32. Paediatric long bone diseases. Neoplasia of the bones. Aetiology, symptoms and therapy
1/49
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
50 Terms
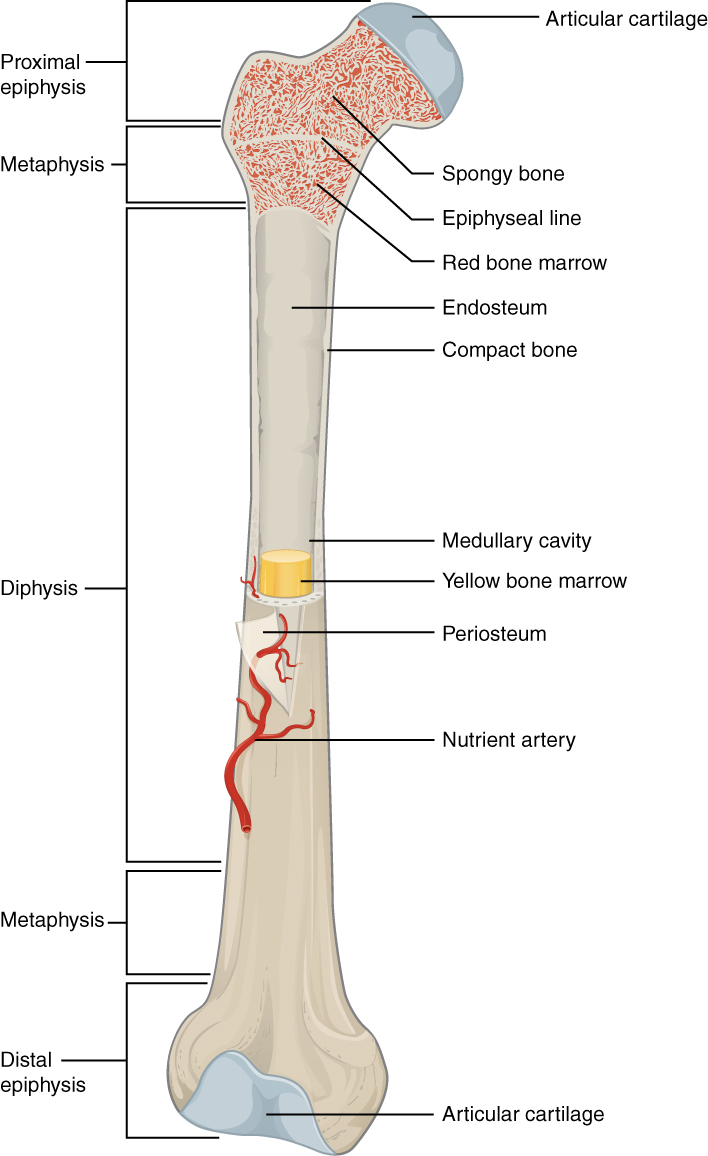
Periosteum (outer thin soft layer)
Endosteum (cortex, compact bone)
Cancellous bone (diaphysis, spongy bone)
Bone marrow (medullary cavity).
What are examples of paediatric long bone diseases?
Panosteitis juvenilis
Hypertrophic osteodystrophy
Junvenile osteodystrophy/nutritional secondary hyperparathyroidism
Legg-Calve Perthes disease (osteochondritis juvenilis)
Short radius/ulna
Aseptic inflammation of all structures of long bones. Self-limiting
What is the aetiology of panosteitis juvenilis?
Unknown (idiopathic). Infection, metabolic disease (protein rich diet, excess Ca), endocrine dysfunction, allergy, autoimmune mechanisms, parasitism & hereditary factors
Acute onset lameness, no trauma, recurrent bouts. Males are more commonly affected.
Palpation (pain), X-ray (blurred trabecular patterns at diaphysis), histopathology
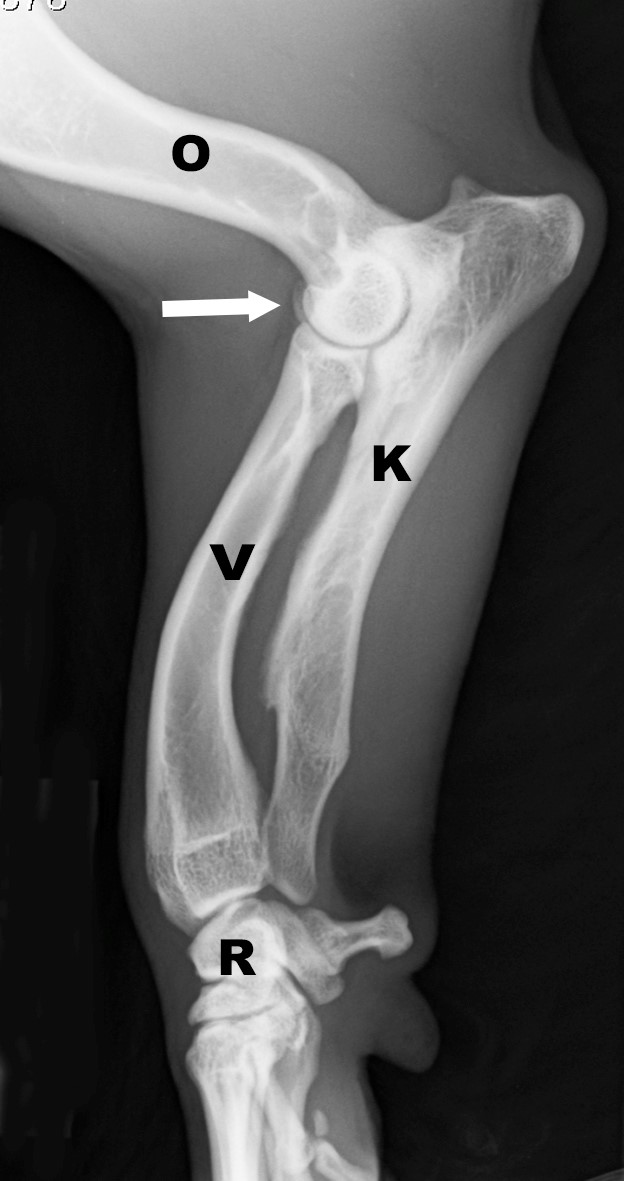
Syndrome of gross swellings in distal metaphysis of the radius, ulna, and tibia of young dogs.
What is the aetiology of HOD
Unknown, possibly vitamin C deficiency, infectious agents, obesity, inherited
Systemic involvement is common (pyrexia, anorexia, pain, arched back, reluctance to move), diarrhoea may be present. Cranial bowing of forelegs & valgus deformity of carpus is common to develop. (characterised by ↓ blood flow → failure of ossification → necrosis → inflammation of spongy bone).

History of acute lameness, fever, increased WBCs
X-ray (double physeal line, secondary extraperiosteal proliferation, calcification along the metaphysis)

Vitamin C, corticosteroids/NSAIDs, antibiotics (sometimes), supportive care (anti-diarrhoeals [loperamide], supportive fluids)
Most dogs recover in 7-10 days, but recurrent bouts are common
Nutritional imbalance (high phosphorus, low calcium e.g. red meat) leading to high PTH

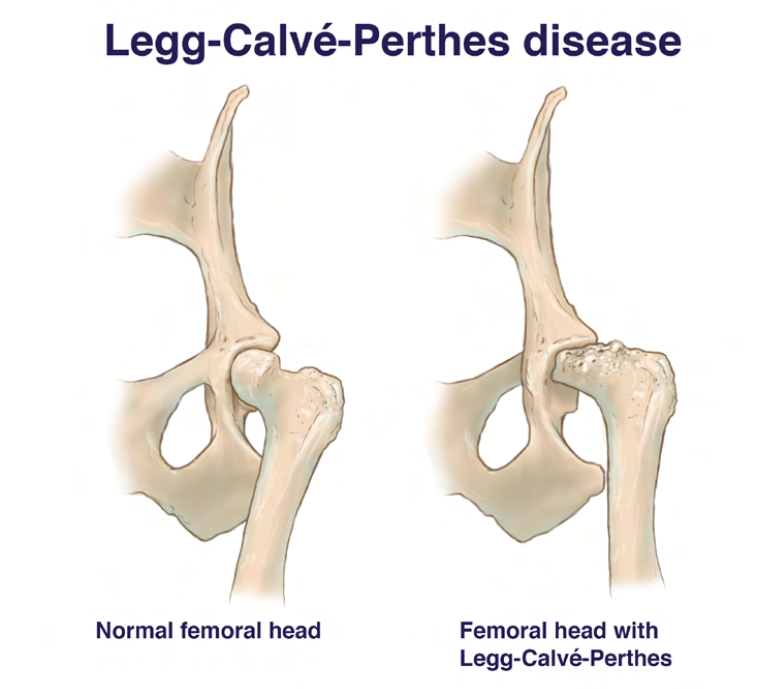
What is the aetiology of Legg-Calve Perthes disease?
Unknown, ischemia may be from vascular compression and sex hormone activity. Genetic cause (homozygosity of autosomal recessive gene) is proposed
What is the pathogenesis of Legg-Calve Perthes disease?
In all cases bone of femoral head & neck undergoes necrosis & deformation, during which animal manifests pain.
Fragmentation phase: Articular cartilage cracks as a result of collapse of subchondral bone.
Ossification phase: Formation of new bone in the necrotic area as part of the healing process, but femoral head & neck are deformed, with resulting joint incongruity & instability.
This condition leads to severe degenerative changes in the entire hip joint & development of marked osteoarthrosis.
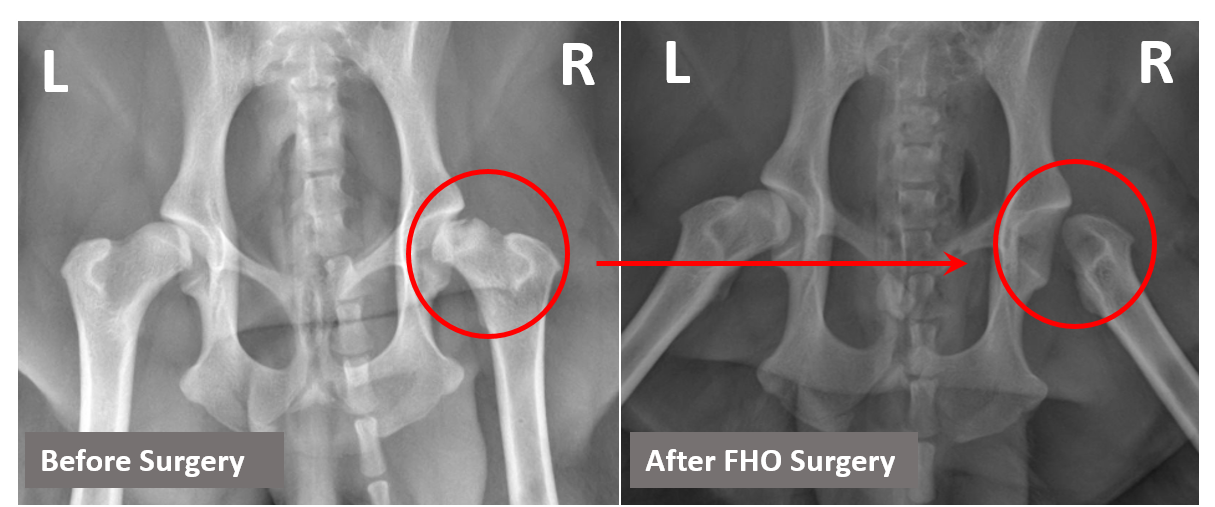
Pain (especially on abduction), crepitus, restricted range of motion, limb shortening, irritability, chewing at hip/flank, progressive lameness, stiffness, muscle atrophy (gluteus, quadriceps).
Lameness is gradual (over 6-8 weeks).
History, clinical signs, X-ray (radiopacity, lysis with apple-core/moth-eaten appearance)
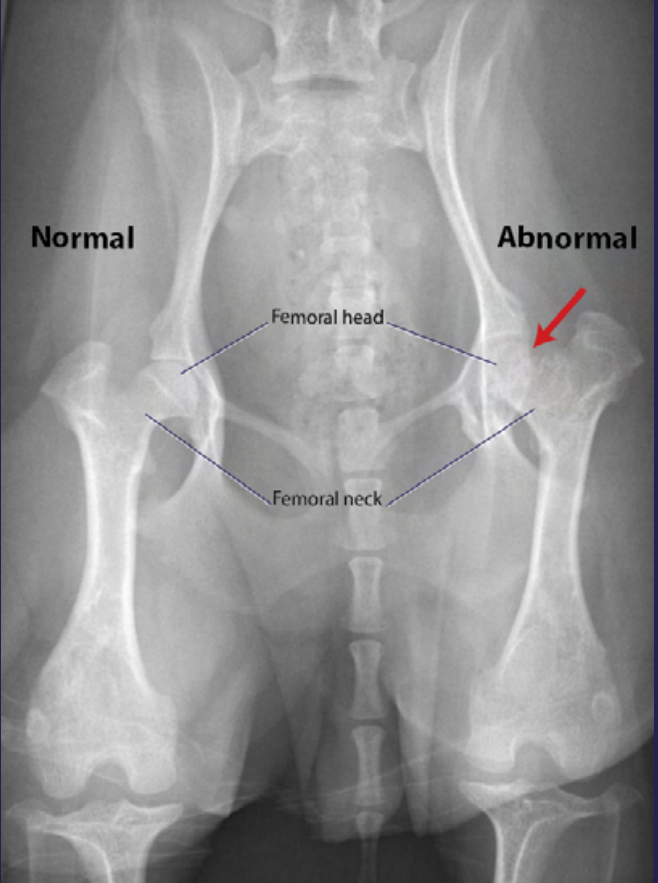
Capital physeal trauma, septic physitis, osteomyelitis, neoplasia, CCL rupture, patellar luxation
Short radius/ulna causing bending in the opposite bone
A metabolic disorder affecting bone growth
Viral disorders
Which metabolic disorders may cause short radius/ulna?
Secondary parathyroidism
Rickets
Hyperphosphatemia (dietary or renal) causing PTH release → bone resorption (Ca and P)
Haemorrhagic necrosis of medullary and endosteal elements in the metaphysis
What are characteristics of benign primary bone tumours?
May grow & cause issues, but are non-cancerous, do not metastasise
What are some examples of benign primary bone tumours?
Osteosarcoma, chondrosarcoma, fibrosarcoma
Mammary gland, lung, prostate, or local tissues (synovial cell sarcoma)
Soft tissue swelling, cortical destruction, lysis, periosteal reaction (sunburst appearance)
Local resection (if possible), amputation (most common), limb salvage procedures (endoprosthesis, allografts)
What is a likely diagnosis for a young dog with bone pain?
Growing pains
What is an example of an innovative treatment for osteochondrosis?
Stem cells