BIOCHEMISTRY 1: Introduction & Principles of laboratory analysis
1/97
Earn XP
Description and Tags
Pathology and Diagnostics
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
98 Terms
what is the use of clinical biochemistry?
To apply general biochemistry to diagnosis and management of clinical conditions by measurements of blood components
what is the aim of laboratory diagnosis?
Laboratory diagnosis aims to
provide objective data to help prove (or disprove) diagnostic suspects identified by clinical examinations
provide preventative medicine (curing pathologies before manifestation)
Control therapies
What are some areas of laboratory diagnosis
Hematology
clinical chemistry
transfusional medicine
clinical microbiology
clinical microscopy
immunochemistry measurements
immunology
molecular biology
What are some areas of laboratory diagnosis: Hematology
blood cells counts and morphology, and hemostasis
What are some areas of laboratory diagnosis: Clinical chemistry
measurements of analytes in biological fluids (serum, plasma, urine, etc.)
What are some areas of laboratory diagnosis: Transfusional medicine
donors screening (for transmissible diseases eg HIV, hepB)
What are some areas of laboratory diagnosis: Clinical microbiology
microscopy examinations (eg urine or other bodily fluids)
What are some areas of laboratory diagnosis: immunochemistry measurements
hormones, proteins, and others
What are some areas of laboratory diagnosis: Immunology
investigation of cellular or humoral immunity
What are some areas of laboratory diagnosis: molecular biology
DNA investigation and search for mutations or polymorphisms (needed in order to determine predisposition of familiarity to certain pathologies)
What is a core laboratory
A huge laboratory serving more than one hospital in a given area.
What is a centralized laboratory?
A lab serving one hospital. Takes care of measuring all parameters for the patients hospitalized in the given hospital.
What is a specialized laboratory?
Perform special tests. Eg. parameters of a rare disease must be measured and established, but this can only be done at a specialized laboratory. These labs are concentrated on curing 1 specific disease.
What is an emergency laboratory?
Performs tests overnight.
What is point-of-care in lab analysis
“Bedside testing”, uses small equipment typically able to measure one parameter at a time. Most useful for chronic diseases and for self testing at home (eg. measuring glucose levels for diabetes).
What are some indications to prescribe laboratory tests?
confirm diagnosis suspected on clinical grounds (eg suspected diabetes mellitus)
exclude diagnosis of diseases (eg D-dimer to assess embolism)
provide prognostic information (hepatic enzymes in cirrhosis)
monitor treatment efficacy by assessing drugs response (plasma coagulability after anticoagulant treatment)
to screen for diseases (STDs, hereditary anemia)
What are the 3 modalities to ask for laboratory testing
physician asks for profile of the patient. A set of parameters relating to a specific organ or disease
Individual tests
Emergency testing
what should you NOT do when prescribing tests?
Never perscribe test if significance is unknown, can’t draw any meaningful conclusions
Refrain from asking test repeats, unless needed (eg mistake in the lab)
Excess of testing for a given clinical condition may (paradoxically) complicate diagnosis and give rise to false-positive.
what should you do when analyzing test results?
evaluate results in comparison with reference (normal) intervals
combine results with clinical examination
take into account methods used for lab testing to interpret the results
how do we obtain the reference intervals for given parameters?
Reference intervals for any given parameter are calculated from results of a healthy population. The reference range should include 95% of the results of the healthy population.
what is the remaning 5% of individuals who do not range in the normal reference intervals?
You have a 5% chance of false positives or false negatives in healthy subjects.
what are the 5 characteristics of laboratory methods?
precision
accuracy
analytical sensitivity
diagnostic sensitivity
diagnostic specificity
What is precision
Precision is defined as the agreement between repeated measurements made on the same sample. Meaning, the more the values are close to the mean value, the higher the precision.
What do we need to estimate precision?
mean value (M)
standard deviation (DS)
Coefficient of variation (CV)
What is the standard deviation?
Degree of dispersion of the results around the mean value.
what is the coefficient of variation?
Standard deviation related to the mean value of the sample (percentage estimate of precision)
How do we calculate the coefficient of variation?
It is equal to the (standard deviation x 100)/(mean value)
What value should the coefficient of variation be?
0-5% is precise
less than 10% is acceptable
more than 10% is unacceptable
What is accuracy?
Accuracy is the concordance between the “observed” and the “true” value
What is the observed value?
The value measured in the patient (in real time)
What is the true value?
It is the actual value of the parameter which is unknown in most cases, determined by the measurement of the same sample by the gold standard method.
how do we estimate accuracy?
repeated measurements made on the same sample
calculation of the mean value: “observed value”
Determination of the “true value” by measurements on the same sample using a gold standard method
calculate the deviation of the “observed value” from the “true value” as a percentage.
What are the limitations to calculating accuracy?
In most cases, the “true values” are unknown. Or they are assessed with “gold standard methods”, which are usually expensive and not used in daily routine.
What are the 3 types of errors in laboratory methods?
casual
systemic
gross
What are casual errors
random deviations around the mean value which are UNAVOIDABLE
what are systematic errors?
Unidirectional deviations which are AVOIDABLE. Eg. getting results consistently higher than you expect, always in the same direction.
What are gross errors?
Errors that occur due to poor organization, they are EASILY AVOIDABLE.
What is an example of a systematic error?
Improper calibration of the system used for the measurement.
What can cause gross errors?
Usually distraction
how is the method if there is a small deviation between values? what errors are there?
The method is precise and accurate, because the values are very similar. Could be due to a mild casual or mild systematic error (but is very unlikely).
How is the method if values are scattered but around the true value? What error is there?
The method is imprecise but accurate. Could be due to high casual error.
how is the methods if values are all deviated in the same direcion with respect to target? what error is there?
The method is precise but inaccurate. Due to high systematic error (unidirectional deviation)
how is the method if values are all outside of the target? what error is there?
The method is imprecise and inaccurate. Due to high systematic and casual error.
What is analytical sensitivity?
The ability of the method to measure small (trace) amounts of analyte.
What are the 2 types of results (sets of data) from tests?
dichotomous
continuous
What are dichotomous results?
They are positive or negative results, you either have one or the other.
What are continuous results?
They are numerical results spread over a defined range.
what is diagnostic sensitivity? what does it indicate?
Ability to identify patients who are “true positive” for the disease - it indicates the probability that the test is positive in any patient actually affected by the disease.
what is diagnostic specificity? what does it indicate?
Ability to identify patients who are “true negative” for the disease - it indicates the probability that the test is negative in any patient not actually affected by the disease.
when is a sensitivity / specificity considered reliable?
When it is above 90%
Formula to calculate sensitivity
(true positive)/(false negative + true positive)
false negative + true positive = the total number of people affected.
formula to calculate specificity?
(true negative)/(false positive+ true negative)
false positive + true negative = the total number of people unaffected.
what are chatacteristics of the way continuous lab values are distributed?
Distribution of values is “bell-shaped”
What are the 2 main parameters considered in distribution of continuous variables?
Mean value
Standard deviation
why is it difficult to place a cut off in continuous variables?
Because there are some healthy patients that are above the cut off and some unhealthy patients below the cut-off, the distribution of values in healthy and unhealthy individuals usually intersects.
what is the reference interval?
Reference interval is the range of values that includes with good approximation, most of the unaffected population (95%)
What are the criteria to estimate reference intervals? 6
select a “normal population”
choose appropriate sample size
choose modality of blood draw and storage modality
use the same modality of measurement
use the same circulation method
evaluate results statistically
how do we choose a "normal population"?
Identify healthy subjects via a questionnaire. The selected population must be representative of the population in terms of age, gender, ethnicity etc.
Why is the sample size important?
Accuracy of estimate increases with increasing sample size, but it is not linear. More than 300 subjects, accuracy is more or less the same.
if values are "normally" distributed, which interval contains 95% of the population?
the interval [Mean±2 Standard Deviations] includes approximately 95% of the investigated individuals and represent the reference interval.
what are the values that get trimmed as "suspicious values" in a normal distribution?
you can either trim 2.5% on each sides, or 5% on one side only depending on the value. For example for liver enzymes the low data are not of pathological significance since you are interested in high levels
what is a skewed distribution?
A distribution that is not bell shaped, [Mean ±2 Standard Deviations] is not a good estimate of the reference interval.
how do we statistically evaluate based on percentiles?
the values that include 2.5-97.5 percentiles are the extreme of the reference interval
what is a possible solution when values are not normally distributed to make them normally distributed?
Transform the traditional value into logarithmic values.
what can be some special groups for reference intervals?
gender (hemoglobin, iron)
age (parameters of liver synthesis, CV parameters)
blood group (vW factor is lower in patients with blood group 0)
how can we tell if an abnormal borderline result should cause concern?
experience and common sense suggest how to act, depending on clinical probability of diagnosis
What are the 2 methods used to estimate the reference interval?
Mean ± 2 Standard Deviations
Percentile system (5% is cut off on one side, or 2.5% cut off on both)
where does venous thromboembolism (VTE) occur?
Deep veins of the legs - deep vain thrombosis
Superficial veins of the legs - superficial vein thrombosis
Cerebral veins - cerebral vein thrombosis
Splanchnic veins - splanchnic vein thrombosis
Artery occlusion of the lung - pulmonary embolism (most critical)
What is the treatment of venous thromboembolism?
anticoagulants, administered either parenteral or orally.
What may be the cause of venous thromboembolism? 6
surgery
cancer
diabetes
pregnancy
oral contraceptive
genetic factors
Venous thromboembolism in surgery
If patients who undergo surgery are not given prophylactic therapy (heparin - used to prevent blood clots in open surgery), there is a high risk of VTE turning into a pulmonary embolism. This occurs due to trauma which happens in tissues (as tissues release tissue factor - primary initiator of blood coagulator)
What is tissue factor?
Tissue factor is a pro-coagulation protein localized in the tissue. If the tissue is damaged (eg. during surgery), TF is released and can cause thrombosis.
VTE in cancer
many cancer cells are pro-coagulants and produce factors that lead to thrombosis
VTE in pregnancy
During pregnancy, pro-coagulant factors spike as a defense mechanism to blood loss that inevitably accompanies child birth.
VTE and oral contraceptives
Oral contraceptives may cause an imbalance between pro and anti-coagulants, which may be the cause of VTE risk.
genetic causes for increased VTE risk
Deficiency of anti-coagulant mechanism such as
Factor V Leiden polymorphism
deficiency of antithrombin
deficiency of protein C or S
What is factor V Leiden?
A pro-thrombotic polymorphism that is relatively frequent in the population (about 3%) and gives rise to VTE risk
what exam is needed to diagnose different types VTE?
compression ultrasonography —> very useful for the diagnosis of proximal DVT in particular
CT scans —> used for pulmonary embolism
what is a laboratory parameter important for diagnosis of VTE?
D-dimer
What is D-dimer?
D-dimer is a molecule obtained from fibrinolysis as one of the fragments.
what happens when blood cells clot in the intact vascular system?
fibrinogen is converted by coagulation into soluble fibrin. soluble fibrin is then stabilized by factor XIII to insoluble fibrin. This is the end of the coagulation cascade. Fibrinolysis of insoluble fibrin leads to production of D-dimer molecule as one of the fragments.
why can D-dimer be used as an index of probability for thrombosis?
D-dimer is characterized by a relatively short half life in the circulation before it is cleared. Its presence, therefore, is an index of fibrin deposition, or probability of thrombosis (increased fibrin —> increased coagulation —> increased thrombosis risk)
how do we take the cut-off value for D-dimer
The cut-off value for any test is determined by looking at the value in the general population. D-Dimer is NOT calculated by looking at the cut-off value, but it is viewed in context of clinical symptoms, by looking at a patient suspected of having a VTE.
what is the cut-off value of D-dimer used for? what can it not be used for?
it is used to EXCLUDE the presence of a DVT, however it cannot be used to CONFIRM a DVT, even though high values can be indicative of a DVT.
why can we exclude VTE with D-dimer?
Because D-dimer is sensitive, but not specific for VTE. D-dimer levels increase due to many non-thrombotic conditions.
what do we use to help diagnose VTE with D-dimer?
we use the Wells-Score system which integrates clinical factors to make the diagnosis
How does the well-score system work?
Patients are examined clinically for signs and risk factors which are all attributed a score of 1 if positive. We then subtract 2 from the total value if an alternative diagnosis is possible. The higher the number, the higher the probability of VTE.
What is the algorithm to EXCLUTE VTE
Measure D-dimer and perform the Wells Score test
If D-dimer is negative (below cut-off) and Wells Score is low, VTE is excluded
If D-dimer is negative, but there is a high clinical probability or D-dimer is positive, we perform instrumental testing (CUS, CT scan)
What is the odds ratio?
The odds ratio (OR) is a measure of the association between 2 variables (eg. presence of polymorphism and presence of VTE)
What is the odds ratio used for?
Estimate whether a particular exposition is a risk factor for a particular disease.
What does it mean if the Odds Ratio is greater than 1?
This means that there is a statistical association that is significant between the occurrence of that parameter and the occurrence of the disease.
What is an odds ratio of 1
1 = standard risk
How is the odds ratio expressed?
By a number and a confidence interval.
what is a confidence interval?
range in which the actual parameter is likely to be found with a high probability
what does it mean if the confidence interval is high?
The value probably hasn’t been calculated correctly.
design of study to calculate the Odds ratio
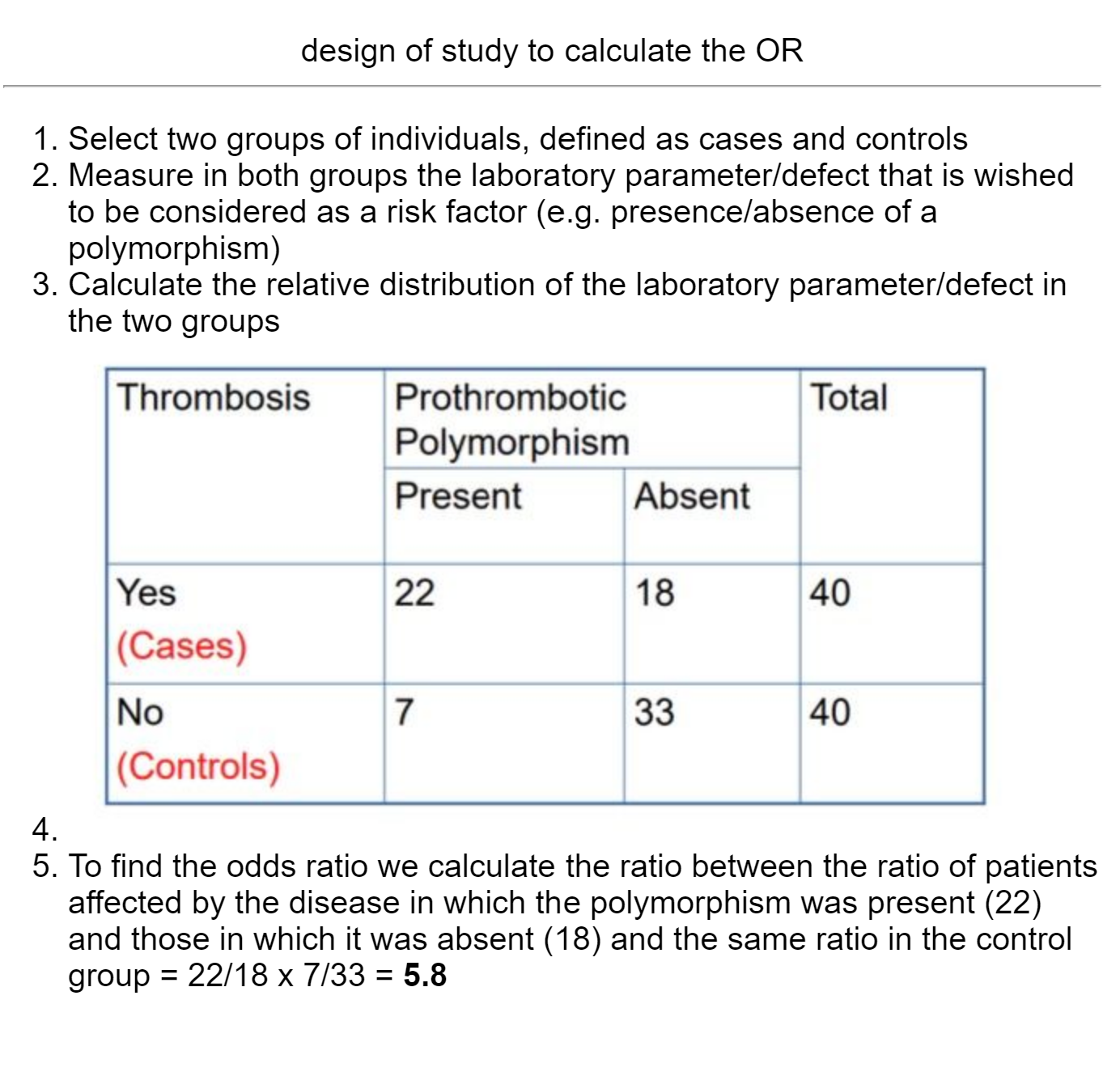
How to we calculate the absolute risk from the odds ratio?
The absolute risk can be calculated by multiplying the relative risk (OR) by the absolute risk of having a disease in the general population.