IMED1001 - Genital Anatomy II (Female Reproductive System) (Week 11)
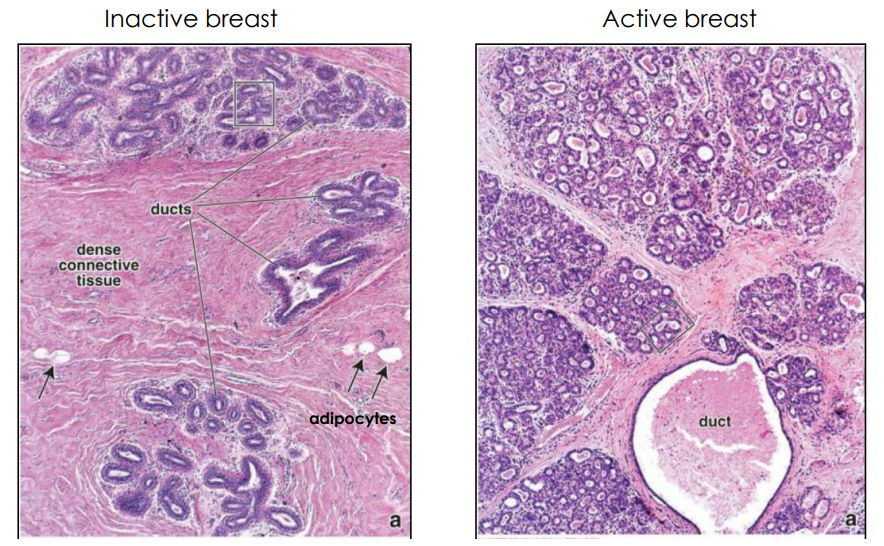
1/30
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
31 Terms
Female Reproductive Structures (NAMING ONLY)
- Breasts/Mammary Glands: breastfeeding
- External genitalia: erogenous zone
- Vagina: sperm deposition
- Uterus: uterine cycle, maintains pregnancy, uterine contractions
- Uterine tubes: fertilisation
- Ovaries: oogenesis and follicular development (oestrogen and progesterone)
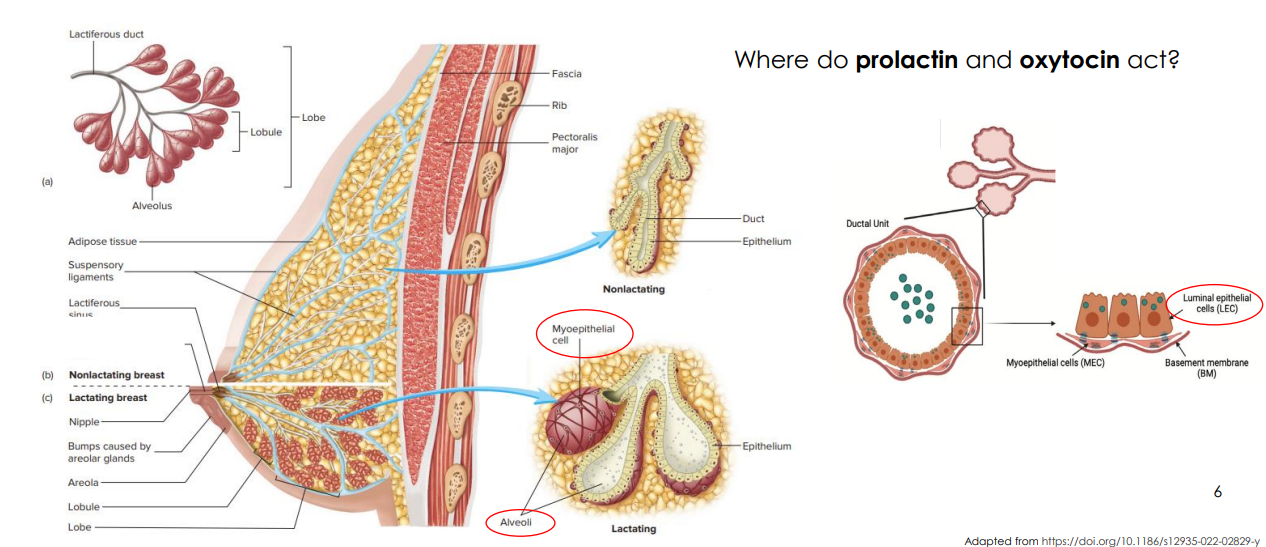
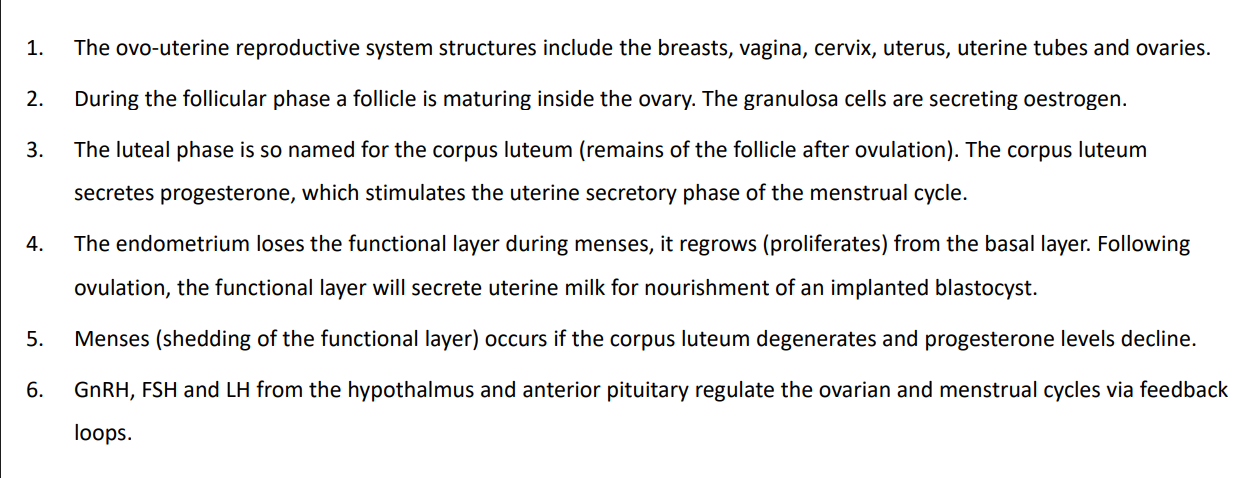
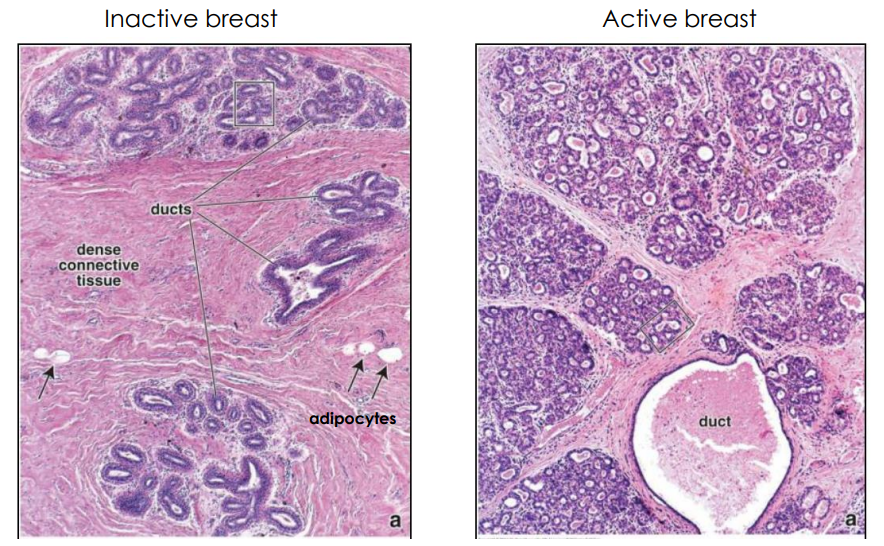
The Breast Tissue Structure
- luminal cells (have lumen) lining the alveoli
- in non-lactating, no alveoli present
- myoepithelial cells are like muscle cells because they can contract
- prolactin targets the luminal cells because its only involved in the production of milk
- for release of milk oxytocin targets the myoepithelial cells
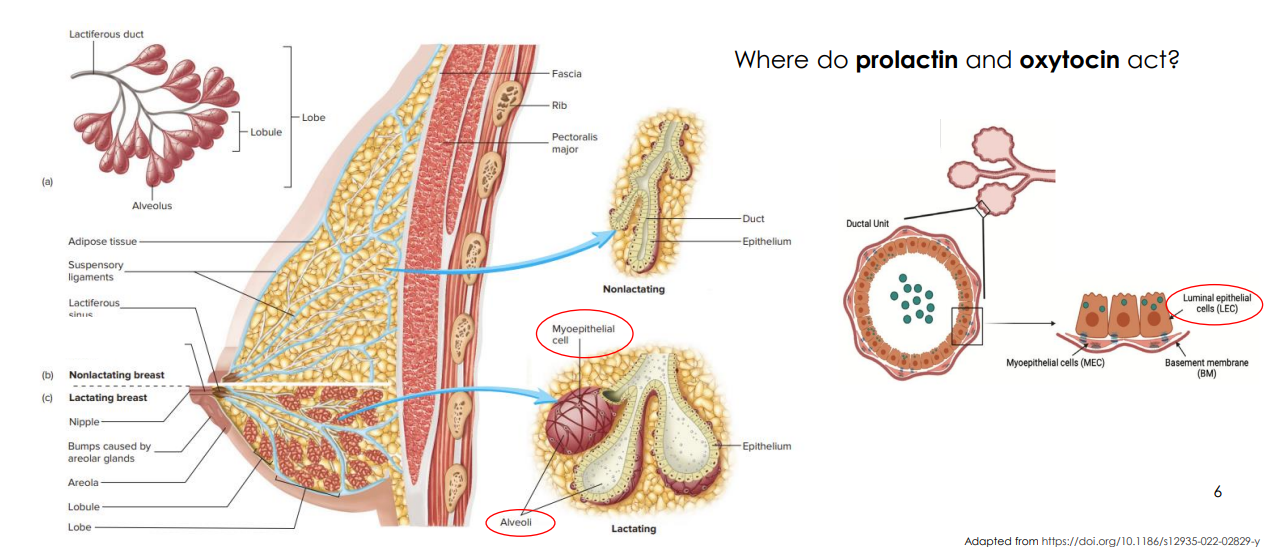
Inactive Vs Active Breast DIAGRAM
- rising estrogen and progesterone during pregnancy trigger the development of more alveoli
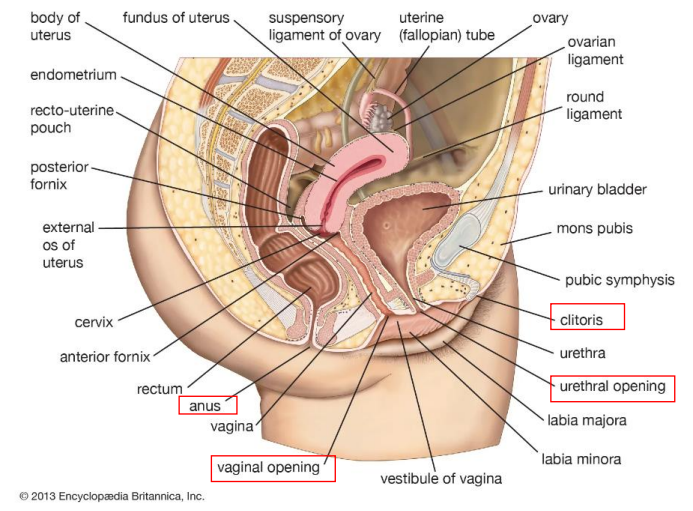
Gross Anatomy of Female Reproductive System
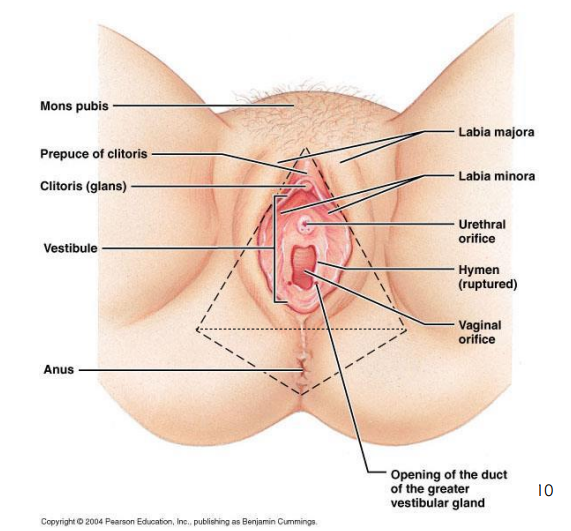
Three Orifices (holes):
1. Urethra
2. Vagina
3. Anus
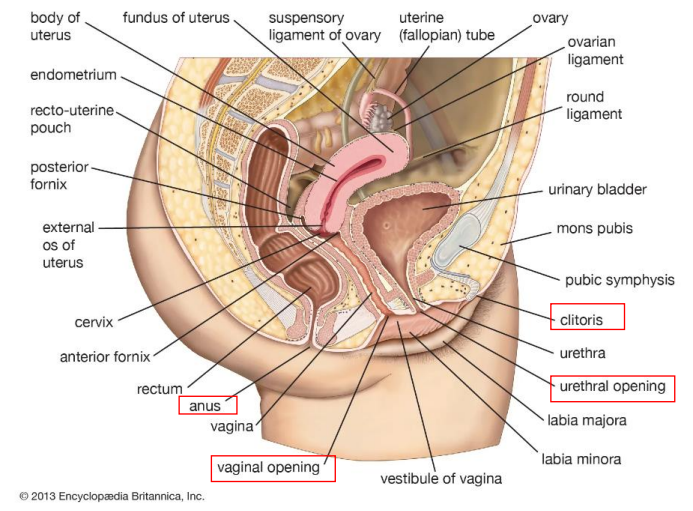
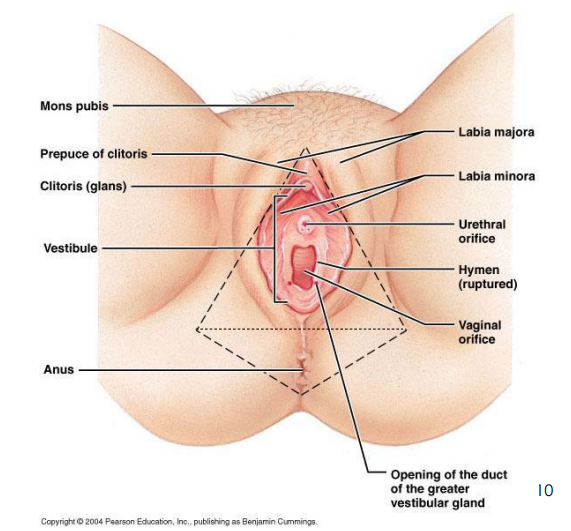
External Genitalia (Monis Pubis, Labia Majora, Clitoris, Hymen, Perineum, Clinical Perineum)
- Monis Pubis: fatty tissue anterior pubic symphysis. Site of coarse hair
- Labia Majora: (sweat and sebaceous gland) and labia minora: folds of skin (minor encloses the vestibule)
- Clitoris: contains corpus cavernous and corpus spongiosum tissues
- Hymen: thin mucous membrane
- Perineum: anterior urogenital triangle (external genitalia), and posterior anal triangle (anal opening)
- Clinical Perineum: between vagina and anus
- perineum is the whole diamond section
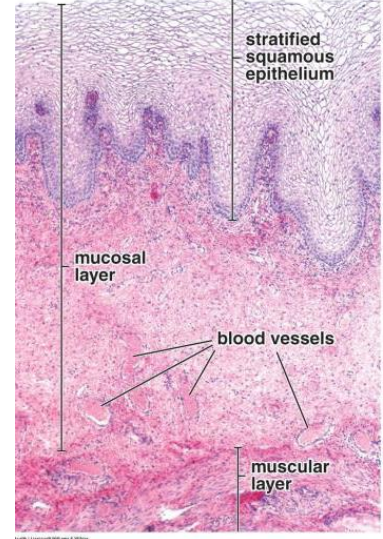
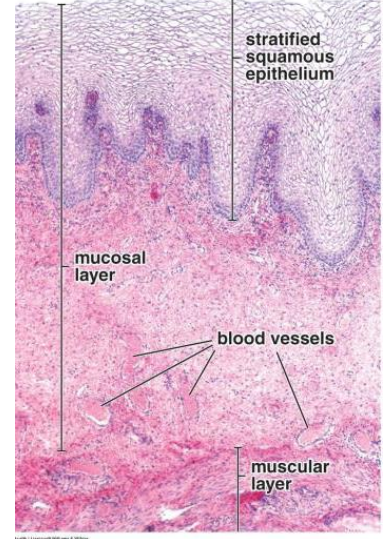
Non-keratinised stratified squamous
- the epithelial cells release glycogen, metabolised by resident Lactobacilli producing lactic acid and decreasing pH (acidic) making it toxic to foreign pathogens
- The muscularis has an outer longitudinal layer and inner circular layer of smooth muscle that can stretch to accommodate intercourse and child birth
- Not a secretory epithelia, relies on cervical secretions
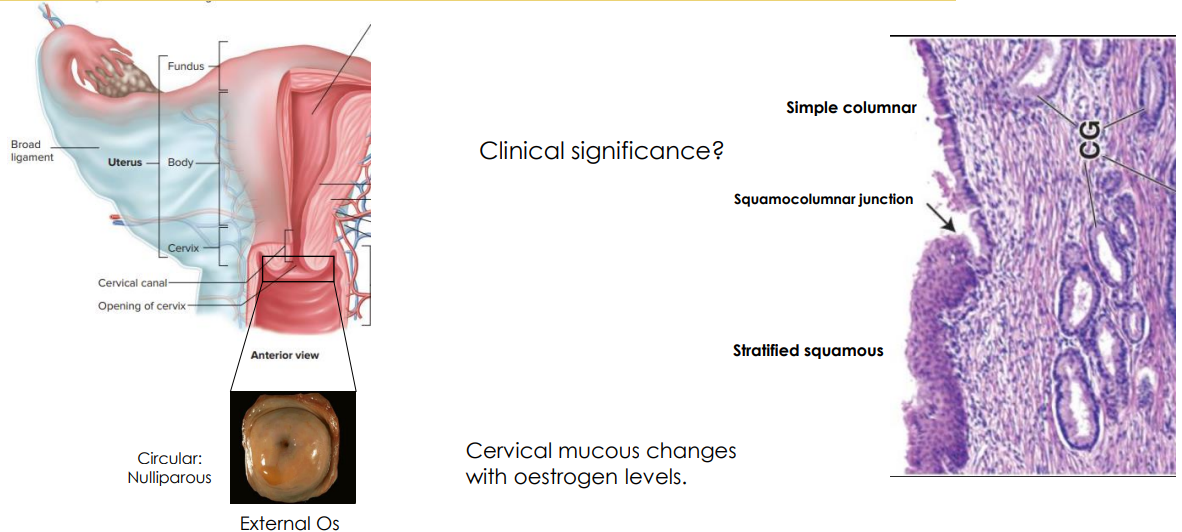
The Cervix Diagram
- within cervix there is a transition zone
- vagina is stratified squamous, if we continue to cervix the epithelial lining changes to simple columnar
- the section it changes is called squamocolumnar junction
- typical hotspot for cervical cancer
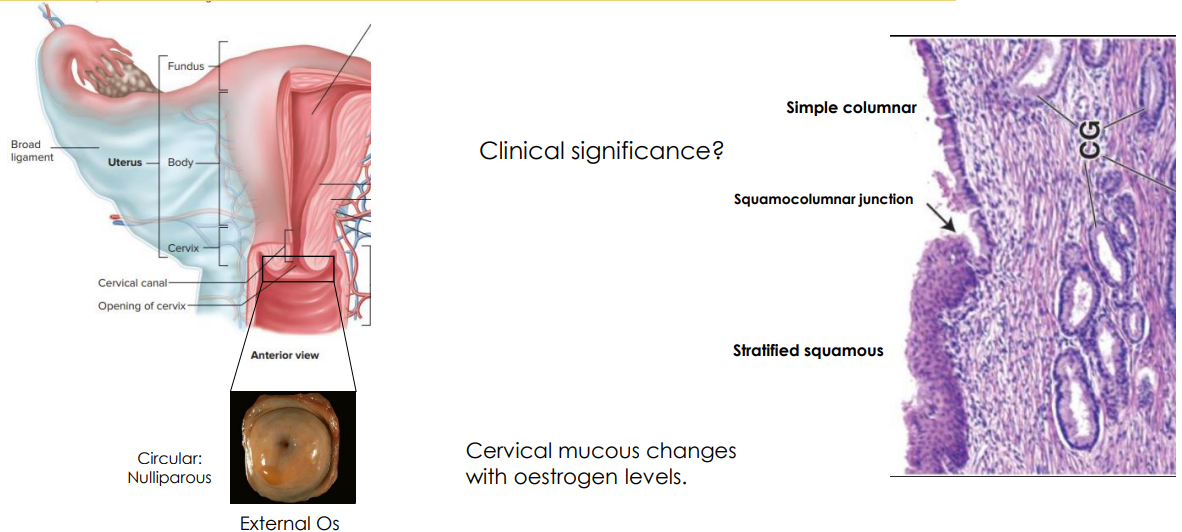
Cervix Secretions
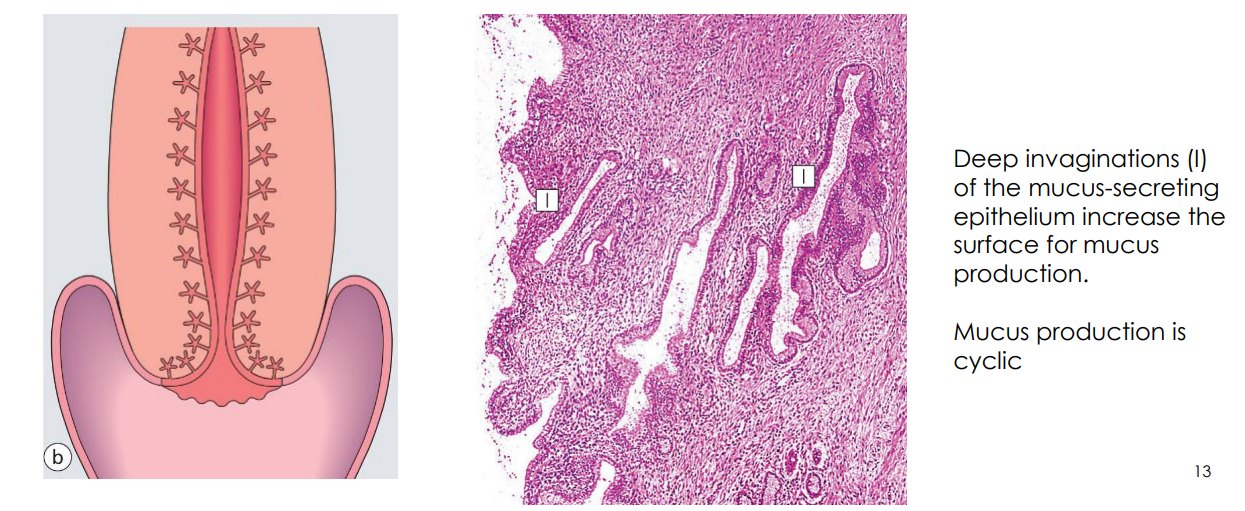
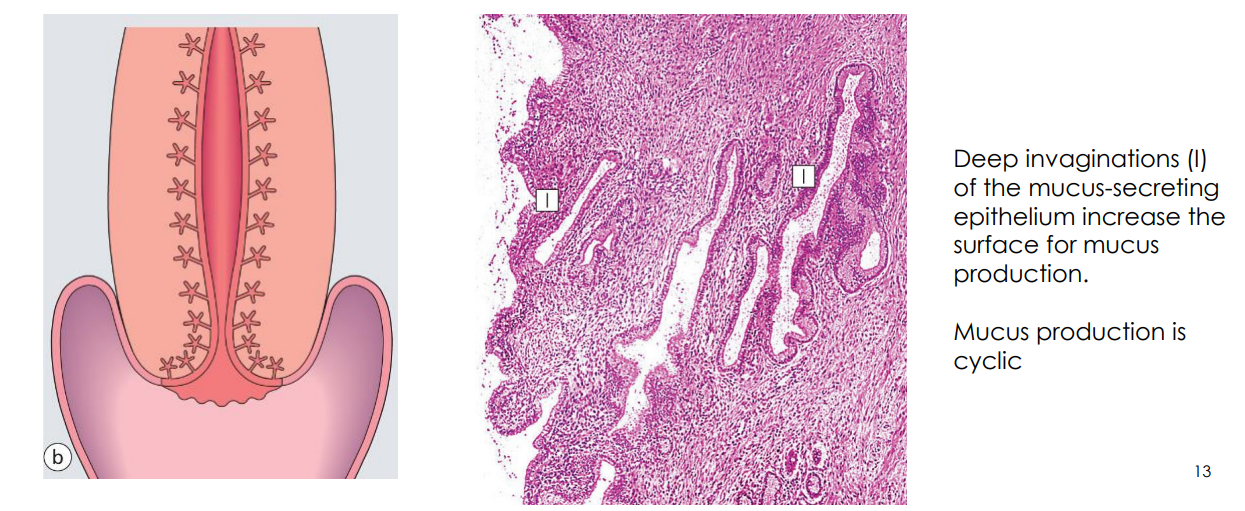
- Deep invaginations (I) of the mucus secreting epithelium increase the surface for mucus production
- Mucus production is cyclic
- cyclic production is dependent on the ovary. the ovary releases hormones to prepare the cervix. ovary releases oestrogen and those levels of oestrogen tell the cervix where its at.
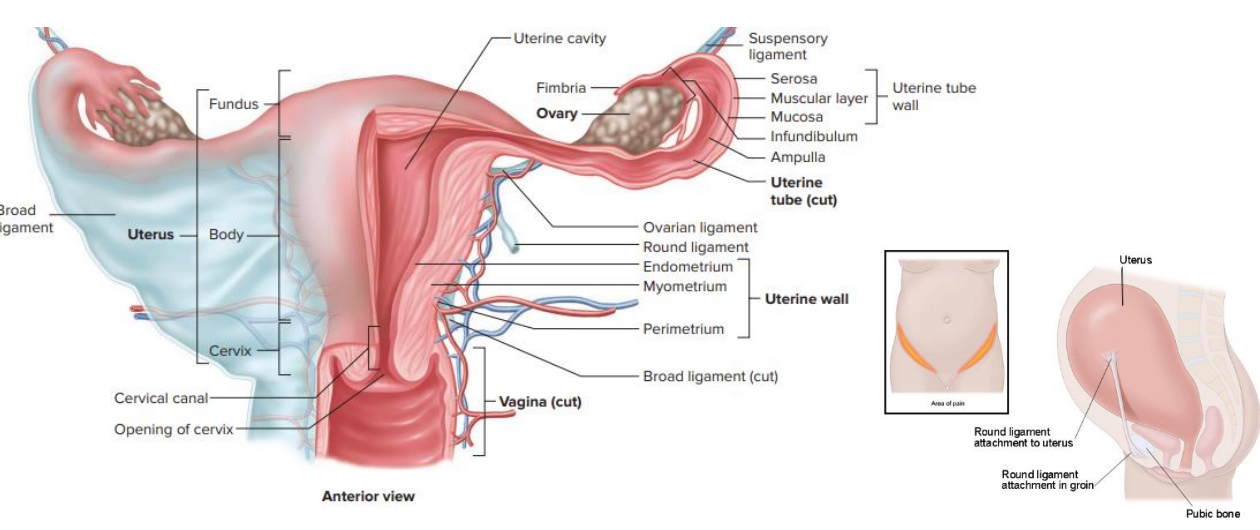
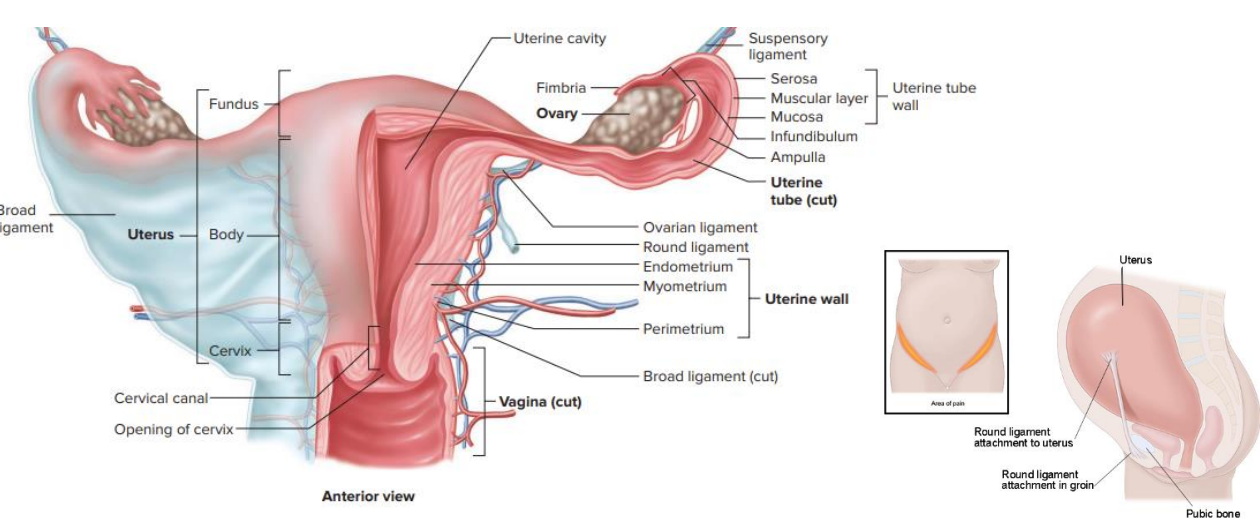
The Uterus Diagram
- once an oocyte is fertilised, we dont want anything else entering
- cervical mucus changes to either allow or block passage of sperm
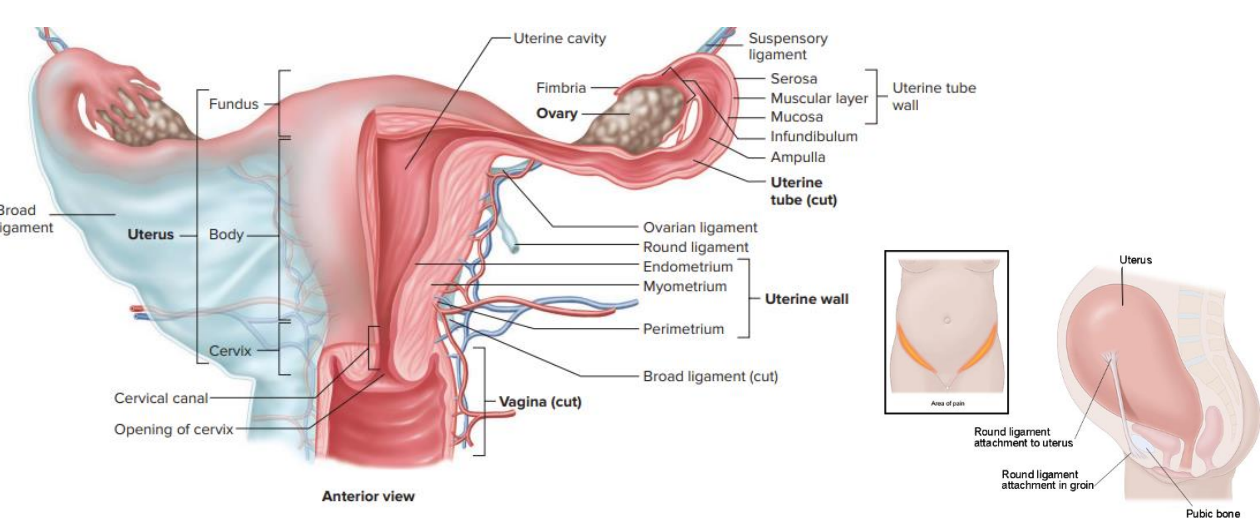
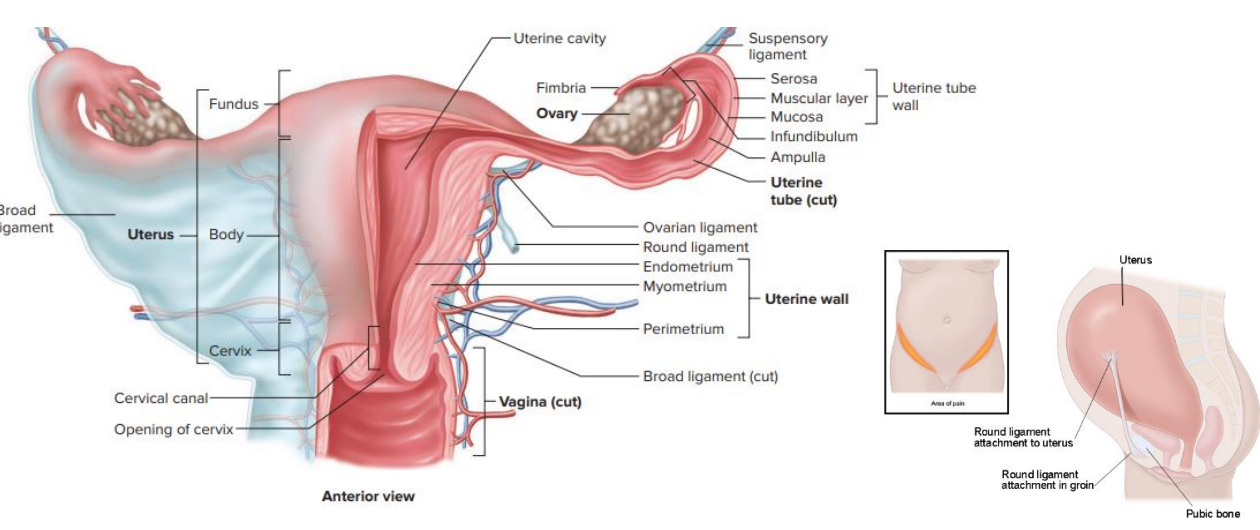
Layers of Uterus
FROM INNERMOST TO OUTERMOST:
- Endometrium
- Myometrium: end goal of birthing baby so it has to be muscular
- Perimetrium
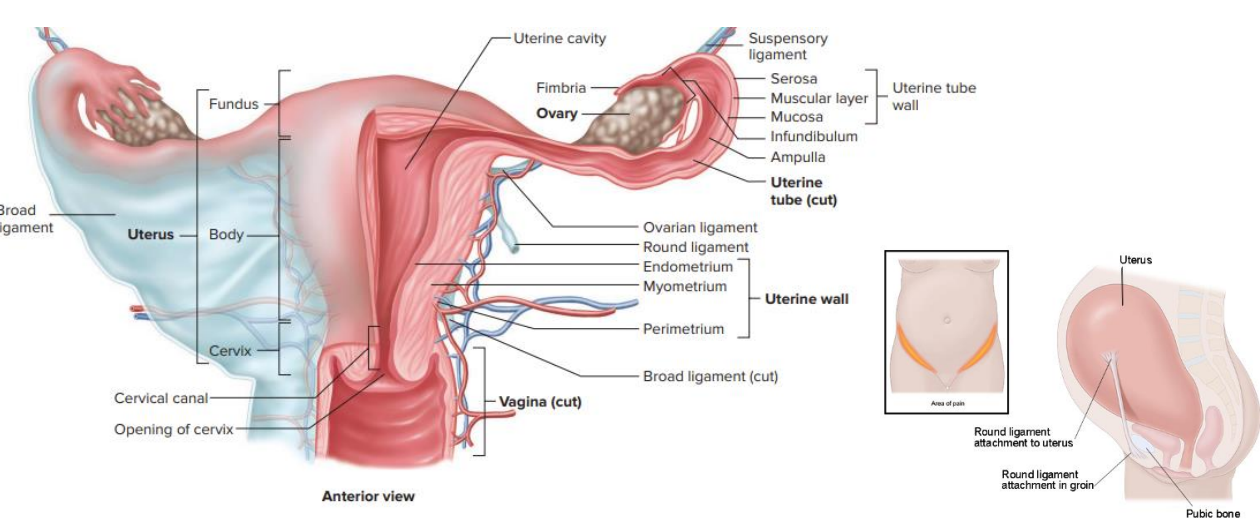
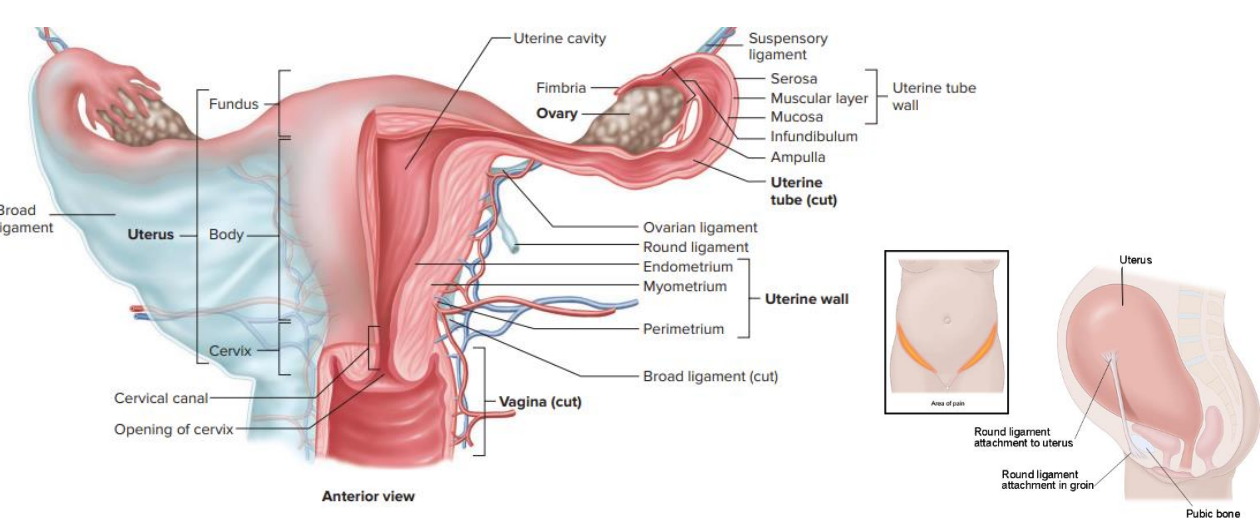
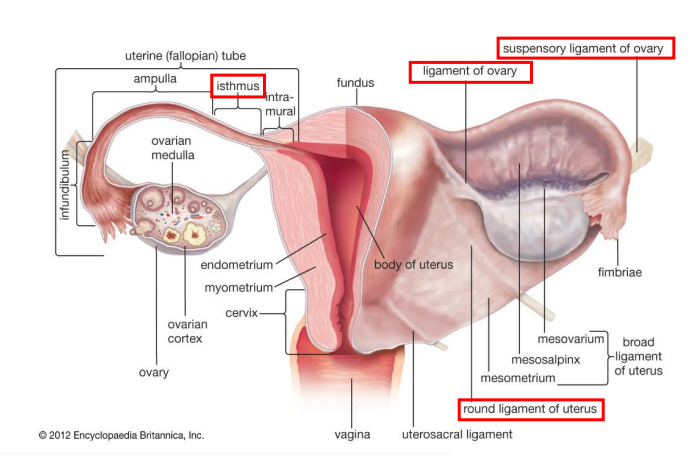
What keeps the Uterus in place?
- broad ligament that is going laterally that is attaching the uterus to the wall of the pelvic cavity
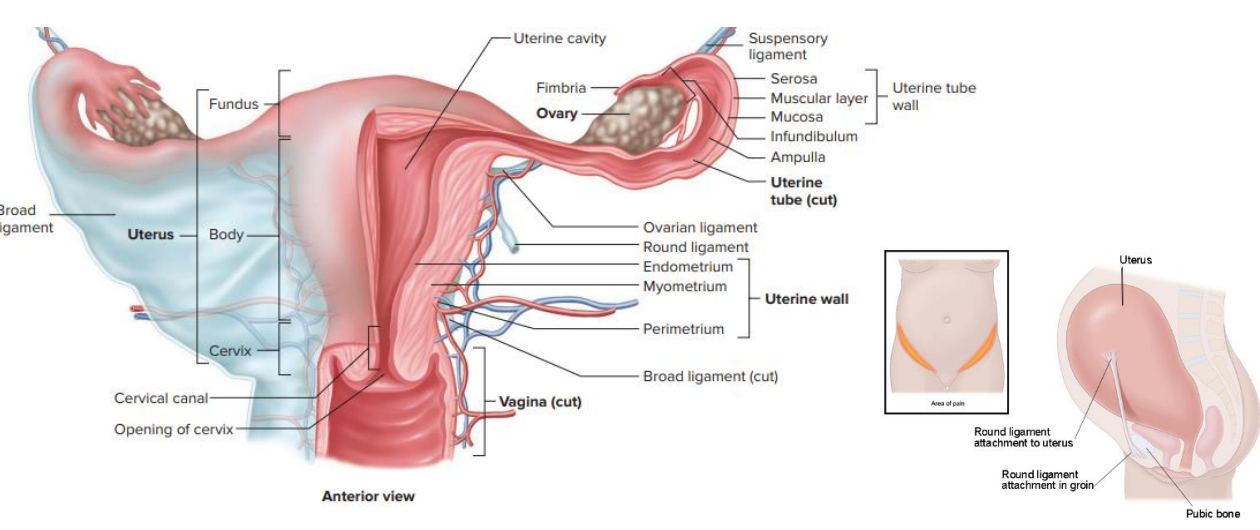
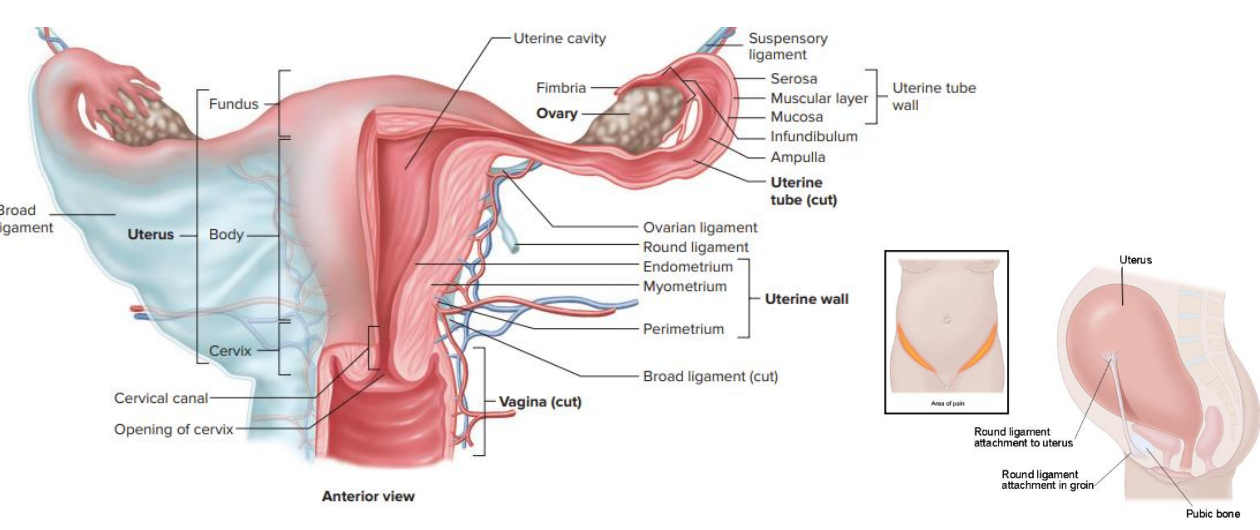
what holds the ovaries in place
- Ovarian ligament: goes from uterus to ovary itself
- suspensory ligament: attaches to ovary on other side
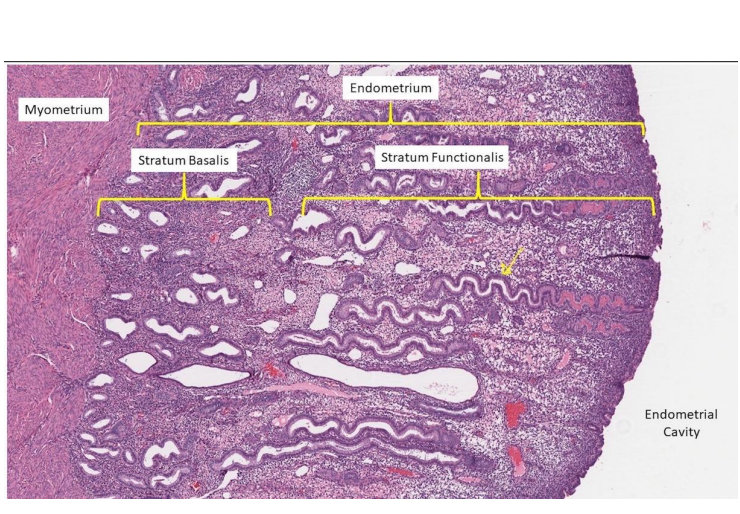
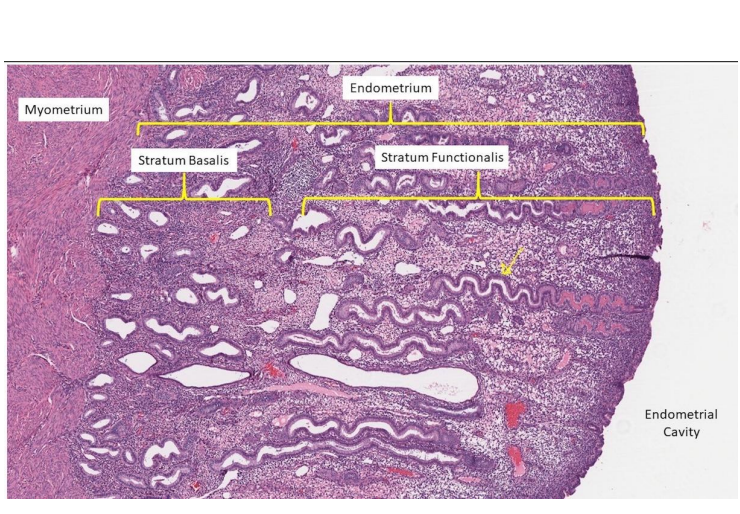
Inside Uterus
ENDOMETRIUM:
- Stratum functionalis (functional layer):
- uterine/spiral glands
- venous sinusoids, uterine capillaries
- responsive to ovarian hormones
Also has a Stratum Basalis (basal layer): origin of uterine/spiral glands, unresponsive to ovarian hormones
MYOMETRIUM:
- middle smooth muscular layer, contractions/growth/stretch during childbirth
PERIMETRIUM:
- outer serous layer (derived from peritoneum)
- spiral glands are the weird snaky looking ones
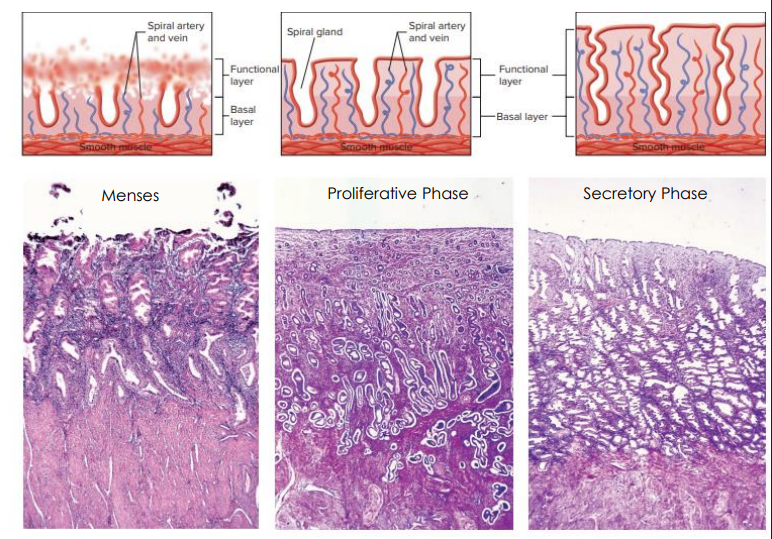
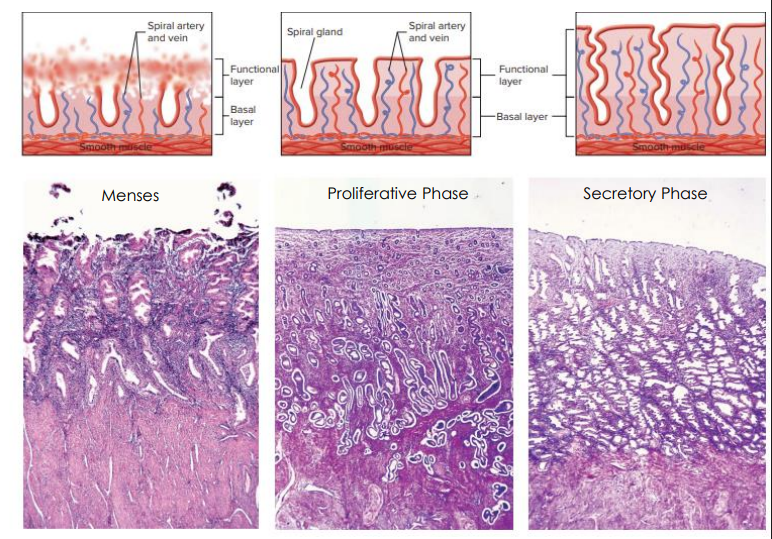
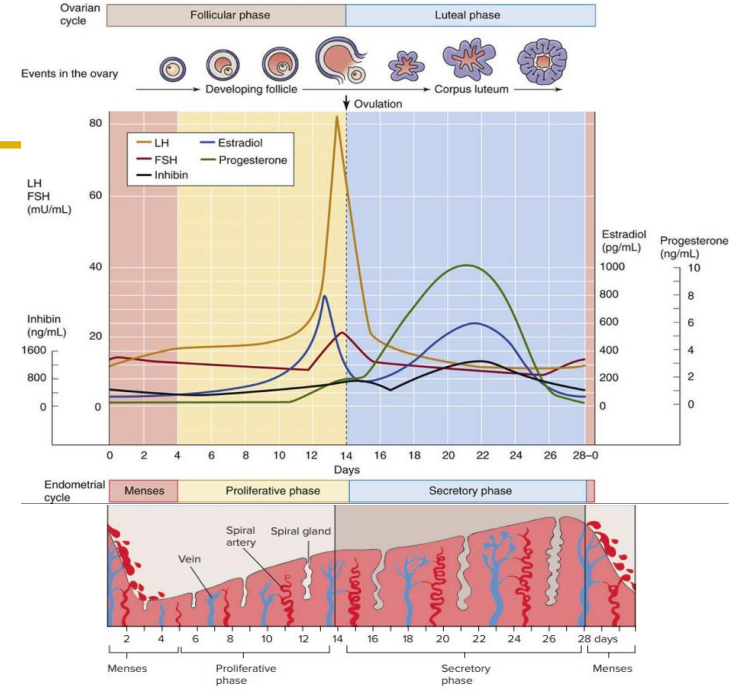
The Uterine Cycle
MENSES:
- Day 1-5
- Stratum functionalis sloughed off
- Menstrual Fluid = stratum functionalis + blood
PROLIFERATIVE PHASE:
- Day 6-14
- responds to oestrogen (from ovary)
SECRETORY PHASE:
- Day 15-28
- responds to progesterone (from ovary)
Spiral Glands secrete glycogen-rich uterine milk (AKA uterine, endometrial or tubular glands)
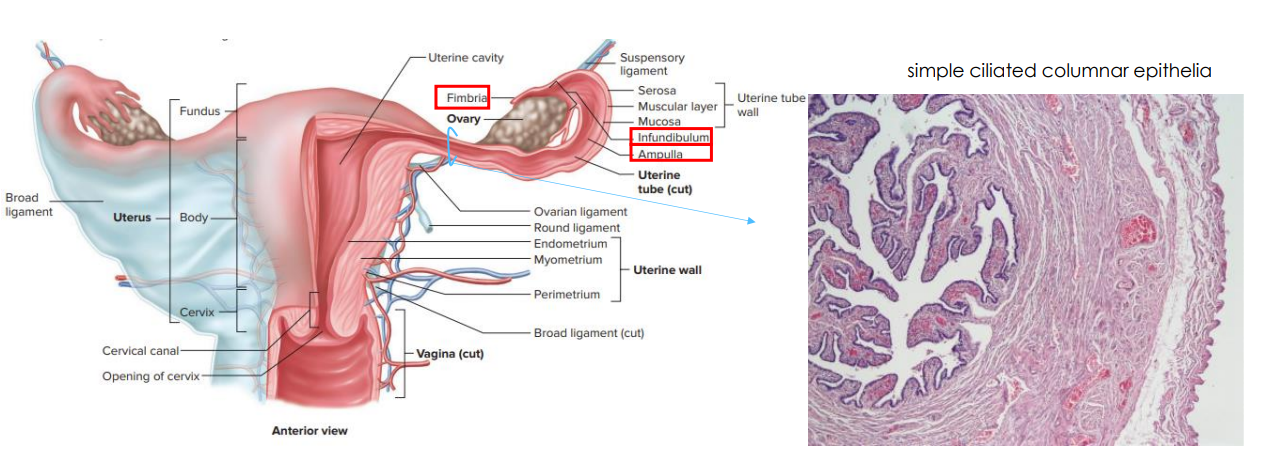
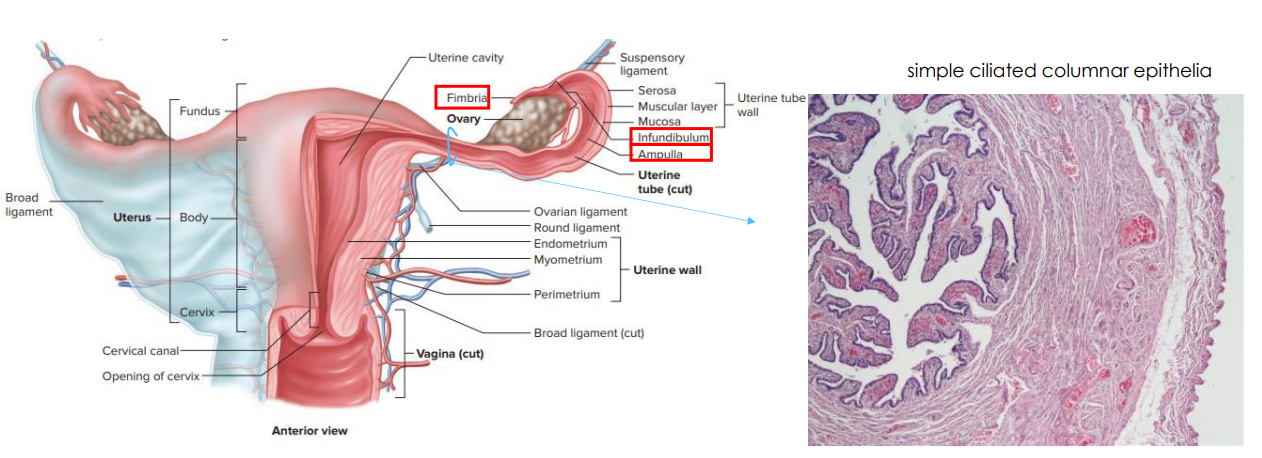
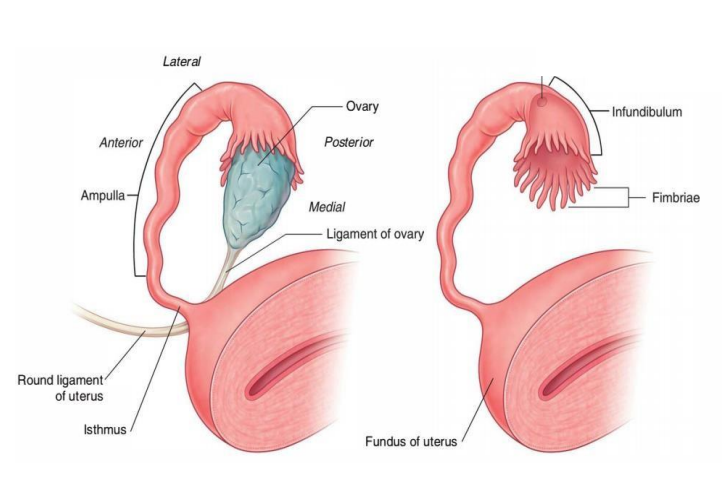
Uterine Tubes
- aka oviduct or fallopian tube
- not directly connected, ovary sits embedded within fimbria (finger like extensions. these beat and allow movement of ovulated oocyte into oviduct)
- leads to infundibulum and ampulla and through the tubes
- the lining of the oviduct is simple ciliated columnar epithelia
- the cilia push the oocyte towards uterus
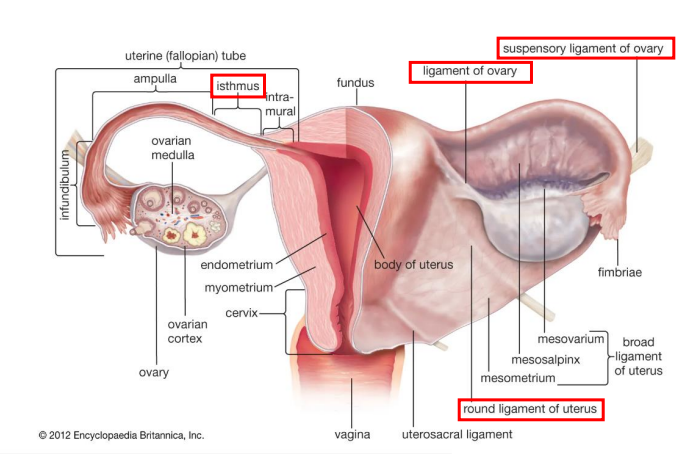
Ovaries
- site for oogenesis and ovulation
- suspensory ligament of ovary contains ovarian blood vessels
- ovarian ligament (ligament of ovary) tethers ovary to uterus
- Round ligament of uterus inserts into labia majora and pulls uterus into anteverted position
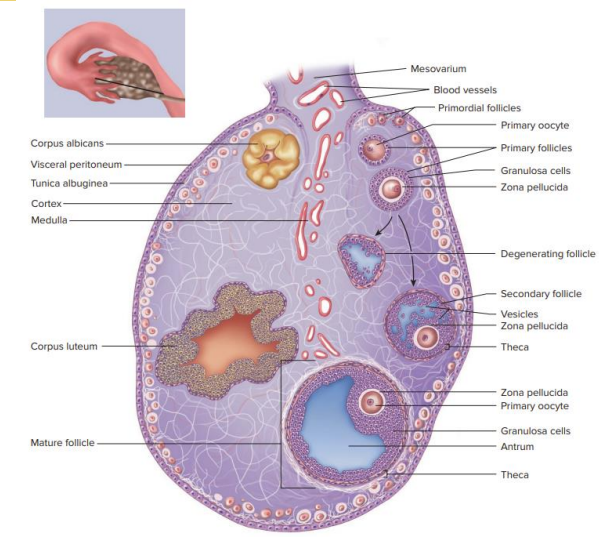
The Ovary
- outer cortex: follicles
- inner medulla: blood vessels, nerves, lympathic vessels
- Oogenesis: differentiation that produces an ovum, a cell competent to further develop when fertilised
- Follicular development: the development of a primordial follicle into a specialised mature follicle to either ovulate its oocyte into the oviduct at mid-cycle to be fertilised or to die by atresia
- Ovulation: mature ovum is released from the ovary into the oviduct
- we know when the follicle is mature because it has antrum (fluid) in it
- degenerating follicle is called corpus luteum
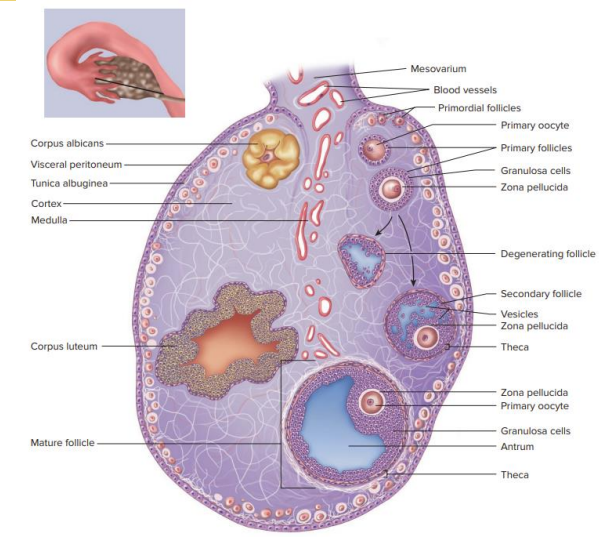
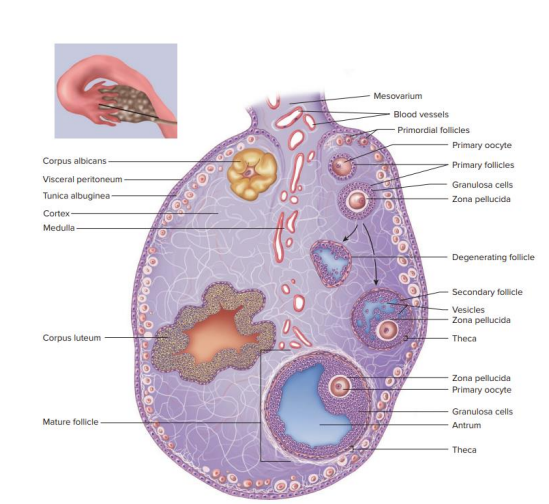
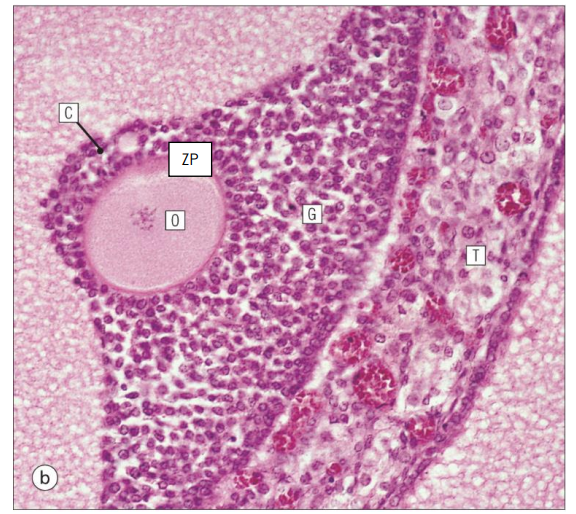
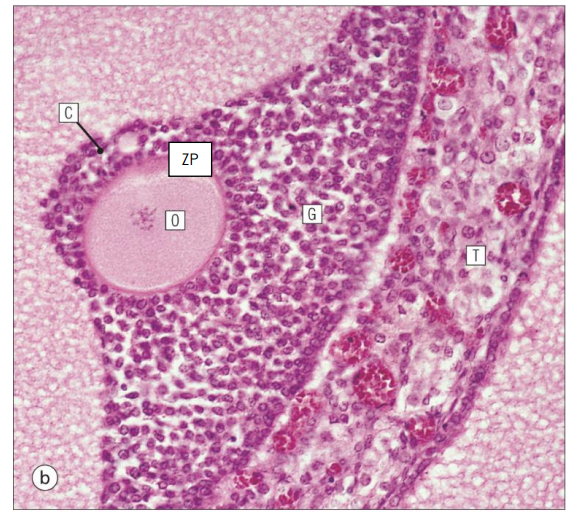
Follicular Development Stages
- Primordial Follicles: Primary oocyte surrounded by single layer of flattened follicular cells
- Primary Follicles: primary oocyte surrounded by multiple layers of cuboidal follicular cells
- Secondary Follicles: fluid-filled spaces develop between granulosa cells (= follicular antrum). Primary oocyte still arrested in first prophase of meiotic division
- Mature Follicles: Large antrum and prominent theca interna layer. Oocyte resume first meiotic division and becomes secondary oocyte.
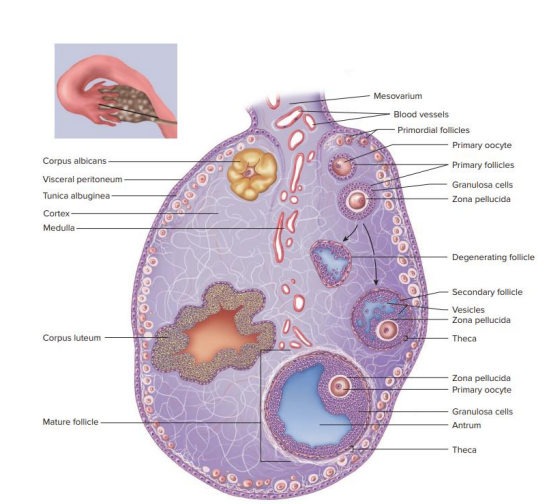
Mature Follicle Diagram
- cumulus radiata is also called corona radiata

Ovulation
- increasing levels of estradial (positive feedback to the hypothalamus and anterior pituitary) triggers surge in Lutenising Hormone (LH) release
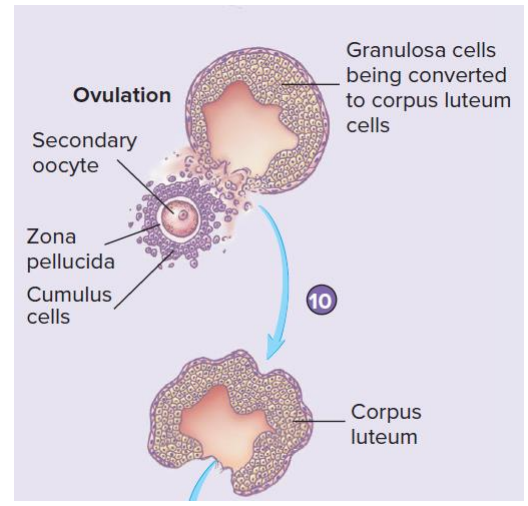
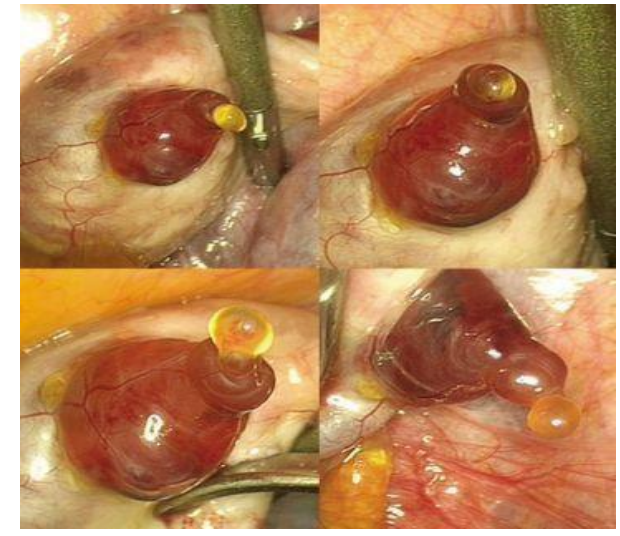
Ovulation Diagram
DIAGRAM ON SLIDE 23
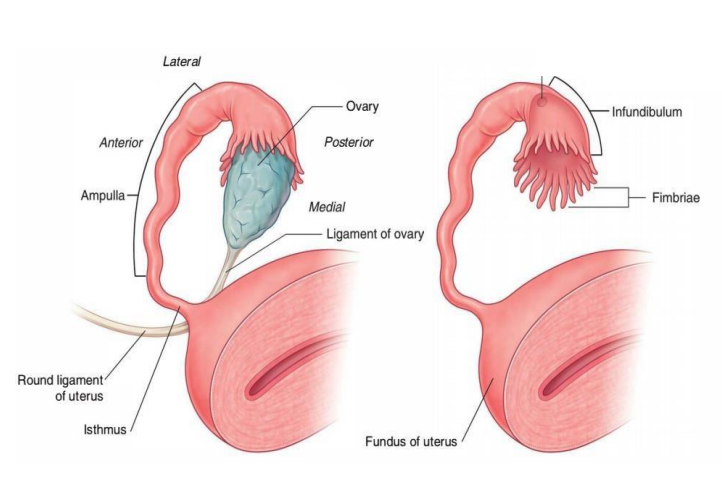
Uterine Tubes Parts
- Fimbriae
- Infundibulum
- Ampulla
- Isthmus
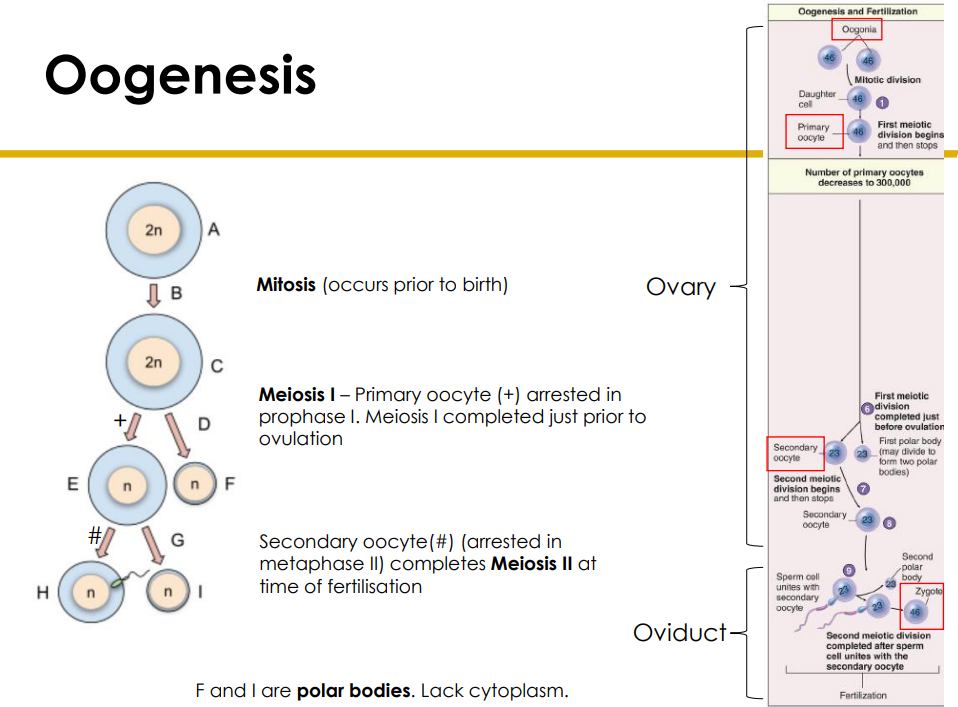
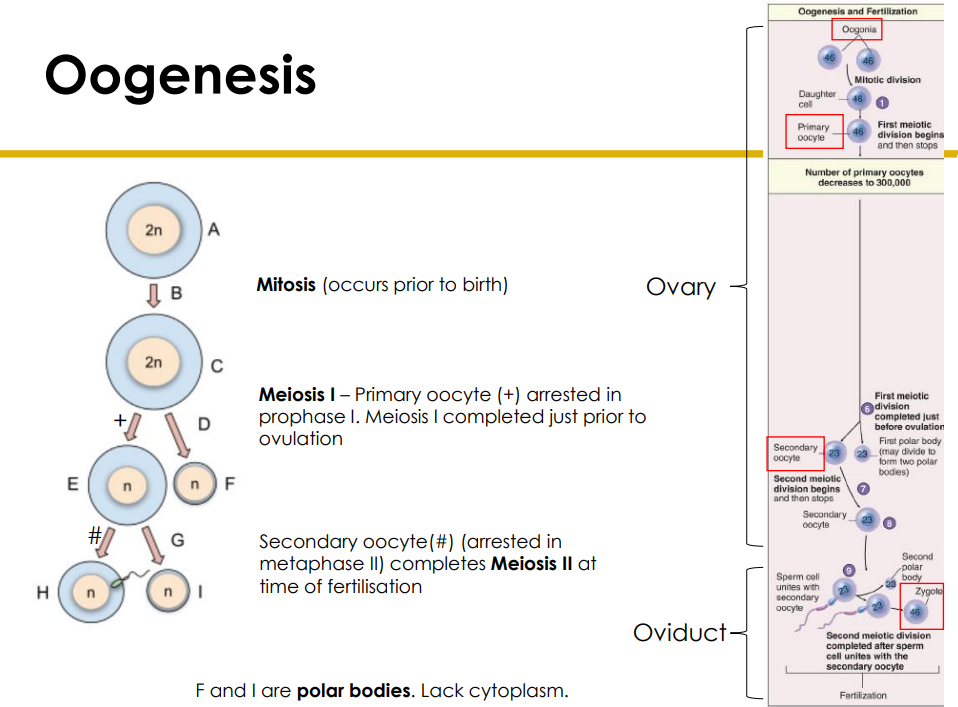
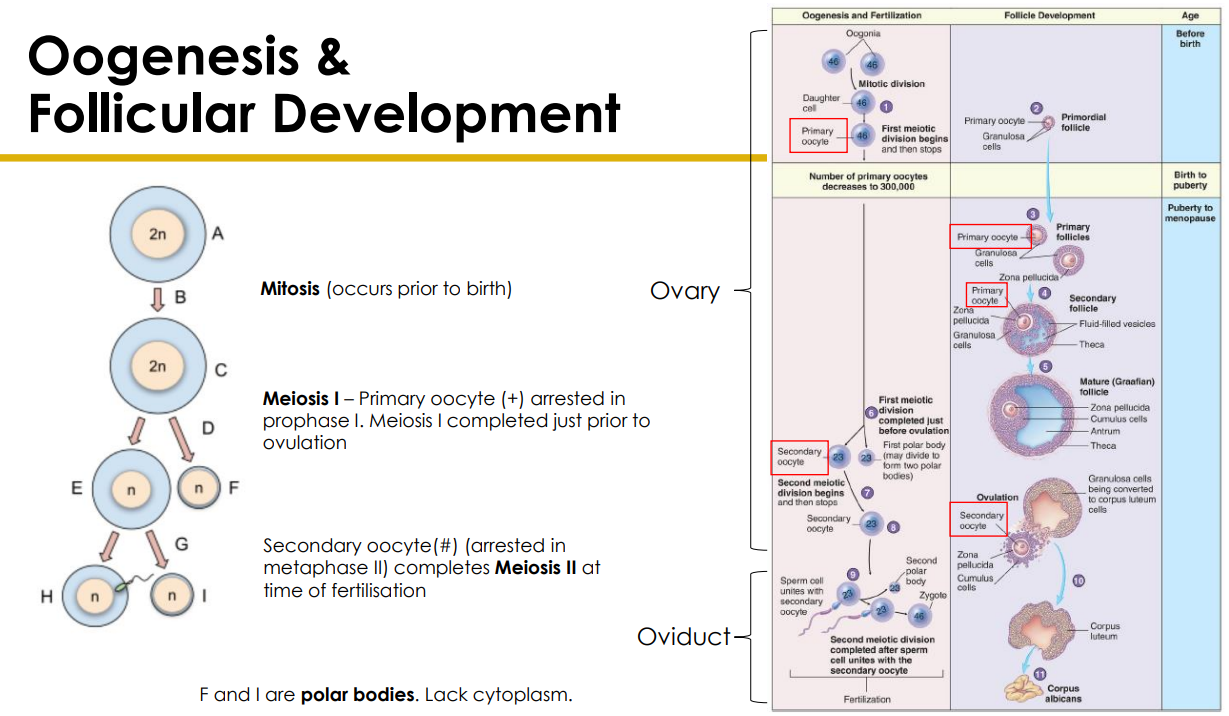
Oogenesis
- Mitosis occurs prior to birth
- Meiosis 1 - primary oocyte (+) arrested in prophase 1. Meiosis 1 completed just prior to ovulation
- Secondary Oocyte (#) (arrested in metaphase 2) completes meiosis 2 at time of fertilisation
- F and I are polar bodies. Lack cytoplasm. basically a ball of DNA
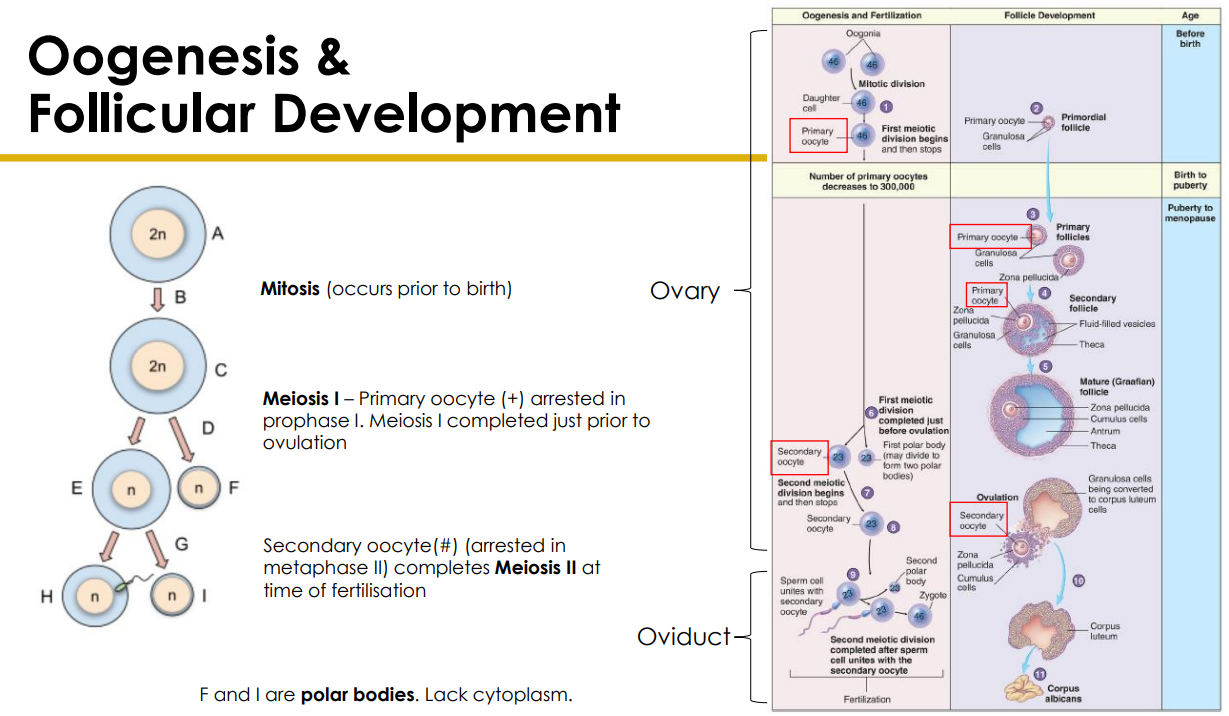
Follicular Development
DIAGRAM ON SLIDE 27
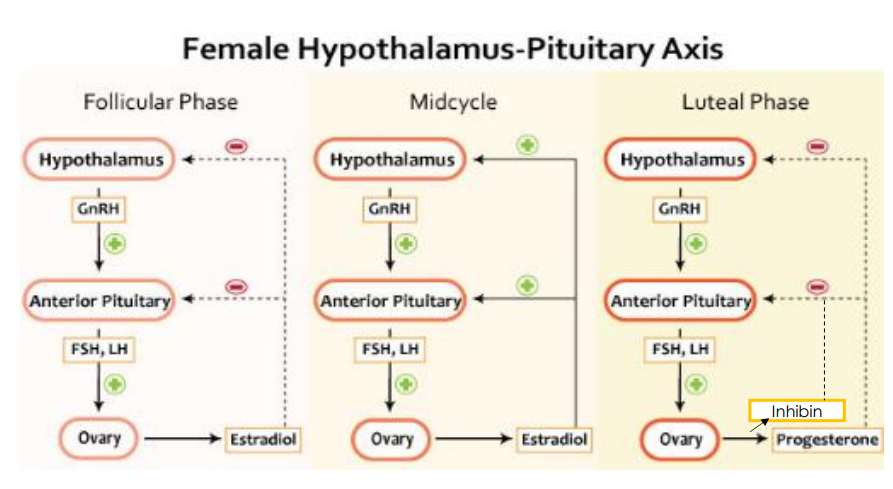
Hormonal Regulation
- estrogen and progesterone released from ovaries
- Regulate: maturation of genitalia, secondary sex characteristics, sexual behaviours and menstrual cycle
- important for maintaining pregnancy
- Relies on anterior pituitary release of lutenising hormone (LH) and follicle stimulating hormone (FSH)
- in turn regulated by gonadotropin releasing hormone (GnRH) from hypothalamus (which increases at onset of puberty and becomes cyclic)
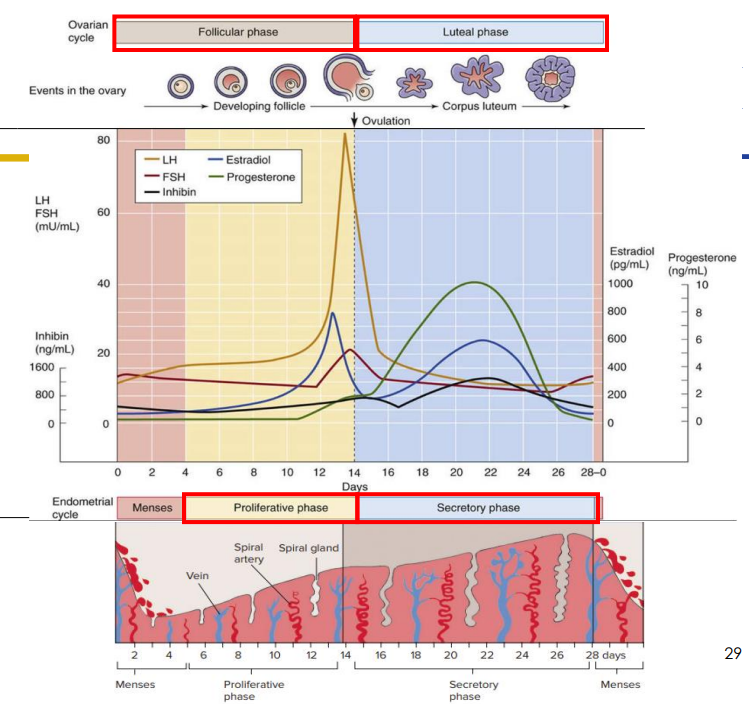
Hormone Levels During Menstrual Cycle DIAGRAM
- estrogen levels spike because big cell with lots of granulosis cells so lots of estrogen being released, and it tells the pituitary that it needs the LH now because its mature
- surge in LH triggers ovulation
- start releasing progesterone and still estrogen which is talking to the uterus to start secretory phase
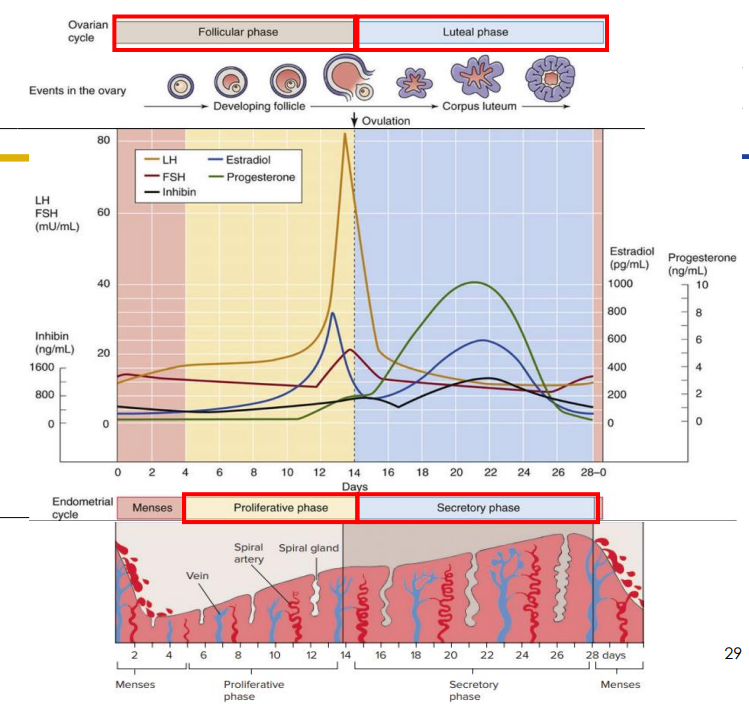
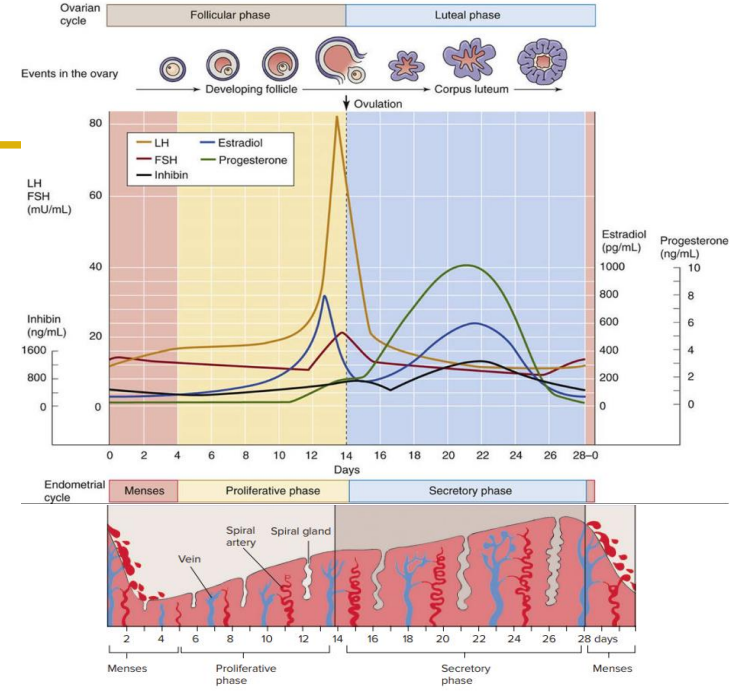
Menstrual Cycle Duration
- menstrual cycle duration varies, usually 21 to 35 days, average 28 days
- Oligomenorrhea if cycles >35 days (means not that many cycles)
- Polymenorrhea if cycles <21 days (means lots of cycles)
- Follicular phase differs
- Luteal phase is usually stable (14 days)
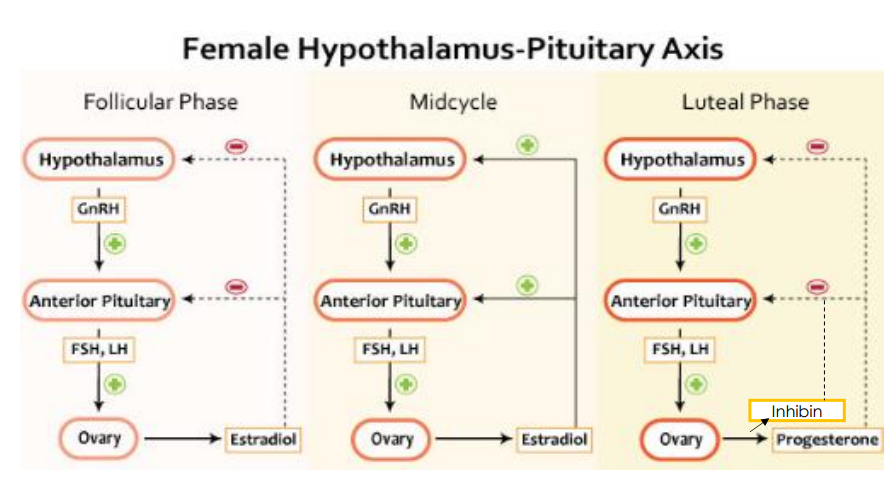
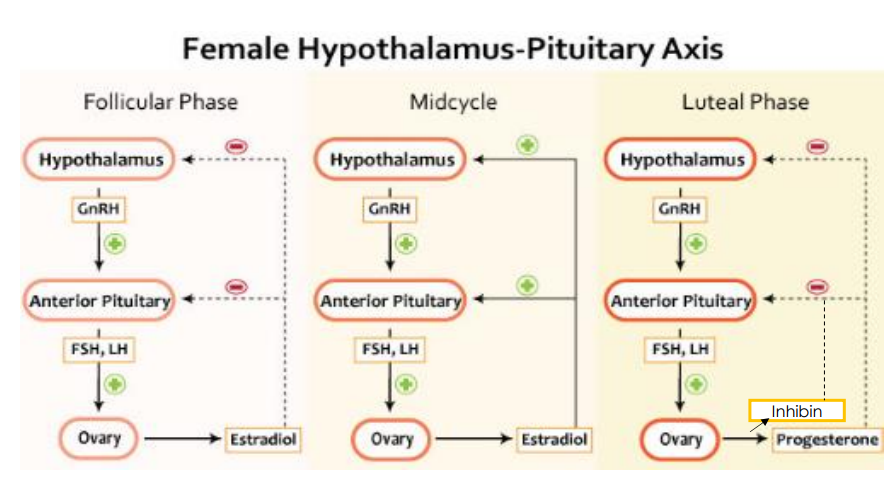
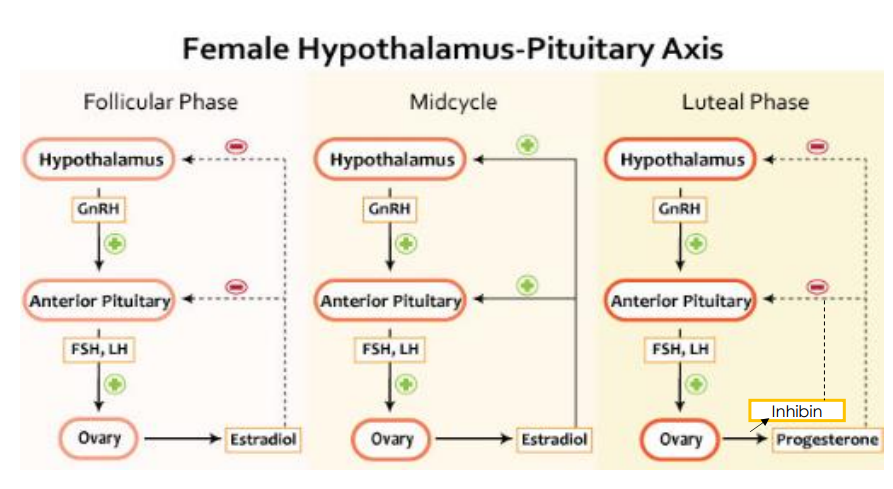
HPG Axis
- FSH targets granulosa cells of follicle
- LH targets theca cells of follicle
- Granulosa cells produce oestradiol
- Luteal cells produce progesterone and inhibin A which reduces FSH secretions
- Midcycle, the rising estridial levels switch from -ve to +ve feedback triggering an LH surge which results in ovulation
Fertilisation
DIAGRAM ON SLIDE 31
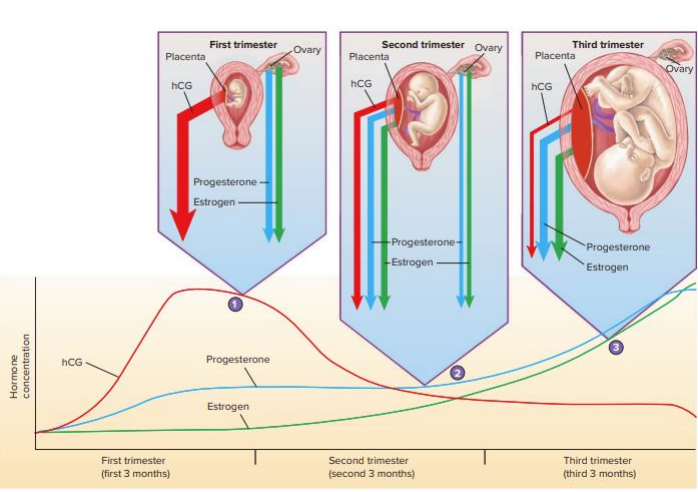
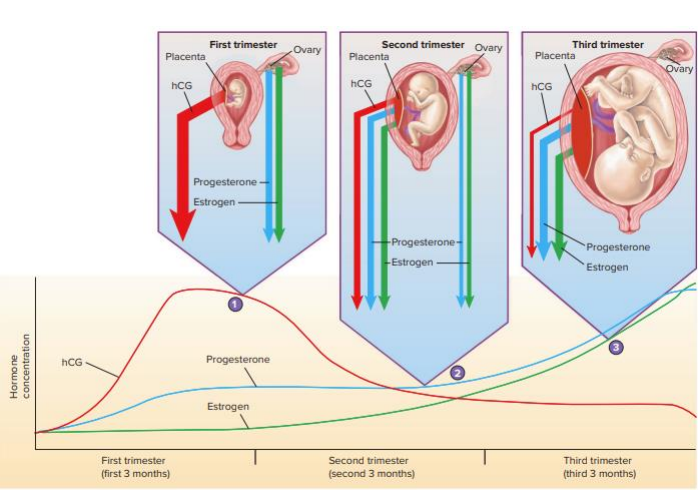
Hormones and Pregnancy
- if fertilisation occurs and pregnancy is maintained human chorionic gonadotropin (hCG) and estrogen and progesterone levels remain high
- placenta releases hCG
- high levels of these prevent release of LH and FSH (preventing follicle development) because it doesnt need another follicle
TAKE HOME MESSAGE
DIAGRAM ON SLIDE 35