Lecture 17 - Copper Part 2, Alfatoxin
1/48
Earn XP
Description and Tags
required reading: list of liver protectants
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
49 Terms
What criteria is part of diagnosis for copper toxicity? hint: signalment, lesions, tests
appropriate source, species (sheep!)
GIT, liver, RBC, kidney
consider liver enzymes, liver biopsy, copper concentration in liver, NOT serum copper
histologic lesions PM to differentiate primary vs secondary
Cu analysis: liver, kidney, feed

Prognosis for Cu toxicity is ___ for clinically affected LA and SA.
guarded to poor
Cu toxicity in production animals are typically ____.
not treated due to cost
With SA, what can be used a treatment for Cu toxicity?
liver protectants, fluids-blood transfusion, corticosteroids, analgesics
The best treatment and prevention of copper toxicity is to ___ ____ ____ via what methods?
enhance copper excretion
Mo-S source to enhance excretion, Zn which competes for GI absorption, chelators to decrease body burden
What is the purpose of a Mo-S source?
Enhance fecal, urinary, biliary excretion AND slows down absorption
What element(s) will compete for GI absorption with copper?
Zn, Fe, Se
What chelators are used in SA copper toxicities? LA copper toxicities?
SA: D-penicillamine
LA: tetrathiomolybdate
others: trientine, BAL
Copper storage disease is __ on the top 5 liver conditions in dogs!
3rd
Copper storage disease was previously called ___.
chronic active hepatitis
Copper storage disease will present around ___ ages and will have signs of what
>2-4 years of age
chronic, intermittent heaptitis: anorexia, vomiting, weakness, lethargy, weight loss
Copper storage disease is historically considered a hereditary disease, inherited ___ in ____ and also seen in ____.
autosomal recessive, Bedlington terrier
West Highland white terriers

Other than the breeds classically associated with copper storage disease, other breeds such as ____ have been affected so other than genetics, secondary problem due to ___ or ____.
dobermans, Skye terriers, labs, mixed etc
hepatitis, too much copper in diet
The best diagnostic indicator for copper storage disease is ____ and ____ at the time of clinical disease and _____.
liver enzyme elevations, elevated bilirubin concentrations
liver biopsy histology lesions + copper levels
How do you treat a dog with copper storage disease?
chronic administration of chelator to reduce body burden → D-penicillamine, or trientine, tetrathiomolybdate as alternative
reduce absorption long term → zinc acetate
List common options for liver protectants
*required reading
S-adenosylmethione (SAMe)
silymarin: extract from milk thistle, silybin active component
Denamarin: SAMe & silybin
Denosyl: SAMe & glutathione
HepatoAdvanced: SAMe & silbyin & Vit E
N-acteylcysteine
Ursodiol
Vitamin E and/or selenium
What are mycotoxins?
secondary metabolites of fungi or mold that is harmful

The synthesis of mycotoxin is determined by ____ and the mold growth is determined by what factors?
mold genetics
substrate composition and texture, temperature, oxygen tension, moisture-humidity, pre-existing damage to feed
NOT ALL MOLDY FEEDS CONTAINS ____
mycotoxins - feed does not need to be moldy to have toxin present
NOT ALL FEEDS THAT CONTAIN MYCOTOXINS ARE ____.
toxic (dose dependent, species dependent, sex age dependent)
lots of fed have ___, to some degree
mold
Never say “I think it may be a ___” because why?
mycotoxin; each mycotoxin causes distinct clinical disease
There is considerable ___ and ___ variation with mycotoxin production
regional, seasonal
True or False? Alfatoxin is NOT a big problem in the PNW
True
What is alfatoxin?
a bisfuranocoumarin compound produced by some strains of Aspergillus flavus, nomius, parasiticus
___ is the precursor in synthesis of alfatoxin. We care about this because?
sterigmatocystin
less toxic than alfatoxin but can cause similar toxicosis
Name the four predominant forms of alfatoxin
alfatoxin B1, B2, G1, G2
What is the predominant form and metabolite of alfatoxin?
aflatoxin B1, and M1 (a primary metabolite and major excretion product in urine and milk)
What are common sources of alfatoxin?
Contaminated cereal grain: especially corn, cottonseed that has been damaged or broken

True or False? Alfatoxin only occurs as storage fungi and develops only when grain is in a storage environment.
False. Alfatoxin occurs as both a field fungi and storage fungi.
True or False? Proper feed processing practices routinely destroy alfatoxins.
False. Alfatoxins are very stable and are not routinely destroyed by most feed processing practices.
Sensitivity to alfatoxins depends on ___, ___, and ___.
species, age, sex
younger, males more sensitive
Aflatoxin toxicity most commonly reported in ___, ___, ___ however many outbreaks occurred in dogs via ____.
cattle, swine, birds
contaminated commercial pet food

What is the mechanism of action of alfatoxins?
potent hepatotoxin, nephrotoxin, immunosupressant, hepatic carcinogen
True or False? Hepatic carcinogens from aflatoxin are more of an issues in residues (milk, meat) and not in humans.
False. Risk is minimal in milk and meat, tightly regulated in production animals due to hepatic carcinogen in humans
Clinical signs of alfatoxin toxicity is related to ___ and is very ___. Acute/chronic signs are more common.
liver, dose-dependent, acute

What are acute clinical signs seen with alfatoxins? Is it more or less common than chronic signs?
vomiting, lethargy, anorexia, weakness, abdominal pain, icterus, if liver failure: petechiation, ascities
more common than chronic signs
What are chronic clinical signs seen with alfatoxins? Is it more common than acute signs?
drop body weight, unthriftiness, drop in production, poor fertility, increase incidence of disease, secondary photosensitization
less common than acute signs
What clinical pathology signs do you see with alfatoxin?
liver damage: elevated ALT, AST, AP, bile acids, hyperbilirubinemia/uria
liver failure: hypocholesteremia, increased PT/PTT, hypoalbuminemia, decreased protein C
renal changes also possible: isothenuria, granular casts, azotemia, glucosuria
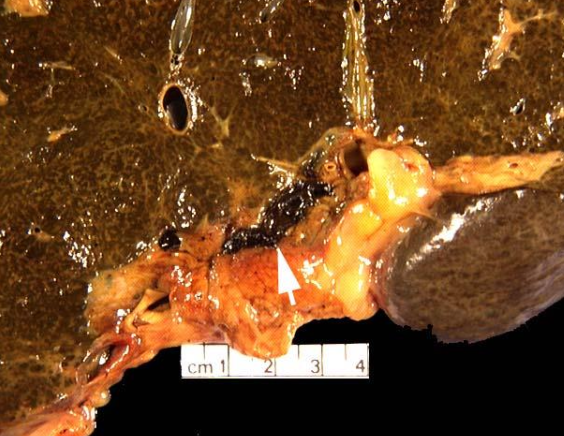
What gross lesions are seen with alfatoxin toxicity? Acute vs chronic changes?
acute: enlarged, friable, heavy, congested, hemorrhagic, icteric liver
chronic: cirrhotic, shrunken
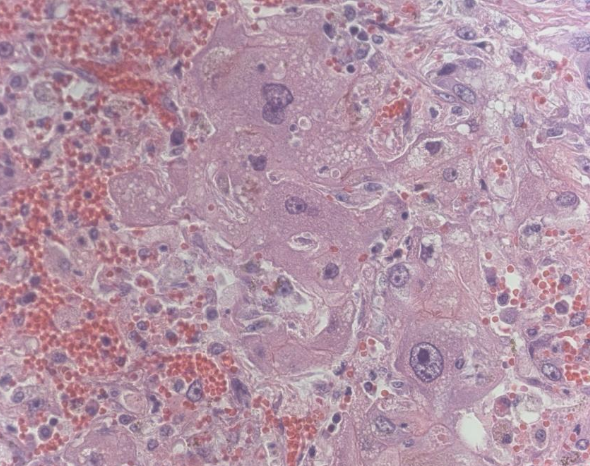
What histologic lesions are seen with alfatoxin toxicity? Acute vs chronic changes?
acute: necrosis
chronic: hepatocytomegaly, biliary hyperplasia, fibrosis
How do you diagnose alfatoxin toxicity? Hint: history, signs, tests
signalment and appropriate feedstuffs (grain)
liver lesions
alfatoxin analysis via chromatography of a representative sample of feed is the best way
What are different methods of alfatoxin analysis? Which is ideal?
liver, kidney, lung - difficult
nonspecific black light screening or ELISA kit screening
chromatography of representative sample of feed is ideal
Remember with regards to chromatography testing of feed, that you may get a “false” negative if:
did not take a representative sample of feed, or
feed containing alfatoxin already consumed/gone by time sampling was done

Dr T says to be careful with what labs?
labs that run feed analysis and also sell binders (conflict of interest)
What is the treatment for alfatoxin toxicity? For LA vs SA?
symptomatic and supportive
LA: not cost effective
SA: liver protectants and supportive
Prognosis for alfatoxin toxicity is ___ however liver has tremendous regenerative capabilities.
guarded
What do you do with all the contaminated feed for livestock?
depends on state, aluminosicilate binders etc
The key for treatment of alfatoxin toxicity is ____.
prevention of mold growth