(17.5.6) Platelets & Hemostasis
1/32
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
33 Terms
Describe the structure and function of Platelets
STRUCTURE
Cytoplasmic fragments of megakaryocytes
Blue-staining outer region; purple granules
Normal 150,000-400,000 platelets/ml of blood
FUNCTION
Granules contain serotonin and ADP
Form temporary platelet plug that helps seal break in blood vessels
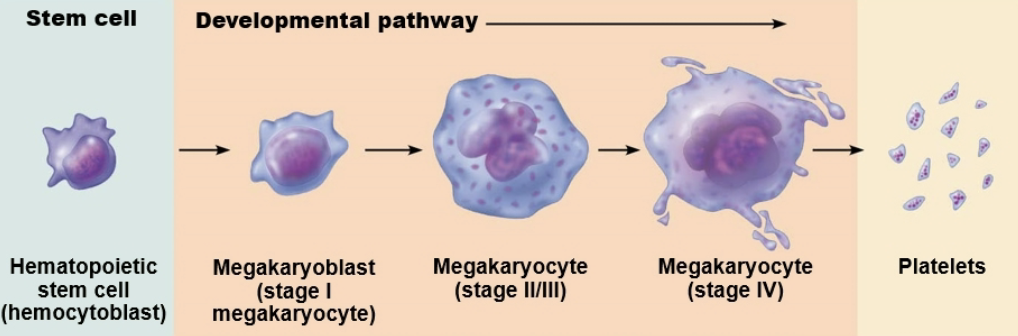
Role of Megakaryocyte
A gigantic cell in the bone marrow that is responsible for forming platelets
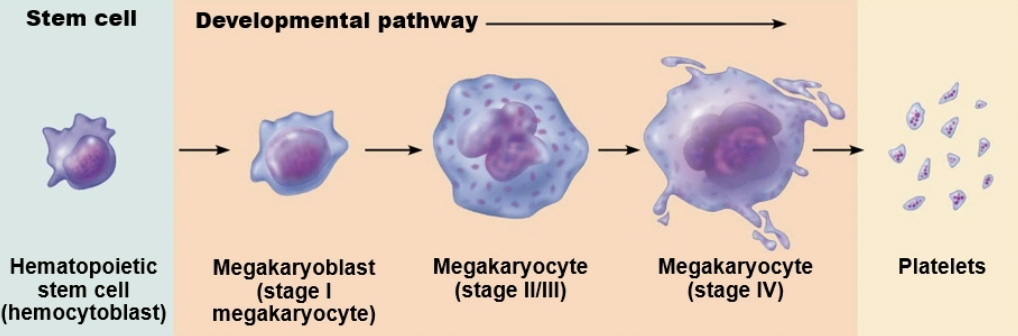
How do platelets enter the blood?
Megakaryocytes place platelets in the blood by passing them through the wall of sinusoidal capillaries (with large openings in their walls) in the bone marrow
What chemicals are involved in clotting process?
Serotonin
Calcium
Enzymes
ADP
Platelet-derived growth factor
T/F: Circulating platelets are kept active
→ False
Circulating platelets are kept inactive and mobile by nitric oxide (NO) and prostacyclin from endothelial cells lining blood vessels
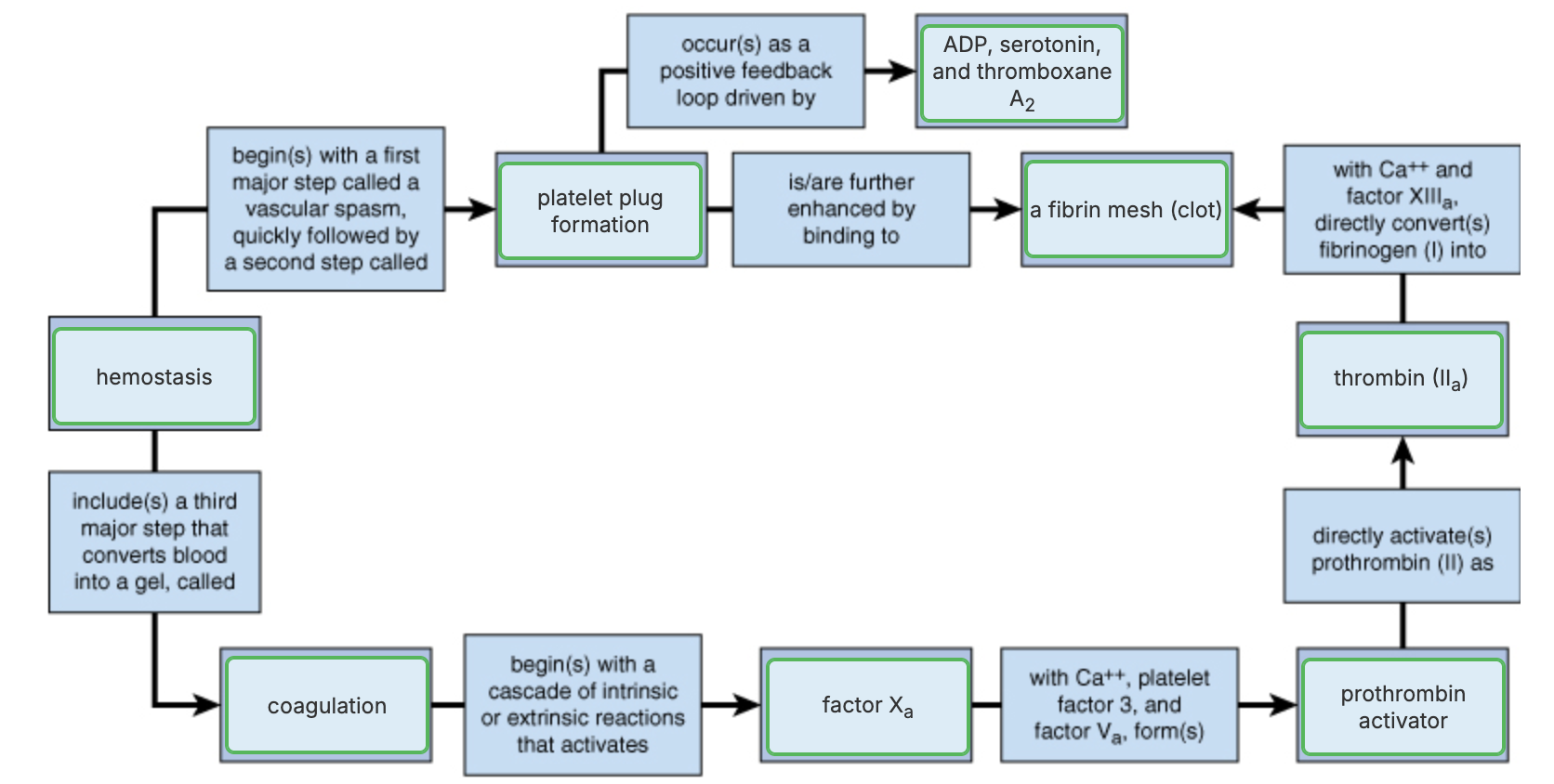
Role of Hemostasis
Fast series of reactions for stoppage of bleeding
Prevention of blood loss
List the major steps of Hemostasis
Requires clotting factors and substances released by platelets and injured tissues
Vascular spasm
Platelet plug formation
Coagulation (blood clotting)
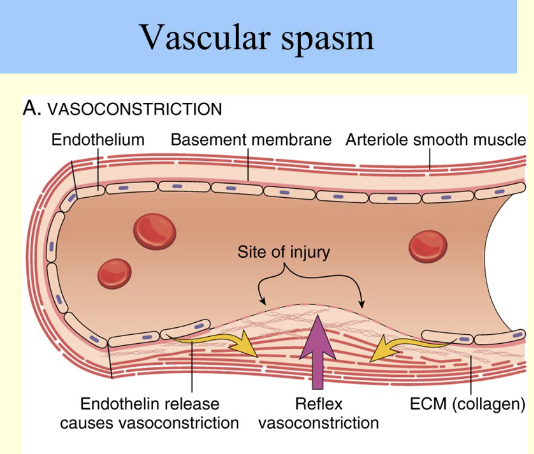
Explain Step 1 - Vascular spasm
Vessel responds to injury with vasoconstriction
Vascular spams are triggered by:
Direct injury to vascular smooth muscle
Chemicals released by endothelial cells and platelets
Pain reflexes
Strongly constricted artery can significantly reduce blood flow until other mechanisms can kick in
Most effective in smaller blood vessels
Explain Step 2 - Platelet Plug Formation
POSITIVE FEEDBACK CYCLE → as more platelets stick they release more chemicals → which cause more platelets to stick and release more chemicals
Aggregating (sticking together), forming a plug that temporarily seals the break in the vessel wall
Platelet plugs are fine for small vessels tears, but larger breaks in vessel need additional step
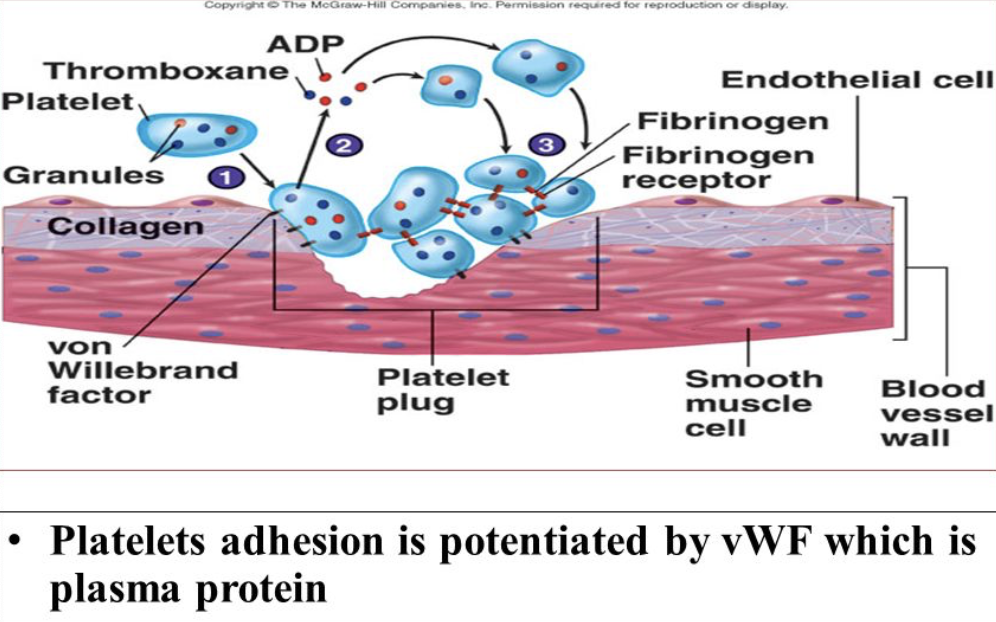
What chemicals are released by Platelets when become activated?
Adenosine diphosphate (ADP)
Potent aggregating agent that causes more platelets to stick to the area and release their contents
Serotonin and Thromboxane
Messengers that enhance vascular spasm and platelet aggregation
Explain Step 3 - Coagulation
Hemostasis → fast series of reactions for stoppage of bleeding
Reinforces platelet plug with fibrin threads
Blood is transformed from lipid to a gel when dissolved blood proteins assemble into fibrin threads
Blood clots are effect in sealing larger vessel breaks
Function of Clotting Factors
FUNCTION → A group of substances, mostly plasma proteins synthesized by the liver, that circulate in blood in an inactive form and work together in series to facilitate the multistep process of blood clotting
Procoagulants
Numbered I to XII in order of discovery
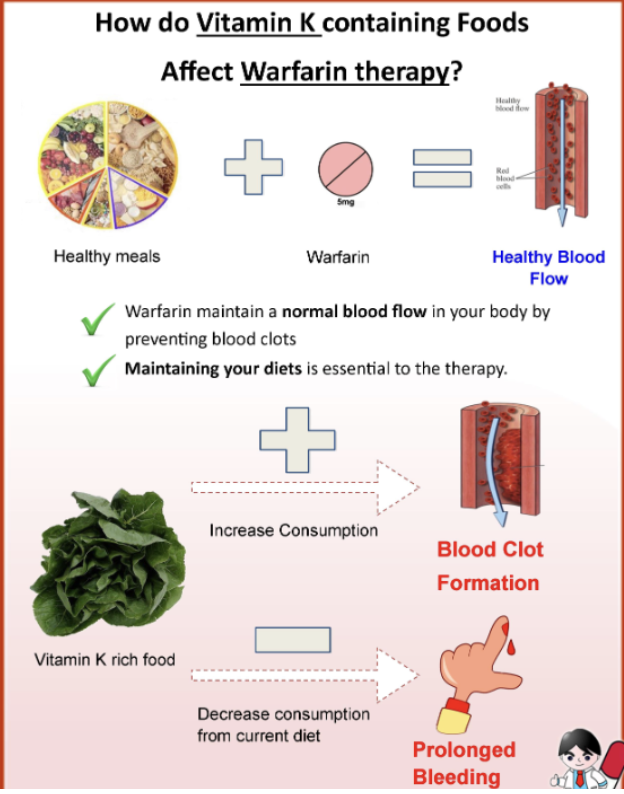
Vitamin K needed to synthesize four factors
Which Coagulation Factors require Vitamin K?
Factor II → Prothrombin
Factor VII
Factor IX
Factor X
How is Coagulation of blood initiated?
COAGULATION → Pathways to Prothrombin Activator
Intrinsic pathway
Extrinsic pathway
Explain Phase I of Coagulation
→ Pathway to Prothrombin Activator
Intrinsic pathway
Intrinsic because the factors needed for clotting are present within (intrinsic to) the blood
Vessel endothelium ruptures, exposing underlying tissue
Platelet cling and their surfaces provide sites for mobilization of factors
Phospholipid surfaces of aggregated platelets
Extrinsic pathway
Extrinsic because the tissue factor it requires is outside of blood
Tissue cell trauma expose blood to → Tissue factor TF
BOTH
Platelet phospholipid membranes
Pathways converge as prothrombin is converted to thrombin
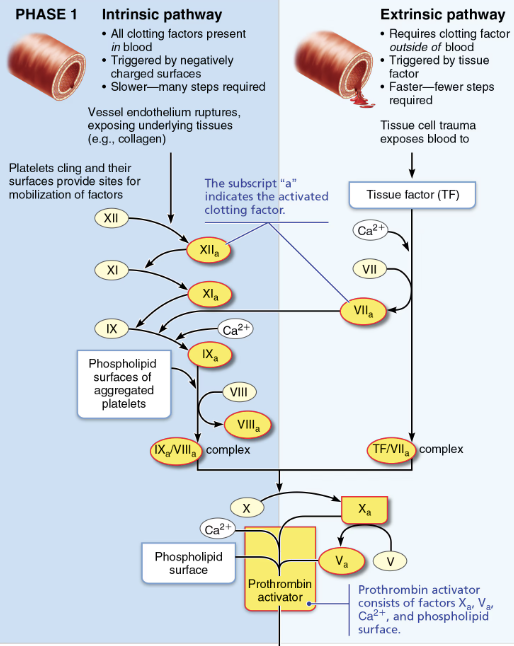
Explain Phase II of Coagulation
→ Pathway to thrombin
Prothrombin activator catalyzes transformation of prothrombin to active enzyme thrombin
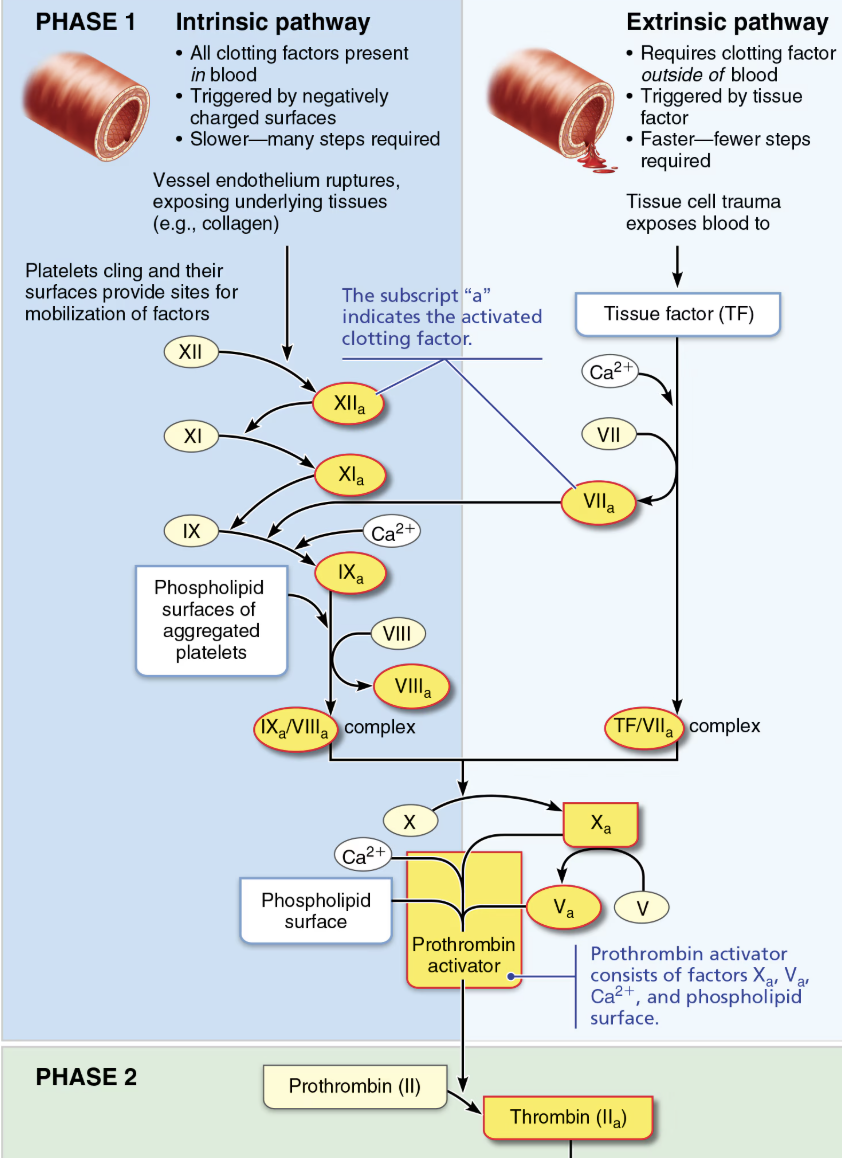
Explain Phase III of Coagulation
→ Pathway to Fibrin Mesh
Thrombin catalyzes the transformation of the soluble clotting factor fibrinogen into fibrin
Fibrin molecules polymerize (join together) to form long, hairlike, insoluble fibrin strands
Fibrin mesh that traps blood cells (platetes) and effectively seals the hole until the blood vessel can be permanently repaired
What prevents fibrin from forming a mesh in a healthy, unbroken blood vessel?
When thrombin is not bound to fibrin, it is inactivated by antithrombin.
Summarize Blood Clotting Process
Vascular Spasm
The injured blood vessel constricts to reduce blood flow to the site of the injury.
Platelet Plug Formation
Platelets are attracted to the injury, where they stick together and form a temporary plug, with the help of von Willebrand factor
Coagulation Cascade Activation
This is a series of reactions involving clotting factors, which are proteins that circulate in the blood in an inactive form
Phase I Extrinsic or intrinsic pathway → both of which converge into a common pathway of Formation of Prothrombin activator
Phase II → Prothrombin activator catalyzes the conversion of a plasma protein called prothrombin into the active enzyme thrombin
Phase III → Thrombin catalyzes the transformation of the soluble clotting factor fibrinogen into fibrin
Fibrin molecules polymerize (join together) to form long, hairlike, insoluble fibrin strands
Fibrin mesh that traps blood cells and effectively seals the hole until the blood vessel can be permanently repaired
Role of Anticoagulants
Factors that normally dominate in blood to INHBIT coagulation
Endothelial cells secrete antithrombin substances such as nitric oxide and prostacyclin
Vitamin E quinone, formed when vitamin E reacts with O2, it a potent anticoagulant
Explain Regulation of Coagulation
Limited amount of thrombin is restricted to clot by fibrin threads → preventing clot from getting too big or escaping into blood stream
Antithrombin III → inactivates any inbound thrombin that escapes into bloodstream
Heparin → in basophil and mast cells inhibits thrombin by enhancing Antithrombin III
What enzyme removes unneeded clots after healing has occurred?
→ Plasmin
Explain what happens to Clots after Hemostasis?
Fibrinolysis → Process whereby clots are removed after repair is completed
Begins within 2 days and continues for several days until clot is dissolved
Plasminogen → plasma protein that is trapped in clot, is converted to plasmin, a fibrin-digesting enzyme
List two major types of Hemostasis Disorders
Thromboembolic disorder
Result in undesirable clot formation
Bleeding disorders
Abnormalities that prevents normal clot formation
List Thrombembolic Disorders
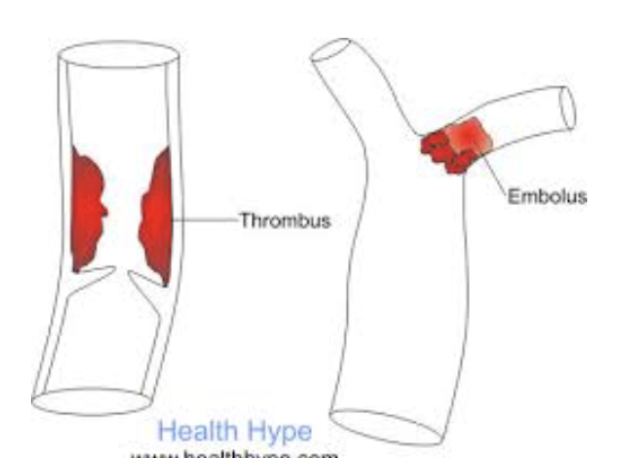
Thrombus
Embolus
Embolism
Compare and Constrast Thromboembolic Disorders
Thrombus
Clot that develops and persists in unbroken blood vessel
Risk factors → May block circulation, leading to tissue death
Embolus
Thrombus freely floating in bloodstream
Embolism
Embolus obstructing a vessel (pulmonary or cerebral emboli)
Risk factors → atherosclerosis, inflammation, slowly flowing blood or blood stasis for immobility
Role of Anticoagulant Drugs and Examples
Used to prevent undesirable clotting
Aspirin
Heparin
Warfarin (Coumadin)
Describe how Heparin works
Anticoagulant used clinically for pre- and post-operative cardiac care
Describe how Watfarin works
Used for people prone to atrial fibrillation
Interferes with actions of vitamin K
List Bleeding Disorders
Thrombocytopenia
Impaired liver function
Hemophilia
Describe Causes and Treatment of Thrombocytopenia
Bleeding Disorder
Deficient number of circulating platelets
Petechiae appear as a result of spontaneous, widespread hemorrhage
Platelet count <50,000/uL is dx
TREAMTNET
Transfusion of concentrated platelets
Describe Causes of Impaired Liver Function
Bleeding Disorder
Inability to synthesize procoagulants (clotting factors)
CAUSES
Vitamin K deficiency
Hepatitis
Cirrhosis
Liver disease - prevent liver from producing bile, which is needed to absorb fat and vitamin L
Describe Causes of Hemophilia
Bleeding Disorder
Includes several similar hereditary bleeding disorders
Hemophilia A → most common type (77% of all cases) due to factor VIII deficiency
SYMPTOMS:
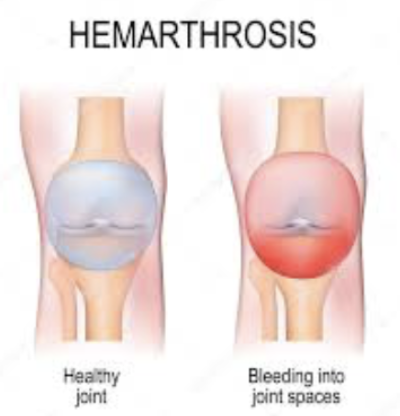
Prolonged bleeding, especially into joint cavities