AOS 1 SAC: SLEEP
1/147
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
148 Terms
sleep hygiene
good habits and practices that support consistent, restful, and high quality sleep
Key sleep hygiene strategies (6)
Consistent Sleep Scheulde - regulates the circadian rhythm
Use your bed only for sleep- builds strong psychological connection to sleep
No screens 1 hours before bed- these disturb natural sleep cycles- blue light interferes with melatonin production
Avoid Caffeine and alcohol before bed-disturbs natural sleep cycles
Relaxation before bed-reduces arousal and helps sleep onset
Exercise Daily (not too close to bedtime)- builds sleep pressure, improves quality
Zeigebers
external environmental cues that help synchronise our interal body clock with the external world
main types of zeigebers
Light based - daylight, blue light, artificial light
Social/ Behavioural- meal times, routines, social interaction, exercise
Adapting to light Zeigeber
morning sunlight exposure resets circadian rhythm
avoiding blue light at night allows melatonin to rise nauturally
TIP: get 10-30 mins natural light after waking, to help reset sleep-wake cycle
Adapting to temprature Zeigeber
sleep is easier when body temp is cooler
warm shower 1 hour before helps trigger natural body cooling
ideal room temp 18-20
adapting to eating pattern zeigeber
avoid heavy meals, caffeine, and alcohol before sleep
eat at consistent times to reinforce daily body rhythms
Circadian Rhythm Disorder
when your body’s internal clock is out of sync with societal expectations
Circadian Rhythm Disorders usually cause
insomnia
excessive sleepiness at the wrong time
daytime fatigue
Types of circadian rhythm sleep disorders
Delayed Sleep Phase Disorder (DSPS)
Advanced Sleep Phase Disorder (ASPD)
Shift Work Disorder
DSPS problems
“Night Owl” Problem
very late sleep schedule (3am-11am)
can’t fall asleep and struggle to wake up in the morning
DSPS symptoms
can’t fall asleep until late
struggle to wake for school/ work
feel very sleepy in the morning
normal sleep quality, just shifted too late
why does DSPS happen (3)
cicadian rhythm wants a later bedtime
very common in teenagers
can become a real issue when responsilities (like school) don’t match
ASPD problems
“early bird” problem
very early sleep schedule (6pm-2am)
get super sleepy in the evening and wake up too early
ASPD symptoms
can’t stay awake in the evening
wake up way too early (and can’t fall back asleep)
tired during the day
Possible causes of ASPD
weaker body clock (SCN)
lower melatonin production
less exposure to light in the evening
Shift Work Disorder problems (SWD)
“I work nights” problem
you work night shifts or rotating shifts- confuses your circadian rhythm
SWD symptoms
can’t sleep well during the day
feel tired at work in the night
insomnia + excessive sleepiness
Why is SWD so bad
you’re awake when your body naturally wants to sleep
sleep is light, short, and easily disturbed
may get 1-4 hours less sleep than normal
risks of SWD
sleep debt
low alertness= more accidents
worse when shifts rotate quickly (e.g. every few days)
long-term health issues
Bright Light Therapy (Phototherapy)
helps to reset biological clock (SCN) using artificial light
how bright light therapy works
you sit near a light box that mimics sunlight (at least 2500-10,000 lux)
sessions last 15 minutes to 2 hours
can be done reading or using your phone
when someone with DSPS should do BLT
use light early in the morning to shfit circadian rhythm earlier
when someone with ASPD should do BLT
use light in the evening/night to shift circadian rhythm later
when someone with SWD should do BLT
evening or before shift to help you stay alert at night
17 hours awake to BAC
0.05%
24 hours awake to BAC
0.10%
Dawson and Reid Study (1997)
40 participants
within-subjects design with counterbalancing
2 conditons: sleep deprivation and alcohol consumption
both groups had to complete computer tasks that tested hand-eye coordination, attention, speed, accuracy, decision making
Cognitive effects from Dawson and Reid Study
as time increased, performance dropped
one full night without sleep can impair thinking as much as being drunk
Affective effects from Dawson and Reid Study
Both sleep deprivation and alcohol can
make you moody, irritable, or short-tempered
affect your motivation and emotional regulation
interfere with your focus, memory, and decision-making
examples of the connection between alcohol consumption and sleep deprivation
being in a bad mood might make you drink more
drinking can affect your sleep
poor sleep can worsen your mood- and the cycle continues
real life application of dawson & reid study
sleep-deprived people may be just as unsafe as drunk people when driving or working
teenagers are especially vulnerable to sleep loss due to late bedtimes, study pressure, and social media
always be cautious about your sleep habits, especially before doing important tasks like exams, work, or driving
Sleep Deprivation
when a person gets less quantity or quality of sleep than needed
voluntary deprivation example
staying up late to watch a sport game or to play a video game with friends
involuntary deprivation example
working night shifts or having a sleep disorder
partial sleep deprivation
getting some sleep, but not enough
total sleep deprivation
getting no sleep at all for a period of time
sleep quantity
how much sleep you get (measured in hours)
sleep quality
how well you sleep- measured by how restored or rested you feel, and whether your sleep was consolidated (not interrupted)
Sleep debt
accumulated sleep loss over time
e.g. sleeping 1 hours less for 5 nights = 5 hours debt
repaying sleep debt
one good sleep (sufficent quality/quantity) can repay the debt
you don’t have to repay debt fully, but need enough recovery sleep to function well
3 main effects of partial sleep deprivation
Affective functioning (Emotions and mood)
Behavioural functioning (actions and physical responses)
Cognitive Functioning (thinking and mental processing)
effects of partial sleep deprivation on Affective functioning
people become irritable, moody, or emotionally reactive
emotional regulation is impaired- tend to overreact or respond inappropriately
harder to read other peoples’ emotions or show empathy
examples of effected Affective functioning
snapping a friends
misreading social cues
feeling overwhelmed easily
effects of partial sleep deprivation on Behvioural functioning
slower reaction time, reduced motor skills, more mistakes
more risky behaviour- crossing roads dangerously, especially when distracted
more school lateness, injuries, inattentiveness, and disruptive behaviour in kids
sleep inertia
grogginess after waking up- can last minutes to hours and affects alertness
excessive sleepiness
trouble staying awake, feeling drowsy during the day
fatigue
low energy and reduced motivation
microsleeps
brief, involuntary episodes of sleep (1-15 seconds)
can be extremely dangerous if driving or working
effects of partial sleep deprivation on Cognitive functioning
attention is impaired- especially boring or repetitive tasks
harder to do complex thinking, make decisions, or solve problems
trouble with simple, monotonous tasks
impaired memory- trouble encoding
problems with short-term memory
factors influencing sleep deprivation (5)
how much sleep was lost
when and why the loss occurred
how often it happens
for how long it continues
the person’s age, health, lifestyle
sleep disturbance
any problem that interrupts your normal sleep-wake cycle, such as:
trouble falling asleep
waking up too often during the night
unusual behaviours during sleep
sleep disorder
more serious than just one-off bad night, it
happens often
distrupts sleep patterns
interferes with everyday functioning (e.g. feeling tired/moody/unmotivated)
types of sleep disorders
primary
secondary
primary sleep disorder
sleep issue is the main problem
not caused by another condition
e.g. insomnia
secondary sleep disorder
sleep problem is a symptom of another issue
could be caused by medical issues, mental health, drugs
e.g. poor sleep due to chronic back pain or anxiety
sleep problems can affect
your emotion (mood swings, irritability)
change your behaviour (slower reaction, poor performance)
hurt your thinking (poor memory, lower concentration)
risks of ongoing sleep problems
mental illness
physical health issues/ problems
Main changes in sleep over lifespan
total sleep time decreases with age
REM sleep drops quickly after birth, then stays fairly stable
NREM stage 3 gradually decreases with age- can disappear especially in men
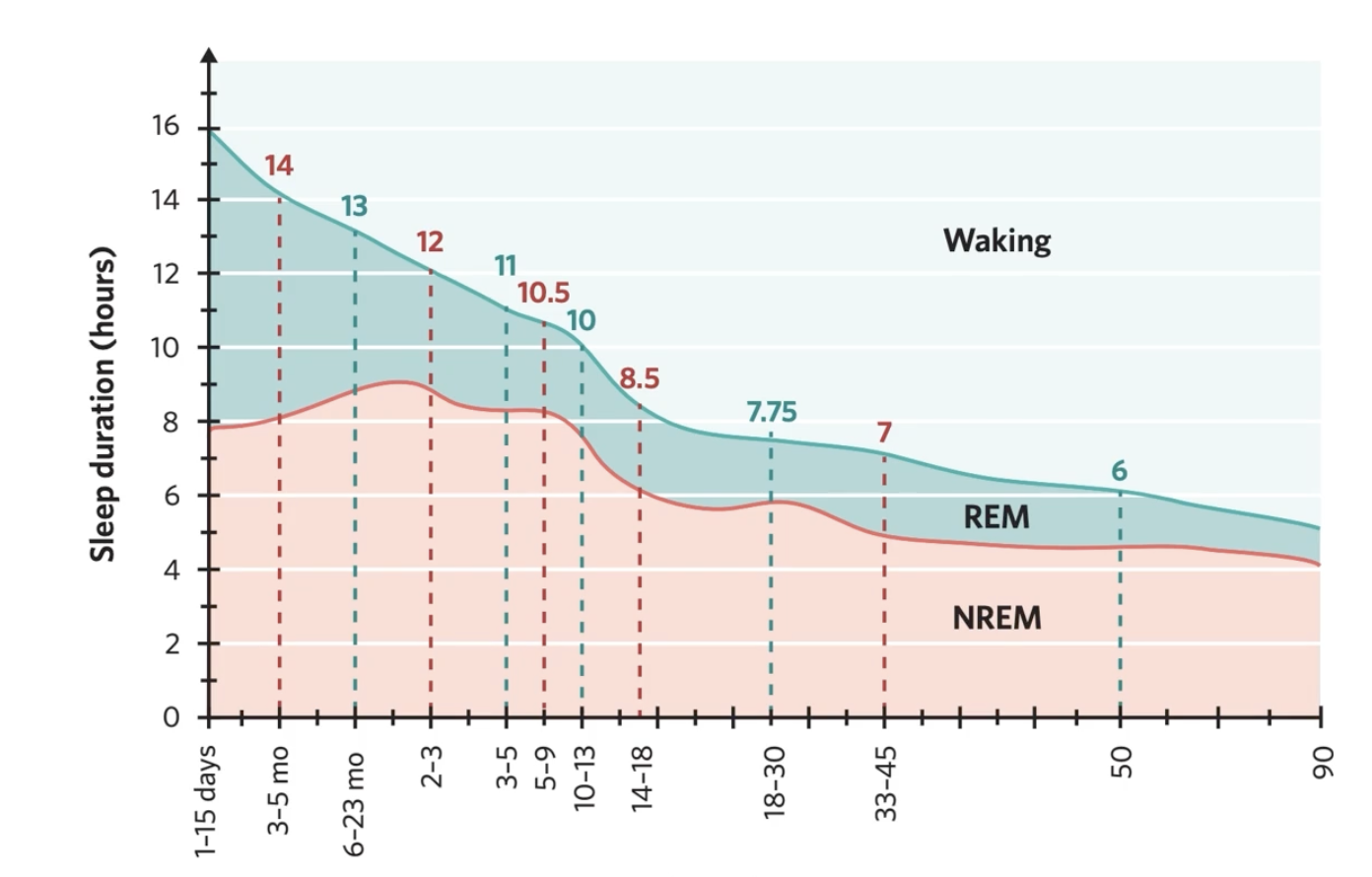
Sleep in newborns & infants (0-2 years) (6)
approx 16 hours a day (in short bursts)
REM = about 50% of total sleep
shorter cycles, only 1 or 2 per episode
sleep onset often starts in REM
very active REM
circadian rhythms not developed until 2-3 months
sleep in children (2-10 years)
11-13 hours a day
NREM stage 3 is very high
hard to wake during stage 3
may skip first REM cycle due to strong deep sleep early in the night
sleep as children grow
REM % slighty decreases
deep sleep starts to reduce after about 10 years
sleep in adolescents (10-18 years)
about 9-10 hours
biological sleep-wake shift → feel sleepy later
lifestyle = less sleep
irregilar sleep patterns
stage 3 sleep drops about 40%
most teens are sleep deprived due to
internal factors
biological clock shift
external factors
school, tech, social life
Sleep in Adults (18-60 years)
about 7-8 hours
20-25% REM sleep
stage 3 sleep gradually decreases
by age 60, half as much stage 3 as at 20
stage 3 can disappear entirely
sleep becomes more fragmented (light, frequent waking)
Older adults (60+ years)
about 6 hours sleep
little to no stage 3 sleep
mostly stage 2 sleep
sleepier earlier in the evening, wake earlier
frequent naps- sleep often interrupted
why do older adults wake often throughout the night
less deep sleep
health issues, meds, reduced melatonin
less exposure to natural light & social cues
NREM Sleep
a type of sleep characterised by a lack of rapid eye movement, and subdivided into three different stages
REM Sleep
type of sleep characterised by rapid eye movement, high levels of brain activity, and low levels of physical activity
sleep cycle features
each lasts around 90 mins
cycle includes
NREM stages 1 → 2→ 3→2
then REM sleep
sleep cycles as night progresses
stage 3 (deep sleep) decreases
REM sleep periods become longer and more frequent
NREM Stage 1 (N1)- light sleep (6)
entry into sleep → transition from wakefulness
duration is about 5 mins (4-5% of total sleep)
brain waves: theta
low arousal threshol- easy to wake
heart rate and body temp drop; hypnic jerks may occur
may feel like you haven’t slept if woken
NREM Stage 2 (N2)- light/moderate sleep
10-25 mins at first → increases in later cycles
slower brain waves, sleep spindles, and K composition
harder to wake than N1
makes up about 50% of total sleep
NREM Stage 3 (N3)- deep sleep
about 20-40 minutes in the first cycle, less in later ones
over 50% delta brain waves
highest arousal threshold → very hard to wake
sleep interia if awoken
important for physical restoration, immune system, growth hormon release
make up about 10-15% total sleep
REM Sleep
about 20-25% total sleep
brain is very active, similar to being awake (beta-like waves)
body experiencing paralysis of skeletal muscles, except eyes and small twitches
breathing, heart rate, blood pressure increase and often irregular
dreaming very common
REM Dreams
narrative, vivid, emotional
NREM Dreams
more thought-like or abstract
Sleep latency
time it takes to fall asleep after trying
Sleep onset
moment a person transitions from awake to asleep
Hypnic Jerk
sudden muscle spasm as you fall asleep (N1)
Sleep inertia
grogginess/ confusion after waking from deep sleep
delta waves
slow, high-amplitude brain waves (seen in N3)
paradoxical sleep
REM Sleep- high brain activity, paralysed body
biological rhythms
natural, repeating cycles in the body and brain
controls physical functions and behaviours
biological clocks
internal timers that regulate rhythms
found in nearly every cell
“Master Clock”
located in the brain and coordinates all the body’s clock to keep them in sync
Circadian Rhythms
approx. 24 hours
endogenous but influenced by exogeneous cues like light, clocks, meals
e.g. sleep wake cycle, body temprature, cortisol levels
Suprachiasmatic Nucleus (SCN)
structure in hypothalamus that regulates an individual’s sleep-wake pattern and helps to release melatonin
controls circadian rhythm
pineal gland
responsible for the production and release of melatonin
Ultradian Rhythms
less than 24 hours
e.g heart rate, breathing, eating pattenrs, hormone bursts
sleep cycle is a key rhythm
Sleep as an ultradian rhythm
one cycle is about 90 mins
repeats 4-6 times a night
alternates between REM and NREM sleep
Suprachiasmatic Nucleaus Features
located in hypothalamus
master biological clock
recieves light info from optic nerves
sends signals to the pineal glands to control melatonin production
How does the SCN help to regulate sleep-wake cycle
light is detected by the eyes
stimulates the SCN in the brain
SCN sends signal to the pineal gland
melatonin hormone is released to the brain
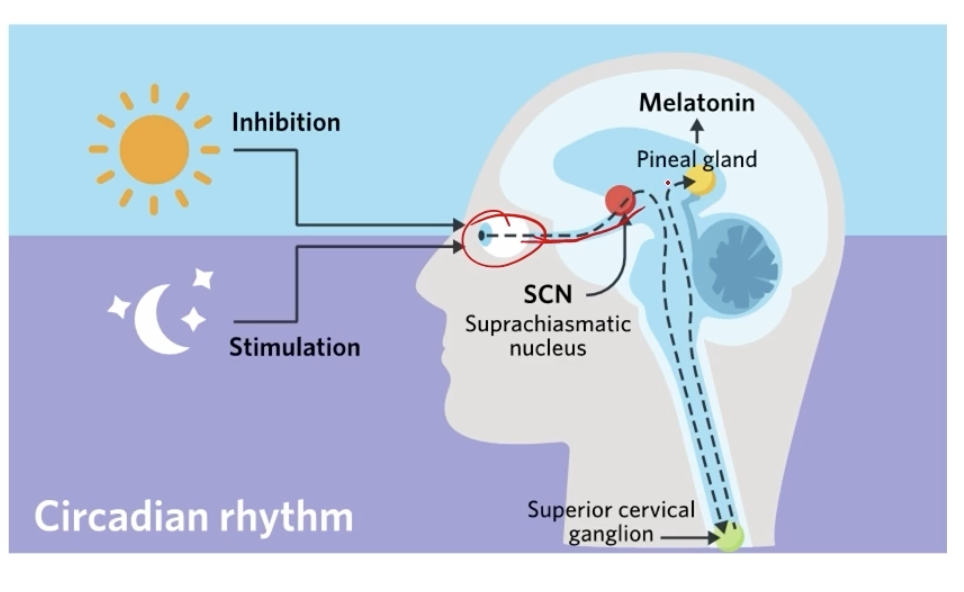
Meltonin
hormone that make the brain feel sleepy
produced by the pienal gland, regulated by the SCN
more meltonin= more drowsy
less light= more melatonin
morning light= melatonin drops= wakefulnes
often referred to as “dracula of hormones”- only come out in the dark
objective
not influenced by personal feelings or opinions in considering or representing facts
subjective
based on or influenced by personal feelings, tastes, or opinions
Physiological Measurements (Objective)
used to gather quantitive data on the body’s internal functions during sleep
brain acitivty (EEG)
muscle activity (EMG)
eye movement (EOG)
heart rate, breathing, temprature, body postition, snoring, etc.
Sleep Diaries (subjective)
used for self-reporting patterns of sleep/ wake behaviour
bedtime
quality of sleep
Video Monitoring
used to observe external behaviours during sleep
sleepwalking
movements
nightmares
Electroencephalogram (EEG)
measures electrical activity in the brain