
Difficult childhood conditions can increase risk
discrimination
dysfunctional families
abuse/trauma
Epigenetic changes? – likely affects different genes to those in BPD or MDD
Schizophrenia As A Neurodevelopmental Disorder
Question as to whether SZ is a neurodevelopmental or neurodegenerative disorder
Age of onset (teenage/early adult) – favours neurodevelopmental hypothesis – a time when the brain undergoes a series of changes
Structural differences in the brain for those with/w/o SZ
Or: a neurodegenerative disorder?
Progression of disease in many cases, if not treated early
Reductions in brain volume → the role of Excitotoxicity?
The potential influence of glutamate
Schizophrenia: Other Risk Factors
Infection with T. gondii is a potential risk factor for SZ and BPD.
The parasite uses cats as definitive hosts and any warm-blooded animal (including humans) as secondary hosts.
Around 30% of the global population is estimated to be infected.
It forms cysts in tissues, including the brain, where it can persist for life.
In rodents, it alters behaviour to make them more likely to be eaten by cats.
It's suggested that T. gondii may also influence human behaviour, potentially contributing to psychiatric disorders.
Schizophrenia: Dopamine Hypothesis
It suggests hyperactivity of the mesolimbic pathway (from VTA to ventral striatum) may contribute to schizophrenia.
Not the root cause, but a final common pathway where multiple factors converge to produce positive symptoms(hallucinations, delusions).
Evidence supporting the hypothesis:
Reserpine (hypertensive drug) depletes dopamine, and when given to SZ patients, it reduces positive symptoms.
Amphetamines, which release dopamine, can induce psychosis, which can be treated by SZ medications.
L-DOPA and dopamine agonists (Parkinson's treatments) can cause psychosis at high doses.
Altered dopaminergic activity (hyperactivity) in certain brain areas may play a role in SZ.
Dopamine Receptors
5 subtypes that can be divided into 2 groups
D1-Like
D2-Like → implicated in SZ
Why Are D2 Receptors the Prime Target for Antipsychotics
Studies have shown that there is a 1:1 ratio between the therapeutic concentration of antipsychotics (neuroleptics) and the concentration required to occupy 75% of DA D2 receptors.
This suggests that activity at D2 receptors is crucial for the anti-psychotic activity of these drugs.
4 Dopaminergic Pathways
Mesocortical pathway from the VTA to the cortex
Involved in emotion, fear, motivation.
Nigrostriatal pathway: substantia nigra to the basal ganglia and into the striatum
Emotion, motivation, cognitive control
Tuberoinfundibular pathway: hypothalamus to the pituitary gland
hormone release from pituitary
Mesolimbic pathway: VTA to the ventral striatum/ nucleus accumbens
motor control
Dopamine Pathways in SZ (Traditional View)
Mesolimbic pathway (VTA → Ventral Striatum): Increased DA transmission here is thought to explain positive symptoms (e.g., hallucinations, delusions) in schizophrenia.
Mesocortical pathway: Decreased DA transmission here is thought to explain negative symptoms (e.g., anhedonia, apathy) and cognitive problems.
Tuberhypophyseal pathway: Involved in hormone release from the pituitary, contributing to side effects.
Nigrostriatal pathway: Regulates motor control, and dysfunction here contributes to Parkinson's disease and motor side effects of antipsychotic medications.
Motor Pathway in Parkinsons (PD)
Pathway involves a loop:
Cortex → Striatum → Globus Pallidus → Thalamus → Cortex.
The substantia nigra provides input to the striatum, which modulates this pathway.
This pathway's dysfunction leads to motor symptoms in Parkinson's disease, such as tremors and rigidity.
Cortical Loop of the Reward Pathway
The loop involved in emotion and motivation (reward pathway) connects:
Cortex → Central Striatum (NA, GP) → Thalamus → Cortex.
The mesolimbic pathway (from the VTA to the ventral striatum) modulates this loop, influencing emotional responses.
The early dopamine hypothesis suggested that increased DA transmission in the mesolimbic pathway contributes to positive symptoms of schizophrenia (e.g., hallucinations, delusions).
Associative Pathway
Pathway connects:
Cortex → Striatum → GP → Thalamus → Cortex.
It is involved in habituation, learning, memory, attention, motivation, emotion, and volition.
The SN-striatal pathway (input from the substantia nigra to the striatum) plays a critical role in high-level cognitive processes.
Dopaminergic Pathways in Schizophrenia (Modern View)
Functional imaging shows that increased DA in the mesolimbic pathway (VTA → VS) doesn't occur as previously thought.
Instead, excess DA activity appears in the nigrostriatal pathway entering the associative striatum, which is likely the explanation for positive symptoms in schizophrenia.
Dopamine Hypothesis (Version 3)
Associative Striatum (AS): Responsible for assigning salience (importance) to stimuli, e.g., threat level.
Excess noise in AS dopaminergic signaling:
Leads to increased (inappropriate) salience assigned to unimportant stimuli, causing positive symptoms(hallucinations, delusions).
Cognitive impairments:
Hypodopaminergic cortical function possibly driven by excessive AS signaling and striatal hyperdopaminergic activity.
Negative symptoms:
Impaired reward-based learning due to excess noise in AS.
Inability to assign importance to rewarding stimuli leads to apathy and anhedonia.
May be driven by striatal hyperdopaminergic signaling.
NMDA Receptors and Glutamine in SZ
Glutamate dysfunction may be the root cause of SZ
NMDA antagonist e.g. ketamine cause psychosis
Positive allosteric modulators of Glutamate receptors may be a therapeutic drug
AMPAkines (positive allosteric modulates of AMPA receptors) may be a new therapeutic approach (but nothing on the market)
Serotonin Receptors in SZ
LSD causes psychosis
-ve symptoms of apathy, and avolition in SZ similar to depression (MDD)?
Probably not the root cause of SZ but 5HT receptor activity in neuro psychotics may give a better therapeutic profile
Muscarinic Receptors in SZ
Receptors play a role in cognitive and negative symptoms in SZ.
Receptor antagonists:
Worsen negative & cognitive symptoms (e.g., scopolamine, a non-selective mAChR antagonist, can cause psychosis).
Antipsychotics without mAChR activity: Lead to serious movement side effects (e.g., tardive dyskinesia).
Antipsychotics with mAChR antagonism: Help avoid movement-related side effects.
Potential therapeutic approach: Muscarinic agonists may be useful, but better side-effect profiles are given by mAChR antagonists.
Selective allosteric modulators: Subtype-selective modulators might be a viable treatment option (less conserved compared to orthosteric sites).
Challenges: Developing drugs targeting the orthosteric (ACh) site is difficult, as this site shows little variation between receptor subtypes.
Dirty Drug
A drug that has effects at its target site and at off-target effects
Antipsychotics as Dirty Drugs
They are normally D2 antagonists/ partial agonists, inhibiting D2 receptors
Actions at many different receptor types
Lack of selectivity gives rise to side effects
BUT! May also give rise to therapeutic benefit e.g. actions at 5HTR (improves therapeutic profile)
Target of Antipsychotics
Aim to target the excess DA in the associative striatum
Consider the mesolimbic pathway and the tuberoinfundibular pathway (& motor branch of the nigrostriatal pathway) → contain DA receptors which may be targeted by the antipsychotics
Have actions at other pathways in the brain
Common Side Effects of Antipsychotics: Extrapyradmial
Movement disorders
Includes:
Dystonia (muscle contraction) and tardive dyskinesia (jerking/ writhing movements) – can be permanent (continue after treatment terminated)
(Motor striatum D2 receptors interference)
Common Side Effects of Antipsychotics: Galactorrheea
Inappropriate milk production
Tuberhypophyseal D2 receptors inhibit prolactin release
Blockage of receptors = hyperprolactinemia = excess milk production
Common Side Effects of Antipsychotics: Cognitive Impairement
? D2 inhibition in cortex; effects at other receptors e.g. anti-muscarinic effects
May act to worsen the cognitive symptoms
Common Side Effects of Antipsychotics: Sedation
? H1 antagonism (like sedating antihistamines) – off-target effects
Common Side Effects of Antipsychotics: Weight Gain
? H1 and 5HTR antagonism
Can lead to diabetes, heart disease etc
Common Side Effects of Antipsychotics: Anti-Muscarinic Effects
Dry mouth
Blurred vision
Memory problems
Cardiac problems
Problems With Antipsychotics
Medication increases the risk of diabetes → hyperglycaemia is a known side effect of these drugs
2012 study found that 10% of people on antipsychotics had T2DM and 37% were pre-diabetic (at risk of development)
Rates here are higher than the general population and there are several explanations for this increased risk
Antipsychotics and Obesity
Many antipsychotics produce significant increases in BMI due to actions at H1 and 5HT receptors
Obesity is associated with T2DM, increased BMI is likely to be a large reason for the increased risk of diabetes for those on antipsychotics
Antipsychotic Induced Insulin Release
Antipsychotics can induce insulin resistance independent of their effects on BMI
This can occur with drugs that don’t produce marked changes in appetite
Antipsychotics are thought to cause insulin release by inhibiting a component of the insulin signalling cascade (Akt) and by decreasing the phosphorylation of one of its targets of the insulin receptor kinase activity, insulin receptor substrate 1 (IRS-1)
Direct Effect of Antipsychotics on Beta Cells
Cause pancreatic beta cell dysfunction in several ways
By acting on muscarinic dopamine, adrenergic and serotonergic receptors, they can decrease insulin secretion
They may decrease cellular [ATP], decreasing insulin secretions
May damage beta cells and induce apoptosis