Exam 3: Motor Speech Disorders, Language, Higher-Order Functions
1/132
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
133 Terms
dysarthria
deficit in the control or EXECUTION of speech (related to strength, speed , range, accuracy of speech movements)
generally neurologic in orgin
can be categorized further into specific subtypes
apraxia of speech
deficit in PLANNING or programming speech movements
generally neurologic in origin
usually co-occurs with other conditions (aphasia or generic dysarthria)
flaccid dysarthria (what is it?, localization, neuromotor, etiology/cause of disease)
reduced ability to move —small, weak movements
localization/lesion: LMN (lower motor neuron)
injury or malformation of the LMN “final pathway” to the neuromuscular junction
neuromotor: weakness
etiology/cause of disease = NMJ disease, Mysathenia Gravis, MS, Bell’s Palsy
phrenic nerves
nerves involved in respiration are spread from the cervical through thoracic divisions of the spinal cord
control the muscles needed for breathing
innervates diaphragm 3-5th cervical segments
injuries to phrenic nerves —> can cause resp paralysis —> can lead to dysarthria
flaccid dysarthria clinical characteristics
clinical:
weakness (paralysis)
hypotonia
diminished reflexes
atrophy
fasciculation (spontaneous muscles contractions)
fibrillations (rapid, irregular heart rate)
flaccid dysarthria perceptual characteristics
perceptual:
hyper nasality
breathiness (continuous)
nasal emission
audible inspiration
short phrases
spastic dysarthria (what is it?, localization, neuromotor, etiology/cause of disease)
bilateral pyramidal UMN damage to pathways of CNS leading to LOSS OF INHIBITION
loss of skilled movements, reduced range of motion
localization: bilateral UMN
damage to the direct & indirect activation pathways+ pyramidal & extrapyramidal pathways
neuromotor: spasticity
etiology/causes of disease: Cerebral Palsy, infarcts of internal carotid/MCA/PCA, ALC, corticospinal or corticobulbar lesion
UMN: Pyramidal/Direct Pathways
consist of corticospinal & corticobulbar tracts
corticospinal = control of limbs/trunk; decussation at the pyramids of the medulla
corticobulbar = control of face, head, neck; decussation depending on CN
activation leads to discrete, skilled movements
lesions cause:
weakness, loss of skilled movements
babinski sign (loss of proper reflex, toes spread out instead of coming together)
UMN: Extrapyramidal/Indirect Pathways
major contributions from premotor areas
crucial connections with basal ganglia, cerebellum, retic form, vestibular nuclei
generally inhibitory— regulates reflexes for maintaining posture and tone
lesions cause:
spasticity (inc resist to stretch)
inc reflexes
weakness
what patterns result from lesions to UMNs?
pyramidal & extrapyramidal damage (UMN)
paralysis
loss of skilled movement
spasticity, loss of inhibition (specifcally extrapyramidal damage)
increased and/or pathological reflexes
spastic dysarthria clinical characteristics
clinical/non- speech characteristics:
dysphagia
excessive, slow facial expressions
pathological laughing and crying
drooling
facial posture fixed (unchanged)
partial smile
*damage from pyramidal tract; bilateral
spastic dysarthria perceptual characteristics
speech/perceptual characteristics:
harshness
imprecise consonants
low pitch
slow rate
strained-strangled quality
short utterances
pitch breaks
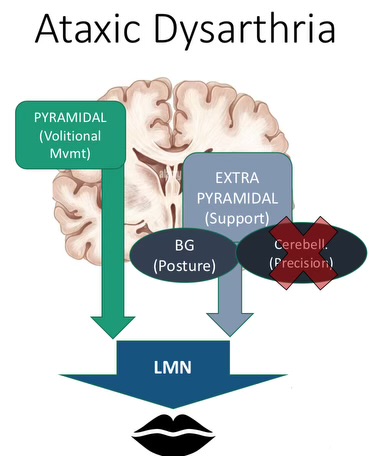
what is ataxia?
neurological condition characterized by the loss of coordination and control of muscle movement
due to damage in cerebellum
how does cerebellum modulate speech? how does damage to the cerebellum affect the body?
cerebellum:
coordinates skilled movement (speed, range of muscular movements)
part of the indirect pathway to LMNs (extrapyramidal support)
receives input from the body and cortex; acts as an error controller (provides to the cortex)
impacts of damage:
errors of force, speech, timing, and range —> difficulty in the coordination of movement
IPSILATERAL control
R cortex, L cerebellum, L side of body
L cortex, R cerebellum, R side of body
ataxic dysarthria
results from cerebellar control circuit dysfunction; errors in coordination
localization: cerebellum
neuromotor: incoordination
etiology/causes of disease: cerebellar hemorrhage, Anoxia, Multiple Sclerosis
ataxic dysarthria clinical characteristics
clincal (non-speech):
hypotonia (low muscle tone)
slow voluntary movements
jerky movements
wide-based gait
tremors
paucity of movement
muscular incoordination
impairments of equilibrium
ataxic dysarthria perceptual characteristics
perceptual characteristics:
slurring/stumbling over words (lack of error correction)
“drunk” sounding speech
irregular articulatory breakdowns
irregular vowel distortions
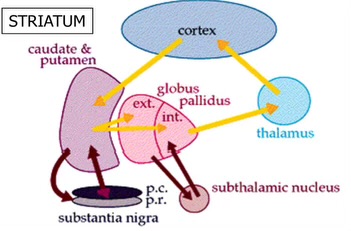
major inputs and outputs of the basal ganglia (circuit)
caudate & putamen: input from cortex, output to globus pallidus
globus pallidus: input from caudate & putamen, output to the thalamus
thalamus: input from globus pallidus, output to cortex
major features of Parkinson Disease
bradykinesia (slowness of movement; difficulty initiating movement)
postural instability
tremor
rigidity
cognitive deficits
hypokinetic dysarthria
hypokinetic dysarthria clinical characteristics
tremor at rest
rigidity “cogwheel”
bradykinesia (slow movements)
hypokinesia (small movements)
masked faces: loss of facial expression
akinesia (lack of voluntary movement)
swallow infrequently, drooling
dysphagia (difficulty swallowing food)
hypokinetic dysarthria perceptual characteristics/non-speech related
monopitch
reduced stress
monoloudness
inappropriate silences
short rushes of speech
increased rate overall
dyskinesia
a movement disorder characterized by involuntary, uncontrolled muscles movements (general term)
types of dyskinesia
hyperkinetic dysarthria
with etiologies of: athetosis, chorea, myoclonus
akinesia
inner sense of restlessness but lack of movement/freezing, difficulty initating movement
hypokinesia (dec amplitude or poverty of movement)
facial rigidity (stiffness in facial muscles)
delayed responses
ballism
movement disorder characterized by involuntary, flinging, and often violent movements of the extremities
large amplitude movements
flinging/ throwing movements
repetitive and varying
usually unilateral (affects one side of the body)
tremors
involuntary movement
rhythmic, oscillatory movement (shakiness, trembling)
tics
involuntary movements
sudden, brief, and repetitive movements or sounds (not necessarily rhythmic like tremors)
hyperkinesia
EXCESSIVE involuntary movements, characterized by an overabundance of muscular activity
(hypokinesia refers to decreased/reduced movements)
hyperkinetic dysarthria? perceptual characteristics?
associated with diseases of the basal ganglia circuit, cerebellar circuit, indirect (extrapyramidal) system
abnormal, rhythmic, or irregular and unpredictable (rapid or slow) involuntary movements
perceptual
visible abnormal orofacial, head, and respiratory movements
variable rate
inappropriate silences
excess loudness variation
prolonged intervals & phonemes expiration/inspiration
transient breathiness
etiologies/causes of hyperkinetic dysarthria
chorea (Huntington’s or non-Huntington’s)
tics
dystonias
myoclonus
Huntington’s Disease
one type of hyperkinetic dysarthria etiology
characterized by chorea, dementia
constant jerky movements, including facial movements, restless/fidgety hands
Chorea (not Huntington’s)
one type of hyperkinetic dysarthria etiology
“dance"- like purposeless, unpredictable movement
due to reduced GABA
multiple etiologies (Wilson’s Disease, Sydenham’s Chorea)
speech (excessive range of movement, sustained vowel fluctuations)
Gilles de la Tourette’s Syndrome
one type of hyperkinetic dysarthria etiology
example of vocal tics
brief involuntary movements or sounds that occur over a background of normal motor activity
simple or complex (simple or complex)
echolalia (repeating what is heard)
palilalia (compulsive repetition of phrases)
under partial voluntary control
dystonias (meige, oromandibular, spasmodic dystonia)
one type of hyperkinetic dysarthria etiology
slow hyperkinesia characterized by involuntary abnormal postures resulting from excessive co-contraction of antagonistic muscles
Meige Syndrome= oromandibular dystonia + forceful, spasmodic closure of the eyes
spasmodic dysphonia= focal dystonia with strained voice quality & stoppages
slow initiation of speech
palatopharyngolaryngeal myoclonus
abrupt RHYTHMIC unilateral or bilateral movements of the soft palate, pharyngeal walls and laryngeal muscles
(not like chorea which is more random)
speech:
intermittent hypernasality
tremor- like variations
momentary rhythmic arrests
athetosis
condition where muscle contractions cause involuntary writhing (twisting/squirming) movements of the limbs, neck, tongue and others muscle groups
inability to maintain a body part in a single position
damage to basal ganglia can cause which movement related diseases?
Parkinson’s Disease (HYPOkinesia)
Huntington’s Disease (HYPERkinesia)
flaccid dysarthria is due to damage in what area?
lower motor neuron (LMN)
spastic dysarthria is due to damage in what area?
upper motor neuron; pyramidal (volitional mvmt)
ataxic dysarthria is due to damage in what area?
upper motor neuron; extrapyramidal support (cerebellum)
unilateral upper motor neuron (UUMN) dysarthria
unilateral innervation = when one side of the brain controls one side of the body
(usually contralateral hemisphere of brain controls the opposite part of body)
BUT usually gets compensated by the unaffected side of the brain except for CNs controlling lower half of face
often UNDERDIAGNOSED because signs do not usually show with compensation from other side of brain; perceptual characteristics are not well-defined
frequently co-occurs with aphasia, apraxia of speech (planning of speech)
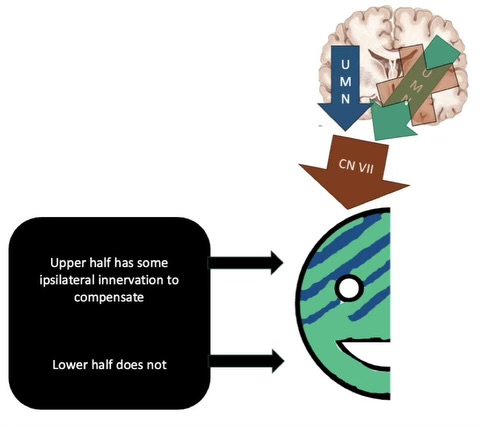
etiologies examples of UUMN dysarthria
vast majority etiologies are vascular (result of stroke)
focal lesions to unilateral UMN, occlusion of L or R carotid artery
UMN pathways
corticospinal
fibers originate from the cerebral cortex, cross at the medulla, and descend to the spinal cord (end destination)
CONTRALATERAL CONTROL
corticobulbar
fibers originate from the cerebral cortex, cross midline somewhere along the brainstem at the level of the CN they innervate
BILATERAL CONTROL (controls both sides of body)
what results in lesions to UMN systems (corticobulbar and corticospinal tracts)?
loss of fine, skilled movements
hemiplegia — paralysis of one side of the body
hemiparesis — weakness on one side of the body
atypical, increased reflexes
hypereflexia, Babinski sign
absent abdominal reflex
Mixed dysarthria
any combination of 2+ dysarthria types across 2+ dimension of the nervous system
important distinction for guiding diagnostics & treatment plans
etiology examples: ALS, multiple CVAs/strokes, TBI, other infectious/metabolic diseases
Amytrophic Lateral Sclerosis (ALS)
type of mixed dysarthria
UMN and LMN are affected
progressive loss of motor neurons
speech: flaccid-spastic dysarthria (spastic speech, flaccid resonance of speech)
wet, gurgled voice
strained- strangled
monopitch
hypernasality
Multiple Sclerosis (MS)
type of mixed dysarthria
demyelination of CNS white matter
speech: ataxic-spastic dysarthria
respiratory problems
may/may not have communication problems
Friedreich’s Ataxia
type of mixed dysarthria
hereditary (autosomal recessive)
speech: spastic- ataxic dysarthria
signs & symptoms= primarily spinocerebellar, cardiac problems are often the cause of death
Wilson’s Disease
type of mixed dysarthria
rare but important to recognize b/c its curable
inadequate processing of dietary copper
distinguishing sign= GOLDEN RING around cornea (Cu deposits)
speech: hypokinetic, spastic, and/or ataxic dysarthria (can manifest in many ways)
apraxia of speech
deficit in PLANNING or PROGRAMMING speech movements
localization: left hemisphere (dominant for language, even if left- handed)
impaired capacity to program sensorimotor commands for the positioning & movement of speech muscles
effortful trial-and-error groping with attempts to self-correct
aware that speech is not executed correctly
automatic + reactive speech is better than volitional/intentional speech
etiology: trauma, stroke, tumor that damages dominant (left) hemisphere structures involved in motor speech
problems that usually co-occur with apraxia of speech
majority (around 80%) have non-verbal apraxia (limb- apraxia) and aphasia
47% have dysarthria
what are the neural substrates for motor planning and programming?
left (dominant) hemisphere
broca’s area
premotor cortex
supplementary motor area
insula
controversy about developmental apraxia of speech (DAS)
uncertainties about the appropriate assessment + treatment protocols, characteristics of the disorder, and if it has a neurological basis
aphasia
an impairment of language (general term)
affect production and/or comprehension
can affect any modality— speaking, reading, writing, auditory, comprehension
due to injury to the brain
dysphasia
congenital/developmental language problem
alexia
impaired reading
agraphia
impaired writing
paraphasic errors
sounds or words are replaced by substitutions so that desired response is only approximated
literal/formal/phonological= incorrect or incomplete phonemes (grass is g_een)
verbal= incorrect words (grass is blue)
semantic paraphasia — the substituted word is related to the intended word (I spent the day working on the computer, i mean TV)
remote paraphasia — the substituted word is, at most, distantly related to the word (You forgot your musketeer, I mean, umbrella)
etiologies/causes of aphasia
#1 etiology: cerebrovascular accident (CVA) = stroke (ischemic or hemorrhagic)
traumatic brain injury (TBI)
tumors
3 parameters used to categorize aphasia
ability to produce (fluency)
ability to comprehend
ability to repeat
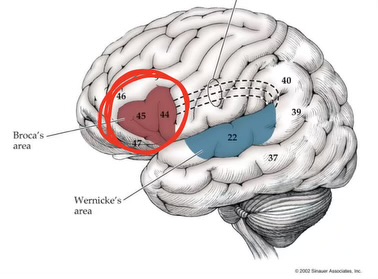
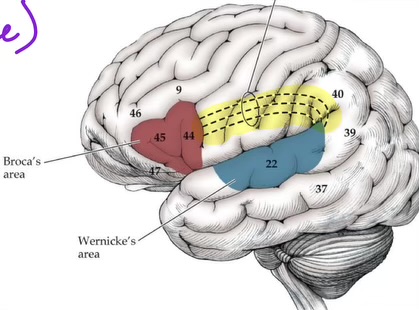
Broca’s Aphasia
non- fluent speech, can comprehend, does not repeat
reduced verbal output
mostly content words
restricted vocab
not a lot of function words
lesion: broca’s area, anterior perisylvian , insular cortex
awareness of impairment can lead to depression
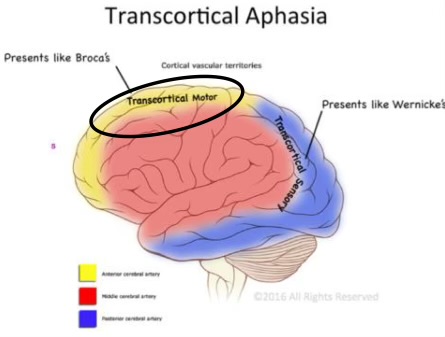
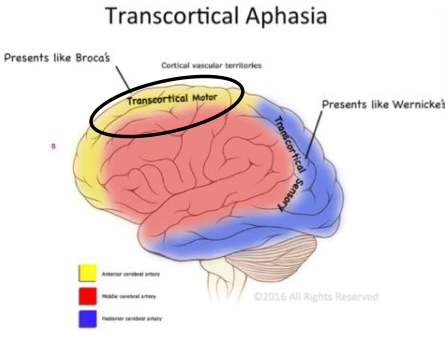
transcortical motor aphasia
non-fluent, comprehends, repeats
limited speech output & syntactic errors (not as severe as Broca’s Area)
lesion: frontal lobe (anterior to Broca’s area)/ supplementary motor cortex
global aphasia
non-fluent, doesn’t comprehend, doesn’t repeat
severe impairment in all modalities (speaking, listening, reading, writing)
restricted vocab, no understanding in any modality, no ability to communicate
lesion: middle cerebral artery which causes frontal-temporal-parietal lesion
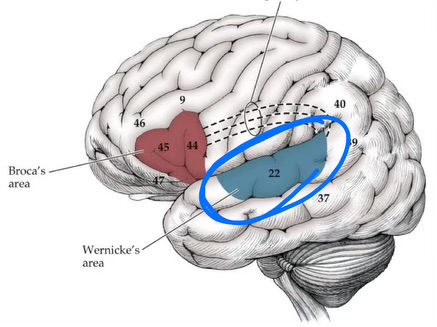
Wernicke’s Aphasia
fluent, does not comprehend, does not repeat
fluent but still paraphasic verbal output (naming difficulty, not as severe as Broca’s)
impaired auditory comprehension + impaired repetition
most common etiology/lesion: infarct to the inferior division of the middle cerebral artery
transcortical sensory aphasia
fluent, doesn’t comprehend, repeats
auditory comprehension is relatively poor
repetition is intact
fluent, well articulated speech
naming impaired
lesion: left posterior temporal- occipital lobe
transcortical mixed aphasia
not fluent, doesn’t comprehend, repeats
comprehension is severely impaired + no purposeful speech output
may have echolila (repeats heard phrases)
lesion: Broca’s + Wernicke’s area are spared, but damage to surrounding frontal, temporal, and parietal lobe
conduction aphasia
fluent, can comprehend, impaired repetition
may or may not have reading and writing deficits
lesion: left arcuate fasciculus, superior temporal regions, or supramarginal gyrus
anomic aphasia
fluent speech, can comprehend, can repeat
difficulty in naming and word retrieval
aud comprehension, reading, and writing are intact
lesion: temporal or parietal lobe, usually associated with focal trauma (specific location)
subcortical aphasias
related to the site of lesion; disrupts connections to and from language areas of the cortex
anterior subcortical aphasia
head of caudate, anterior putamen (basal ganglia)
non-fluent (with dysarthria), mild deficits with naming + aud comprehension
thalamic aphasia
damage to dominant thalamus
fluent with paraphasic errors, intact comprehension
progressive aphasia
due to neurodegenerative processes
primary progressive aphasia
word finding and naming issues
many variants, depending on language modalities that are impaired
issues with the classical model (of aphasias)
oversimplified
most ppl with aphasia have problems with all modalities of language, regardless of aphasia type
patients don’t all fit the “classical models”
neuroimaging shows
syndromes don’t map well onto lesions
alexia with agraphia
lesion: left inferior parietal lobule (supramarginal and angular gyri)
cannot read or write
overlaps with wernicke’s aphasia and evolves during recovery
alexia without agraphia (pure alexia)
lesion: left posterior cerebral artery (PCA) territory
patients can write, but not read what they have written
often accompanied by visual field deficit and inability to name colors
5 higher level functions of the brain
1) perisylvian network= language
2) parietofrontal network= spatial cognition
3) occipitotemporal network= face and object recognition
4) limbic network = retentive memory
5) prefrontal network= cognitive and behavioral control
language
symbolic representation of thoughts
spoken, written, and signed
language dimensions
phonology= rules of how the SOUNDS of language are organized (ex: ks sound only occurs in middle or end of word, not in the beginning)
morphology= rules governing how words are FORMED (ex: grammatic endings change meaning/diff tenses)
semantics= rules governing the MEANING of words and combinations (ex: knowing the diff b/w a pen and pencil)
syntax= rules abt how words are combined to form SENTENCES (proper grammar in a sentence)
pragmatics= rules abt the use of language in CONTEXT (ex: knowing to take turns in a convo)
what side of the brain is generally associated with language specialization?
left (for most people)
but language lateralization can change after injury
what is the categorical and representational hemisphere?
dominant + non-dominant hemispheres have been replaced with complementary specialization
CATEGORICAL hemisphere— usually LEFT
sequential- analytic processes (language + analytic reasoning)
functions: verbal ability, fast temporal processing, details
REPRESENTATION hemisphere — usually RIGHT
visuospatial relations (recog of faces, musical themes)
functions: musical ability, emotional recognition, abstract language
Broca’s Area
formation of words
ordering of words
output for spoken language
Wernicke’s Area
involved in word comprehension (receives fibers from visual cortex + aud cortex)
surrounds primary aud cortex
arcuate fasciculus
AKA conduction area
connects Wernicke’s area to Broca’s area (white matter tract)
important for REPEATING and SPEAKING a written word
Exner’s Area
writing output pathway
above broca’s area
broca’s area organizes signals from posterior language areas —> relays them to exner’s area
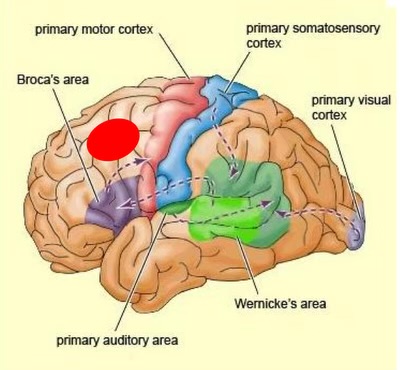
visual word form area
processes the word as a whole
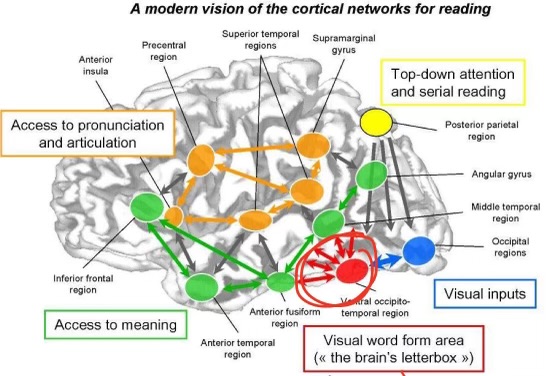
angular gyrus
perception of written language, as well as other language processing functions
adjacent to visual receptive areas
lesions can result in impaired reading (alexia) + writing (agraphia)
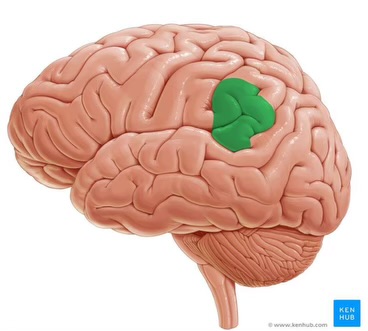
what cognitive functions are affected by lesions to frontal lobes?
executive functions, working memory, planning, inhibition/impulse control, speech production (Broca’s Area)
insula
beneath the lateral fissure (where temporal, parietal and frontal lobes come together)
function:
relays somatosensory info
planning and coordinating speech/language + swallowing
higher order functions
language
attention
memory
visuospatial functions
executive functions
mathematical functions
social cognition
reasoning
problem-solving
critical thinking
lateralization of brain functions
left hemisphere
fast temporal processing
details
verbal ability + language
praxis + skilled motor function
right hemisphere:
spectral processing; acoustic pitch
visuospatial attention + analysis
emotional recognition
localized functions
lesions affecting the frontal lobes and their connections impact executive functions (ex: attentional control, declarative learning)
lesions on the mesial temporal lobes affect declarative learning
lesions on subcortical structures (cerebellum + basal ganglia) can affect non-declarative learning
lesions affecting the thalamus can affect sustained attention
limitations of functional localization
neurons are highly interconnected
brain is incredibly plastic in health and disease (localiz wouldnt be that accurate)
brain functions are highly interdependent
what cognitive functions are affected by lesions to mesial/medial temporal lobes?
new long-term, declarative memories, emotional processing, language
what cognitive functions are affected by lesions to basal ganglia and cerebellum?
basal ganglia= regulating movement, planning/sequencing, motivation/reward
cerebellum= motor coordination, language/speech, visual-spatial memory
what cognitive functions are affected by lesions to thalamus?
sensory integration, memory (episodic memory b/c connects to hippocampus), regulation of attention
four features that brain disorders tell us about healthy brains
localization of cognitive functions
shown by analyzing lesion sites
different regions of the brain are specialized for different functions)
onset and clinical course of the brains’s capacity to adapt to changing circumstances
individual variability in symptoms and outcome
recovery and neuroplasticity in health and disease
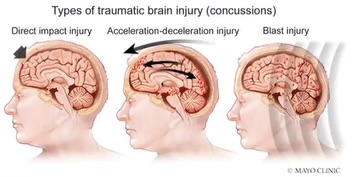
coup-contrecoup
type of TBI
injury to one side of head (i.e during fall) or injury to opposite side of head as the brain hits against opposite side of injury
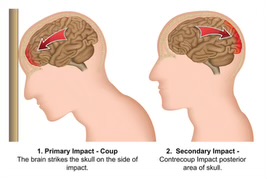
acceleration/decelertion
a sudden stop causes head to go forward and then back, as in a car accident
edema
type of brain injury
swelling of brain tissue; causes pressure
hemorrhage
type of brain injury
rupturing of blood vessels
focal injury/lesions
type of brain injury
lesions just beneath the point of direct impact
sheering
type of brain injury
twisting of axons that causes trauma & diffuse white matter/axonal injury
Complications associated with TBI
polytrauma (other body parts also affected)
emergent care (life-threatening)
medications
cognitive issues
behavioral issues