sex differences pt 2
1/64
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
65 Terms
(gender
the socially constructed roles, behaviors, expressions, and identities that a society considers appropriate for men, women, and people of other gender identities.
(sex definition
the biological and physical characteristics typically used to classify humans as male or female at birth.
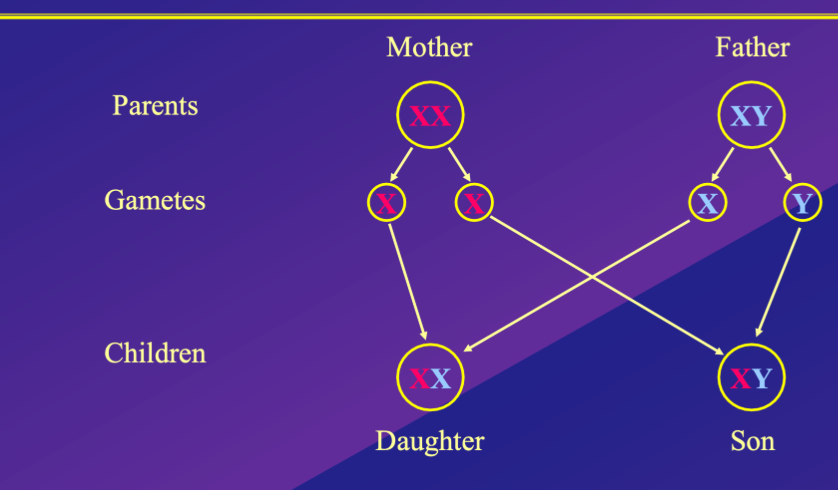
How is a sex determined in mammals : 1 chromosomes
1 – the production gametes (reproductive cells/ sex chromosomes) can be used to determine sex
Typically in mammals
In mammals sex is determined by the combination of sex chromosomes in the fertilised egg
Typically in mammals
Female – XX chromosomes which produce gametes (egg cells) that carry one haploid x chromosome
Male – XY chromosomes, produce gametes (sperm cells) that carry either an X or y haploid chromosome cell
During fertilisation haploid gametes combine to produce either one XX (female) or XY (male) zygote, determining sex
are cell types in mammals diploid or haploid?
Mammals have Haploid reproductive cells – each sex has one set of chromosomes, rather than 2 sets of matching chromosomes
(diploid
Diploid cells contain two complete sets of chromosomes, one set inherited from each parent.
In humans: Diploid cells have 46 chromosomes (23 pairs).
These are typical body cells (also called somatic cells) — like skin, muscle, and nerve cells.
(haploid
Haploid cells contain only one set of chromosomes, meaning they have half the number of chromosomes of diploid cells.
In humans: Haploid cells have 23 chromosomes.
These are gametes — sperm and egg cells.
(gamete
a reproductive cell of an animal or plant that carries half the genetic information of an individual — meaning it is a haploid cell (n)
Types:
Sperm cell (male gamete)
Egg cell or ovum (female gamete)
Chromosome number:
In humans: 23 chromosomes (haploid)
Gametes fuse during fertilization to form a zygote (a diploid cell with 46 chromosomes).
(Gonad
an organ in the reproductive system that produces gametes — the reproductive cells (sperm or eggs) — and also often produces sex hormones.
what determines the babys chromosomal sex?
A The presence or absence of Y chromosomes
B Number of X chromosomes
A - because of the Gene SRY
How is a sex determined in mammals : 2 the Gene SRY
it is the absence of the Y chromosome which determines sex: in the 1990’s discovered that
- The SRY gene is located on the Y-chromosome
- it is the Testis-Determining Factor: Is responsible for developing the sexually undifferenciated foetal gonad into a testis/ 2 testes (male specific sex organs)
- in its absence, the gonad will develop into an ovary – if gene isn’t turned on
- This is when sex differentiation begins to develop
study found that if SRY gene inactivated in mice - even if XY chromosomes , female sex will develop, not male
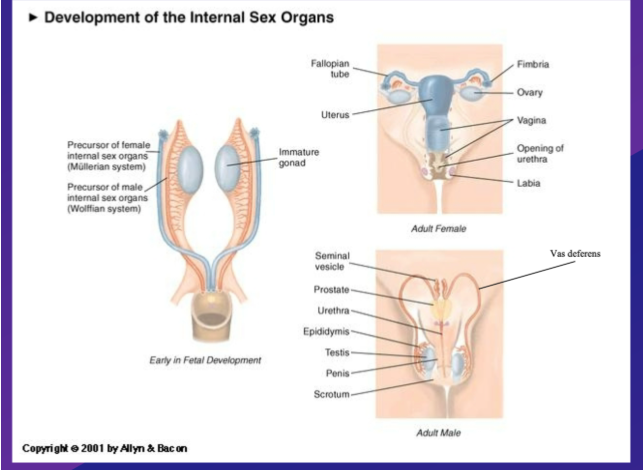
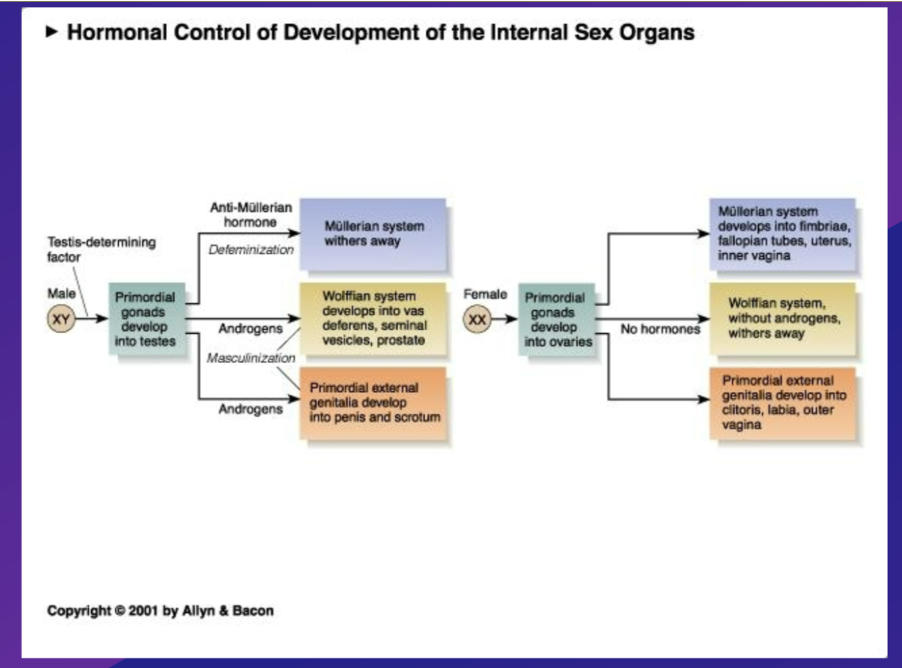
How is a sex determined in mammals : hormones - development of internal anatomy
2 precursor systems exist – which are both initially preset
Mullerian system - Precursor to female internal sex organs
Wolffian system – precursor to male internal sex organs - if gonads turn into testes and start producing required hormones
Once SRY has turned gonads into testis, hormones determine sex differences
if XY chromosome:
Testis produce testosterone – this occurs in early embryonic development
Early testis produces 2 types of hormones:
– Anti-Mullerian Hormone (defeminising) – responsible for getting rid of mullerian system:
binds to receptors in Mullerian system, causing it to disintegrate and eventually be removed i.e. destroys Mullerian system
– Androgens (masculinising) – group/ category of hormones means “man making” in Greek , (e/g/ testosterone is an androgen), responsible for maintaining the wolffish system: , have to be present and bind to receptors within the wolffian system to enable it to continue existing and eventually develop into the internal anatomy of the male system, only if there are androgens. –
• in the presence of these hormones (Anti-Mullerian Hormone and Androgens) internal genitalia will develop in a male specific pattern.
In the absence of these hormones (if Anti-Mullerian Hormone and Androgens not produced), internal genetalia/ will develop in a female specific pattern – i.e. female sex organs will develop. (primary sexual characters)
if XX chromosome - if gonad becomes ovary
if ovary developed , it produces no hormones at all.
but as testes are not present to produce hormones
No anti-Mullerian hormone – the female system will not be erased and so will develop and become established within physiology - female sex system will be maintained
no androgens present – wolffian system disappear –
which hormones do testes produce during early embryonic development?
– Anti-Mullerian Hormone (defeminising) – responsible for getting rid of mullerian system
– Androgens (masculinising) – group/ category of hormones means “man making” in Greek , (e/g/ testosterone is an androgen)
Mullerian system
Precursor to female internal sex organs
Wolffian system
precursor to male internal sex organs - if gonads turn into testes and start producing required hormones
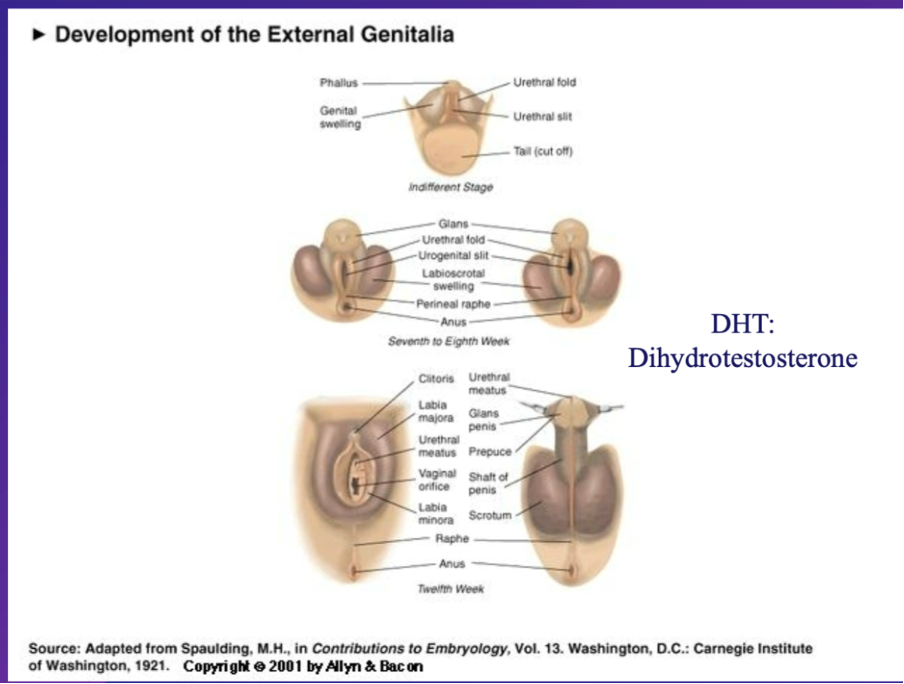
How is a sex determined in mammals : hormones - development of external anatomy
initially undifferentiated –regardless of XY or XX embryo
7-8weeks - once gonad has turned into testes or ovary, the external genitalia are sensitive to androgynes – particularly dihydrotestosterone
DHT - ( a hormone produced by the testes which binds to specific receptors and is required to turn external anatomy into male specific external anatomy e.g. scrotum, penis e.t.c)
if XY -
testes produce DHT , DHT binds to specific receptors and triggers the development of undifferentiated external anatomy into male specific external anatomy
XX chromosomes
if testes not present or cant perform its function due to e.g. absence of receptors , no DHT will produced to trigger male specific development and so female specific external anatomy will develop
i.e. what would become a
scrotum in a male developes into the external labia in females
penis shaft in a male developes into the internal labia
male glands would become a clitoras
gonads production of hormones which influenced development of internal and external sex specific hormones
summarise development of sex differences in mammals
1 - chromosomes XX or XY
2 - gene SRY - testes or ovary development
3- testes hormones = internal genitalea
4 - DHT androgen from testes = external geniatelea
dihydrotestosterone (DHT)
a hormone produced by the testes which binds to specific receptors and is required to turn external anatomy into male specific external anatomy e.g. scrotum, penis e.t.c
– a person with persistent mullerian duct syndrome has:
A -Male external genitalia, with testes, male and female internal genitalia
B -Female external genitalia with ovaries, male and female internal genitalia
C- Female external genitalia with testes and female internal genitalia
D -Male external genitalia, but only female internal genitalia
E- Female external genitalia, but only male internal genitalia
Answer = A
Because anti mullerian hormone only gets rid of mullerian system – doesn’t influence wolffian system
extra clarification -
Wolffian system is fully functioning e.g. making androgens etc., but anti- mullerian hormone isn’t functioning (either its not produced or the receptors aren’t there for it to bind to), so male internal sex organs will be fully formed but female internal genitalea will also develop – presence of uterus even though its not connected to anything e.g vagina as external male genitaleahas developed
The external genitalia of a person androgyn insensitively syndrome are….
A male
B female
Answer b - female
Explanation -a Person who is insensitive to androgynes – they make androgens but there are no (functional) receptors for the androgens to bind to as a result no extenrla genetic will develop in a male specific pattern
actions of hormones : define the two actions/ effects hormones can have
organisational or activiational
organisational hormone
effect of the hormone remains even after the hormone has been removed/ is absent post change. Often occurs during a sensitive period (e.g. embryonic development) i.e. its permanent
activation hormone
effect is reversible, depending on presence or absence of hormone –
Same hormones can have both types of effects dependent on context
are hormones utilised pre puberty during sex diffentiona development organisation or activation?
organisational as e.g. development of male/ female internal and external anatomy is permanent
however during puberty hormone role are both activational and organisational effects, one hormone can have both effects depending on context
puberty - characteristics / what happens
sex hormones can function within Organizational and/or activation roles
• Secondary Sexual Characters develop (everything prior was primary sexual characteristics)
• Pubic and axillary hairs are androgen (androstenedione) sensitive in both males and females
Which of these secondary sexual characteristics are due to organizational hormonal effects? (think trans people changes via hormones)
A-Increased facial hair in men
B -Increased muscle mass in men
C-Breast development in women
D-Wider pelvis in women
E-Wider shoulders in men
F-Lowering of the voice in men
C , D, E, F are organisational
all are secondary sexual characteristics
facial hair – activation: reduced Testeron reduced facial hair production
muscle mass – activation: ability/ ease of building muscle mass is influenced by testosterone levels
C = both:
if hormones reduced post breast development = organisational as if you lose all your hormones after you will still have breasts, but antinational as tissue volume will be reduced
D/E – oransational as they are skeletal features, so harder to change
F – organisational: once a mans voice drops it drops forever
But can prevent voice drop
Castrati men, 1800’s – men were castrated before puberty to keep soprano voice for their whole life
Can a hormone be just activation ?
Yes
how does puberty onset occur 1/2
During childhood, sex hormone levels are almost undetectably low
• Developmental timing mechanism starts puberty
• Sex differences in mechanisms and timings occur
further explanation
intitially Gonads (eggs/sperm) not making hormones, but at some point during teenager years hormones produced which change us into adult/ sexually mature humans via the development of secondary sexual characteristics (up until this point it has been the development of primary sexual characteristics)
(gonade
a reproductive organ that produces gametes (sperm or egg cells) and typically also secretes sex hormones.
Developmental timing mechanism
the biological processes that regulate when puberty begins and is initiated/ influenced by a range of factors – environmental, social and biological factors (e.g. weight and genetics) – the DTM ensures that puberty onset occurs in primal time according to these species specific factors
what factors influence the Developmental timing mechanism puberty onset/ when does puberty onset typically occur in women?
weight : evidence
Puberty onset age in women
1840’s– was 17
1960s – 13
studies now know When women’s hit 47 kilos puberty onset occurs – funds study which evidences this – studies on girls who have more fat hit puberty earlier - potentially due to evolution/ survival
Genetics also a big influence – mothers first period age between child and mother correlate in women, also occurs in father son dynamics – and puberty onset do readings
what is GNRH
gonadotropin releasing hormone
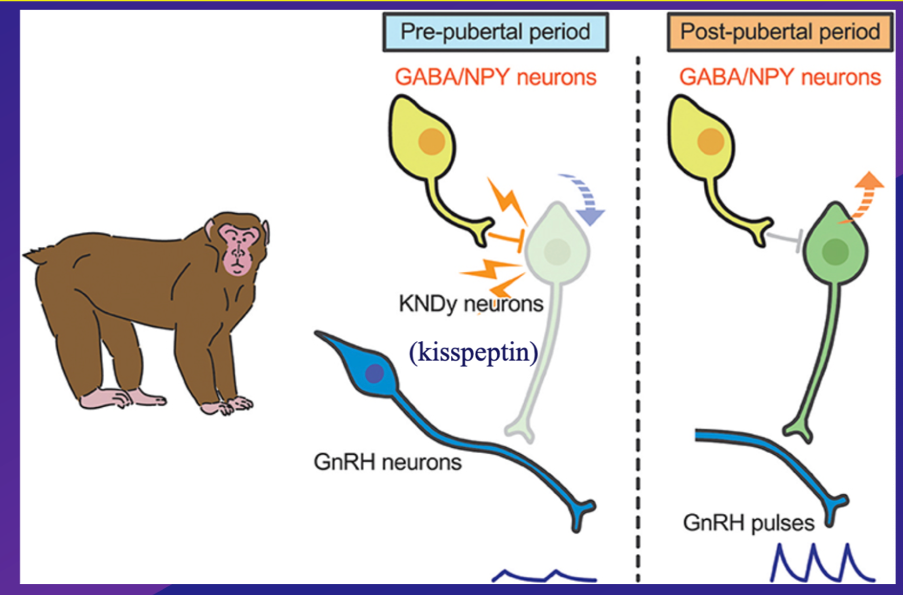
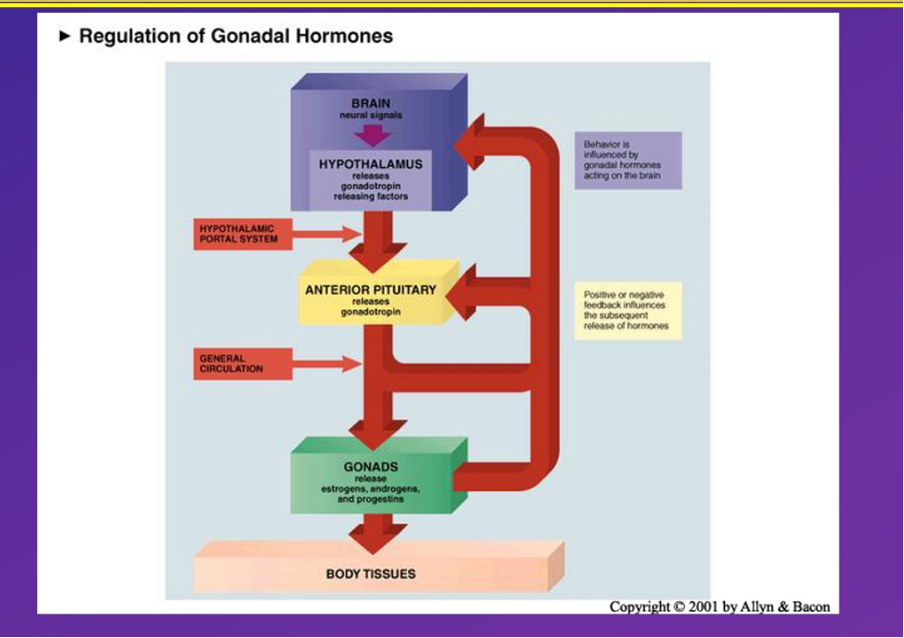
how does puberty onset occur 2/2 - Hypothalamo-Puitary-Gonadal (HPG) Axis
During childhood GnRH are largely inactive, inhibiting Gonadotropin release via indirect inhibtion –
NPY/ GABAergic inhibitory neurons are very active during childhood, they inhibit Kisspeptine (KSPY) neurons from generating action potentials and stimulating GNRH neurons, preventing them from releasing GNRH
once developmental timing mechanisms communicates, during puberty onset, NPY/ GABAergic neurons change and become less inhibitory and in some cases excitatory enabling kisspeptin neurones to become more activated and generate excitatory action potentials which stimulate GNRH neurons, enabling GNRH to be released in pulses every two hours –
within the Hypothalamo-Puitary-Gonadal (HPG) Axis GnRH is released in pulses every two hours by neurons in the hypothalamus into the bloodstream via blood vessles in the pituitry portal system, this blood containing GnRH is then immediately transferred into the pituitary stalk and then GnRH hormones binds to GnRH receptors in the anterior (portion of the) pituitary gland, triggering the production and release of gonadotropin hormones : Luteinizing Hormone (LH) Follicle-Stimulating Hormone (FSH) which travel to the gonads and stimulate a cascade of hormonal events that cause sex specific puberty onset in males by causing teste to produce testoerone or females by causing overaies to produce oestrodile
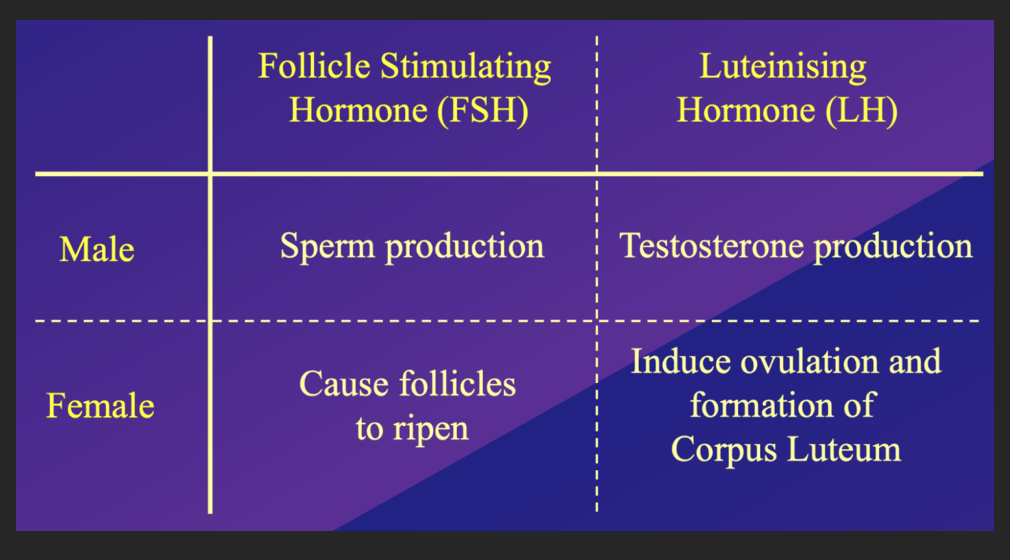
effect of gonoadotripon hormones on males and females:
follicle stimulating hormone -
males - sperm production
female - causes follicles to ripen
luteinising hormone
males - tester one production
female - induce ovulation and formation of corpus luteum
what do these images illustrate?
the invovledvement of GNRH in puberty onset - illustrated within the pituitary portal system in image 2
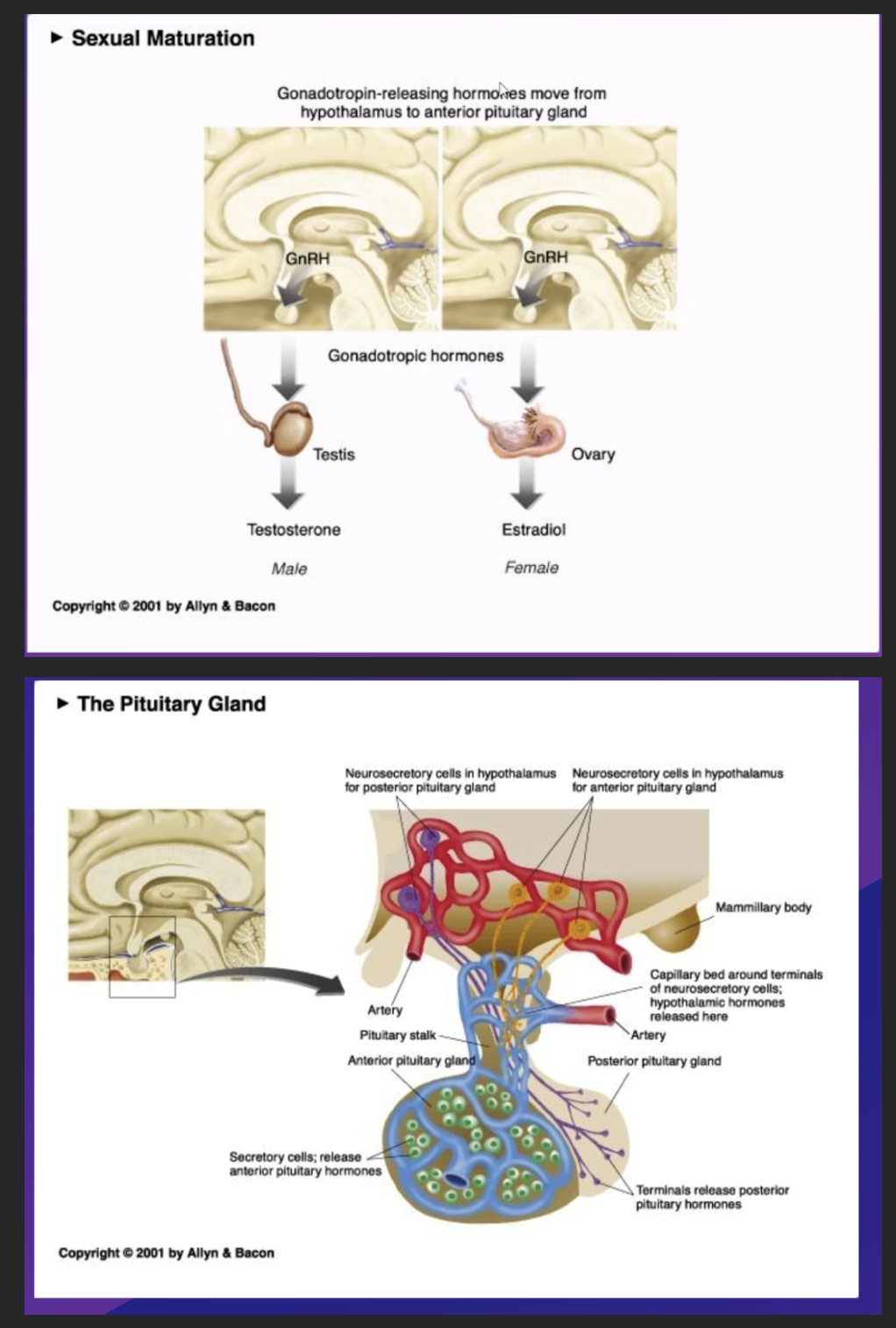
GNRH
gonadotropin releasing hormone – hormones which trigger the release of gonadotropins
define Gonadotropins
any group of hormones secreted by the pituitary which stimulate the activity of the gonads. i.e. hormones which go to the gonads
two types which have different effects in males and females
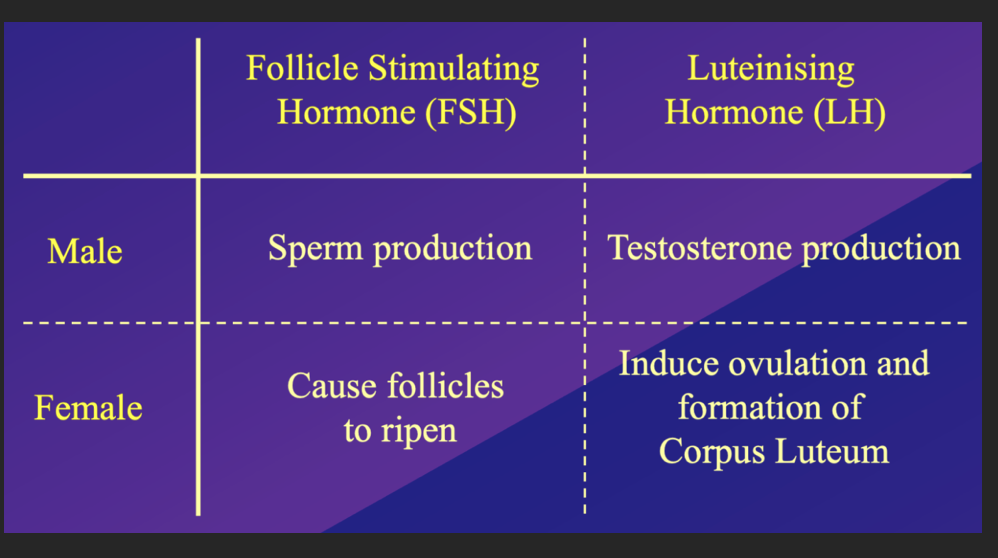
list the two types of gonadotripns released during puberty onset , and their effect on males and females
follicle stimulating hormone -
males - sperm production
female - causes follicles to ripen
luteinising hormone
males - tester one production
female - induce ovulation and formation of corpus luteum
their names are from female physiology - so they essentially say what they do to female physiology
(what is the corpus letup
The corpus luteum is a temporary structure that forms in the ovary after ovulation, the release of an egg from a follicle.
Key Points:
Formation: After the egg is released, the ruptured follicle transforms into the corpus luteum.
Function: The corpus luteum produces progesterone and estrogen, hormones that are crucial for maintaining the endometrium (lining of the uterus) and supporting an early pregnancy.
KPY/ kisspeptin neurons
direct activators of GnRH neurons
GABAergic neurons
directly regulate kisspeptine neuons, indrieclty influences GnRH neurons
ER - GABA/NPY always inhibitory?
GABA (always inhibitory) /NPY (not always inhibitory) neurotransmitter containing neurons. = neurotransmitters which are lreased by neurons adjacent to GnRH neurons to inhibit them from releasing sex hormones until pubrty onset
What is the system called where the hypothalamus communicates to the pituitary gland which then communicates to the gonads?
Hypothalamo-Puitary-Gonadal (HPG) Axis
What is the Hypothalamo-Puitary-Gonadal (HPG) Axis
what happens during puberty onset?
A system which explain how the hypothalamus communicates to the pituitary gland, which then communicates to the gonads.
Some Neurons in the hypothalamus terminate at blood vessels and release the messenger molecule GnRH into the blood stream
binds to receptors in the anterior pituitary gland which trigger secretory cells, cause them to produce and release gonadotropins. (in pumps every approx two hours I think)
These gonadotropins (hormones) are then released into the bloodstream throughout the whole body and bind to its complimentary receptors in the gonads – and where the subsequenrly make an impact
Gonadotropins influence
In males – testes/ effect testosterone
In females – ovaries: effect estradiol, progesterone
puberty : the HPG - axis effect in typical males during puberty / post puberty
describe the negative feedback system
THe HPG- axis acts. simple negative feedback loop in males - enabling testoerone levels and sperm production to be maintained at a ertan volume
LSH produces testerone cause T levels to increase post puberty onset, to maintain homeostasis HPA axis utilises a negative feedback system in whch if T levels too high specialised recpetorsi n the blood which bind to T detects this, causing production rates of T to be reduced via inhibiting GNRH release. similarly I this is too low, lack of receptors binding to T results in increased T production enabling a baseline production rate to be maintained
within the HPG-axis The hypothalamus releases GnRH, which stimulates the pituitary to release LH and FSH.
LH and FSH act on the testes, leading to the production of testosterone.
resulting in increasing levels of testoeron, if levels rise beyond threshold point, receptors detect this, negative feedback then occurs as receptors inhibit GNRH and subsequent gonadotropins production and release, decrease the release of GnRH, LH, and FSH into the bloodstream
similarly if levels drop too low, receptors within the blodostream detect this, and transmit messages which increase GNRH production within the Hypothalamus subsequently releasing increased gonadotropins
thus controlling the production of sperm and maintaining hormonal balance.
What are consequences on the HPG axis of taking anabolic steroids?
A) testes make low amounts of testosterone
B)the pituitary makes extra LH and FSH
C)the hypothalamus produces less GnRH
D)testes will shrink
E)testes make more testosterone
Can be multiple answers
Context: Anabolic steroids mimic testosterone / artificial testosterone to build muscles
ACD
Because use of anabolic steroids will look like T levels are high to the hypothalamus and anterior pituitary gland because it binds to the T receptors in the Pituitary gland and hypothalamus, receptors will then falsely detect that T receptors are high
Causing the hypothalamus to stop producing GnRH and the pituitary gland to in turn stop producing Gonadotropins, causing T production to be reduced in the testes and shrink because they aren’t being stimulated by either FSH or LH – this is a logn term effect that will only occur if you are a chronic user of anabolic steroids as if celsl used to produce sperm/ T aren’t stimulated
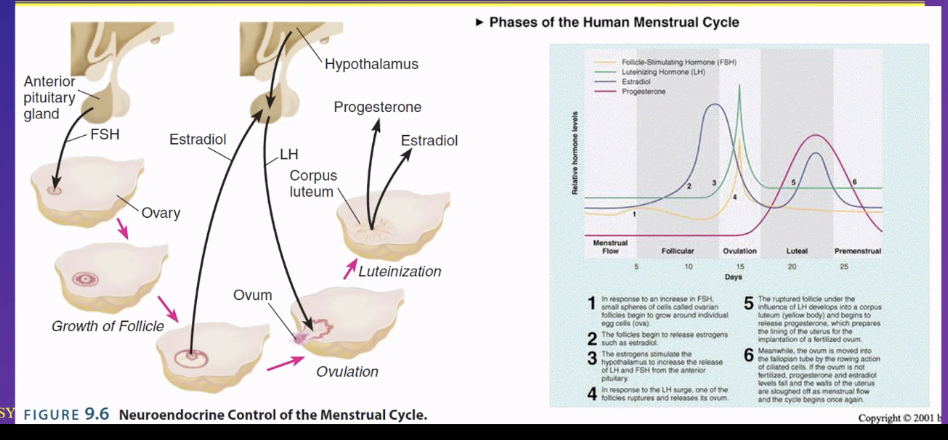
HPG axis in a typical female during/ post puberty - human mammels during
negative feedback loop
as we are fertile year round)
- More complicated than in males
- continuous 4 week cycle - as we are fertile year round)
Graph to the right shows the levels of 4 different hormonsi n the bloodstream thoguhout one menstrual cycle
Diagram on left illustrates what happens: phases of the menstrual cycle
Stage 1 – menstrual flow i.e.period
Each ovarian follicle contains one egg cell (oocyte)
1) Increased release of follicle stimulating hormone (FSH) from the anterior pituitary gland occurs.
these hormones bind to ovarian follicles (small spheres of cells in the ovaries) l, causing them to ripen and begin to grow around their individual egg cells (ova) via local interactions
only one dominant follicle developed fully , the others degenerate between day 5-13 (during the follicular phase), as it grows it starts
2) As the dominant follicle grows it begins to produce and release oestrogens such as oestradiol , causing oestradiol concentration in the blood to increase.
3) Once a threshold amount of oestradiol has been produced, it will stimulate the hypothalamus and trigger GnRH production, increasing the release of LH and FSH from the anterior pituitary in a short but highly concentrated peak
4) ovulation occurs In response to the LH surge, the dominant follicle ruptures and releases its ovum (egg) which then goes down the fallopian tubes
5) after ovulation, the ruptured follicle, develops into a corpus luteum (yellow body) under the influence of LH and actively produces and release progesterone primarily (which up intil this point has been very low) and estrogen, which prepares (by thickening upand maintains) the uterin lining for the embryo implantation if fertilisation occurs.
These hormones also inhibit the hypothalamus and pituitary gland , temporarily preventing them from releasing FSH and LH – providing the function of prevent new follicles from developing which the body prepares for a possible pregnancy. (enacting negative feedback)
6) If fertilisation occurs, the ovum is transferred into the fallopian tube by the rowing action of ciliated cells, if fertilised the embryo signals the corpus luteum to continue producing hormones until the placenta gradually takes over the role of hormon production at approx. 10-12 weeks of pregnancy , once it fully takes over the corpus luteum degenerates.
7) If fertilisation does not occur/ If the ovum is not fertilised, the corpus luteum breaks down (degenerates) after approx. 10-14 days, causing the progesterone and estradiol hormone levels to fall sharply as they are no longer being produced.
8) Menstruation begins - The decline in these hormones (particularily progesterone) causes the walls of the uterus to shed be sloughed off as the menstrual flow, resulting in menstrual bleeding- marking day 1 start of a new cycle beginning once again
9) When the drop in estrogen and progesterone hits a low enough point – the uterin lining will get discarded again – a period will occur , at the end of which peak will occur and cycle will start again
As the pituitary gland is no longer inhibited , FSH will be released again which stimulates new follicle production in the ovaries, enabling the cycle to begin again
(ER - why is negative feedback necessary in Female HPG axis
Estrogen and progesterone exert negative feedback on the hypothalamus and pituitary to regulate the release of GnRH, LH, and FSH.
Because if FSH (Follicle-Stimulating Hormone) wasn’t inhibited, it would continuously stimulate multiple follicles to develop, potentially leading to:
1. Multiple follicles maturing at the same time, which could result in the release of multiple eggs (increasing the chance of multiple pregnancies, like twins or triplets).
2. Disruptions in the menstrual cycle, as new follicles would keep developing instead of following a coordinated cycle. – as could lead to multiple dominant follicles and the overproduction of eggs or multiple ovulations, and oluation could occur at innapropriate itmes in the cycle which could lead to cycles that are too short or too long
(How does progesterone only pill prevent pregnancy?
Progesterone is only high during the luteal phase, during this phase no new ovulation can occur – if you get pregenense progesterone levels stay high aswell – preventing ovulation. fertilisation of another egg from occurring. So if you take a progesterone only pill this will also prevent pregnancy and ovulation from occurring
(The negative effects of anoabolic steroids on females
Same as males , all the secondary sexual characteristics that are typical of males you would get too e.g. facial hair, muscle mass increase, voice drop e.t.x because these steroids mimic testosterone
(What is the difference between a follicle and the fallopian tube?
follicle is a small, fluid-filled sac within the ovaries that contains an immature egg (oocyte).
The fallopian tubes are tubes that connect the ovaries to the uterus.
(Estrogens
- a group of hormones that play key roles in the female reproductive system and contribute to the development of female secondary sexual characteristics
List three types of variation that can occur regarding sexual differentiation
◦ Androgen Insensitivity Syndrome
◦ Sa-reductase deficiency
◦ Congenital Adrenal Hyperplasia
What is Androgen insensitivity syndrome
The body is insensitive to androgens if androgen receptors are unable to function due to a genetic mutation on the X chromosome
What is Androgen insensitivity syndrome effect on XY individuals pre-puberty and during puberty
summarised
◦ Gonads develop as testes
◦ Androgen receptors do not work
◦ Testosterone cannot do its normal job
Gonads secrete anti-Mullerian hormone and androgens but due to lack of compatible receptors to bind to, androgens are unable to perform function of developing internal male genitalea/ masculinising effect
due to presence of anti-mullarian hormone female internal sex organs wont develop either
Due to lack of androgens, gonad will not develop into testes, so DHT will not be produced inhibiting the development of male specific external anatomy
due to the lack of DHT female external anatomy will develop, but the vagina is hollow
individual is perceived and typically raised as female , typically identify as female
at puberty the person undergoes female specific puberty characteristics but cannot have biological children due to a lack of ovaries and uterus – female internal sex organs
Is typically described in males (46 XY individuals)
Testes although cannot be used to produce androgens , can still produce enough oestradiol to trigger typically late puberty onset developing female secondary sexual characteristics during late onset puberty,. – wont be able to experience a period due to lack of uterus but experience e.g. breast development etc. puberty onset can sometimes be helped with hormone supplements to increase onset
Testosterone will also be produced significantly , but due to androgen insensitivity although its produced it cant do anything ,so no secondary sexual male characteristics will develop
What is Androgen insensitivity syndrome effect onXY individuals pre-puberty and during puberty
If XX chromosome - AIS doesn’t effect individuals :
- No anti malarian hormone, internal female genitalea will develop, no androgens present – wolffian system will dissipate (no androgens were meant to be present anyways) e.g. the receptors for androgens (e.g. testoerone/ dihydrotestosterone aren’t functioning.
- As testes don’t develop, no DHT is produced so female external anatomy will develop
- Producing XX individual who undergoes female specific pubtery and is able to produce children
what is the treatment for people with androgen insensitivity syndrome
Treatment upon diagnoses
Sometimes the testes are removed upon diagnosis – due to perceived risk of them becoming cancerous
Individuals can receive hormone treatment which results in them experience typical female hormone change and continue living as women
Complete Androgen Insensitivity Syndrome in 46,XX individuals leads to
A- Masculinized external genitalia
B- Lack of pubic hair
C -Testes
D -Infertility
Read question carefully XX= FEMALE
Answer – B
Because
Not infertile because infertility isn’t dependent on testosterone at all
The only thing on list that depends on androgens (testosterone or androstenedione) in both men and women is pubic hair and axillary hair.
So if insensitive to androgens pubic hair will not develop
complete 5a-reductase deficiency (5 alpha reductase deficiency)
5a-reductase = An enzyme that converts Testosterone into Dihydrotestosterone (DHT)
5a-reductase deficiency = (partial = a reduced) completed = an absent conversion of testosterone to DHT
DHT is necessary for the prenatal development of male external genitalea during embryonic development – needs to bind to receptors to develop male external genitalea
46, XY individiausl
children are born with female external genitalia, but only male internal genitalia – as anti mullerian hormone is fully functioning so internal female genitalea will be erased
typically perceived and raised as female, identify as female pre puberty
during puberty -
Testosterone levels get so high that even the receptors that are normally only sensitive to DHT begin responding to the high Testeron levels because of the molecular similarity, enabling testoerone to “mimic” DHT. As a result external male genital begins to develop/ a penis will begin to develop at puberty as – labia physically turns into a penis and scrotum
typically identify as men , post puberty onset
46 XX individuals
can have 5 alpha reductase deficiency
has significantly less impact as DHT isnt a significant influencer of female physiology, btu they may pass it on to their children
cause
Can be caused by a genetic mutation in a gene that produces the 5a reductase enzyme
evidence - Region in Guatemala where these people are so common they are called “quevenoches” I think which translates to “penis at 12” - prominent in small populations where rare genes are more likely to be continued formg eneration to generation and be more common
XY indivdial treatment
Identified in infancy/ earl childhood – genital surgery to address partially develop male external genitals – creating/ constructing a penis
Most receive testosterone replacement therapy to induce male secondary sexual characteristics - puberty onset
Internal male structures remain function, external typically wont fully develop
What I 5a reductase?
An enzyme that turns Testosterone into Dihydrotestosterone (DHT)
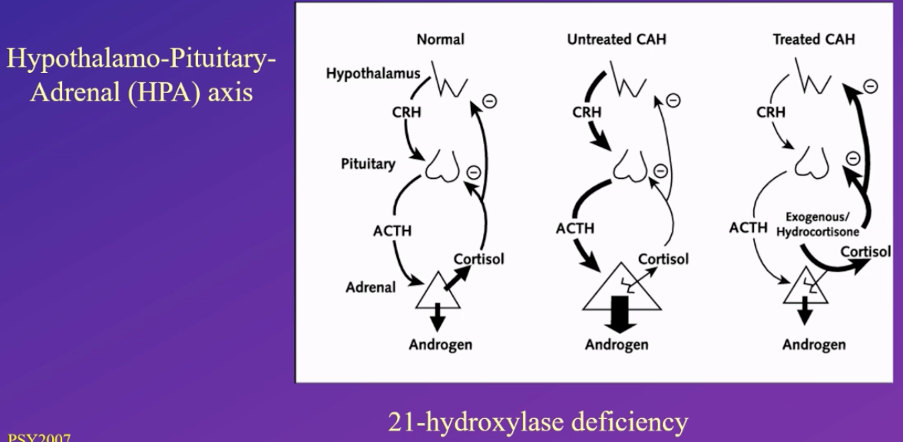
Congenital Adrenal Hyperplasia - what causes CAH
the adrenal cortex in the adrenal gland produces cortisol hormone (i.e a stress hormone)
21 hydroxylase enzyme – an enzyme which makes the final contributions to make cortisol
People with CAH
21 hydroxylase doesn’t function fully, as a result cortisol cant be produced inhibiting its ability to function
Congenital Adrenal Hyperplasia - what is cortisols function
Cortisol function in the body/ why is it an important molecule: when an individual is
- When an individual is stress
- Maintaining the salt and water balance in the body
- Involved in energy balance of e.g. monitoring glucose in the bloodstream
Congenital Adrenal Hyperplasia - what is the impact of CAH on xx indviduals
In developing female embryo – normally no androgens are present, but under these conditions increased androgen presence will occur, resulting in high levels of pre-testosterone being produce, resulting in some primary male sexual characteristics developing during embryonic development in addition to female internal genitalea
As a result of high levels of prenatal testosterone the external genitalae will be partially masculinised – can range from e.g. larger clitoris to a fully developed penis depending on factors such as testosterone levels – resulting in ambiguous genitalea
Congenital Adrenal Hyperplasia - what is the typical diagnosis and treatment of CAH on xx indviduals
diagnosis -
Typically identified shortly post-birth as this condition is usually easily identified in females at birth
Not typically identified with males until low cortisol elve symptom occur
treatment
- Typically treated shortly after birth and once diagnosed as this condition is usually easily identified in females at birth
- Typically get corrective surgery so external gentialia look exclusively female, still have the potential of fertility, identify as female post diagnosis – male external genitalea has only partially develop
- If male external genitalea has fully developed, even if they know chromosome sex the parents may choose to raise the baby as a boy, or get corrective surgery and raise a girl
-Individuals given extra cortisol, or a replacement for cortisol called - exogenous hydrocortisone – which mimics cortisol
HPA axis is a negative feedback mechanism, so by supplying external cortisol the HPA axis will reduce cortisol precursor production, inhibiting low cortisol levels and symotoms
Both solving the symptoms relating to low cortisol levels and reducing high tester one levels
Congenital Adrenal Hyperplasia - what is the typical gender assignment of CAH on xx indviduals, do individuals experience gender dysphoria?
Gender assignment
- 5% of CAH girls assigned female at birth have gender dysphoria – feel like being female isn’t their gender (more than the general population)
- 12% of CAH "girls" (46 XX individuals) assigned male at birth have gender dysphoria
- Conclusion – i.e. the majority of 46 XX children assigned male at bith (with female specific internal genitalea) were happy being men , but 12% weren’t – highlights how ocmpelx gender identity is and infleunces of how you look – external anatomy nad internal influecnes via e.g hormones, environemt – surrounding/ how you were raised
-
Congenital Adrenal Hyperplasia - what is the impact of CAH on XY indviduals
XY indvdials – males
- High amount of androgens will develop due to incomplete cortisol precursers
- For XX indivdials the excess androgen isn’t problematic - Intenral and external male
specific development isn’t altered by CAH / presence of additional testoerone
- Low cortisol symptoms develop , typically become evident later in life
Congenital Adrenal Hyperplasia - what is the diagnosis/ treatment of CAH on XY indviduals
diagnosis
- more diifcult to identify in males – as they have high levels of testerone during early development anyways
- condition is typicaly diagnosed when symptoms associate with low cortisol leves become prevalent
- treatment – treat low cortisol to adresss excess androgen is typically only treatment.