yang - calculations and dosing
1/9
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
10 Terms
BSA calculation

chemotherapy in obese patients
use actual body weight to calculate cytotoxic chemotherapy (IV and oral dose regardless of obesity status
no evidence that short- or long-term toxicity is increased with full weight-based doses
in pts receiving chemotherapy dosed on the basis of actual body weight, myleosuppression is the same or less pronounced in obese pts with cancer than in non-obese pts
chemotherapy dosing in children
traditional dosing of chemotherapy agents is based on BSA
EXCEPTION: infants — “little sacks of water”
body weight best approximates blood flow to major organs of elimination
chemo dosing in infants
goal dose per keg (actual body weight), NOT dose per m2
to convert a dose/m2 to a dose/kg, divide the dose/m2 by 30
this equation assumes a 30 kg child is 1 m2
carboplatin dosing
carboplatin dose (mg) = target AUC (mg⋅min/mL) x [GFR (mL/min) + 25 (mL/min)]
limitations:
small number of patients (men, non-obese)
measured GFR vs calculated GFR
Consider using ethylene diamine tetraacetic acid (EDTA) or a 24-hour urine to measure CrCl (not a serum creatinine-based mathematical equation) when dosing at an AUC greater than 6 or when using an un-capped CrCl.
Cockcrof-Gault Equation (CrCl calculation)
usually cap GFR at 125 mL/min with normal renal function (max dosing)
pts with abnormally low serum creatinine (Cr), including elderly or cachectic pts —> considering using a minimum CrCl of 0.7 mg/dL to avoid overestimation of CrCl
overweight or obese patients
BMI ≥ 25kg/m2 - Recommend using an “adjusted BW” rather than actual body weight
Adjusted body weight (kg) = ideal body weight (IBW) + 0.4 x (total body weight [TBW] – IBW)
BMI < 25kg/m2 – Recommend using actual weight
![<ul><li><p>usually cap GFR at <strong><u>125 mL/min</u></strong> with normal renal function <strong><u>(max dosing)</u></strong></p></li><li><p>pts with abnormally low serum creatinine (Cr), including <strong>elderly or cachectic pts</strong> —> considering using a <strong>minimum CrCl of 0.7 mg/dL</strong> to <u>avoid overestimation of CrCl</u></p></li><li><p>overweight or obese patients</p><ul><li><p><strong>BMI ≥ 25kg/m<sup>2</sup> </strong>- Recommend using an <strong>“adjusted BW” </strong>rather than actual body weight</p><ul><li><p>Adjusted body weight (kg) = ideal body weight (IBW) + 0.4 x (total body weight [TBW] – IBW)</p></li></ul></li><li><p>BMI < 25kg/m<sup>2</sup> – Recommend using actual weight</p></li></ul></li></ul><p></p>](https://knowt-user-attachments.s3.amazonaws.com/87c617e5-ff49-4914-b229-40fe2ed95a68.png)
infusion volume
V = rate x time
maintenance hydration
Calculation of daily fluid requirements for children/adults based on body weight or BSA
In the hospital, children are given hydration at a rate designed to meet their maintenance requirements
Frequently ordered as “IV + PO”: RN tracks how much the patient drinks and supplements with IV hydration as needed to make the total fluid intake = their maintenance rate
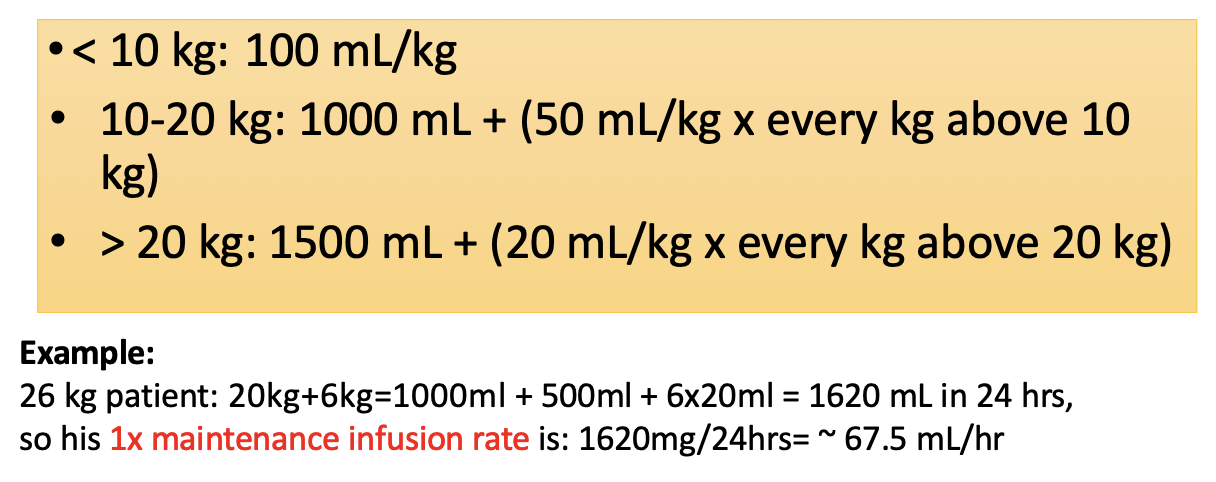
pediatric calculation of 24-hour maintenence fluid volume
based on body weight
adults calculation of 24-hour maintenance fluids volume
based on BSA
(BSA x 1500 mL/m2 ) / 24 hrs
twice maintenance:
2x the calculated fluids