CNS Path
1/99
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
100 Terms
What are the different types of glial cells? Briefly describe them.
- Microglia = Resident macrophages
- Astrocytes = Support cells. Make up the BBB, participate in ion excahnge, responsible for forming "scar tissue" in the CNS, etc.
What cells contribute to the white matter of the CNS and how?
- Oligodendrocytes produce CNS myelin (vs. Schwann cells in the PNS)
What are ependymal cells?
- Cells lining the ventricular system
What is the choroid plexus?
- Blood vessels lined by specialized epidenymal cells -> CSF production
Define the following terms:
A. Encephlo-
B. Myelo-
C. Meningo-
D. Polio-
E. Leuko-
F. Malacia
A. Of or pertaining to the brain; also cerebro-
B. Of or relating to the spinal cord
C. Membrane/meninges
D. Denoting grey matter
E. Denoting white matter
F. Necrosis/softening
Define the following words:
A. Leukoencephalomalacia
B. Poliomyelomalacia
C. Meningoencephalomyelitis
A. necrosis (malacia) of the white matter of the brain
B. necrosis (malacia) of the grey matter of the spinal cord
C. inflammation of the meninges, brain, and spinal cord
What are the 4 primary defense mechanisms of the CNS?
1) Mechanical barriers (skull, vertebrae, meninges)
2) Microglia (Resident tissue macrophages)
3) The BBB
4) The blood-CSF barrier
What is the function of the BBB?
- Limits entry of pathogens and small molecules (including many therapeutics) to the brain via the blood
What types of molecules/things can cross the BBB?
- Many lipid soluble molecules can diffuse across the cell membrane and are NOT excluded.
What are the components of the BBB?
- Vascular endothelium, sealed with tight junctions
- Capillary basement membrane
- Astrocyte foot processes wrapping around capillaries (Secrete paracrines that promote tight junction formation)
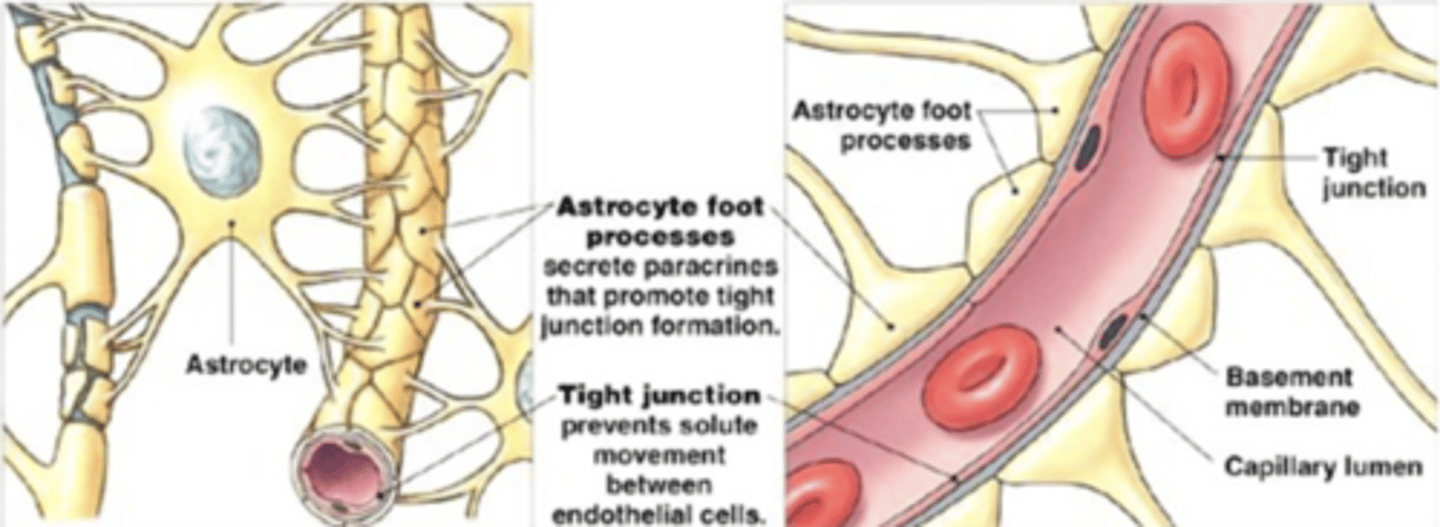
What is the function of tight junctions?
- Prevent solute movement between endothelial cells
What sort of things can compromise the BBB?
- Microwaves
- Radiation
- Trauma
- Hypertension
- Infection/inflammation
What is the function of the blood-CSF barrier?
- The same as the BBB but located in the choroid plexus (Limits entry of pathogens and small molecules (including many therapeutics) to the brain via the blood)
What are the components of the blood-CSF barrier?
- Vascular endothelium
- Modified ependymal cells
What is the basis for neurotropism?
- The ability of microorganisms to breach the four immune barriers of the nervous system (physical barriers, microglia, BBB, Blood-CSF barrier)
What are the portal of entry to the nervous system?
1) From the "head holes"
2) From the blood
3) From the neurons (retrograde axonal transport)
How do the "head holes" act as a portal of entry to the nervous system? Does this method bypass the BBB?
- Extension of inflammation from the eyes, eras, sinuses, nasal cavity, tooth roots, guttural pouch, etc.
- Direct extension bypasses the Blood-Brain barrier
How does the blood act as a portal of entry to the nervous system? Does this method bypass the BBB?
- Hematogenous/systemic infections (with the caveat that the organisms must be able to breach the Blood-brain barrier)
- No, but some "Trojan Horse" organisms carried intracellularly by leukocytes can sometimes pass
How do neurons (retrograde axonal transport) act as portals of entry to the nervous system? Does this method bypass the BBB?
- Some pathogens have receptors that encourage uptake by axonal processes; Following uptake, the pathogen is transported retrograde up the axons to the neuronal cell body, where it exerts its effects.
- Yes; Bypasses the BBB
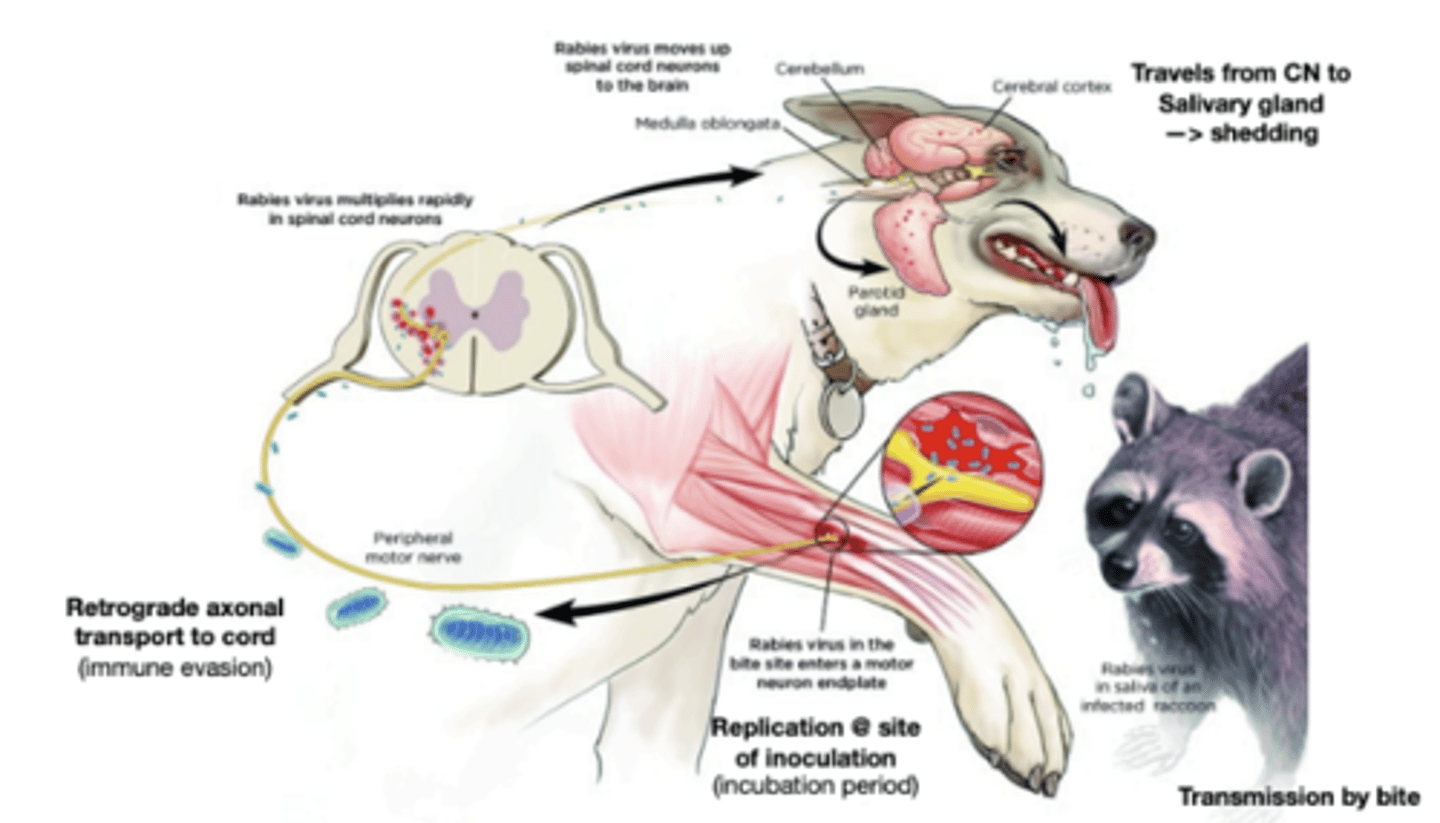
Describe the pathogenesis of Rabies as an example of neurons/retrograde axonal transport as a portal of entry to the nervous system.
- Rabies virus in the saliva of an infected raccoon is transmitted by bite -> There is replication at the site of inoculation(incubation period) -> Retrograde axonal transport to cord (immune evasion) -> Rabies virus multiplies rapidly in spinal cord neurons -> Rabies virus moves up spinal cord neurons to the brain -> Travels from CNS to the salivary gland (Shedding)
What is the critical first step for neurologic patients?
- Neuroanatomical localization of lesions based on a thorough neurologic exam.
- Note: especially important for submitting for radiology or pathology (tell them where to look)
What are some components of a thorough neurologic exam?
- Mental status
- Gait and posture
- Postural reactions
- Cranial nerve exam
- Spinal reflexes
- Pain sensation
A head tilt is indicative of a problem with the ____________ system. How can neuroanatomic localization be further broken down for this lesion?
- Vestibular
- Central (brainstem/cerebellum) vs. peripheral (Ear)
Describe whether each of these clinical signs would occur with a peripheral or central vestibular dysfunction
A. Altered mentation
B. Head tilt
C. Loss of balance
D. Vestibular ataxia
E. Cranial nerve deificts
F. Horizontal nystagmus
G. Rotary nystagmus
H. Vertical nystagmus
I. Nystagmus of a changing direction
J. Positional ventral
K. Horner Syndrome
L. Proprioceptive deficits
M. Cerebellar signs
A. Central
B. Both
C. Both
D. Both
E. In peripheral -> VII, occasional V; In central -> Multiple
F. Peripheral; Uncommon with central
G. Both
H. Central
I. Possible in central
J. Both
K. Possible in peripheral, rare in central
L. Usually in central
M. Possible in central
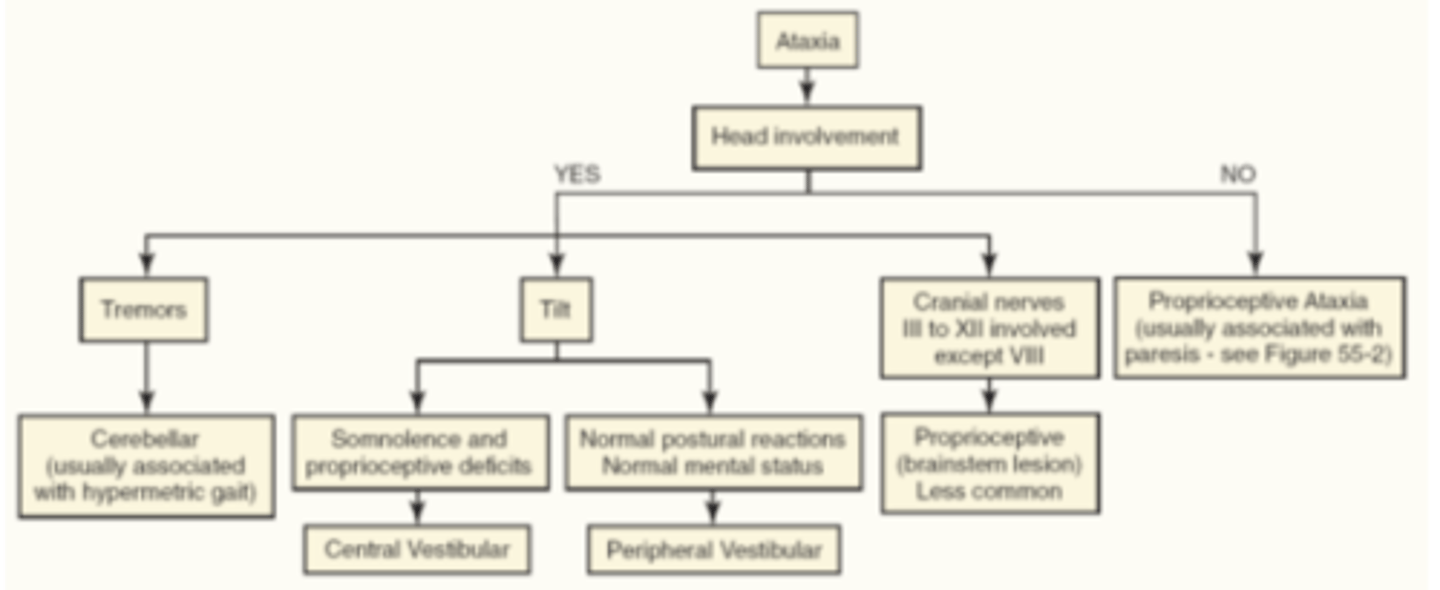
Regarding ataxia, what is the first thing one should consider when trying to come up with a neuroanatomic diagnosis/lesion localization? What does this tell you?
- Whether or not there is head involvement
- If there is no head involvement -> Proprioceptive ataxia (usually associated with paresis)
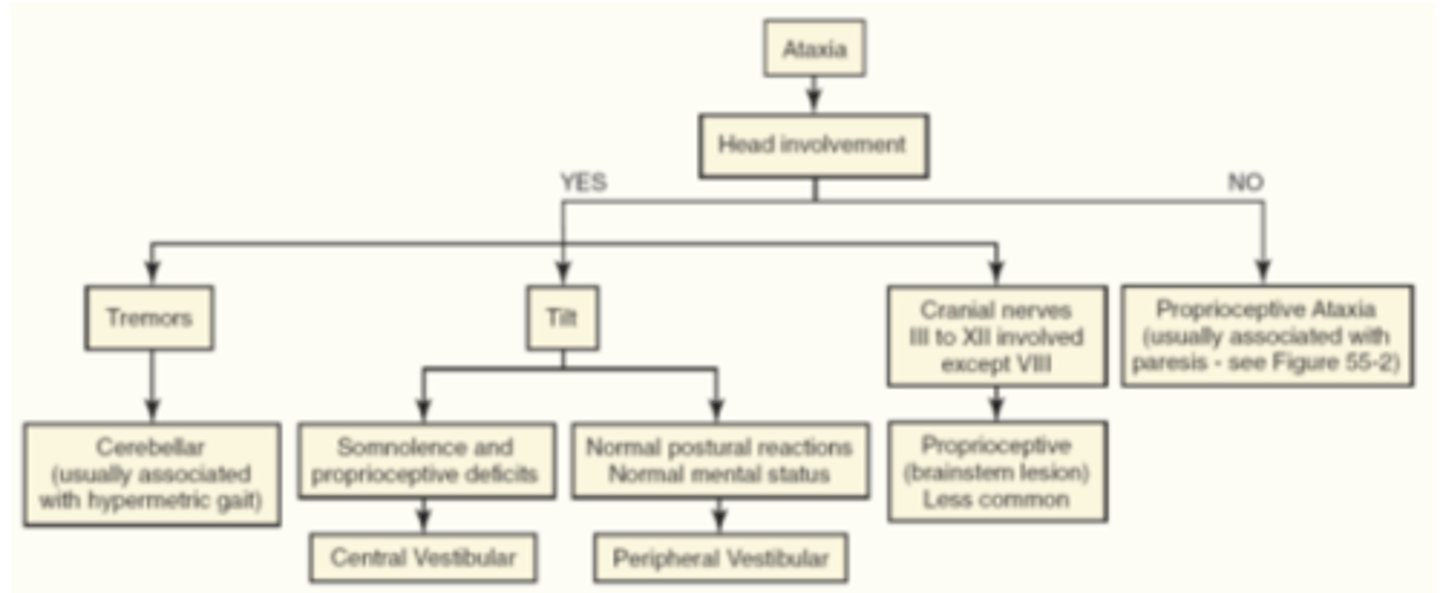
If there is head involvement in an ataxic patient, what is the next thing you should consider?
- Ask yourself whether there is head tremors, head tilt, or CN involvement
- If there are head tremors -> Cerebellar ataxia (usually associated with hypermetric gait)
- If there is a head tilt with normal postural reactions and normal mental status -> Peripheral vestibular ataxia
- If there a head tilt with somnolence and proprioceptive deficits -> Central vestibular ataxia
- If there is a head tilt with CN involvement -> Proprioceptive (brainstem lesion) ataxia
What are some tips for generating a list of differential diagnoses for neurologic patients?
- Rank differentials for site and signalment (What is most likely in THIS patient?)
- Start with generic "big picture" differentials before jumping to specific diseases/agents
Bilaterally symmetrical lesions are more likely due to ____________ causes but not all _______________ diseases produce symmetrical lesions.
- Systemic/Systemic
Keep _______________ as a top of mind differential diagnosis for when dealing with neurologic mammals.
- Rabies
What are some extracranial causes of neurologic signs?
- Severe systemic illnesses may result in "moribund" animals who appear neurologic, disoriented, stumbling, etc. but do not have a primary neuropathic disease
What are differentials diagnoses for seizures (Consider extracranial vs. intracranial)?
- Intracranial: Inflammation, neoplasia, malformation, trauma, toxins, neuronal degeneration, idiopathic epilepsy
- Extracranial: Hypoglycemia, liver disease, hypocalcemia, renal disease, hypoxia
What are some methods for diagnosis of neurologic disease?
- Thorough neurologic (and physical) exam, including anatomic neurolocalization
- Minimum database
- Imaging
- Pathology
- CSF Analysis
What is included in a minimum database when diagnosing a patient with neurologic sigins? What is the purpose?
- BW: CBC/Serum chemistry
- r/o extracranial or systemic disease
What are some indications for imaging when diagnosing a patient with neurologic signs?
- Trauma
- Neurologic signs localized to the brain, CNS, or spinal nerves
When is biopsy of a lesion indicated in a patient with neurologic signs? When might it be necessary?
- If other tests have failed to yield a definitive diagnosis (poking the brain is usually a last resort)
- May be necessary for differentiating neoplasia from mimics (inflammatory or infectious disease, vasculitis, etc.) or benign from malignant neoplasms
What are indications for CSF analysis?
- Abnormal neurologic exam
- Recurring fever of unknown origin
- Neck or limb pain
What does increased protein in the CSF indicate?
- Increased protein is nonspecific (Seen in many diseases; So basically, it doesn't mean much)
Increased cells in the CSF is called ______________.
- Pleocytosis (Example: Neutrophilic pleocytosis)
Describe a normal cytology of the CSF.
- Normally ~80-90% large mononuclear cells and lymphocytes; <10% neutrophils
Describe the sensitivity of CSF analysis for infectious agents.
- CSF analysis is not sensitive for infectious agents. Some organisms such as fungi may be seen on cytology, but bacteria are rarely observed
- Culture (or PCR) more sensitive
Describe the proper collection method for CSF analysis.
- Collect into EDTA tubes for fluid analysis; Red top (no additives) for culture)
Desrcibe the stability of CSF samples.
- Sample stability is low: CSF must be analyzed ASAP after collection (same day) to minimize cell degradation. If sending to a reference lab, ship overnight on ice.
__________ contamination of CSF samples is very common.
- Blood (another reason to add EDTA - anticoagulant)
In general, CSF analysis is neither sensitive nor specific. CSF analysis is most sensitive for ______________ disease.
- Inflammatory
You are most likely to see CSF changes with what types of lesions?
- Acute (vs. chronic) lesions)
- With meningeal or periventricular (vs. parenchyma) lesions
Will CSF analysis detect neoplasia?
- Round cell tumors (lymphoma, histiocytic sarcoma) may be detected, but other probably not.
What differentials should be considered when mild pleocytosis is observed? Moderate pleocytosis? Severe pleocytosis?
- Mild (5-25 microliters): Consider viral infections, trauma, vascular disease
- Moderate (25-100 microliters): Consider fungal/protozoal infection
- Severe (>100 microliters): Consider bacterial, immune-mediated disease
Which differentials should be considered given the following findings on CSF analysis?
A. Neutrophilic pleocytosis
B. Eosinophilic pleocytosis
C. Lymphocytic pleocytosis
D. Mononuclear pleocytosis
E. Mixed pleocytosis
A. Bacterial meningoencephalitis, Fungal meningioencephalitis, Toxoplasma, Immune mediated (SRMA), IVDD, neoplasia, trauma/hemorrhage
B. Protozoal, fungal (Cryptococcus), algala, helminthic, salt toxicity (pigs), lead toxicity (cows)
C. Rabies, Distemper, Fungal meningoencephalitis, NME, Toxoplasma, Rickettsia, Listeria
D. Neospora, GME, Rickettsia, Subarachnoid hemorrhage, Granulomatous disease
E. Fungal (Blastomyces), Protozoal, FIP, GME
True of false: Congenital and developmental disorders are uncommon in animals.
- False; They are common and "come in many flavors"
What are causes of developmental disorders in animals?
- Inherited
- Infectious
- Toxic
- Sporadic (idiopathic)
What is a tetrogen?
- Any agent or factor that causes malformation of a developing embryo
What are major patterns/categories of developmental disorders in animals?
- Failure to develop (aplasia, hypoplasia, dysplasia, dysraphism)
- Premature degeneration (cerebellar atrophy, viral encephalitis)
- Functional disturbances with normal structure (lysosomal storage disease, epilepsy)
Many congenital defects in animals are associated with viruses. Which viruses?
- Arboviruses ("arthropod borne") such as West Nile Virus and Bluetongue Virus
- Pestiviruses such as BVDV, Classical Swine Fever, and Border Disease virus
- Parvoviruses, such as Canine and Porcine Parvovirus and Feline Panleukopenia virus
Neural tube defects in early gestation create _____________.
- Dysraphisms (Also called "Organo-schisis" such as palatoschisis or cranioschisis)
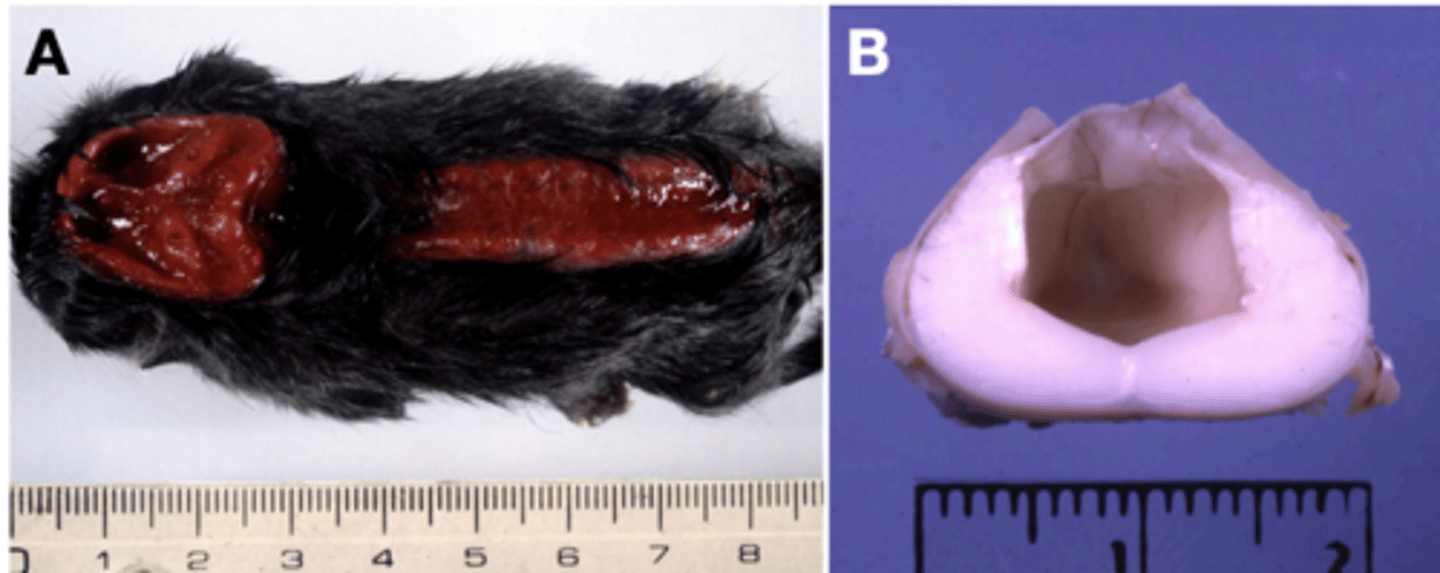
What are examples of dysraphisms in the brain? In the spinal cord?
- In the brain: Anencephaly, encepahlocele, meningecele, meningoencephalocele
- In the cord: Spina bifida (Amyelia (A), hydromelia (B), Meningomyelocele, dermois sinus)
Define microcephaly.
- Small brain
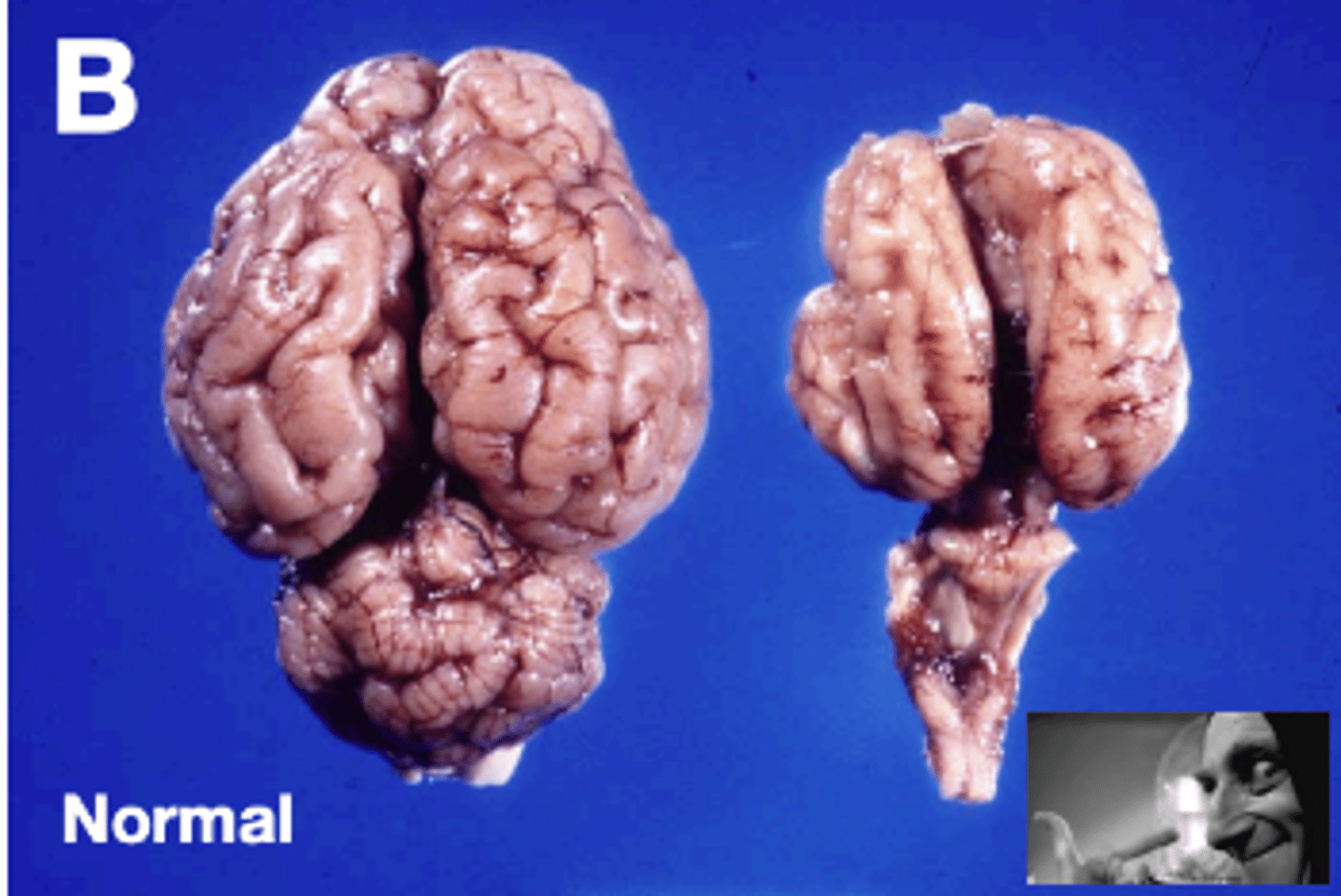
Define lissencephaly. In what species is this normal?
- Smooth brain
- Normal in birds, rodents, and rabbits
Define pachygyria.
- Thick gyri
Define holoprosencephaly.
- "whole prosencephalon" - fusion of the two hemispheres of the prosencephalon into one structure. Also associated with cyclopia.
Define polymicrogyria.
- Many small gyri
What implications does the BBB have for drug administration?
- The BBB excludes many molecules including drugs. Selection of drugs permeableto the BBB (such as lipid soluble drugs) is desirable for treating intracranialdisease. Radiation may increase the penetration of drugs into the CNS
Describe the general pathogenesis of Wobblers.
- Spinal cord compression (usually in the region of the neck) by bony structures which can be static (compressed all the time regardless of movement) or dynamic (occurs with certain movements)
Cerebellar hypoplasia and dysplasia are very common. Why?
- Due to extensive postnatal development of the cerebellum. In animals, most cases are associated with in utero viral infection
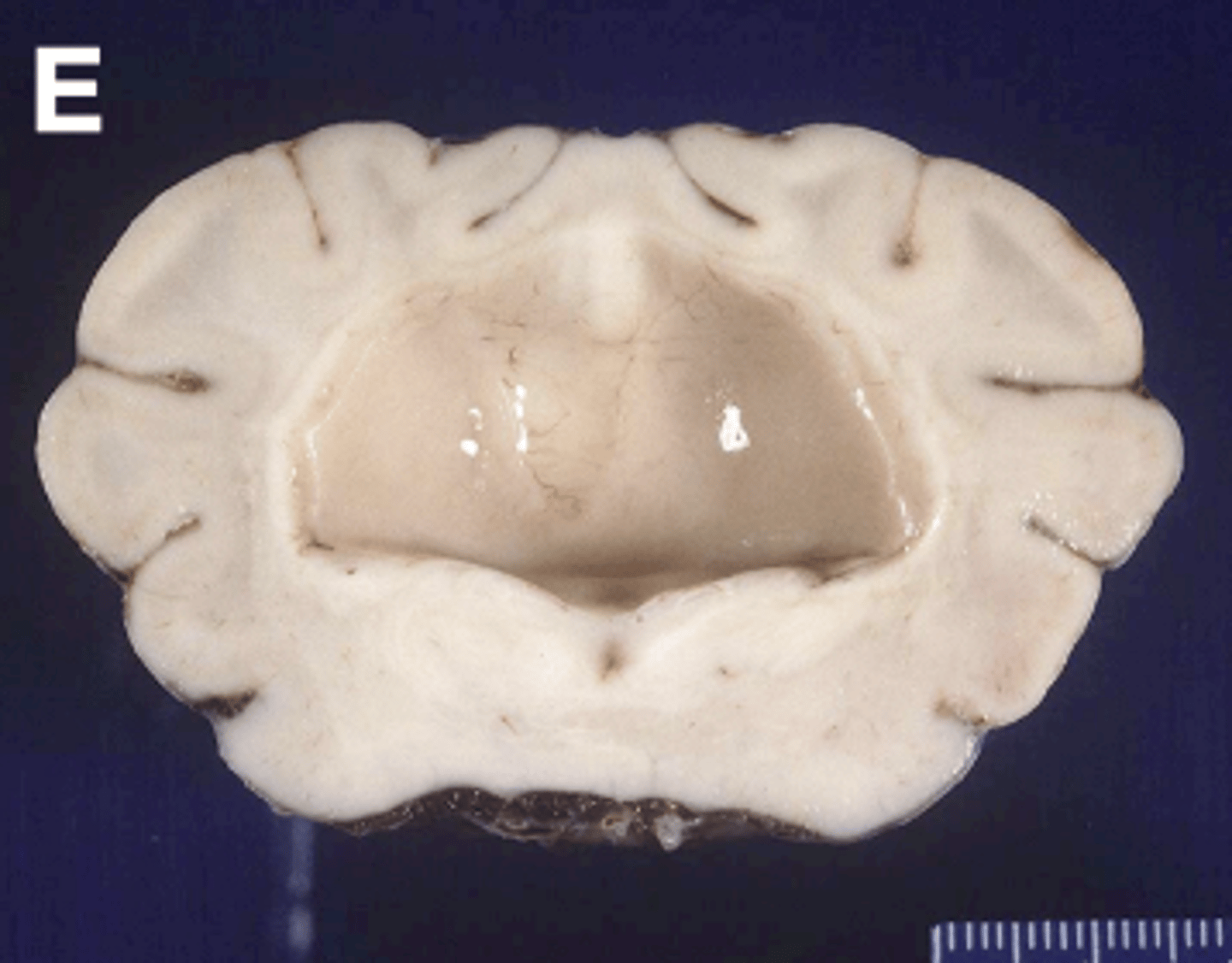
Hydrocephalus is very common in animals, and can be either ________________ or __________________ but is almost always due to what?
- Congenital
- Acquired
- Obstruction of CSF flow
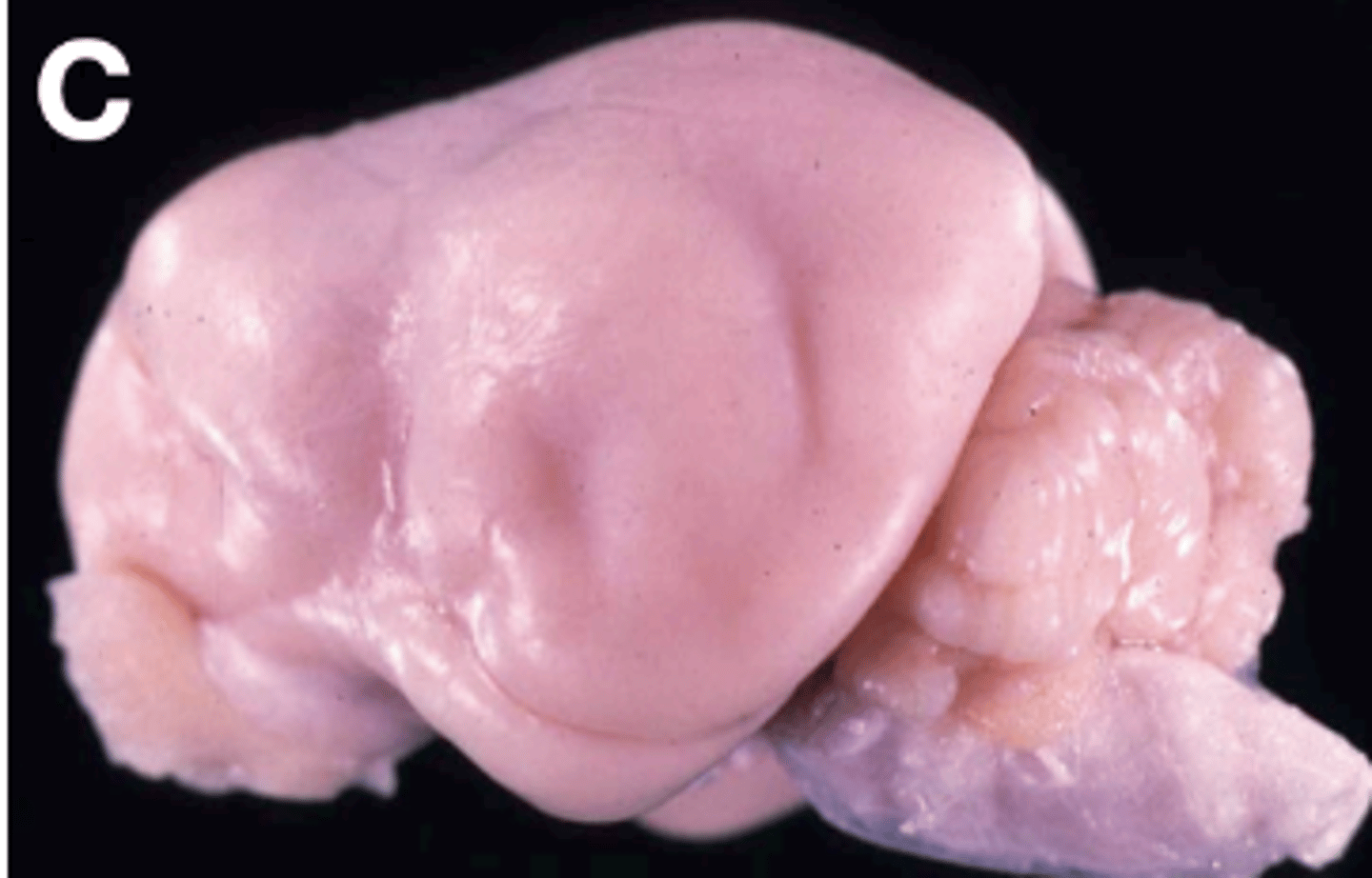
Describe the pathogenesis of congenital hydrocephalus. What is a common occurrence in conjunction with it?
- Due to malformation of the mesencephalic aqueduct resulting in obstruction.
- The skull is still growing, so associated craniofacial defects are common (domed head, open fontanelle, ventrolateral "sunset" strabismus; There may be other concurrent congenital defects
Congenital hydrocephalus is a common finding in what animals?
- Brachycephalic animals
Describe the pathogenesis of acquired hydrocephalus.
- Obstruction of the ventricular system by exudate or mass effect.
Is acquired hydrocephalus associated with craniofacial defects?
- No; It generally occurs in adults
Vertebral malformations in animals are often _____________, and occasionally ____________.
- Congenital
- Degenerative
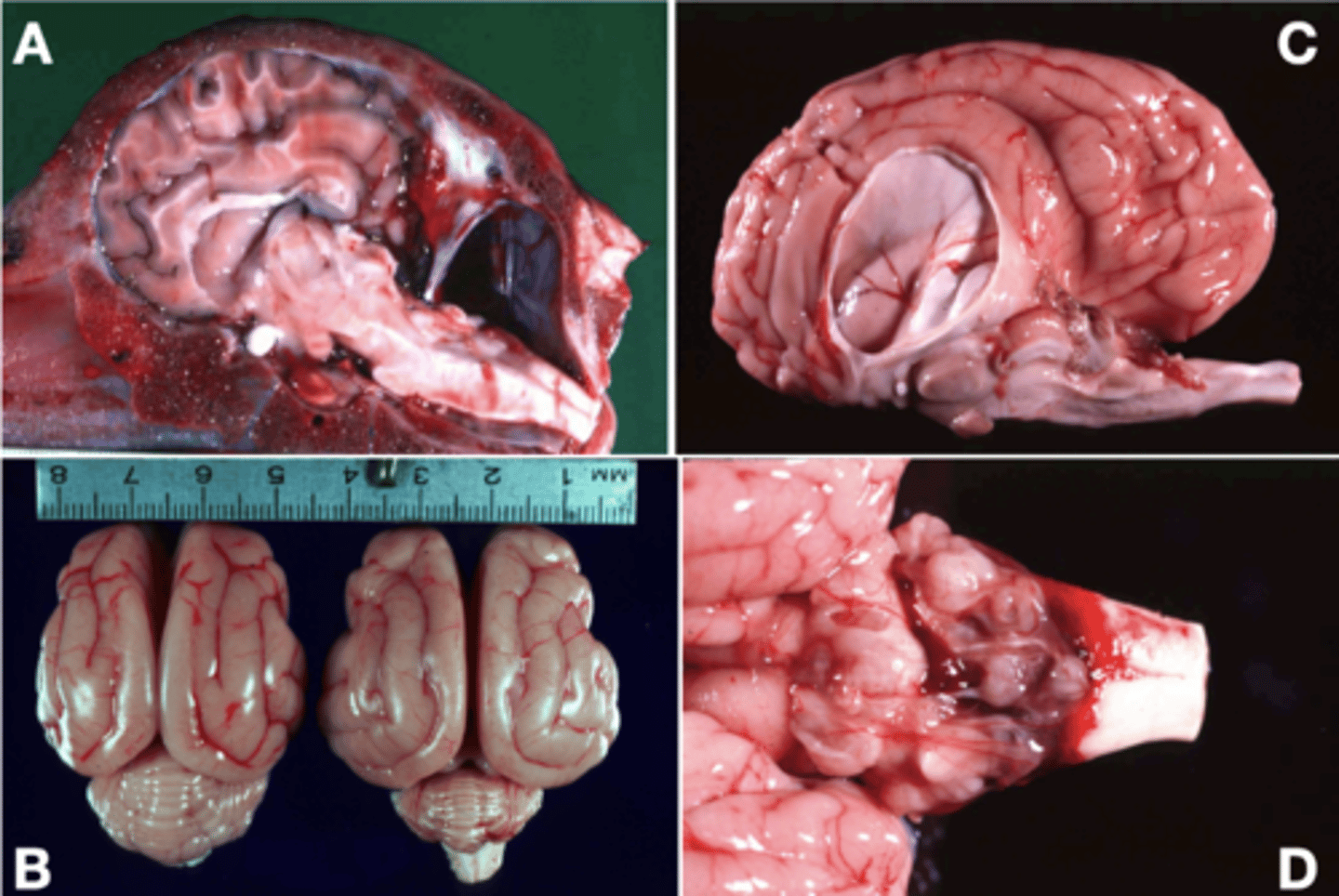
What are the most common/significant vertebral malformations in dogs and horses? Progressive spinal cord compression results in what?
- Static (constant compression)
- Dynamic (compresison only when the neck is bent)
- Progressive spinal cord compression results in degeneration of the cord
Vertebral malformations (static or dynamic) result from many different pathogeneses. What are some of them?
- Abnormally shaped vertebral bodies or occiput
- Fusion of vertebral bodies,
- Joint laxity or luxations
- Articular degeneration
What vertebral malformations do chondrodystrophic dogs tend to get?
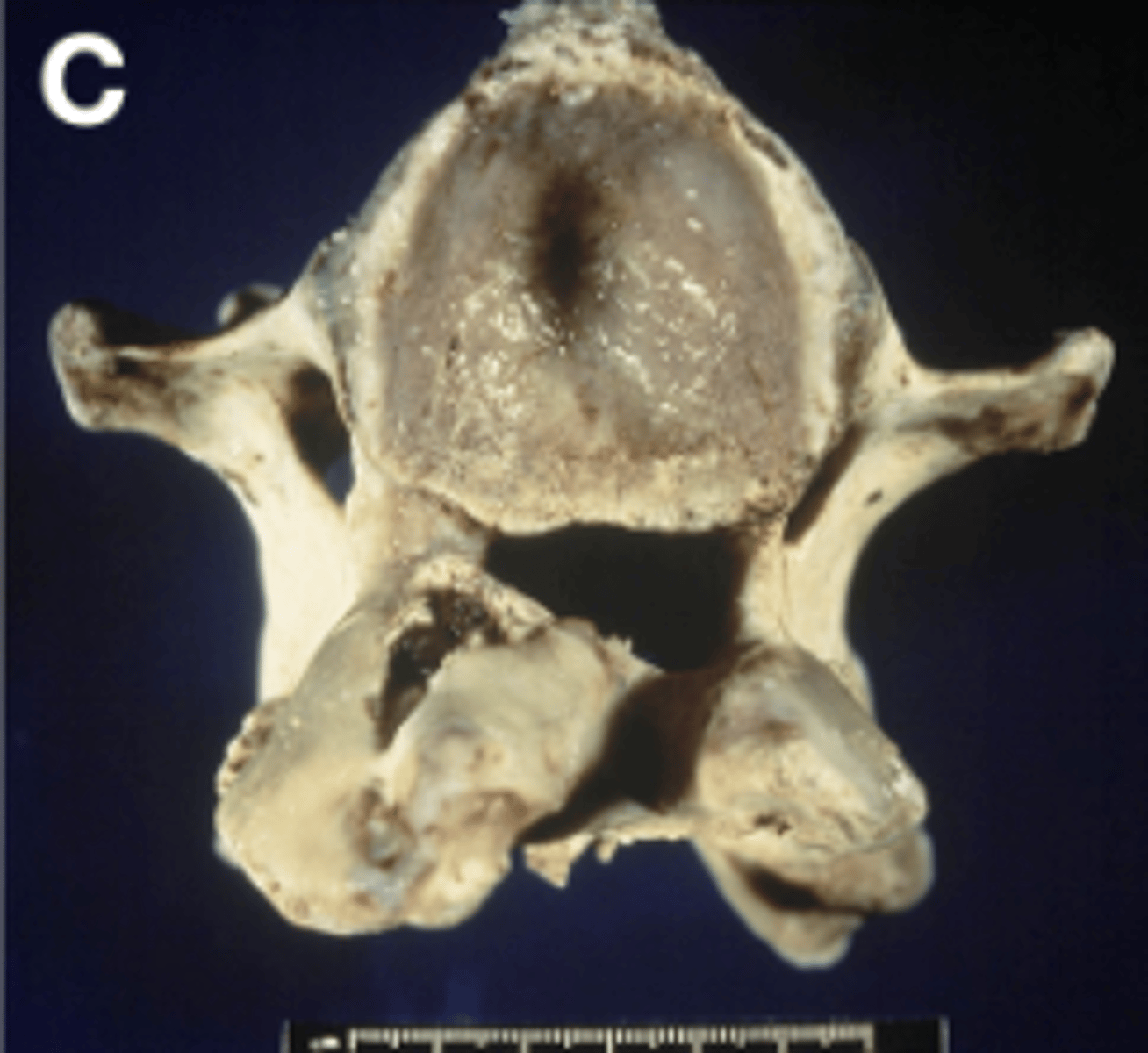
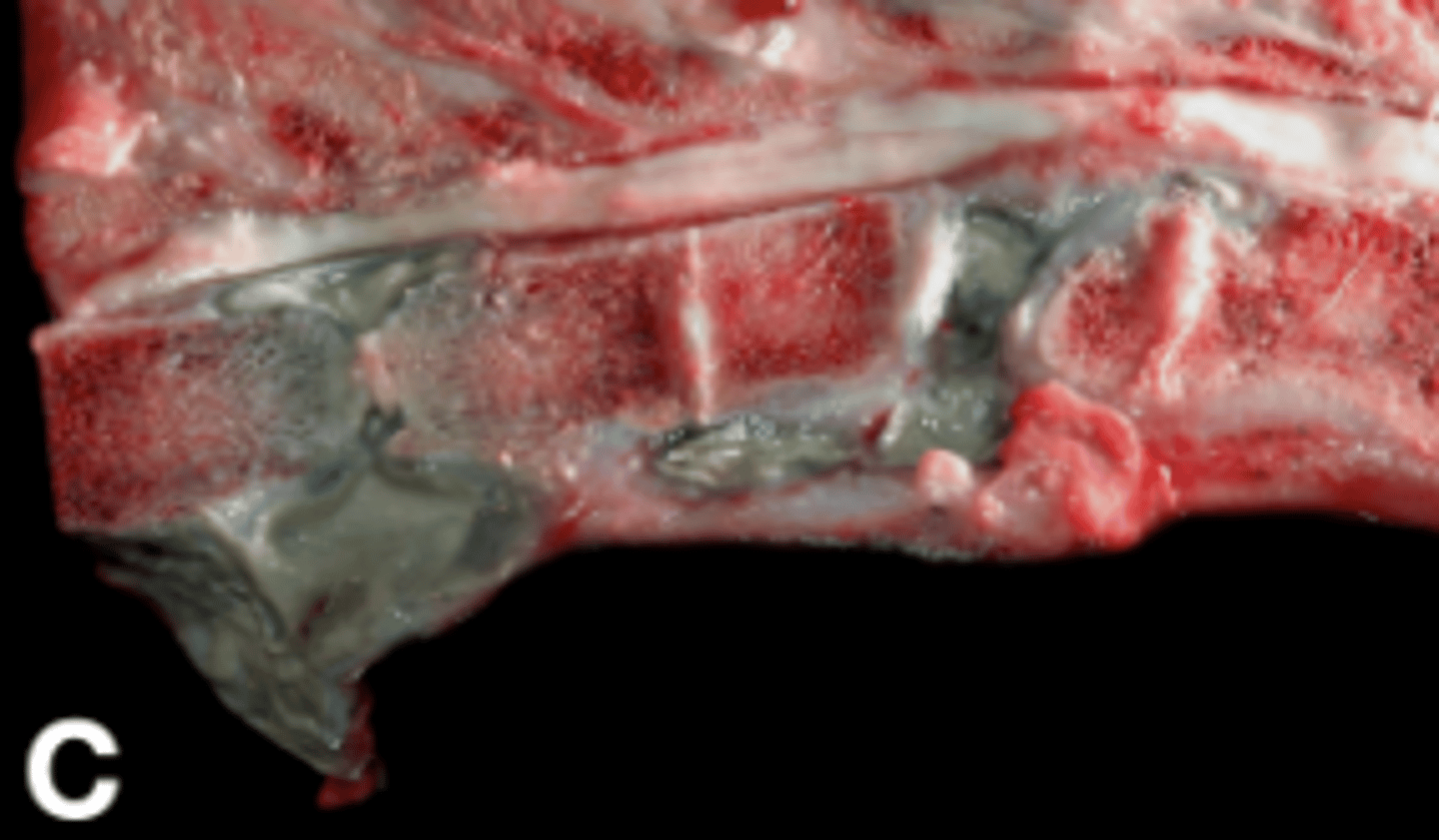
- Hemivertebrae (A) and block vertebrae
What vertebral malformations do Cavalier King Charles Spaniels tend to get?
- Caudal Occipital malformation ("Chiari-like" malformation) (C)
What is Wallerian Degeneration?
- Degeneration and partial dying back of an axon following focal axonal injury (such as that caused by spinal cord compression).
A neuron can survive loss of _____________, but not loss of _________________.
- Axon
- Cell body
What is necrosis? Describe its gross appearance.
- Selective death of specific cell types
- Tissue architecture is retained, so this is often not grossly visible.
Describe the relative susceptibility of CNS cells to necrosis.
- Neurons are highly susceptible > Olgodendria > Astrocytes > Microglia, vessels
What sort of insults can cause neuronal necrosis?
- Hypoxia, hypoglycemia, infection, toxicity, loss of stimuli or inputs (upstream or downstream), etc.
Describe the difference between primary and secondary demyelination in regards to whether the neuron survives.
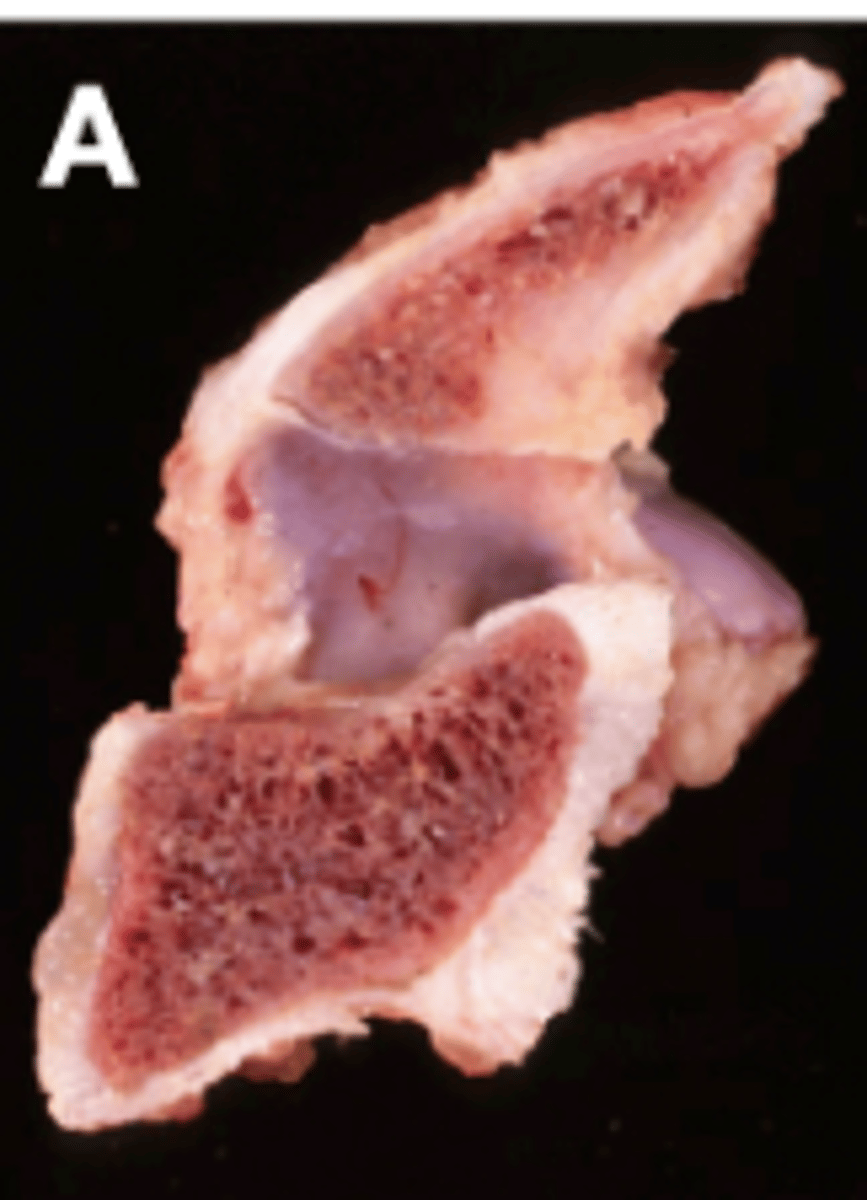
What is malacia?
- "Softening"; Pan-necrosis of all cell types (neurons and glia) which results in grossly visible softening or liquefaction o the tissue
The ___________ of malacia may give a clue to the etiology.
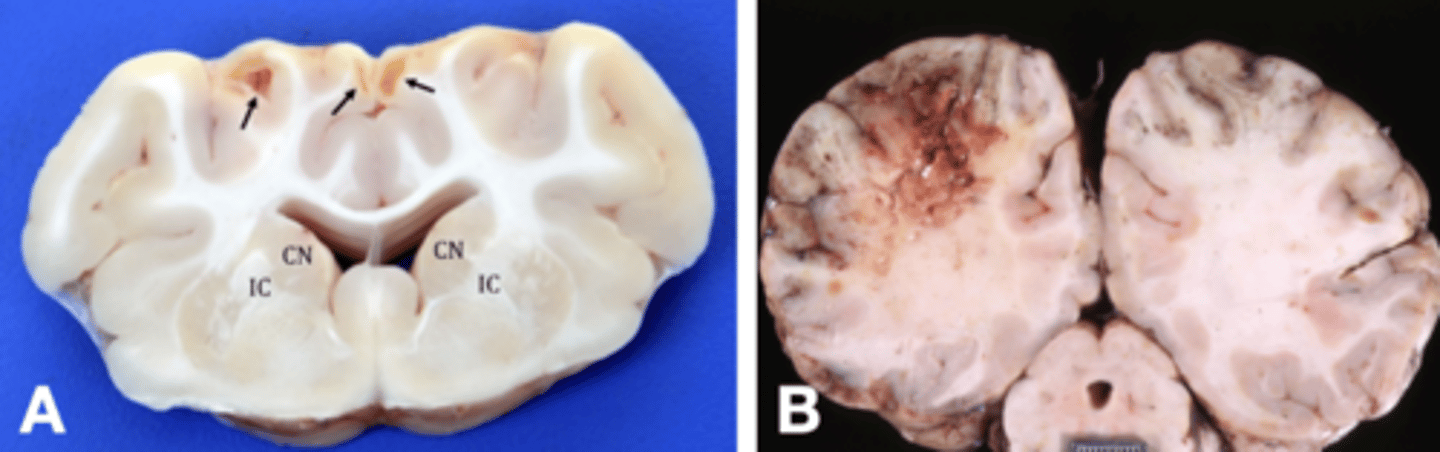
- Distribution (Polio vs. Leuko, encephalo vs. myelo, symmetric vs. non-symmetric)
Describe the commonality of malacia. What are some causes?
- One of the most common lesions of the CNS
- Nonspecific with many causes (bacterial or fungal infection, vitamin deficiency, toxin ingestion, ischemia, trauma)
Polioencephalomalacia occurs in ruminants due to what? Ocucrs in pigs due to what?
- Thiamine deficiency
- Salt toxicity
Leukoencephalomalacia occurs in horses due to what?
- Mycotoxin deficiency
What is primary demyelination? Include causes.
- Myelin loss surrounding intact axons due to abnormalities or loss of oligodendria (Viral, heritable, immune-mediated, nutritional, toxic)
What is secondary demyelination? Include causes.
- Death of the axon results in loss of trophic factors and secondary loss of myelin.
- Caused by anything that results in axonal loss (Trauma, malformation, disc disease, etc.)
Which is more common in animals, primary or secondary demyelination? Where does it occur?
- Secondary
- It occurs most often in the spinal cord where it accompanies Wallerian Degeneration.
What is the difference between primary and secondary demyelination in regards to whether the neuron survives?
- An axon can survive without myelin (primary), but loss of an axon will cause immediate disintegration of the myelin sheath (secondary).
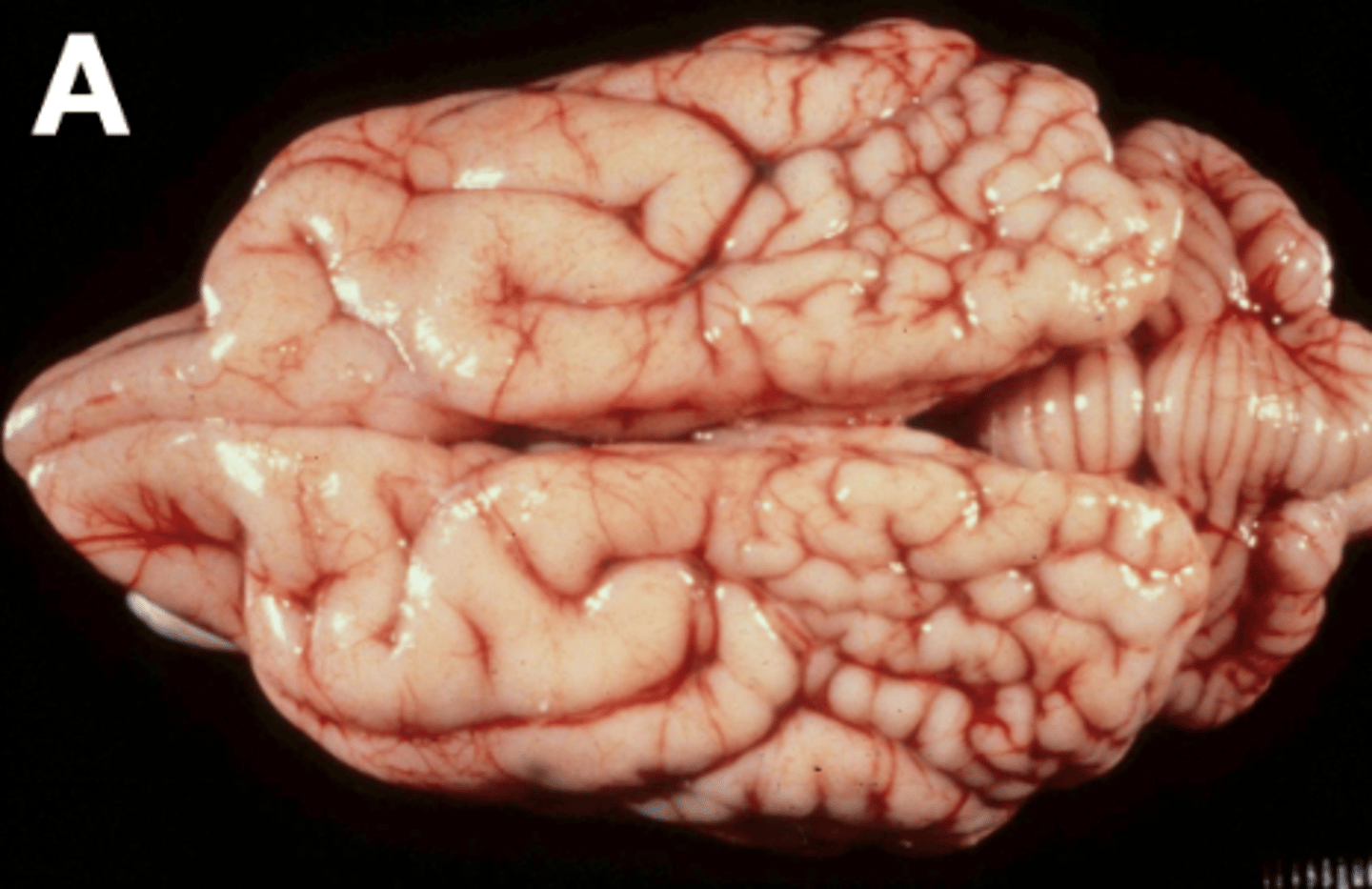
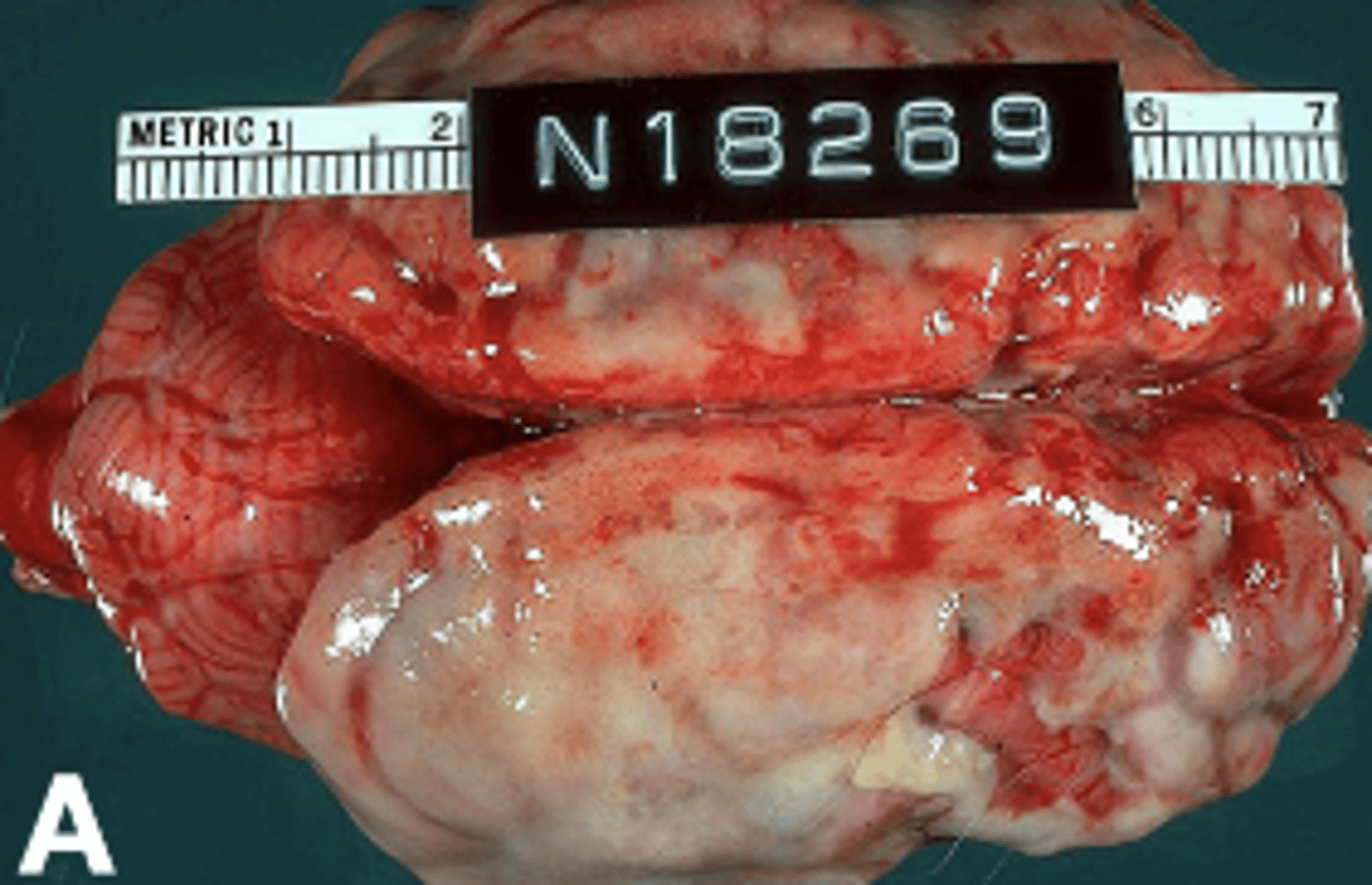
Inflammation of the brain results in increased what?
- Intracranial pressure
When inflammation of the brain is severe, it can result in what?
- Flattening of the gyri and herniation of parts of the brain
What are various forms of herniation of the brain?
- Cerebellum through the foramen magnum ("coning" of the cerebellum)
- Cerebrum through the tentorium cerebelli (Transtentorial herniation)
- Cerebrum across the falx cerebri (midline septum)
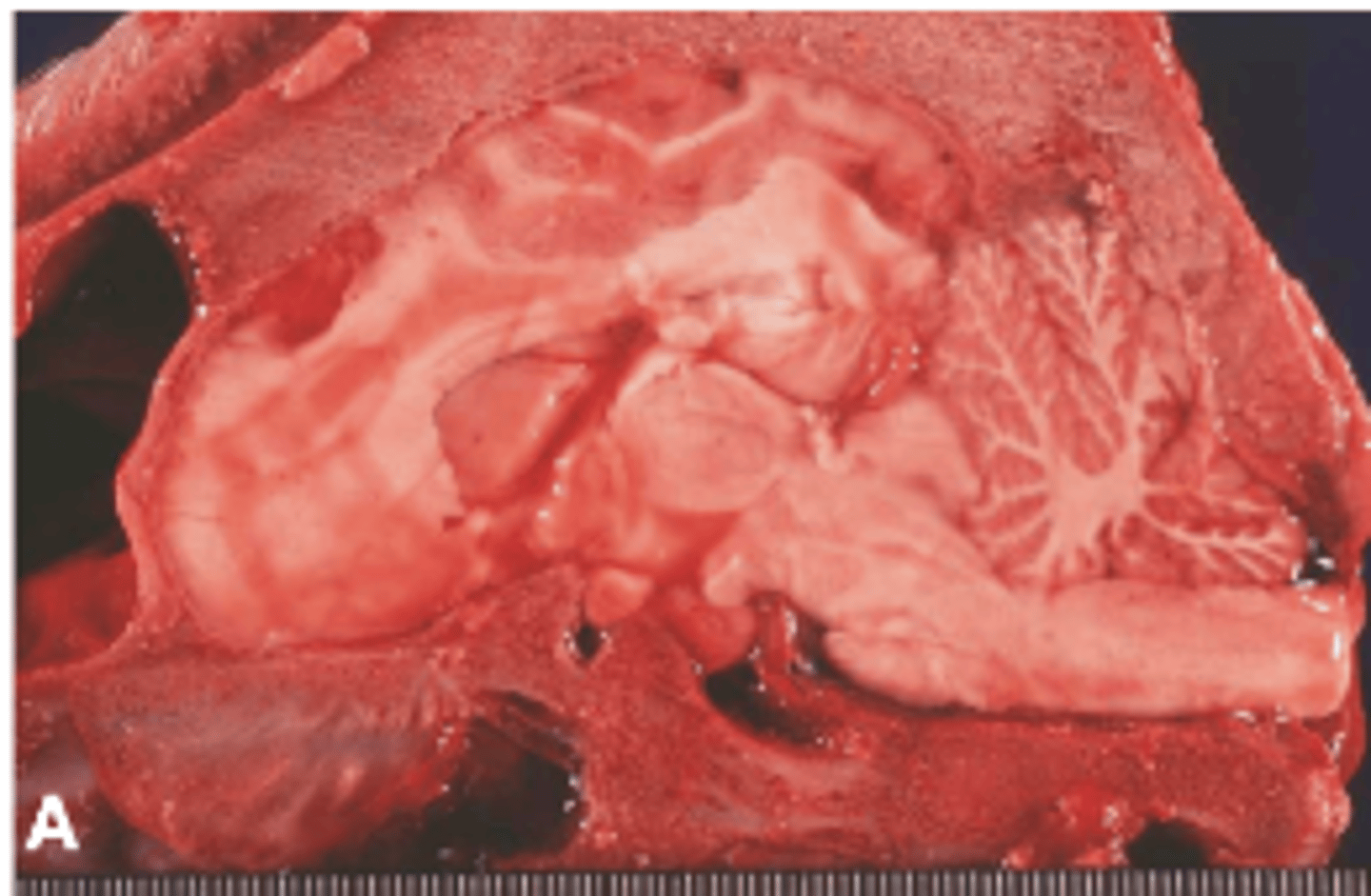
- Bacterial meningitis/meningoencephalitis is often _____________ and is most common seen in ___________ animals, especially ____________.
- Suppurative
- Septic
- Neonates
What lesions are observed with bacterial meningitis/meningoencephalitis?
- Malacia is common
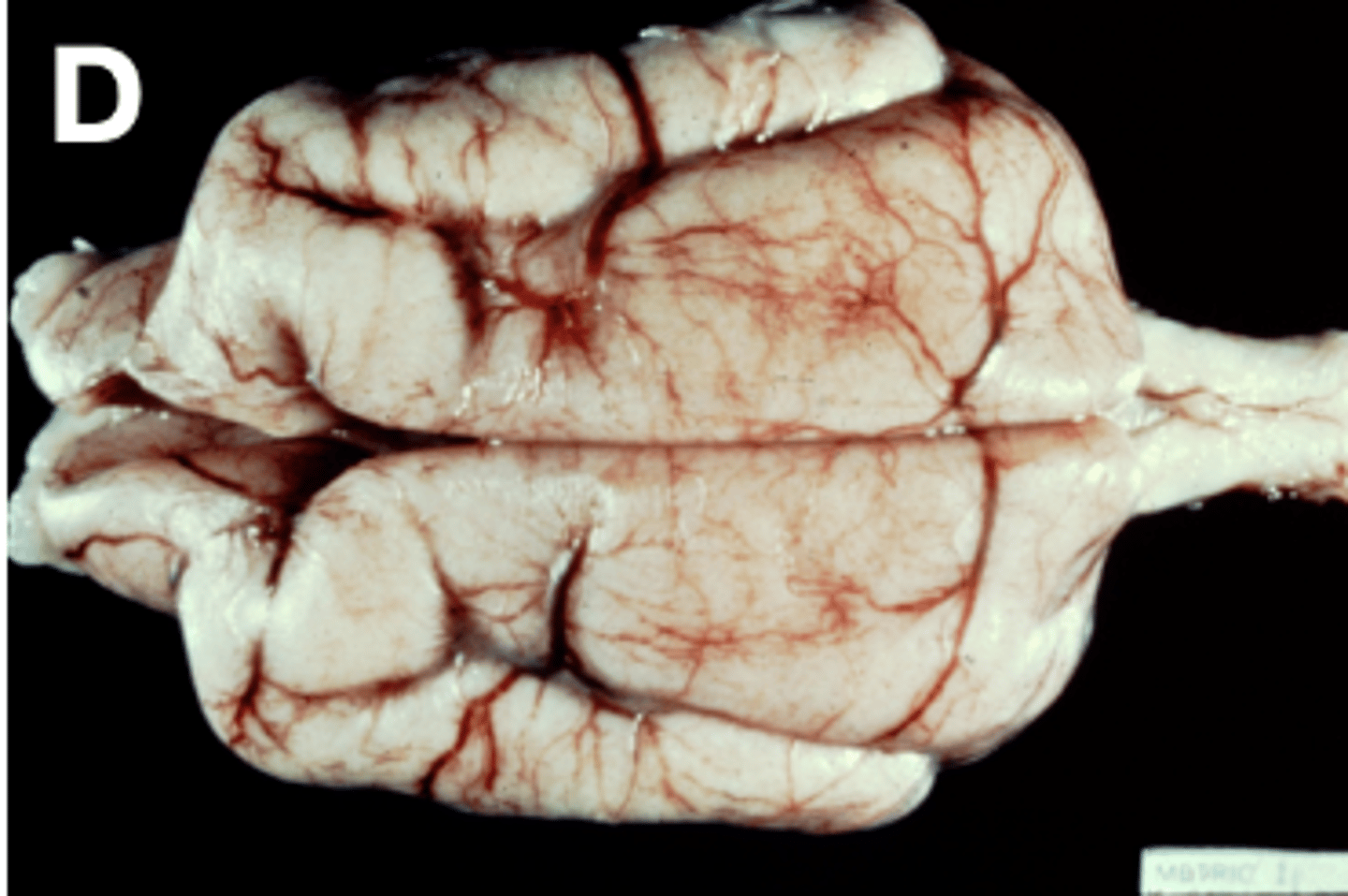
- Discospondylitis (C) (inflammation of the intervertebral discs and adjacent vertebral bodies) is often due to hematogenous bacterial infection
Viral encephalitis is usually ___________ and disease is ___________ apparent grossly. _______________ involvement is less common. What is an exception to this rule?
- Lymphoplasmocytic
- Rarely
- Meningeal
- Exception: FIP causes pyogranulomatous vasculitis, and often affects the CNS
Some viruses which cause viral encephalitis are associated with what?
- Persistent infections
- Congenital malformations
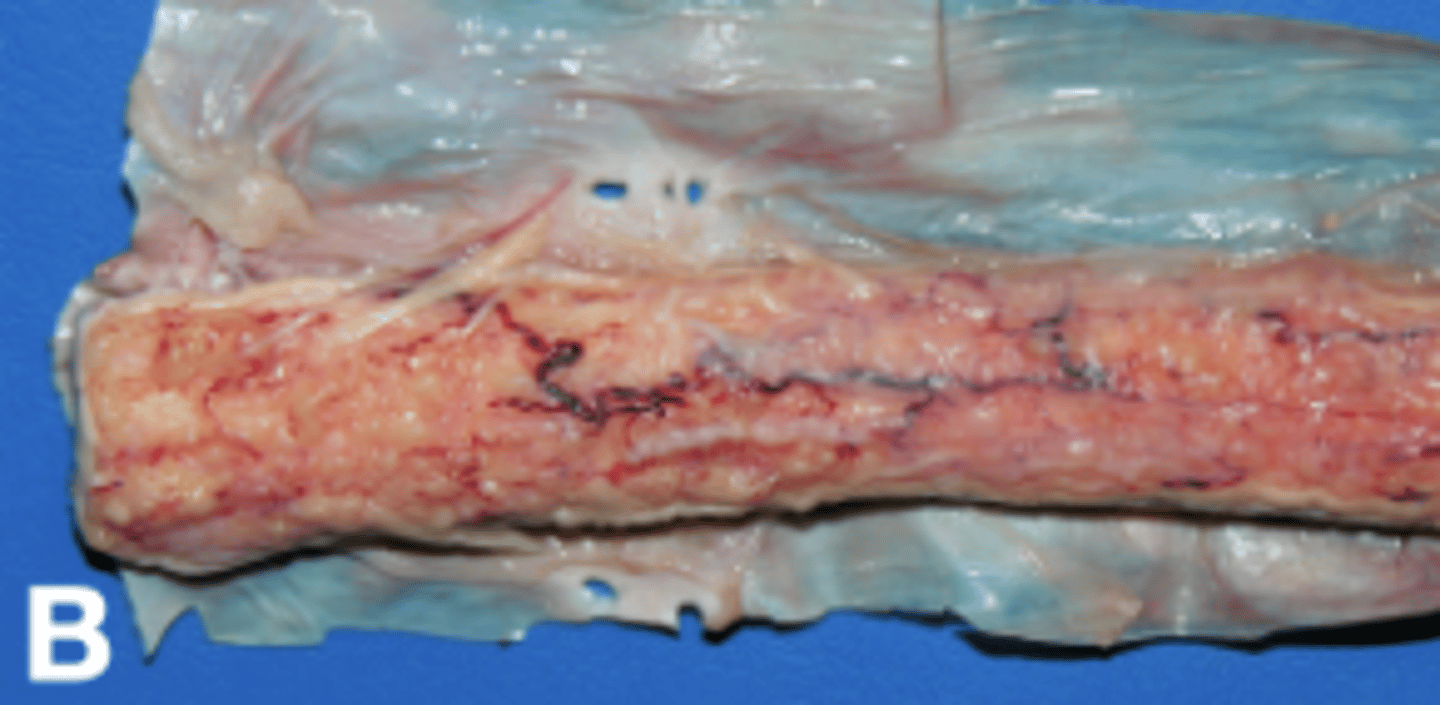
Fungal infections (and higher bacteria) usually result in ________________ to ________________ exudate (B). This may mimic _____________ grossly. ________________ patients are often at an increased risk.
- Granulomatous
- Pyogranulomatous
- Neoplasia
- Immunocompromised
Parasitism often results in _______________ or ____________ inflammation.
- Eosinophilic
- Lymphoplasmocytic
What is meningoencephalitis of unknown origin (MUE)?
- Umbrella term for multiple idiopathic breed-associated sterile meningitis syndromes in dogs, including Granulomatous Meningoencephalitis (GME)(D), necrotizing meningoencephalitis (NME), and others.
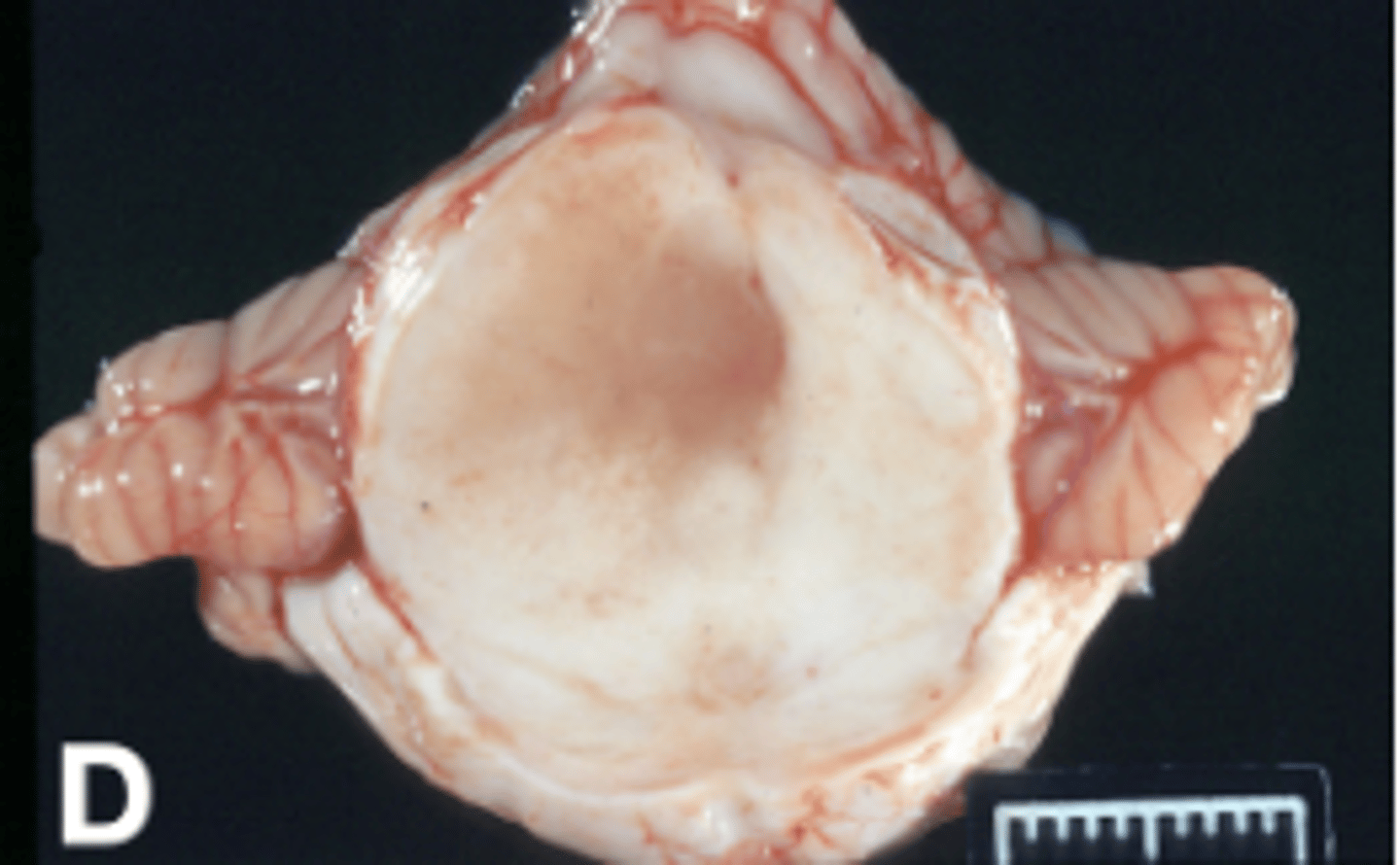
MUE is suspected to have an __________________________ basis. It may mimic ___________ grossly and on imaging.
- Autoimmune
- Neoplasia
What is the most important rule-out for neurologic mammals, especially if wild, unvaccinated, or there is history of human exposure (bite/scratch)?
- Rabies