Vitreous physiology and Biochem
1/56
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
57 Terms
vitreous fxns
storage area/ avenue for metabolites
shock absorber
light transmission/refraction
source of ascorbic acid - vitamin C
physical support
whats the insoluble part of hte vitreous
collagen (type 2)
describe the collagen of the vitreous
type 2
varying density and orientation of collagen fibers
provides firmness, rigidity, stiffness, resistance to tensile forces, and transparency due to think fibrils
synthesized by the granular endoplasmic reticulum of vitreous cells (hyalocytes found in cortex)
where is the highest conc of collagen
cortex
where is the collagen the densest
vitreous base
where is collagen the least dense
central medullary vitreous
where are hyalocytes found
cortex
whats the soluble portion of the vitreous
hyaluronic acid
describe hyalouronic acid
synthesized by hyalocytes in the vitreous cortex
long unbranched MPS chain assuming sphenoid shape that forms a 3D sponge like network coiled wi the collagen matrix
high negative charge
reinforces and stabilizes collagen network
retains water for rigidity
provides viscosity
controls diffusion
steric hinderance
hydrophillic
what gives the viscoelastic properties of hte vitreous
collagen + HA structure
describe ascorbic acid (Vit C) in the vitreous
free radical scavenger from hyalocytes or aqueous
keeps a hypoxic env
absorbs UV light
main viscosity reducing agent
sugars in teh vitreous
aid in metabolism of hyalocytes and neigboring structures
metabolism occurs in vitreous cortex
diffuse from retinal/choroidal circulation or posterior aq
electrolytes in the vitreous
ionic diffusion
Na
K
Cl
HCO3
Ca
phosphates
lactic acid
what happens to the vitreous as we age
the vitreous turns from a gel to more of a liquid
it liquifies
where does vitreous liquification start
in the medulla where theres less collagen conc
no hyalocytes or dense collagen
acellular
at what age does vitreous liquification start
age 4
adult eye is 20% liquid
by 80-90 its >50% liquid
what structural changes happen to collagen/HA
theres an inc in MW
this happens bc of the formation of new covalent cross links btw peptide chains
collagen fibrils are visible as bundles instead of spaced out fibrils
synchysis
liquification creating vacuoles
syneresis
collagen fibrils contract and shrink and pull off (separation)
together, synchysis and syneresis aer
liquefaction and the formation of lacunae
posterior vitreous detatchment
increased liquid volume of vitreous results in a collapse of the vitreous centrally
this pulls the posterior vitreous forward
ILM thickens w age and does not adequately hold inserted collagen fibers
collagen fibrils collapse and aggregate into sheets of collagen fibers
what part of the retina is the vitreous normaly attached to
ILM
where does a PVD happen
its a separation of the posterior vitreous from the ILM of the retina (posterior to the vitreous base)
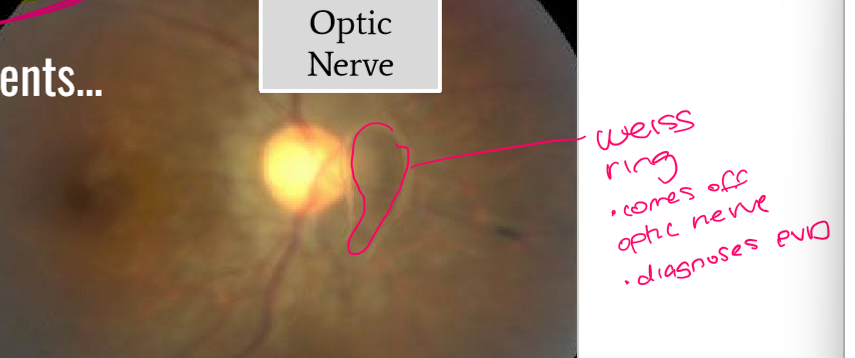
whats the order a PVD detaches in
peripherally
macula
optic nerve
total PVD w a Weiss ring
what are symptoms of a PVD
floaters
flashes of light
as vitreous detaches it pulls on the retina
in a regular PVD, _________ and ________ occur simultaneously
synchysis and syneresis
what happens in an anomalous PVD
pathology or high RE causes the processes of synchysis and syneresis to not happen simultaneously
some areas stay attached while some separate
can tug on BV and cause bleeding
what factors contribute to a PVD
ocular inflammation
aphakia/psuedoaphakia
aging
RE - high myope >6
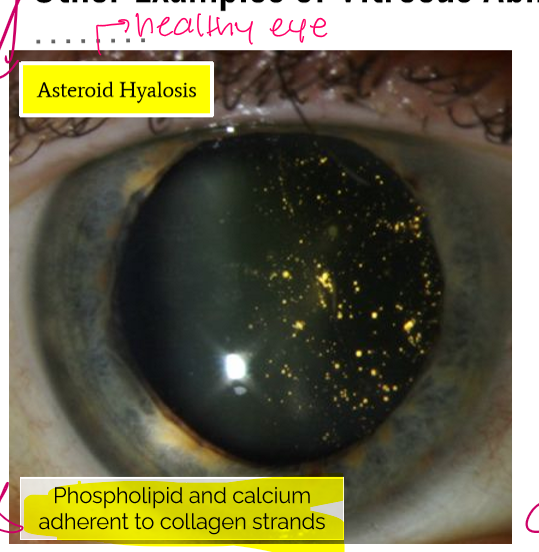
what happens in an asteroid hyalosis
phospholipid and calcium adherent to colagen strands
healthy eye
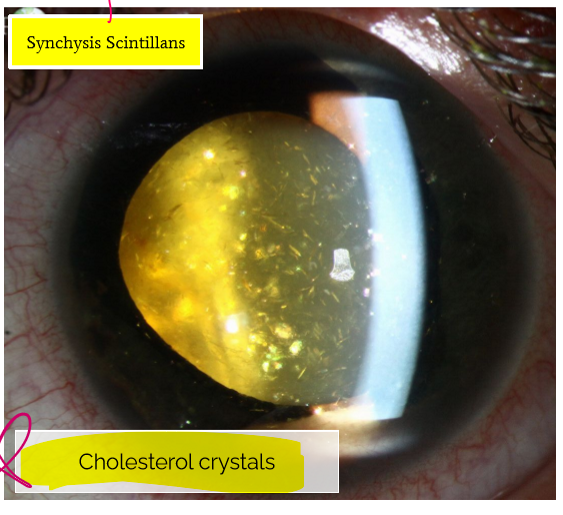
what happens in synchysis scintillans
cholesterol crystals
trauma - retinal detachment
what are anterior attachments of the vitreous???
anterior hyaloid membrane
bergers space
how does the intact vitreous provide protection against nuclear lens changes
anterior vitreous adherent to posterior lens in younger patients
much higher incidence of NS following vitrecotmy in patients over 50
what specific thing protects the lens from oxygen and how
ascorbate
regulates intraocular molecular oxygen
protects against oxidative stress
maintained by a sodium dependent transporter in the pigmented layer of the CB ep
does the gel or liquid state of the vitreous have a higher conc of ascorbate
gel
myope gets a cataract gaster bc they liquify faster
if the vitreous, how does this impact the lens
we get an accelerated cataract
PVD and peripheral structures
may also damage the cells of teh TM
intact gel and crystalline lens protective against open angle glaucoma (POAG)
may induce apoptosis and neuronal cell death
how many blood supplies to retina
2
high oxygen demand due to metabolic activity
one of the best perfused organs
how does blood get to the retina?
aortic arch —> (right only: brachiocephalic artery) —> common carotid —>ECA and ICA —> ophthalmic artery —> Posterior ciliary arteries —> choroid
—>ophthlamic artery —> Central retina artery —> retina
what part of the retina does the CRA supply
inner 2/3
what part of the retina does the choriocapillaris supply
outer 1/3 - photoreceptors
what has he highest blood flow/ is most perfused
choroid
what does it mean that the eye is a closed sphere
blood vessels enter as arteries, merge w capillaries, and exit as viens
retinal vasculature (veins and arteries) travel together as they enter the gloe thru the center of the ONH and branch into _______________________________
4 quadrants throughout the posterior pole and peripheral retina
describer retinal arterioles
arteriole more narrow
brighter reflex
2/3 A/V
no pulsation
describe arteries
high pressure
smaller lumen
thick smooth muscle
sensitive to sympathetic
tight jxns = BRB of vascular endo
autoregulation = maintain itself by vasoconstriction/dilation
wheres the outer BRB
RPE adn tight jxns
wheres the inner BRB
retinal vascular endo tight jxns
does the choriocapillaris have tight jxns
no, fenestrated - leaky
how does the retina drain
venous outflow is mediated by the CRV and vortex veins
these are branches of the superior and inferior ophthalmic veins
path of venous outflow / drainage
CRV
ophthalmic vein
CAV sinus
describe a venule
not holding high velocity blood
thinner wall
large lumen
tight jxns - BRB
autoregulation
more sensitive to parasymp
describe retinal veins
larger
no prominent central reflec
VOLD
pulsate
whatas the equatio nfor perfusion pressure
Perfusion pressure = P arterioles - P veins
P arterioles = 65- 70
P veins = 10-21 similiar to IOP
what do arteries and veins share at crossing
a common adventitia
autoregulation of retinal vasculature
ability of retinal vasc to constrict or dilate in response to blood pressure, allowoing maintenance/ consistency of blood flow
autoregulation is done in the
retina
inner 2/3 only - not choroid bc those are fenestrated
autonomic system impacts
choroid