Leishmaniasis - Epidemiology, pathology & immunology
1/21
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
22 Terms
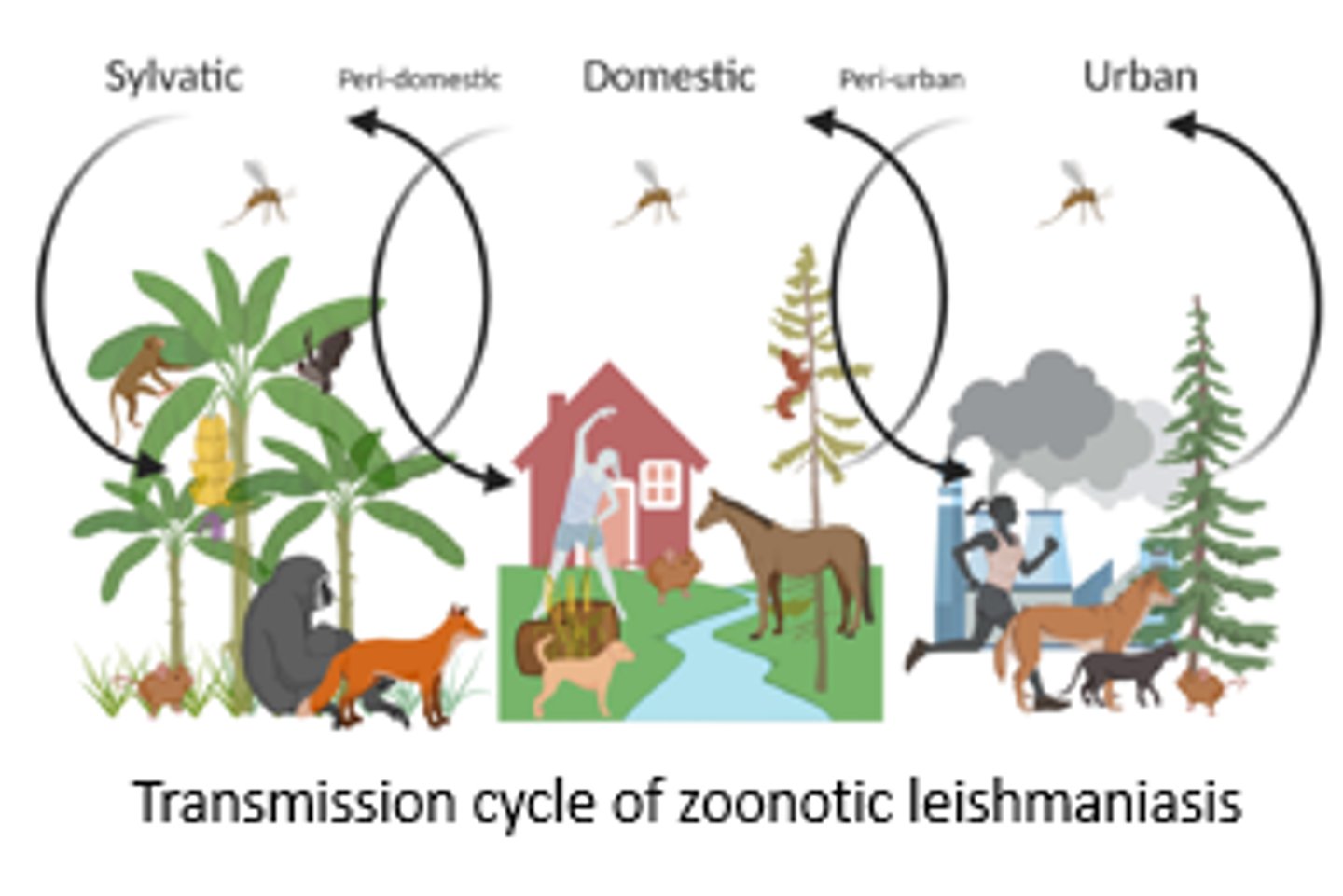
Epidemiology of leishmaniasis
•Leishmaniasis is the 3rd most important vector-borne disease after malaria and lymphatic filariasis.
•Majority of leishmaniasis are zoonoses (reservoir in animals -> spread to humans)
•L. tropica is an anthroponotic species (main reservoir in humans -> spread to animals).
•Deterioration of eco-systems by humans contribute to the spread of the disease.
Increased risk factors for contracting leishmaniasis:
•Sex (male↑)
•Poverty (open houses, mud or straw huts, mud floor)
•Poor sanitation
•malnutrition
•Living in close proximity to animals (livestock, dogs)
•Dog ownership
•Living in overcrowded households
•Migration into endemic area
•Urbanization management (close to sandfly breeding grounds)
Canine Leishmaniosis
Not all dogs show clinical signs (resistance for some breeds)
Signs of CanL in symptomatic dogs:
•Weight loss
•Skin lesions (mostly head, paws)
•Lymphadenopathy
•Fever
•Anaemia
•Splenomegaly
CanL an emerging disease?
•Cases of CanL in dogs UK (non-endemic) has increased
- Even transmission from dog to dog in one UK household has been described
•In Spain seroprevalence rates in stray dogs in Madrid is on the increase
•Asymptomatic dogs can transmit the disease
•Epidemic outbreak of CanL in Colombia caused by L.braziliensis and L.panamensis in 2012
Feline leishmaniosis
-Feline leishmaniosis is sporadically reported worldwide.
-Caused by L.infantum in Southern Europe, but also found were L. amazonensis (Brasil), L. major (Portugal), L. mexicana (USA), L. braziliensis (Brazil).
- Often asymptomatic unless immunocompromised.
live stock
- recent study in Iran looked at Leishmania infections in their livestock
=> Identified L. infantum and L.major
-Horses are equally affected = cutaneous lesions in neck, legs, scrotum.
-> caused by L. infantum in Old World;
-> L. braziliensis, L. panamensis, L infantum in the New World
Wildlife => sylvatic reservoir
Reservoir hosts for L. panamensis and L. guyanensis are dog, sloth, opossum, ant eater.
Clearing forests for frontier farming
-> edge of natural foci with human dwellings
-> spillover of L. guyanensis into peri-domestic transmission cycle in Brazil.
Coffee plantations in New World do provide new places for Leishmania transmission
Prevention methods
1. personal protection
2. Vector population control
3. Reservoir population control
personal protection (sandfly bite)
- Insecticide treated bed nets (LLINs)
•Long clothing/ no exposed skin -> insecticide impregnated fabrics
•Use of ectopic insecticides
•Prevent going outdoors between dusk and dawn.
Cutaneous leishmaniasis (CL):
• Involves skin epithelial cells at site of sand fly bite => skin lesions on exposed body parts
• caused by L. tropica, L. major complexes (Old World) and L. mexicana, L. braziliensis complexes
(New World)
• self healing after months to years often with scaring.
• Often multiple lesions in close proximity

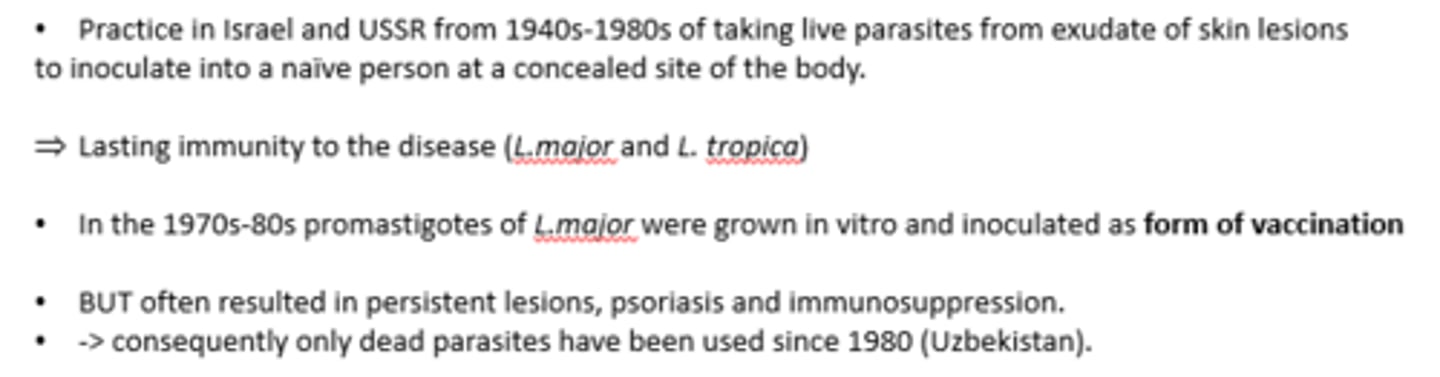
Leishmanization
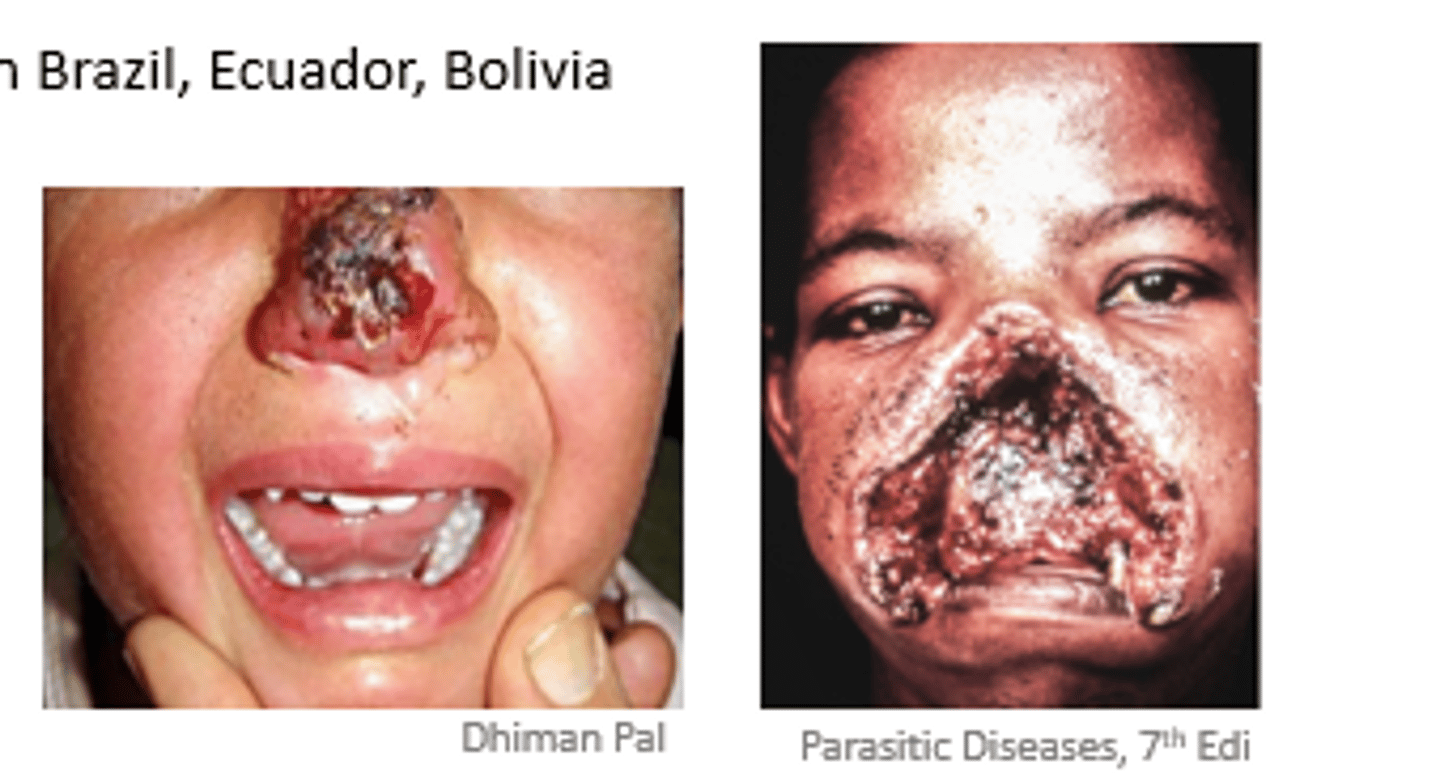
Mucocutaneous Leishmaniasis
•Caused by infection with L. braziliensis complex
•BUT <10% of infected people develop mucocutaneous form of the disease (patient’s age and nutritional status can increase risk)
•From a primary cutaneous bite parasites inside macrophages metastasize to mucocutaneous junctions (oral cavity, urogenital, anal areas) -> erode soft tissue
•Where? Mucocutaneous belt = Northern Brazil, Ecuador, Bolivia
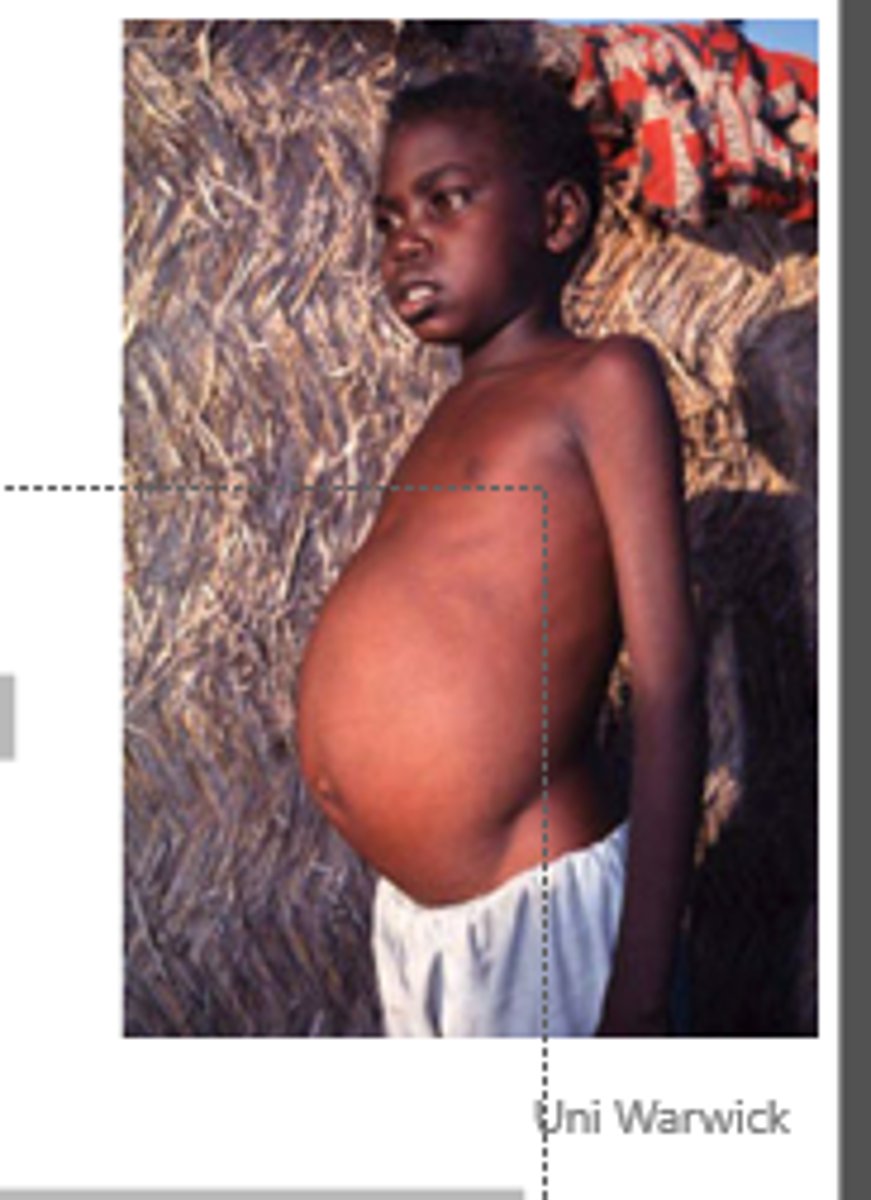
Visceral Leishmaniasis (Kala-azar)
•Involves endothelial tissue, liver, spleen and bone marrow
•caused by L.donovani and L.infantum (Old world) and L.infantum (New world)
•Fatal if left untreated
•Incubation period of 3-6 months
•fever, weight loss, lymphadenopathy, anemia; later hepatosplenomegaly with darkening of skin
•Cause of death is a compromised immune system => co-infections
Diagnostics
1. Parasitological:
•Microscopic examination of bone marrow or splenic aspirate, buffy coat samples or tissue sample from CL
•Parasite isolation and culture in vitro, or in vivo
2. Serology
•ELISA
•Lateral flow strips (with rK39 antigen) VL
•Fluorescent antibody test
•Direct agglutination test (DAT) -> promastigotes get agglutinated in presence of Ig
3. Molecular
•PCR and qPCR
Treat ment options
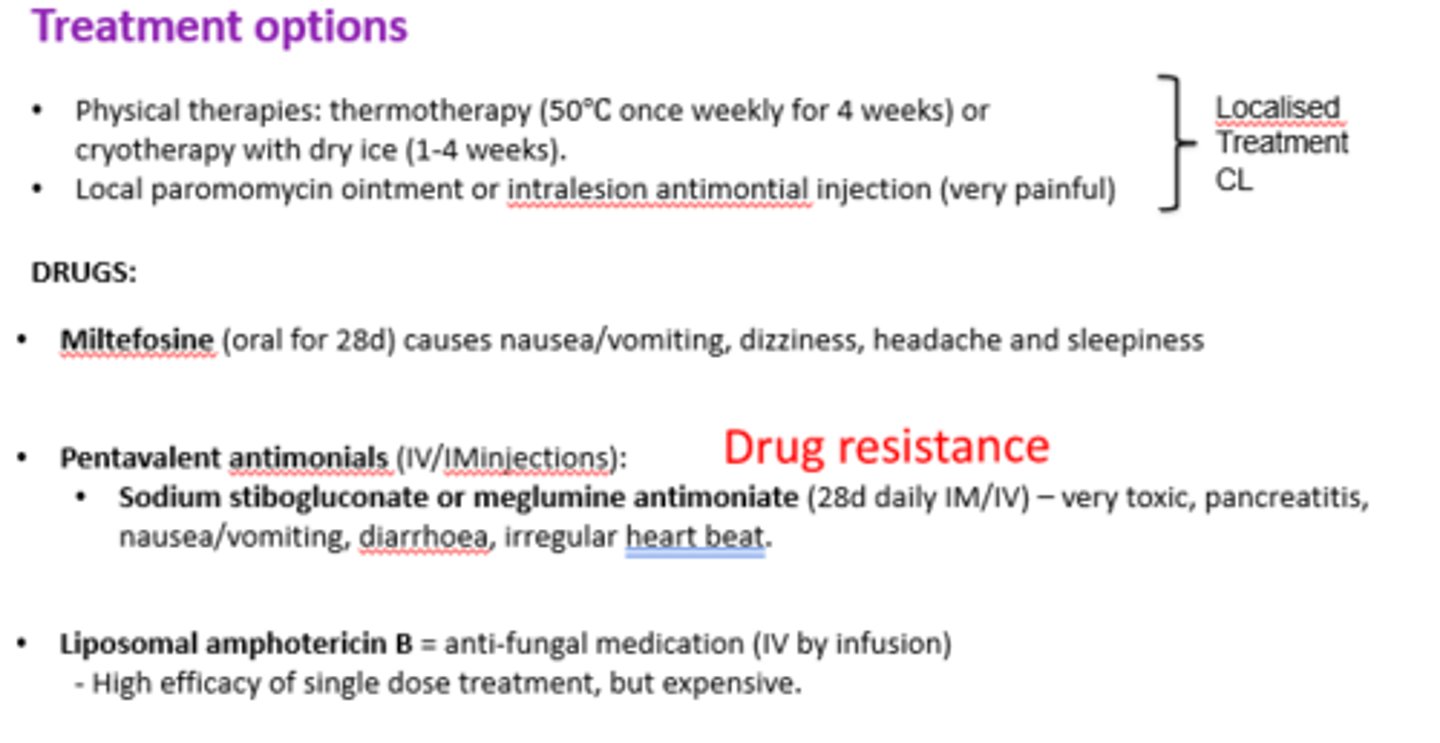
Treatment of CanL
-Drugs in use might improve symptoms but they will not eliminate the infection
-Same drugs as used in humans!
•Pentavalent antimoniate (methylglucamine antimoniate) injections for 4-6 week
•Allopurinol (oral) until clinical signs disappear (potentially lifetime)
•Miltefosine (oral) for 4 weeks
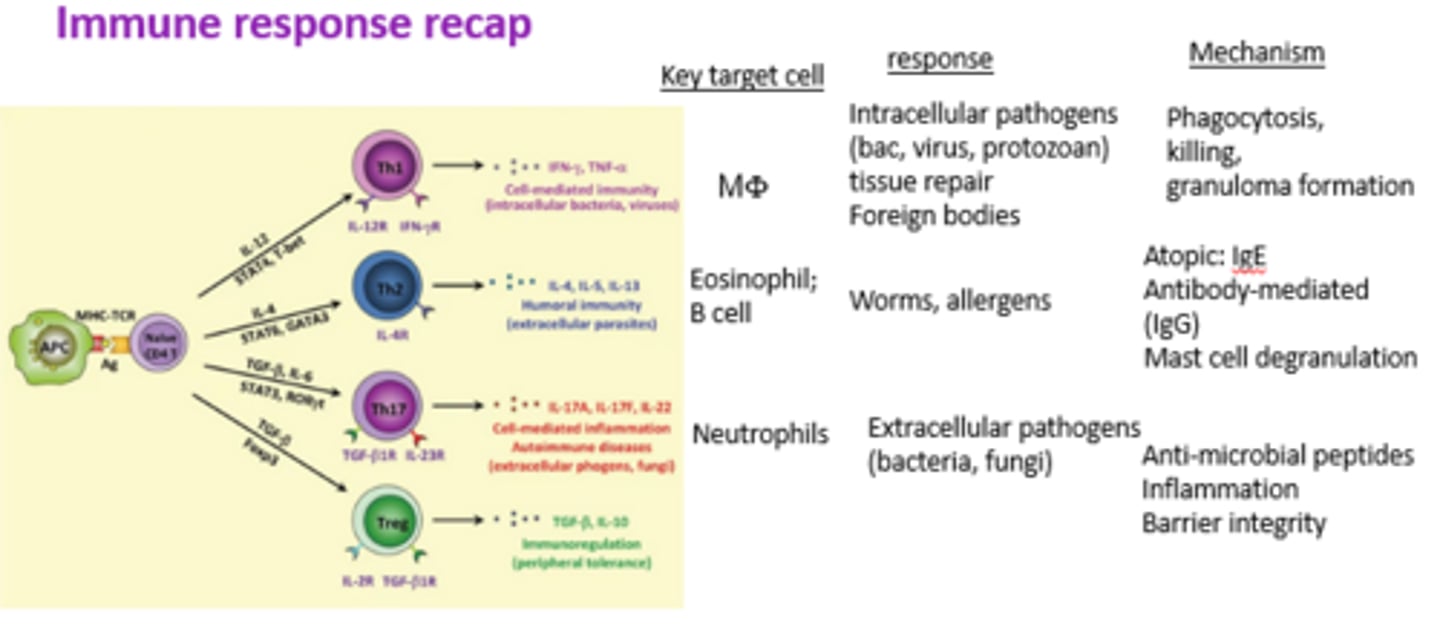
Immune response to Leishmania
•Parasite replicates in macrophages
•Persistence in tissue leads to chronic infection
•Outcome of the disease depends on the host inflammatory response
Immune response recap
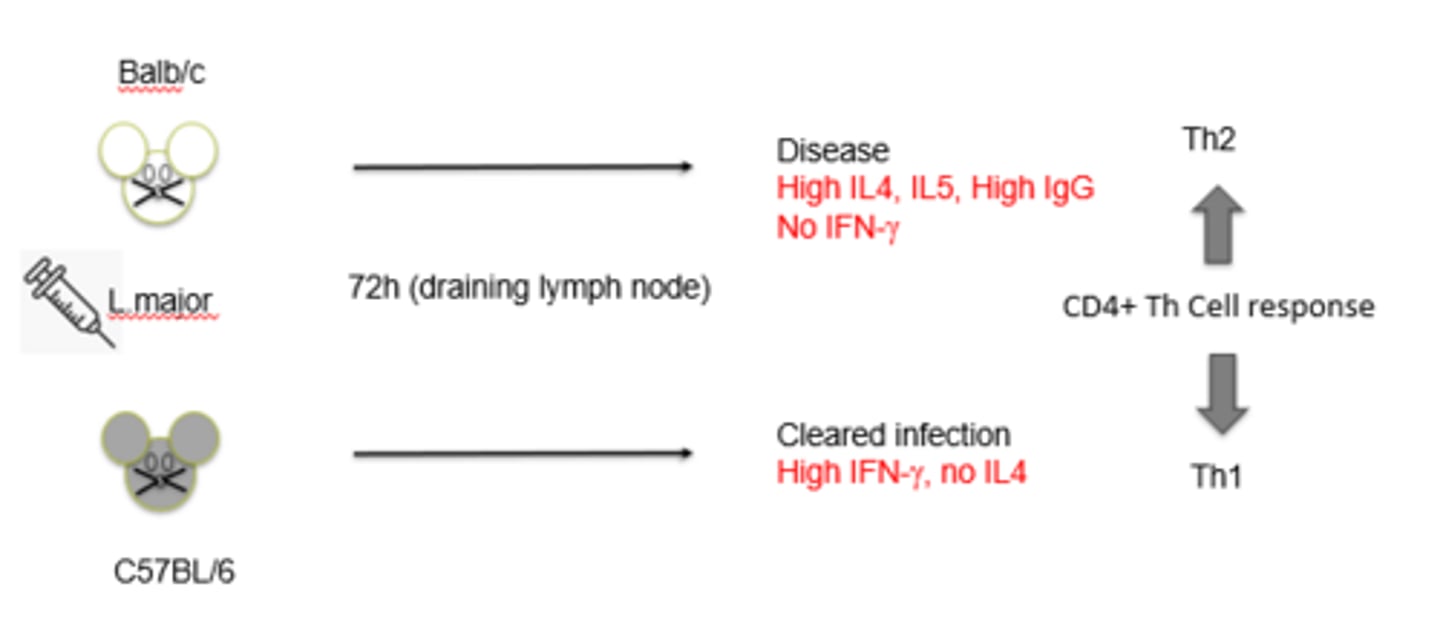
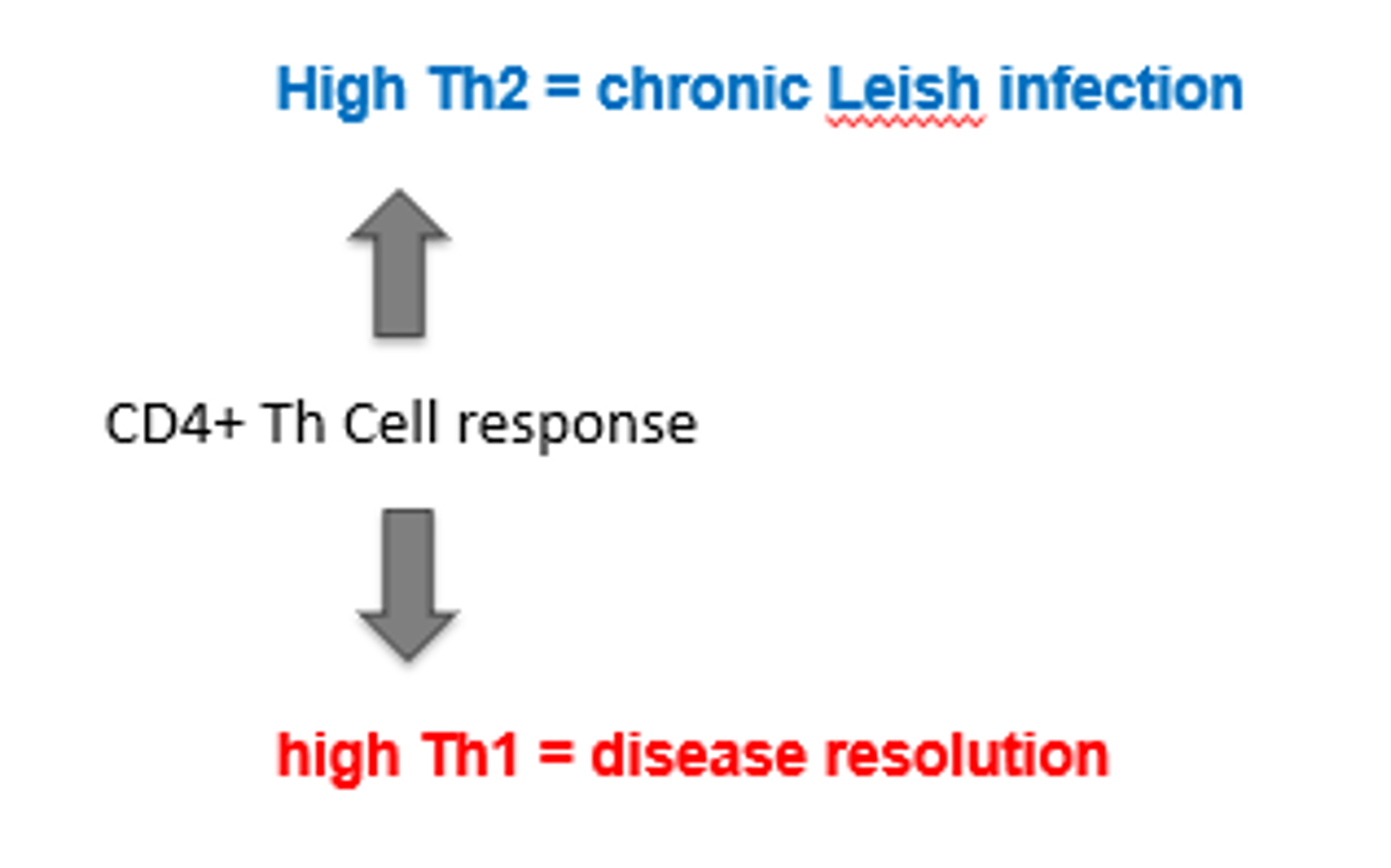
T helper subsets control disease outcome
T helper subsets control disease outcome 2
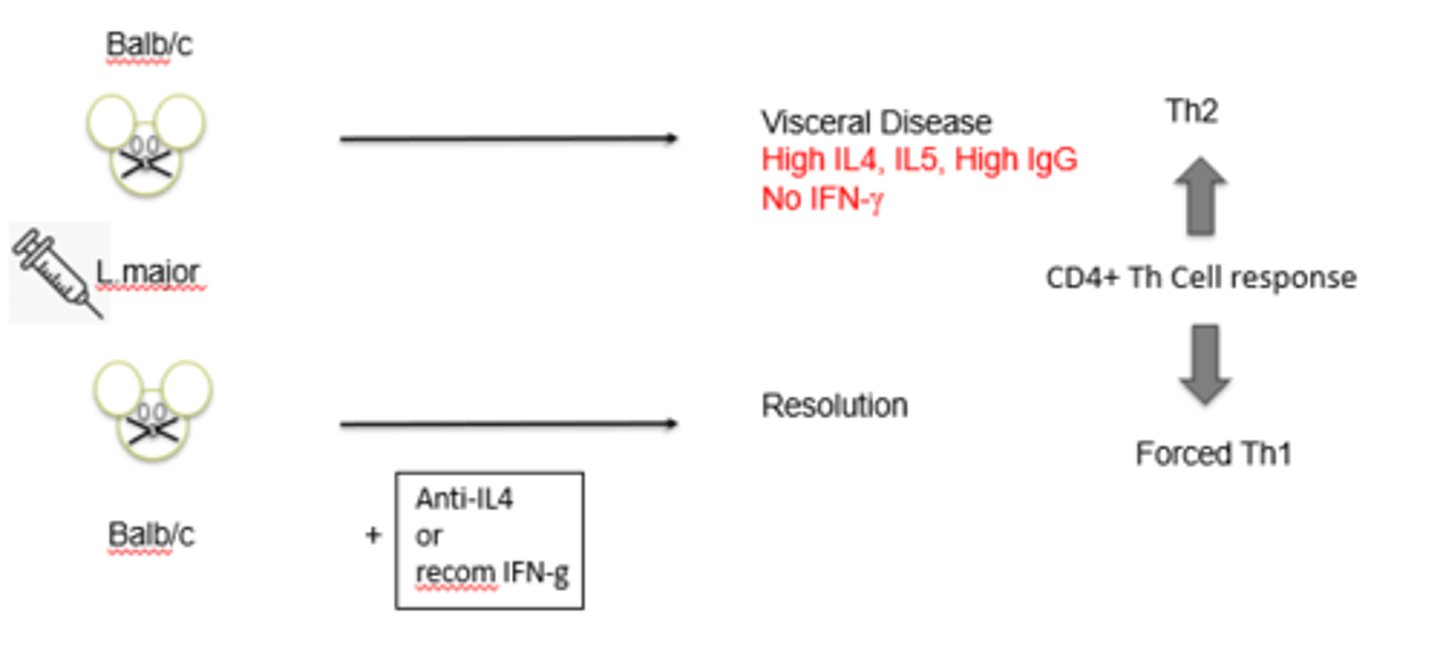
Leishmaniasis is a spectrum of disease, depending on the balance of Th1/Th2 immune-response
How does Leishmania manipulate the host immune system?
-Impairment of antigen presentation
-Impairment of proinflammatory cytokine secretion
-Inhibition of NO production (blocking iNOS)
-Induction of immunosuppressive IL10, TGF-b