Critical care
1/30
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
31 Terms
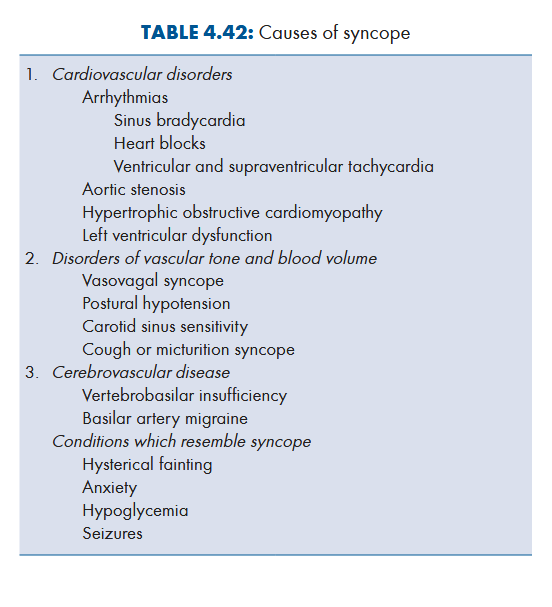
Causes of syncope
Syncope due to AV block
Stokes-Adams attack
Investigations to be done for syncope
ECG, echo, Holter ECG and electrophysiological studies to diagnose cause
Upright tilt test: confirms diagnosis of vasovagal syncope
EEG, CT, MRI: diagnose neurological cause
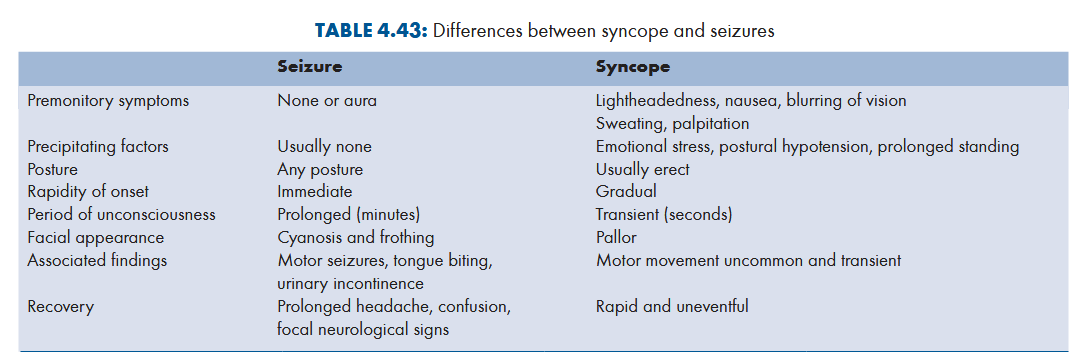
Differentiate seizures from syncope
Treatment of syncope
Immediate action
Place patient in supin postion with head tilted to side to maximise cerebral blood flow
Peripheral stimulation like sprinkling cold water over face
Clothing should be loosened
Patient should not be allowed to rise again till weakness no longer persists
Instructions:
Avoid situations causing syncope
Try to assume recumbent position as soon as they feel premonitory symptoms
What is cardiac arrest
Abrupt cessation of cardiac pump function
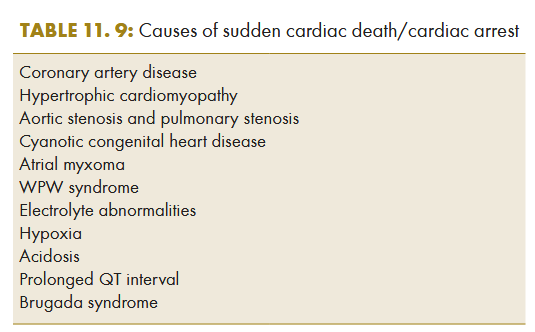
Causes of cardiac arrest
Management of cardiac arrest
Initial response and basic life support
Defibrillation
Advanced life support
Postresuscitation care
Long-term management
Sequence to be followed during resuscitation of an adult
Assessment of unreponsiveness
Activation of emergency medical services
BLS until defibrillation is available
Defibrillation if indicated
Intubation
Administration of appropriate medicine
What is ACLS
Consists of ECG monitoring, endotracheal intubation and setting up IV line in large peripheral vein or central vein
Immediate therapy: defibrillation, O2 and cardioactive drugs
Immediate defibrillation to be performed if ECG reveals abnormality in rhythm. If unsuccesful, patient is intubated and IV line is set up while circulation is supported by external chest compressions
IV epinephrine results in vasoconstriction and increase CO to brain
Clinical features of Hypovolemic shock
Mild hypovolemia (loss of < 20% of blood)
Anxiety and tachycardia
Moderate (20-40% blood lost)
Tachycardoa, tachpnea and postural hypotension
Severe (> 40% loss of blood)
Hypotension
Tachycardia
Tachypnea
Oliguria
Signs of reduced cerebral perfusion: agitation, confusion, drowsiness, coma
Cold and clammy extremeties
Reduced central venous pressure
Multiple organ failure
Diagnosis of hypovolemic shock
History of blood loss or fluid loss
Occult blood loss should be considered
Measurement of hemoglobin and hematocrit may be normal and hence misleading
Management of hypovolemic shock
Assess ABCs
BP, pulse rate, RR, urinary output, arterial O2 saturation and mental status should be monitored
Volume resuscitation: isotonic saline or Ringer’s lactate given through rapid IV infusion. Blood transfusion or packed cell transfusion required when there is continuing blood loss and hemoglobin < 10 g/dL. Infusion of inotropic agents such as dopamine, dobutamine or vasopressin may be required to maintain CO
Supplemental O2 and endotracheal intubation (if needed)
What is neurogenic shock
Caused by traumatic high spinal cord injury, spinal anesthesia or head injury
Warm extremeties (venodilation)
Vagal stimulation: increase in parasympathetic tone leading to hypotension, bradycardia and syncope
Management
Norepinephrine
Correction of hypovolemia
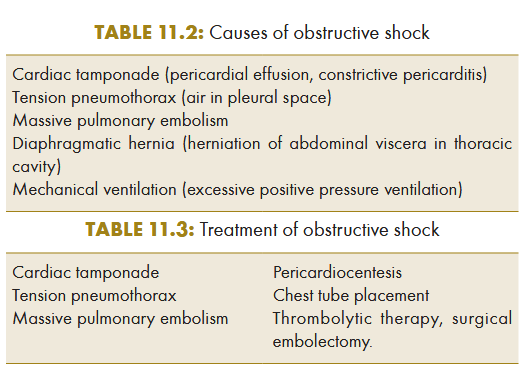
Causes and treatment of obstructive shock
Clinical features of septic shock
Fever, chills, hypotension, altered mental status and features of end organ failure
Hypoperfusion of brain: encephalopathy causing restlessness, confusion, delirium and coma
ARDS: due to pulmonary oedema
Acute renal failure and acute tubular necrosis
Increased levels of serum bilirubin and hepatic enzymes
DIC
Causes of septic shock
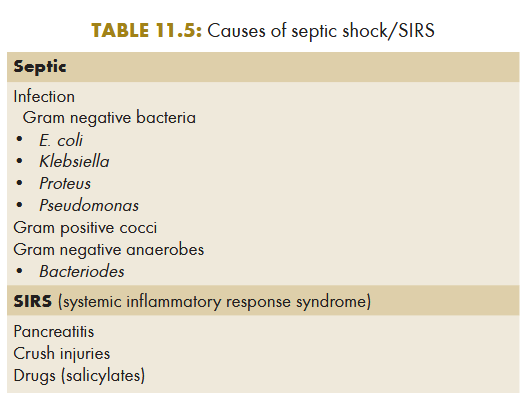
Investigations to be done for septic shock
Blood culture
TLC: leukocytosis (polymorphonuclear leukocytosis)
Increase serum urea and creatinine (renal dysfunction)
Increased bilirubin and hepatic enzymes
Low platelet count, increased PT and aPTT (DIC)
Arterial blood gas analysis: hypoxia and metabolic acidosis
CXR: signs of ARDS
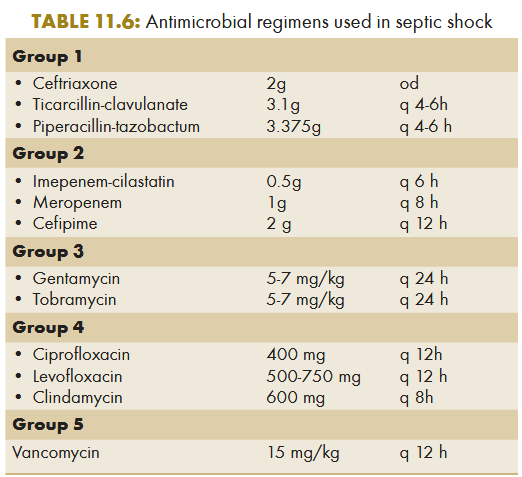
Management of septic shock
Empirical therapy with broad spectrum antibiotics (one from group 1 or group 2 + 3)
Fluid administration is usually required to correct hypotension: monitorred by measuring CVP
Inotropic or vasopressor agents may also be given for hypotension
Associated with relative adrenal insufficiency: hydrocortisone (50 mg 6 hourly for 5-6 days)
Drotrecogin alfa (activated human protein C) as continous infusion of 24 mcg/kg/hr for 96 hrs
Causes of cardiogenic shock
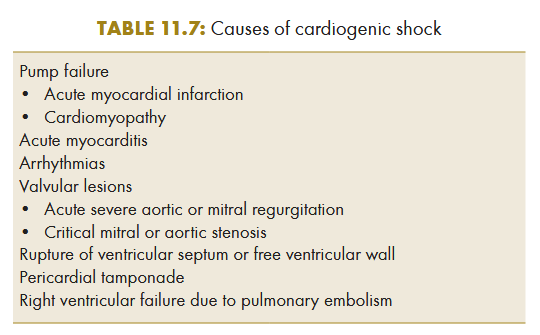
Clinical features of cardiogenic shock
Arterial hypotension
Weak and rapid pulse
Cold extremeties and cyanosis
Oliguria
Altered mentation
If associated with MI: severe chest pain, dypnea, anxiety, sweating, S3 gallop and systolic murmurs
If associated with LVF: raised JVP and pulmonary rales
Investigations to be done for cardiogenic shock
CXR, ECG and echo
Management of cardiogenic shock
O2 inhalation to maintain PaO2 of > 60 mmHg. Endotracheal intubation and mechanical ventilation may be required
Hematocrite maintained at > 30%
Fluid replacement to maitain preload and ventricular function
Pressors post adequate fluid resuscitatin
Dopamine: variable effects according dose (low: increases GFR, moderate: increases myocardial contractility and HR, high: vasoconstriction)
Dobutamine (2-20 mcg/kg/min). May be combined with amrinone or milrinoma
Norephinephrine: 2-10 mcg/min
Aortic counterpulsation
Treatment of underlying cause
Clinical manifestations of anaphylaxis
Skin lesions: urticaria, angioedema
Respiratory distress due to laryngeal edema, laryngospasm or bronchospasm (feeling of tightness of chest, stridor and wheezing)
Hypotension and shock: cold extremeties, decreased urinary output, peripheral cyanosis and altered sensorium
GI manifestations: abdominal cramps, nausea, vomitting, diarrhea
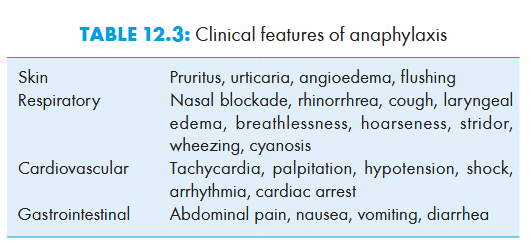
Diagnosis of anaphylaxis
Clinical
Based on history
Elevated serum tryptase during episode confirms diagnosis
Treatment of anaphylaxis
Adrenaline 0.3-0.5 mg IM or SC. Repeated injections can be given at 20 min intervals if needed
Higher dose + glucagon may be needed in patients on beta blockers
Airways management: 100% O2 to be administered
If laryngeal edema doesnt respond to epinephrine: tracheostomy
Bronchospams: inhalation of beta 2 adrenergic agonists (terbutaline, salbutamol) and IV aminophylline
IV fluids to maintain instravascular vol
Hypotensive patients: vasopressors (dopamine, norepinephrine)
H2 receptor antagonists (diphenhydramine, promethazine) useful in relieving skin symptoms and abdominal cramps
Glucocorticoids may reduce prolonged reactions or relapses (hydrocortisone 200 mg or methylprednisolon 125 mg IV)
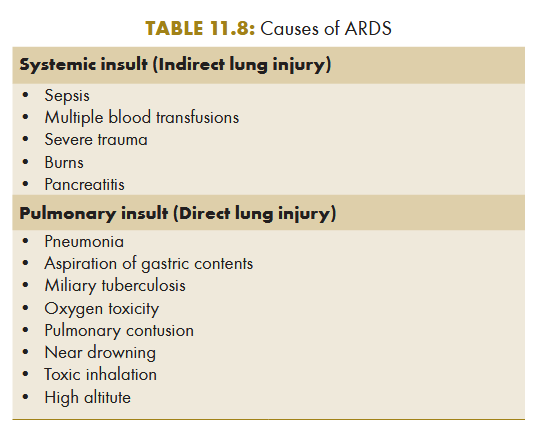
Causes of ARDS
Clinical features of ARDS
Rapid onset dyspnea following causative agent within 12-48 hrs
Tachypnea, labored breathing and intercostal retraction
Crepts on auscultation
Multiorgan failure
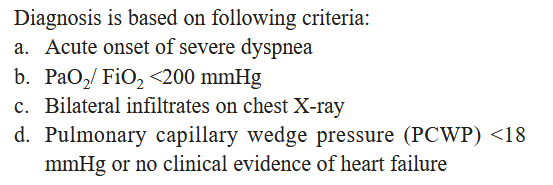
Diagnosis of ARDS
Investigations to be done for ARDS
CXR PA view
Arterial blood gases
Hemogram
Blood sugar, urea and serum creatinine
LFT
Serum amylase/lipase
Treatment of ARDS
Recognition and treatment of cause
Minimising invasive procedures
Venous thromboembolism prohylaxis
Management of nosocomial infection
Mechanical ventilation: Positive pressure mechanical ventilation with lowest level of PEEP and supplemental oxygen required to maintain the PaO2 above 60 mmHg or SaO2 above 90% is used. Volume cycle ventilation with small tidal volumes have been shown to reduce mortality over standard forms of mechanical ventilation.