Lecture 12-13 Vitamin D
1/40
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
41 Terms
What is absolutely crucial to ask when dealing with vitamin D toxicity?
What is the EXACT name/form and it the dosage in IU or units/mg?
Why must you know the exact name/form of vitamin D?
All have different half life, toxic doses, onsets of action
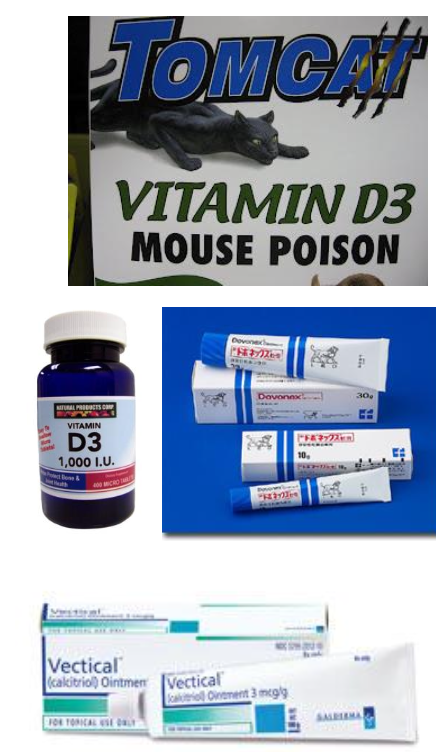
__ form is 1 of the 5 rodenticides on market.
Cholecalciferol, Vitamin D3
What are the top sources of vitamin D toxicity?
Vitamin or vitamin-mineral supplements
Cholecalciferol rodenticides
Human medications like calcitriol, donovex
Vitamin D toxicity is primarily a small or large animal issue?
small animal
What is a less common source of vitamin D toxicity for small animals?
feed math/mixing errors
Vitamin D toxicity in large animals happen how?
not common, might happen with plants with 1,25-dihydroxycholecalciferol or math/mixing errors in feed
Describe and give an example of a rodenticide product with cholecalciferol
d-CON post-2018 0.075% cholecalciferol residential
soft, highly palatable green

Vitamin D toxicity most commonly occurs in ___ via ___, ___, ___, ___, ___.
dogs (but can occur in any species)
medications, vitamin/vitamin-mineral supplements, rodenticides, mixing/math errors, plants
True or False? Secondary or relay vitamin D poisoning commonly occur.
False. RARE.
Is Vitamin D3 water or fat soluble? How does this affect toxicity?
Fat soluble so undergoes enterohepatic recirculation, stored in fat
What signalments are more sensitive to vitamin D?
cats, kittens, puppies MORE sensitive than adults
With cats, kittens and puppies, use ___ of adult toxic dose.
1/10
Describe the mechanism of action of cholecalciferol
cholecalciferol absorbed in SI if fat/bile acids present → liver converts to 25-hydroxycholecalciferol aka calcidiol/calcifediol via 25-hydroxylase → kidney converts to 1,25 dihydroxycholecalciferol aka calcitriol via 1-alpha hydroxylase
Rank the half-life and biological activities of cholecalciferol, 25-hydroxycholecalciferol, and 1,25 dihydroxycholecalciferol
cholecalciferol: low biological activity
25-hydroxycholecalciferol: higher biological activity and long half-life 15-29 days to 2-5 months
1,25 dihydroxycholecalciferol: highest biological activity, most potent, shortest half life
There is a ___ phase between ingestion and onset of clinical pathologic changes with cholecalciferol-vitamin D3-supplements and rodenticide and feed. The lag may be ___ to ___, dependent on ___. ___ and ____ mechanisms also contribute.
lag,
12-36-72 hour, 5 days, dose
metabolic activation, overcoming homeostatic mechanisms
Vitamin D medications (not cholecalciferol) may see onset ___ and is ___ dependent.
<3-6 hours, dose
All cholecalciferol and metabolites causes persistent ___ and ___. Eventually this causes ____ within 3-7 days. What are the 3 sources causing this problem?
hypercalcemia, hyperphosphatemia, soft tissue mineral deposition
enhances Ca and P absorption from GIT, increase osteoclastic activity in bone, increase Ca reabsorption by distal renal tubules
Why is there sometimes a time delay in presentation with vitamin D toxicity?
lag phase in clinical signs that are dependent on dose, form of vitamin D (metabolism), and overcoming homeostasis
Signs with cholecalciferol can occur within ___ , acute ___ as early as ____.
12-36 hours, renal failure, 24-48 hours
Initial signs of vitamin D toxicity?
Hypercalcemia causes anorexia (1st sign), GIT, neurological signs, lethargy, altered mentation, obtundation, muscle weakness, vomiting, diarrhea, polyuria
Progressive signs of vitamin D toxicity?
Metastatic mineralization causing cardiac, renal, lung signs. Most commonly acute kidney injury as early as 24-48 hours to 2-3-7 days
Ca x P > __ mg/dL think soft tissue mineralization
60-70
How else besides the Calcium Phosphorus Solubility index can you monitor soft tissue mineralization?
radiographs

Death is usually the result of what with vitamin D toxicity?
multiple organ failure (mostly renal, GIT, cardiac, respiratory, vascular)
What can you see BEFORE clinical signs appear with vitamin D toxicity?
elevated Ca and P
May see ionized hypercalcemia as early as ___ with cholecalciferol and earlier with others
12-72 hours
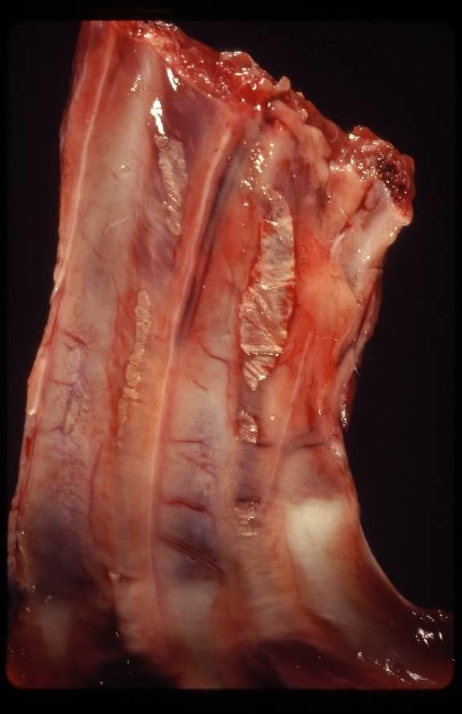
Describe the gross lesions from vitamin D toxicity
mineralization up to 2-3-7days post exposure in multiple tissues including atria, lung, arteries, kidney, GI mucosa
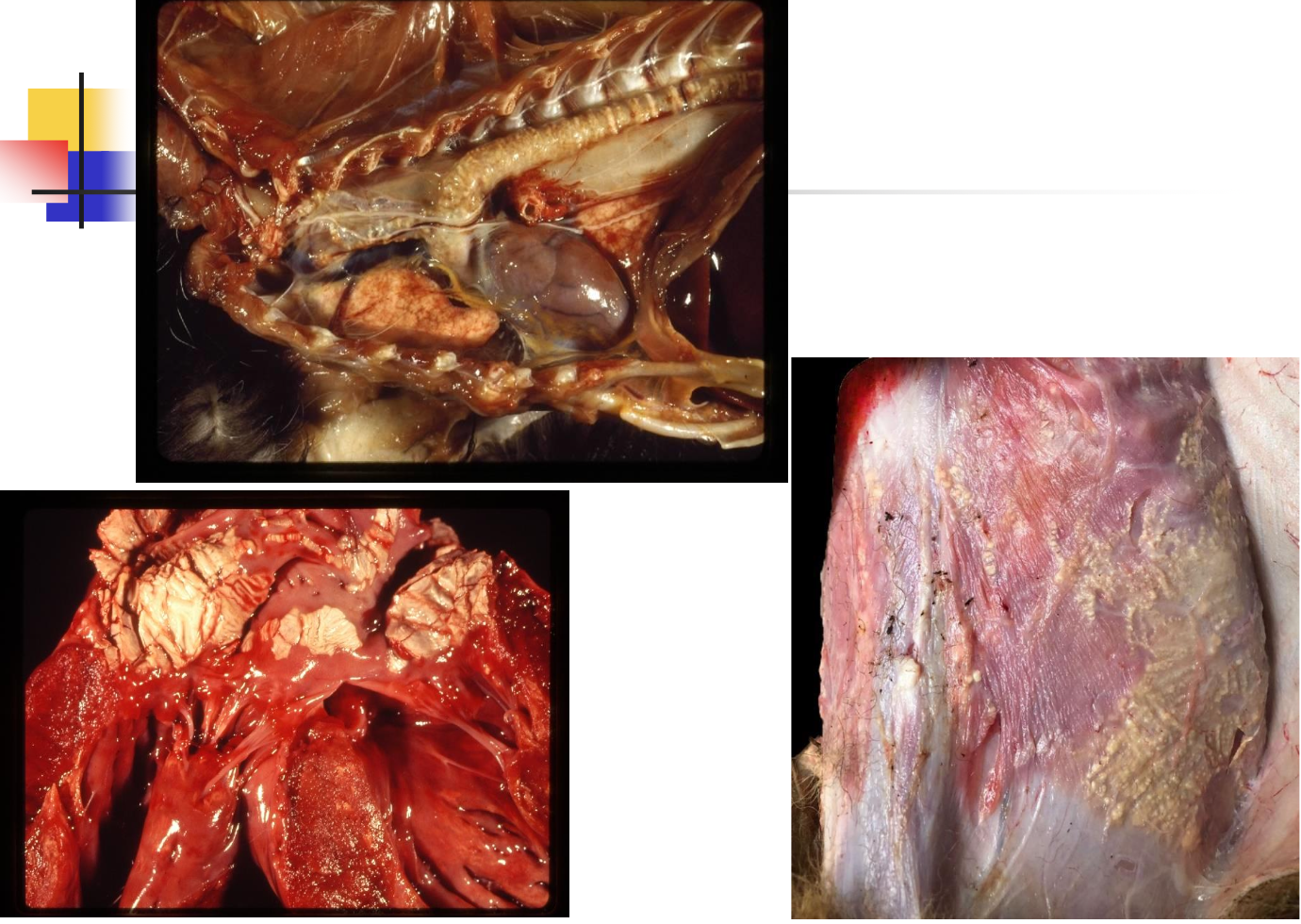
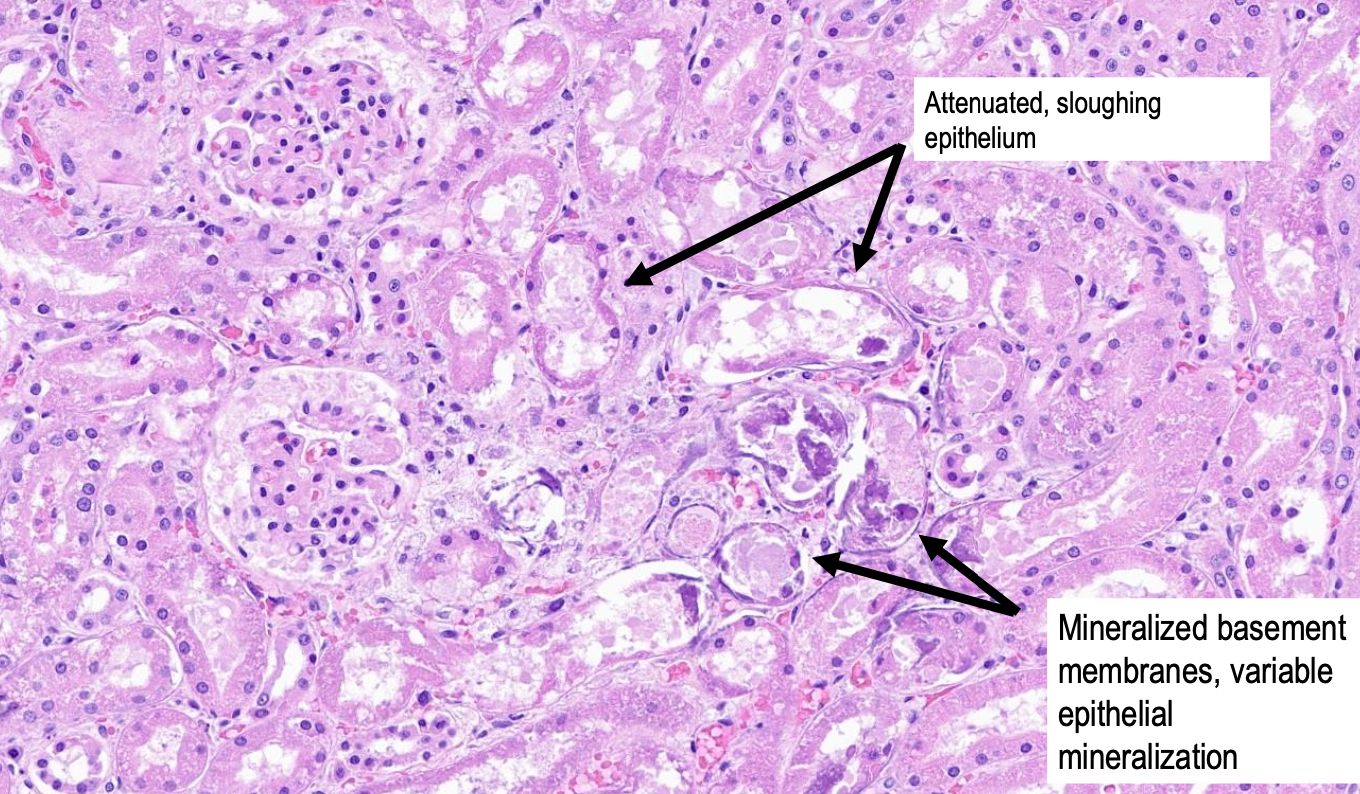
Describe the microscopic lesions from vitamin D toxicity
mineralization/degeneration and necrosis of renal tubular epithelium,
hypertrophy and hyperplasia of parafollicular cells of thyroid
Diagnosis of vitamin D toxicity is based on:
history with access to D products, clinical signs, hypercalcemia and/or hyperphosphatemia, r/o other differentials of hypercalcemia
What are the acronyms for hypercalcemia differentials?
GOSHDARNIT, HOGSINYARD
GOSHDARNIT describes ddx for hypercalcemia
Granulomatous
Osteolytic processes (not common)
Spurious
Humoral hypercalcemia of malignancy, primary Hyperparthyroidism, Hyperthyroidism
D vitamin D toxicity
Addison’s disease (hypoadrenocorticism)
Renal
Neoplaisa, Nutritional
Idiopathic (cats), Iatrogenic
Tumor
HOGSINYARD describes ddx for hypercalcemia
Hyperparthyroidism
Osteolysis (not common)
Granulomatous disease
Spurious
Iatrogenic, Idiopathic (cats)
Neoplasia
Youth
Addison’s, Acidemia
Renal
D Vitamin D toxicity
True or False? Chemical analysis to diagnose vitamin D toxicity is not commonly offered because it may not correlate with whether a P will become symptomatic and not likely to receive results quickly enough.
True.
True or False? An asymptomatic patient with vitamin D toxicosis is one that just does not have clinical signs.
False. An asymptomatic patient with vitamin D toxicosis has no clinical signs AND normal Ca and P.
Describe the treatment for asymptomatic vitamin D toxicosis
Decontaminate: consider emesis up to 3-6 hours, consider cholesytramine over AC or after first dose AC/sorbitol, TID with food x4d
Monitor labs: iCa, P, PCV/TP (hydration), BUN/Cr/USG (hydration and renal) SID-BID x4d
Monitor signs: anorexia and PU/PD
If dose very high, consider prednisone, prednisolone, fluid therapy
Describe the treatment goals for the symptomatic vitamin D toxicosis
GOAL is to lower Ca/P
Describe the treatment plan for the symptomatic vitamin D toxicosis regarding decontamination and treatments
Decontaminate: consider emesis up to 3-6 hours, consider cholesytramine after first dose AC/sorbitol, TID with food x4d
Biphosphonates: inhibit osteoclastic actvitiy, takes 2-4d, peak at 3d (targets bone, kidney)
Fluid therapy: physiologic saline, plasmalyte, norm-R 2-2.5x maintenance to promote calciuresis, Na and Ca compete
Prednisone/Prednisolone/Dexmethasone: if fluids, biphosphantes not working, promote calciuresis
Low Ca/P diet, GI protectants prn, Oral P binders
Furosemide questionable
What and how should you be monitoring in the symptomatic P with vitamin D toxicity?
at minimum SID until maintaining normal signs/parameters, monitor iCa, P and other parameters q3-6h prn
How long does the patient need to be monitored for if they were symptomatic with vitamin D toxicity?
until P maintaining normal signs and normal clinical pathology
may be days, weeks, months
What should you do when P is maintaining normal signs and normal clinical pathology?
wean meds off slowly, about 25% decrease every 3d to avoid rebound effect