PATHOLOGY OF THE UTERUS
1/73
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
74 Terms
These are the most common cystic lesions of the vagina and usually are found incidentally
during sonographic examination
Gartner Duct Cyst
Most common congenital abnormality of female genital tract is____________resulting in obstruction.
imperforate hymen
Obstruction of the uterus and/or vagina may result in the accumulation of fluid, blood, or pus. What are the MEDICAL TERMINOLOGY for fluid, blood, and pus?
Hydrometra, Hemantometra and Pyometra
________________is seen in hysterectomy patients after surgery.
• The upper size limit of a normal vaginal cuff is 2.1 cm.
• If the cuff is larger than this or contains a well-defined mass or
areas of high echogenicity, it should be regarded with suspicion
for malignancy, especially in the patient who has a previous
history of cancer.
• Nodular areas in the vaginal cuff may be due to post-irradiation
fibrosis.
The Vaginal Cuff
The ____________(posterior cul-de-sac) is the most posterior
and inferior reflection of the peritoneal cavity.
• Because of its location, it is frequently the site of intraperitoneal fluid
collections. As little as 5 mL of fluid has been detected by
transvaginal sonography.
• Fluid in the cul-de-sac is a normal finding in asymptomatic women
and can be seen during all phases of the menstrual cycle.
• Pathologic fluid collections may be associated with ascites, blood
resulting from a ruptured ectopic pregnancy, hemorrhagic cyst, or pus
resulting from an infection. Pelvic abscesses and hematomas can also
occur in the cul-de-sac.
• Sonographic characteristics help to differentiate these findings.
Rectouterine Recess

It is located between the rectum and uterus and is also called the____________?
Pouch of Douglas
• Lies posterior to bladder between lower uterine segment and vaginal canal
• The cervical canal extends from the internal os where it joins the uterine cavity, to
the external os, which projects into the vaginal vault.
• Cylindrical portion of uterus that enters vagina and measures 2 to 4 cm in length
Cervix
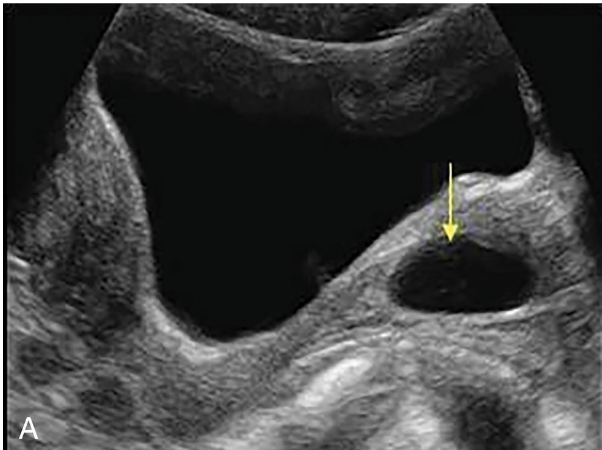
• Benign cysts in the cervix which result from chronic cervicitis and are seen frequently in middle-aged women. This cyst results from an obstructed dilated transcervical gland and is also called an epithelial inclusion cyst.
• Chronic inflammatory retention cysts
• Asymptomatic although may cause pain/bleeding with coitus
• On sonographic evaluation include:
• discrete
• round
• fluid-filled
• anechoic
• usually measuring less than 2 cm;
• they may be multiple.
• Occasionally, nabothian cysts may have internal echoes that may be caused by hemorrhage or infection.
Nabothian Cyst
• Present clinically with irregular bleeding.
• Benign condition arises from the hyperplastic protrusion of epithelium of
endocervix or ectocervix.
• Chronic inflammation most likely factor
• Polyps may be pedunculated, projecting out of cervix, or broad-based.
• Ultrasound may or may not see cervical polyps, depending on location.
Cervix Polyps
• Small percentage of leiomyoma (myoma tumors, fibroid
tumors) occur in cervix.
• When myoma is small, patient asymptomatic; as mass enlarges,
bladder or bowel obstruction may result
• Myoma may be pedunculated and prolapse into vaginal canal.
• Sonography may assist in determining the location and
thickness of the stalk.
• Fluid infusion with sonohysterography enhances visualization.
Cervical Leiomyoma
• Cervical stenosis is acquired condition.
• Obstruction of cervical canal at internal or external os resulting
from
• Radiation therapy
• Previous cone biopsy
• Postmenopausal cervical atrophy
• Chronic infection
• Laser or cryosurgery
• Cervical carcinoma
• Menopausal patient may be asymptomatic even though stenosis
can produce a distended, fluid-filled uterus (the result of an
accumulation of uterine secretions, fluid hydrometra, pyometra,
or hematometra).
• Intracavitary fluid collections can be readily seen on ultrasound
and may be indirect indicator of cervical stenosis.
• Premenopausal patients may experience abnormal bleeding,
oligomenorrhea, amenorrhea, cramping, dysmenorrhea, or
infertility.
Cervix Stenosis
• Squamous cell carcinoma is the most common type of cervical
cancer.
• Precursors are cervical dysplasias classified as mild, moderate, or
severe.
• When full thickness of epithelium composed of undifferentiated
neoplastic cells, lesion referred to as carcinoma in situ
• The detection of these abnormalities is attributed to screening with
Papanicolaou (Pap) smears because most of the early lesions are
asymptomatic.
• Advanced cervical cancer is usually evident clinically.
• Sonography may demonstrate a solid retrovesical mass, which may be
indistinguishable from a cervical myoma.
• Transvaginal and translabial ultrasound may demonstrate bladder,
ureteral, vaginal, or rectal involvement and may be used in staging
cervical cancer.
• CT and MRI are preferable because they are superior methods for
staging and evaluating lymphatic spread.
• Areas of increased echogenicity or hypoechoic areas with an irregular
outline signify changes compatible with cervical carcinoma.
• Ultrasound is also helpful in guiding biopsies of the cervix and vagina.
• Translabial or transperineal sonography may be used instead of or with
the transvaginal approach to help define the cervical area.
Cervical Carcinoma
Carcinoma in situ (in place), what stage is this?
Stage 0
Confined to the cervix, what stage is this?
Stage I
Extends beyond cx but not to pelvic wall, what stage is this?
Stage II
Extends to pelvic walls, what stage is this?
Stage III
Extends beyond the true pelvis, what stage is this?
Stage IV
What is the Differentail Consideration for the Uterus for ENLARGES UTERUS?
➢ Pregnancy
➢ Postpartum
➢ Leiomyoma
➢ Adenomyosis
➢ Bicornuate or didelphic uterus
Differential Considerations for the Uterus for UTERINE TUMOR?
➢ Leiomyoma
➢ Carcinoma
Differential Considerations for the Uterus for THICKENED ENDOMETRIUM?
➢ Early intrauterine pregnancy
➢ Endometrial hyperplasia
➢ Retained products of conception or incomplete abortion
➢ Trophoblastic disease
➢ Endometritis
➢ Adhesions
➢ Polyps
➢ Inflammatory disease
➢ Endometrial carcinoma
Differential Considerations for the Uterus for ENDOMETRIAL FLUID?
➢ Endometritis
➢ Retained products of conception
➢ Pelvic inflammatory disease
➢ Cervical obstruction
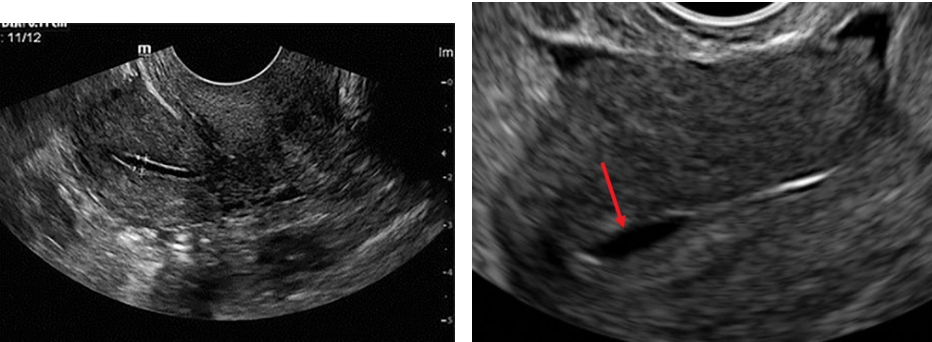
Differential Considerations for the Uterus for ENDOMETRIAL SHADOWING?
➢ Gas (abscess)
➢ Intrauterine device
➢ Calcified myomas or vessels
➢ Retained products of conception
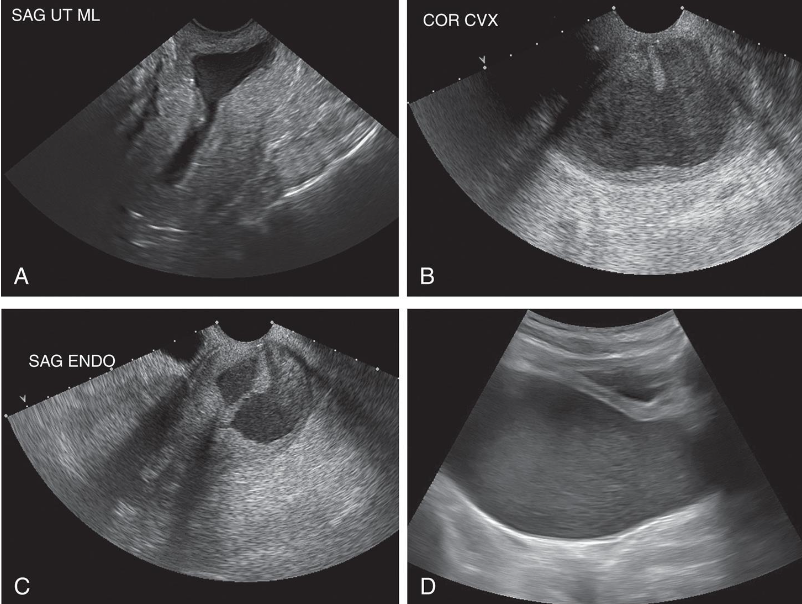
– Incomplete development of one side of the
uterus leads to a unicornuate uterus (i.e., a
uterus with one tube)
– The uterus will appear small and more
lateral in position on sonogram
– A rudimentary horn may be visible
This is?
Unicornuate Uterus
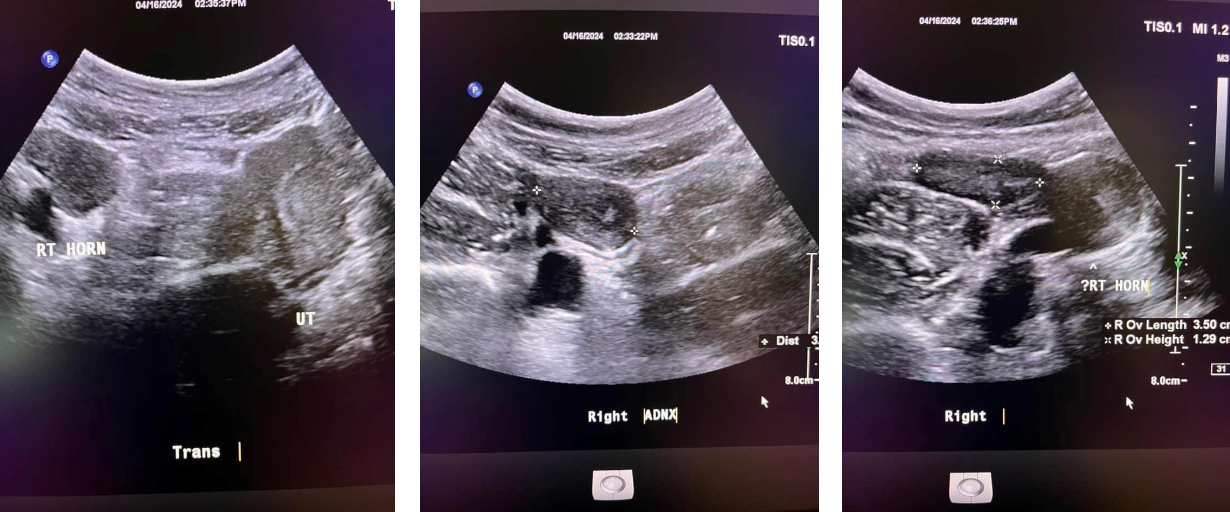
This is?
Unicornuate Uterus
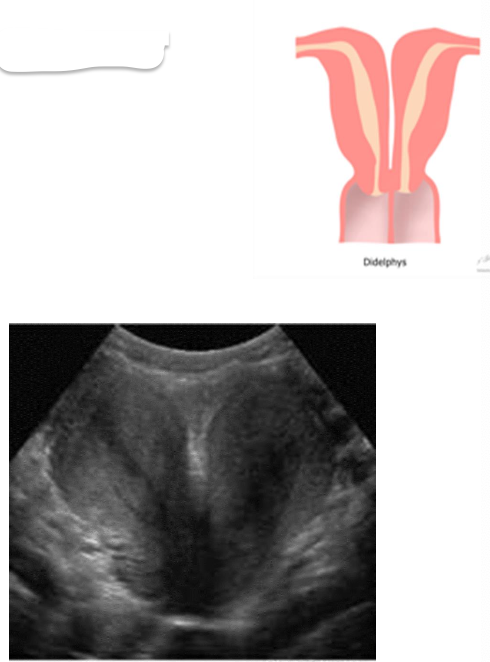
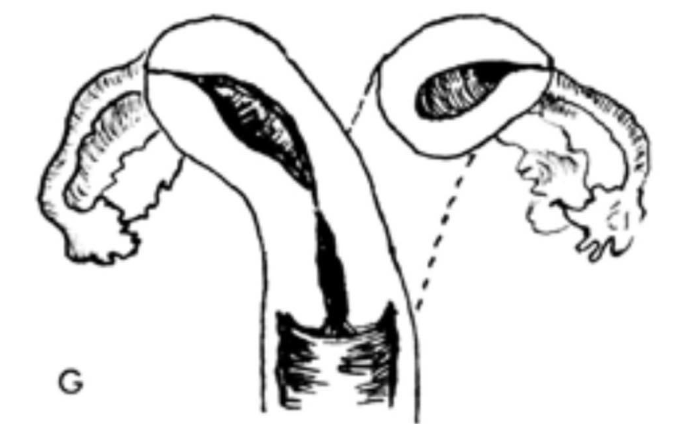
– Double vaginas, cervixes, and uteri function separately
– The two uteri are at approximately a 450 angle to one another
Uterus Didelphus
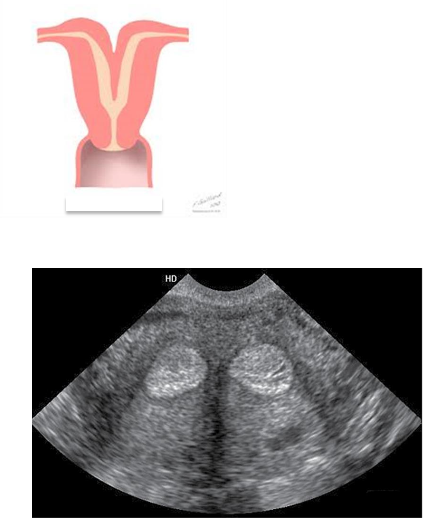
– Improper fusion leads to two partially or completely separate bicornuate uterine cavities.
– The uterus is heart-shaped
– Most common congenital uterine anomaly.
Bicornuate uterus
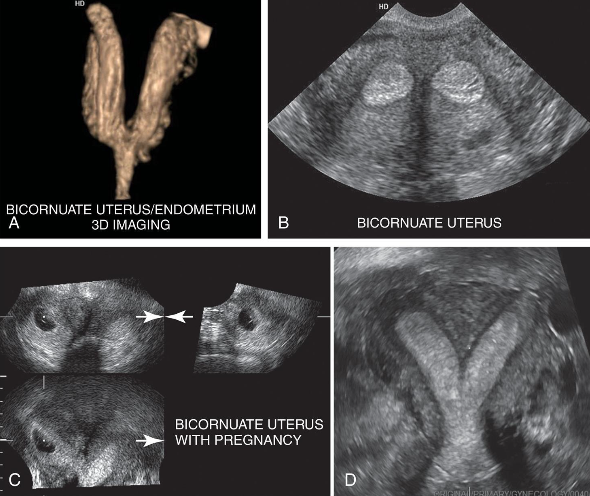
This is?
Bicornuate Uterus
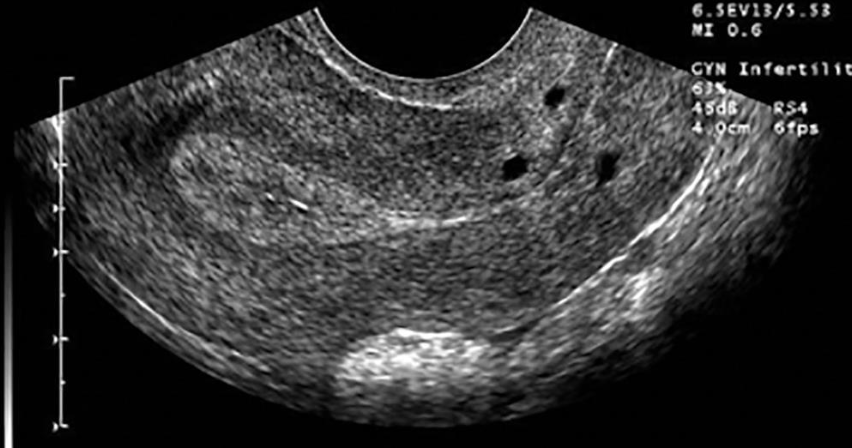
– Two partially or completely separate endometrium form.
– The uterus is normally shaped
– Most common congenital uterine anomaly causing infertility.
Septate Uterus
Also called Myomas, Fibroids, and Fibromyomas
Most common pelvic tumor
More common in African American women nulliparous (never borne offspring)
Smooth muscle cell composition
Liquefaction, necrosis, hemorrhage, and ultimate calcification may take place.
Degeneration occurs when myomas outgrow their blood supply; calcification
May be pedunculated
Clinical symptoms include
➢ enlarged uterus
➢ profuse and prolonged bleeding
➢ pain
Myomas are estrogen dependent and may increase in size during pregnancy, although about half of all
myomas show little change during pregnancy.
Myomas identified in the first trimester are associated with an elevated risk of pregnancy loss, and
this risk is higher in patients with multiple myomas.
They rarely develop in postmenopausal women, and most stabilize or decrease in size following
menopause because of a lack of estrogen stimulation.
They may increase in size in postmenopausal patients who are undergoing hormone replacement
therapy.
Tamoxifen has also been reported to cause growth in leiomyomas. A rapid increase in myoma size,
especially in a postmenopausal patient, should raise the level of concern for a neoplasm.
The signs and symptoms of leiomyomas depend on their size and location.
Submucosal myomas may erode into the endometrial cavity and cause irregular
or heavy bleeding, which may lead to anemia.
Fertility may be affected by submucosal or intramural myomas, which may
impede sperm flow, prevent adequate implantation, or cause recurrent miscarriages.
It is particularly important to diagnose submucosal leiomyomas because they are a
well-established cause of dysfunctional uterine bleeding, infertility, and
spontaneous abortion. Small submucosal leiomyomas may be removed
hysteroscopically (a fibroid removal treatment).
Uncommonly, a pedunculated subserosal lesion develops a long stalk and is
migratory; it can implant into the blood supply of the broad ligament, omentum, or
the bowel mesentery.
Transvaginal sonography is often helpful in showing the uterine origin of the
mass and identifying the stalk. Occasionally, a pedunculated myoma becomes
adherent to surrounding structures and develops an auxiliary blood supply.
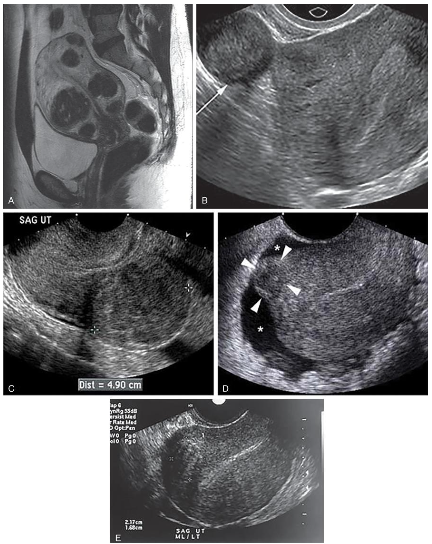
Sonographic Findings of Leiomyomas
• Uterine enlargement or irregular uterine wall contour with a heterogeneous myometrial texture pattern.
• Look for contour distortion along the interface between the uterus and bladder.
• The myomas alters the normal homogeneous myometrium
• Myomas can be associated with endometrial infection and cancer.
• Blood debris and polyps can artifactually widen the endometrium; therefore definitive diagnosis of the
cause of abnormal bleeding require an endometrial biopsy.
• Cystic degeneration can occur during pregnancy and cause pain. Doppler should be used to assess
the vascularity of myomas.
The sonographic study should include measurement of the uterus in three dimensions: (1) cervix to
fundus, (2) widest anteroposterior diameter, and (3) widest transverse diameter at fundus diameter.
The texture of the myoma (calcific, complex, or anechoic), size, and location are described.
Individual myomas are measured if they are discrete.
The shape of the endometrial complex and its thickness are also described; alterations in the
endometrial border will be evident if a myoma is present. This is especially important in women with a
history of abnormal bleeding.
Myomas can be associated with endometrial infection or cancer. Blood debris and polyps can
artifactually widen the endometrium; therefore, definitive diagnosis of the cause of abnormal bleeding
might require an endometrial biopsy or sonohysterography.
Although ultrasound is used to identify myomas in women with abnormal bleeding, uterine
enlargement, or infertility, MRI—with its tissue differentiation characteristics—can be more
sensitive for evaluating the exact location, size, and number of myomas.
Tamoxifen is a ___________drug.
Breast Cancer
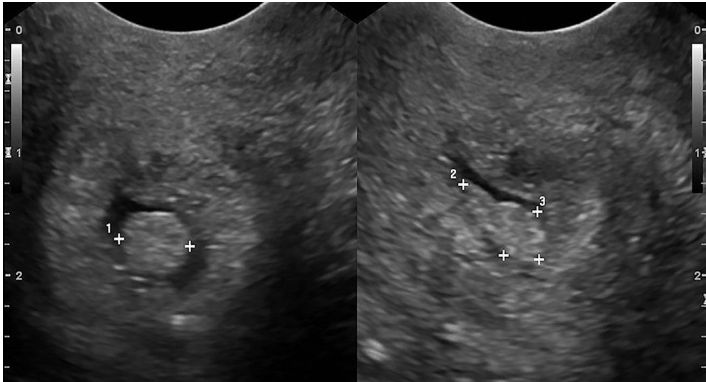
Leiomyomas can be_______________________?
Submucosal, Intramural, Subserosal
(displacing or distorting endometrial cavity with subsequent irregular or heavy menstrual bleeding, Infertility)
What kind of Leioyomas can this be?
Submocosal
(confined to myometrium; most common type): may enlarge to cause pressure on adjacent organs; Infertility or recurrent pregnancy loss.
What kind of Leioyomas can this be?
Intramural
(projecting from the peritoneal surface of uterus): Can become pedunculated and appear as extrauterine masses, may enlarge to cause pressure on adjacent organs
What kind of Leioyomas can this be?
Subserosal
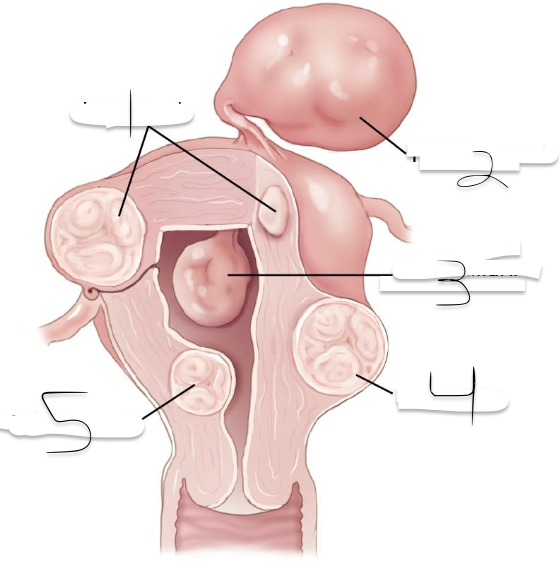
1?
Intramural
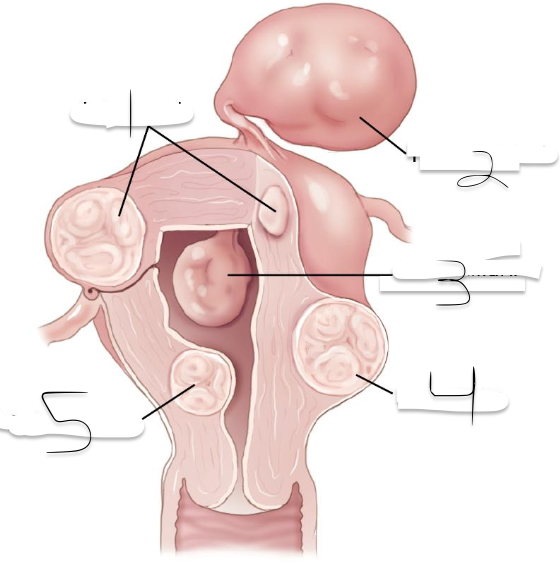
2?
Pedunculated
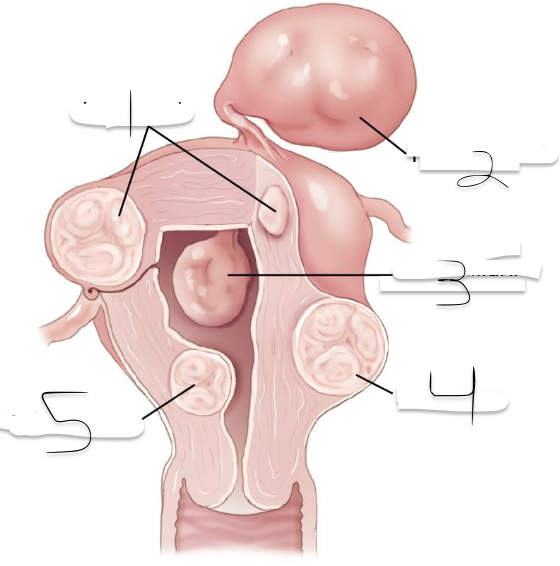
3?
Intracavitary
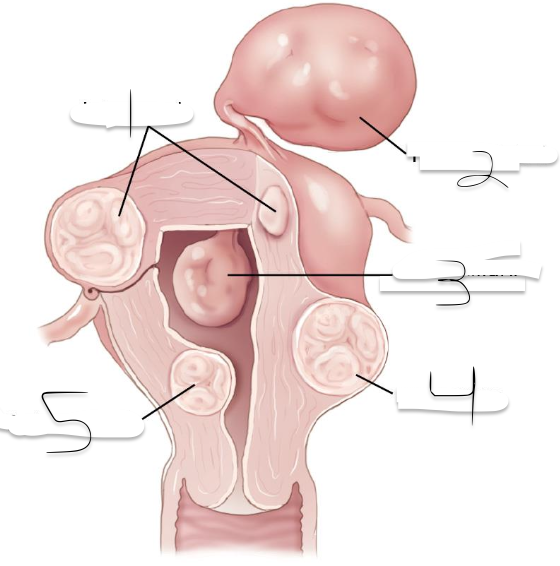
4?
Suberous
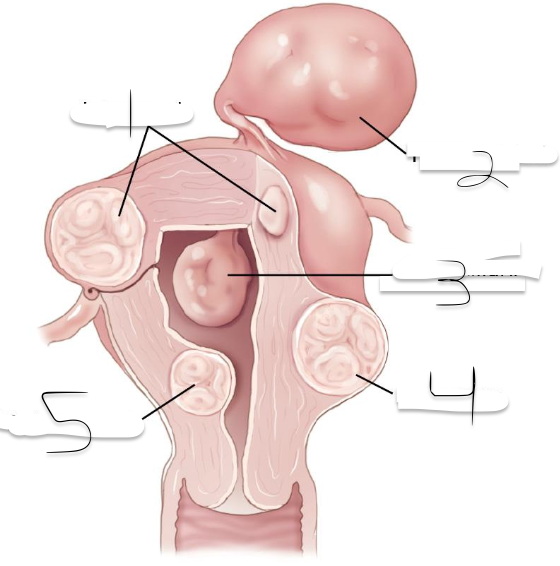
5?
Submuscosal
What is the Treatment of Myomas?
In case of infertility and submucosal myoma, surgery by myomectomy often treatment of
choice
In cases of menorrhagia, women now have several choices:
➢ Least invasive treatment is hormonal suppression to stop bleeding.
➢ Endometrial ablation uses radiofrequency, microwaves, freezing, or heating ablative technology to ablate or
remove the endometrium and any small surrounding myomas.
➢ Uterine artery embolization (UAE) Small plastic particles are injected into the blood supply to the myoma to
terminate flow.
➢ High intensity focused ultrasound (HIFU) High-intensity focused ultrasound (HIFU) involves the
application of “therapeutic” sonic waves to the uterus and myoma. The myoma is ablated by heating the
tissue and causing tissue death.
➢ Hysterectomy
Rare, solid tumor arising from myometrium or endometrium
Commonly in fundus of uterus
Most common in women 40 to 60 years of age
Rapid growth
Sarcoma botryoides: very rare condition in children characterized by
grapelike clusters of tumor mass
Sonographic findings
Leiomyosarcoma may resemble myomas or endometrial carcinoma with
features of solid or mixed-solid and cystic texture.
Clinically, rapid enlargement of solid uterine mass in perimenopausal or
postmenopausal patient raises concern about development of
malignancy.
Uterine Leiomyosarcoma
Myomas are the most common cause of uterine calcifications.
A less common cause is arcuate artery calcification in the periphery of the uterus.
These calcifications are thought to occur as a consequence of calcific sclerosis within these vessels
and can indicate underlying diseases, such as diabetes mellitus, hypertension, and chronic renal
failure. Such calcifications have been termed Monckeberg arteriosclerosis and appear in arteries
throughout the body.
Sonographic Findings:
➢ Focal areas of increased echogenicity
➢ Shadowing
➢ Peripheral echogenic rim.
Uterine Calcifications
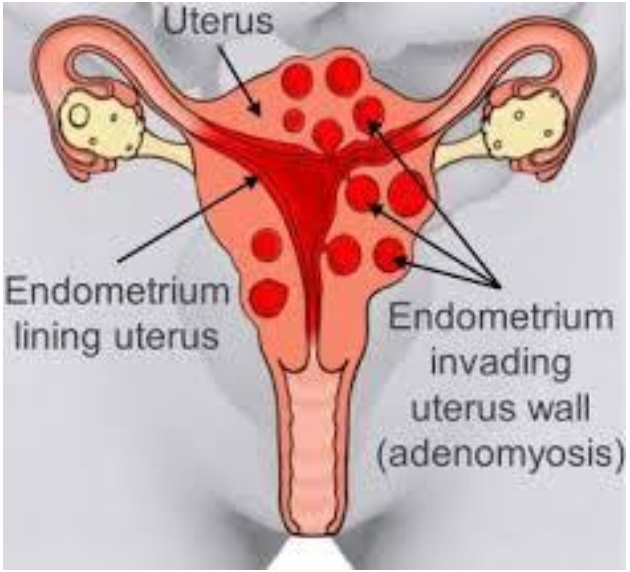
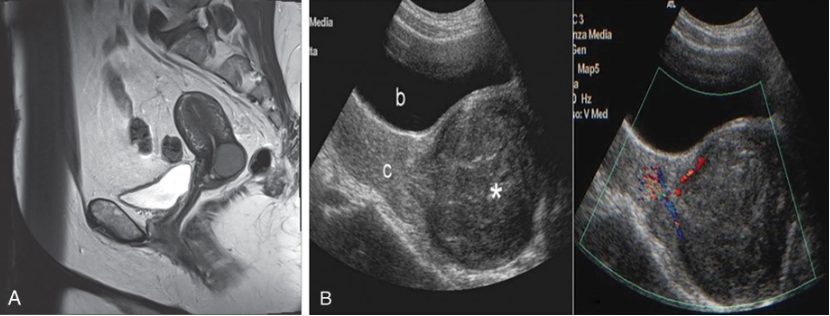
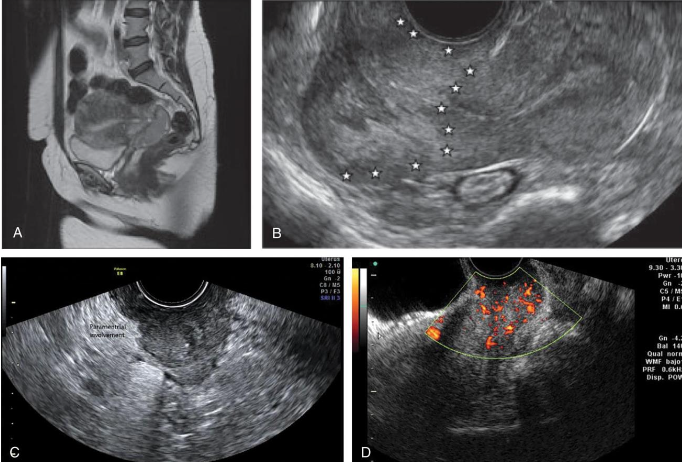
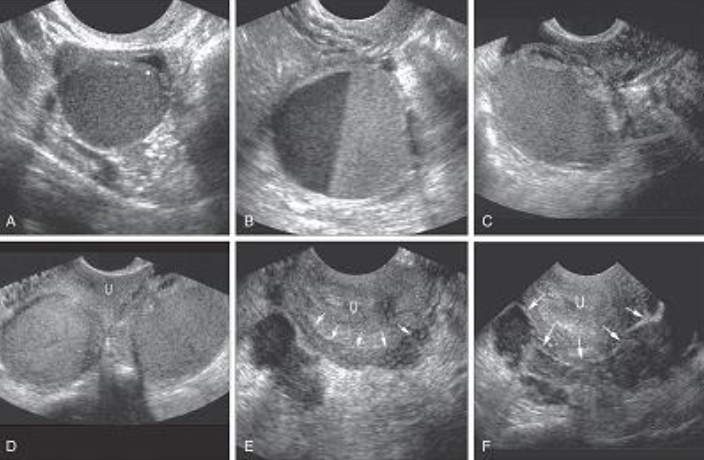
Benign disease
Diffuse or focal
Global infiltration of endometrium
Sonographically presents as bulky enlarged uterus without focal mass
Adenomyosis is ectopic occurrence of endometrial tissue within myometrium; more common in
posterior aspect
The tissue penetration usually reaches a depth of at least 2.5 mm from the basal layer of the
endometrium.
Adenomyosis may arise from multiple pregnancies and deliveries with subsequent uterine shrinking.
Elevated estrogen levels may also promote the growth of myometrial islands of endometrial tissue.
Adenomyosis is often classified into diffuse and focal forms. The more common form is diffuse
adenomyosis.
It represents a reactive hypertrophy of the myometrial muscle, which produces uterine enlargement
but usually not to the extent seen with leiomyomas.
Focal adenomyosis is sometimes called adenomyoma, referring to isolated implants that typically
cause reactive hypertrophy of the surrounding myometrium and produce diffuse uterine enlargement.
Less common than the diffuse form, focal adenomyosis (adenomyoma) lacks a hypoechoic border that
is seen with fibroids, not endometriosis. Adenomyosis can be appropriately managed with hormone
therapy.
Patients with adenomyosis are often multiparous and older than patients with endometriosis.
The patient presents with heavy, painful abnormal menses, and on physical examination, the uterus is
found to range from normal to three times normal size and is globular in contour, boggy, and
somewhat tender.
Hypermenorrhea
➢ Abnormal uterine bleeding
Menorrhagia
➢ Prolonged/profuse uterine bleeding
Metrorrhea
➢ Irregular, acyclic bleeding
Dysmenorrhea
➢ Pelvic pain during menstruation
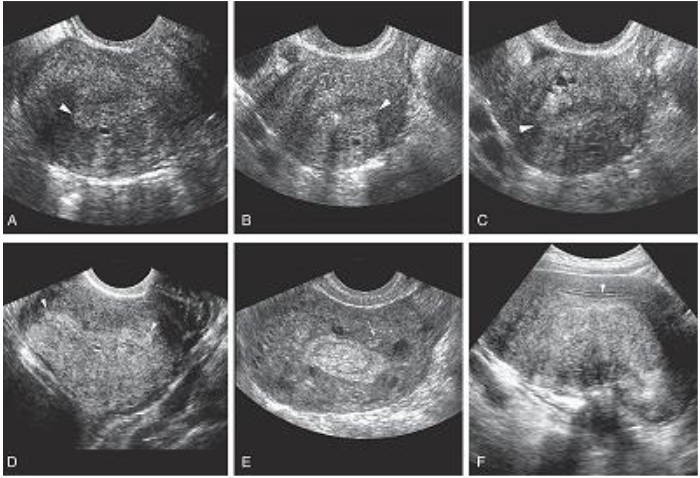
Sonographically, diagnosis may be difficult.
Most common presentation of extensive adenomyosis is:
➢ Diffuse uterine enlargement
➢ Thickening of posterior myometrium
➢ Indistinct border between endometrium and myometrium (involved area being slightly more
anechoic than normal myometrium)
Has been described as Swiss cheese or honeycomb pattern
Calcifications resulting from prior instrumentation are seen along inner myometrium and cervix.
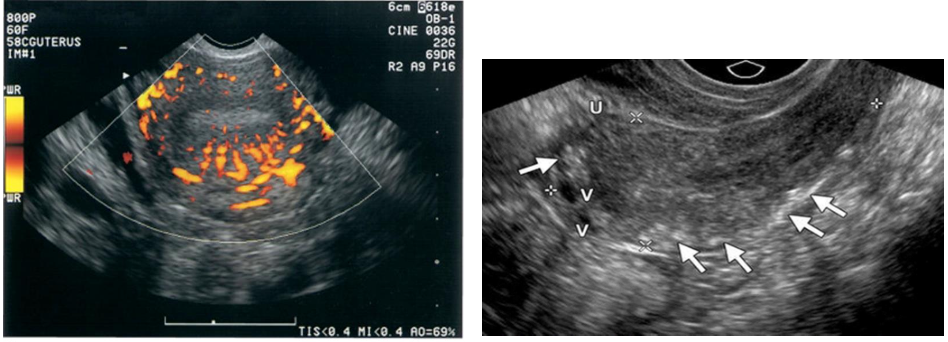
Doppler studies have also proven helpful in differentiating uterine pathology, as color flow studies of
uterine masses show that myomas and sarcomas typically demonstrate a feeding artery, but
adenomyosis rarely demonstrates feeding arteries.
Adenomyosis is not always reliably diagnosed by ultrasonography, and
caution is advised because these findings are similar in appearance to
uterine myomas, muscular hypertrophy, myometrial contractions,
endometritis, endometrial carcinoma, and the presence of increased
endometrial secretions.
The presence of myomas has been shown to limit the ability to diagnose
the severity of adenomyosis.
Although not reliably diagnosed by ultrasonography, adenomyosis is well
characterized by MRI, which currently is thought by many to be the
best technique for the presurgical diagnosis of adenomyosis.
Adenomyosis
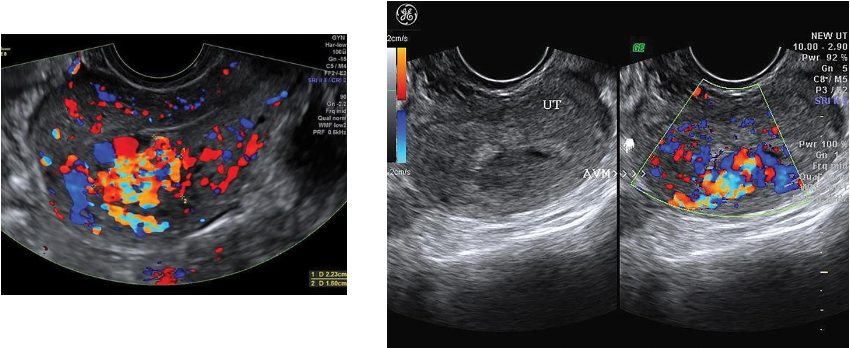
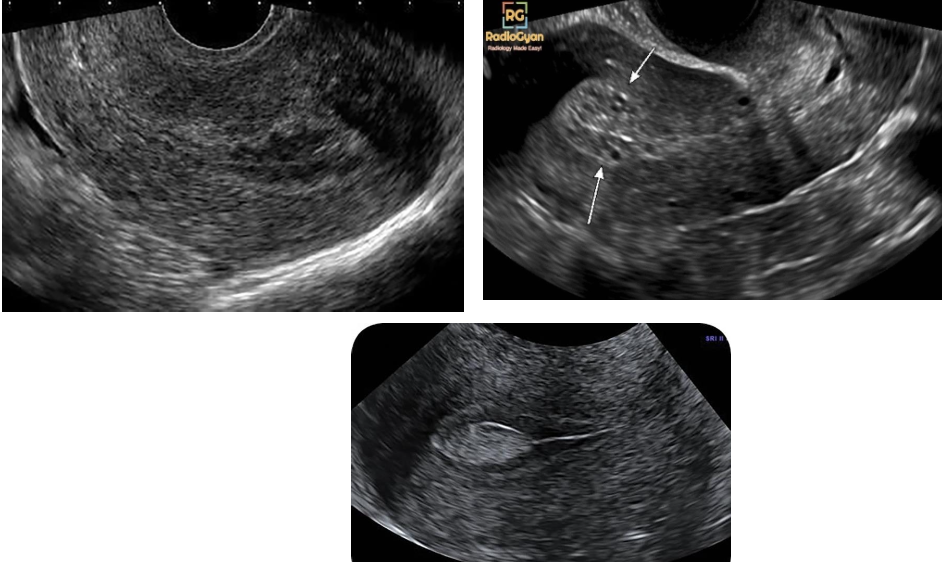
-consist of vascular plexus of arteries and veins
without intervening capillary network.
Rare; usually involving myometrium and rarely endometrium
Congenital or teratogenic (acquired) due to pelvic trauma, surgery, or gestational
trophoblastic neoplasia
Clinically, women of childbearing years have metrorrhagia with blood loss and anemia.
Diagnosis critical because dilation and curettage may lead to catastrophic hemorrhaging
Sonographic findings
Sonographically, serpiginous, anechoic structures seen within the pelvis
Uterine AVMs may appear as subtle myometrial inhomogeneity, tubular spaces within myometrium,
intramural uterine mass, endometrial or cervical mass
Color Doppler diagnostic to show blood flow within anechoic structures
May be florid-colored mosaic pattern with apparent flow reversals and
areas of color aliasing
Spectral Doppler shows high-velocity, low-resistance arterial flow
coupled with high-velocity venous flow with arterial component.
Arteriovenous Malformations
What is the landmark for identification of long axis of uterus?
Endometrial canal
Echogenicity of endometrial tissue is?
compared with homogeneous, medium-level echogenicity of middle
layer of myometrium.
The endometrium should be measured?
perpendicular to the long axis of the uterus.
What is the measurement of the endometrium?
The calipers should be placed at the maximum anterior to posterior diameter of the outer borders, from echogenic border to echogenic border.
The hypoechoic halo surrounding the endometrium should not be included in the measurement because this represents the inner compact layer of myometrium.
Fluid, if present, should not be included in endometrial measurements.
What is the Endometrial thickness (mm) for MENSTRUAL CYCLE?
2-3
What is the Endometrial thickness (mm) for EARLY PROLIFERATIVE PHASE?
4-6
What is the Endometrial thickness (mm) for PERIOVULATORY PHASE?
6-8
What is the Endometrial thickness (mm) for SECRETORY PHASE
8-15
Abnormally thick endometrium results from variety of condition: ?
➢ Early intrauterine pregnancy
➢ Gestational trophoblastic disease
➢ Endometrial hyperplasia
➢ Secretory endometrium
➢ Estrogen replacement therapy
➢ Polyps
➢ Endometrial carcinoma
Many endometrial pathologies, such as hyperplasia, polyps and carcinoma, can cause abnormal leeding, especially in postmenopausal patient.
___________is a common condition in which functioning endometrial tissue is present outside the
uterus.
The ectopic tissue can be found almost anywhere in the pelvis, including the ovary, fallopian tube,
broad ligament, the external surface of the uterus, and scattered over the peritoneum, cul-de-sac, and
even the bladder.
The endometrial tissue cyclically bleeds and proliferates.
In the diffuse form, this leads to disorganization of the pelvic anatomy with an appearance similar to
PID or chronic ectopic pregnancy.
Two forms of endometriosis have been described: diffuse and localized (endometrioma).
The diffuse form is more common, consists of endometrial plantings within the peritoneum, and is
rarely diagnosed by sonography.
The localized form consists of a discrete mass called an endometrioma, or chocolate cyst, and can
frequently be found in multiple sites. The patient with an endometrioma is usually asymptomatic.
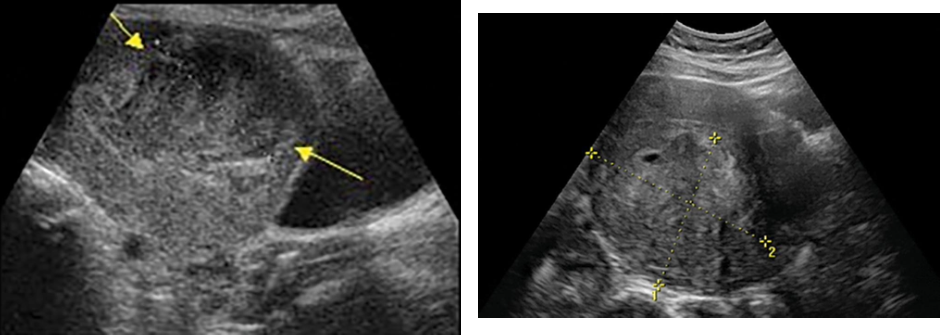
Sonographic Findings
Endometriosis may appear as bilateral or unilateral ovarian cysts with patterns
ranging from anechoic to solid, depending on the amount of blood and its
organization (Fig. 44.19).
The ovaries are typically adherent to the posterior surface of the uterus or stuck in the
cul-de-sac and may be intimately associated with the rectosigmoid colon and difficult
to define.
Obscured organ borders and multiple irregular cystic masses also suggest either
disseminating cancer or pelvic infection, and the clinical picture and serial
sonographic studies determine when and if exploratory surgery is indicated.
Clinical findings include severe dysmenorrhea, chronic pelvic pain from peritoneal
adhesions and bleeding, or dyspareunia
Endometrioma
Sonographic Appearance
➢ Well-defined unilocular or multilocular
➢ Predominantly cystic mass containing
➢ Diffuse homogeneous, low-level internal echoes (Fig. 44.20).
➢ Occasionally a fluid-fluid level can be seen.
➢ Small linear hyperechoic foci may be present in the wall and are thought to be
cholesterol deposits accumulating in the cyst wall.
Clinical symptoms help to differentiate endometriosis from a
hemorrhagic ovarian cyst, ovarian neoplasm, or tubo-ovarian abscess.
Endometriosis
Disorders of endometrium may also occur in menopausal patients with breast cancer
receiving tamoxifen therapy.
Tamoxifen is a partial estrogen receptor antagonist used in postmenopausal women
with estrogen receptor positive breast cancer.
The effects on the uterus include epithelial metaplasia, hyperplasia, and even
carcinoma. In these patients, transvaginal scanning may show thickened, irregular
cystic endometrium. These patients frequently have biannual serial ultrasound
examinations of their uterus and endometrium. A biopsy is performed in suspicious
cases.
This is the ___________
PATHOLOGY OF THE ENDOMETRIUM
Two possible explanations for the cause of endometriosis are presented.
The first is that the chronic retrograde flow of menstrual fluid through the tubes and into
the pelvis may produce implantation and proliferation of endometrial cells with cyclic
bleeding. This is the “transtubal migration” theory.
The second theory involves the evaluation of endometrial activity in susceptible cells that
retain the embryonic capacity to differentiate in response to hormonal stimulation. The
resulting tissue bleeds and proliferates with the resultant production of pain, scarring, and
endometrium-lined collections of blood known as endometriomas.
Endometriosis may occur in any menstruating female.
Clinical symptoms include painful periods (dysmenorrhea) or painful intercourse
(dyspareunia); lower abdominal, pelvic, and back pain; irregular bleeding; and infertility
secondary to adhesions and fibrosis.
Endometriosis & Endometrioma
This is ?
Endometriosis
This is?
is the most common cause of abnormal uterine bleeding in
both premenopausal and postmenopausal women. Hyperplasia develops from
unopposed estrogen stimulation.
It appears as a thickening of the endometrium.
In premenopausal women, if the endometrium measures more than 14 mm (double
thickness), hyperplasia is suggested.
The optimal time period for this assessment in a woman still having menses is day 6
through day 10, after bleeding and before the endometrium is again stimulated.
In asymptomatic postmenopausal women, 8 mm (double thickness) is the upper limit of
normal. However, women on sequential estrogen and progesterone replacement
regimens may have endometrial thickness up to 15 mm during the estrogen phase; the
thickness decreases after progesterone is added.
Ideally a woman using sequential hormones should be studied at the beginning or
end of her hormone cycle, when the endometrium is theoretically at its thinnest.
Hyperplasia is less common during the reproductive years, but it may occur with
persistent anovulatory cycles, with polycystic ovarian disease, and in obese women
with increased production of endogenous estrogens.
Hyperplasia may also be seen in women with estrogen-producing tumors, such
as granulose cell tumors and thecomas of the ovary.
Because hyperplasia has a nonspecific sonographic appearance, an endometrial
biopsy is necessary for diagnosis. Sonohysterography can also be performed to
evaluate the internal structure of the endometrial canal.
Most women with postmenopausal uterine bleeding are experiencing endometrial
atrophy.
On transvaginal sonography, an atrophic endometrium is thin, measuring less than
5 mm.
If the postmenopausal patient has irregular bleeding and a thickened endometrium,
this may warrant a sonohysterography procedure or an endometrial biopsy.
Ultrasound is used to help the clinician triage which patients are candidates for
biopsy. Clinicians may use the endometrial measurement alone (for example, greater
than 5 to 8 mm without bleeding), or they may use symptoms as their criteria (for
example, less than 5 to 8 mm with bleeding).
Sonographic Findings
The endometrium is usually diffusely thick and echogenic with well-defined margins.
Focal or asymmetric thickening can occur. Small cysts representing dilated cystic
glands may be seen within the endometrium.
Although cystic changes within a thickened endometrium are more frequently
witnessed in benign conditions, they can also be observed in endometrial carcinoma.
Endometrial Hyperplasiaa

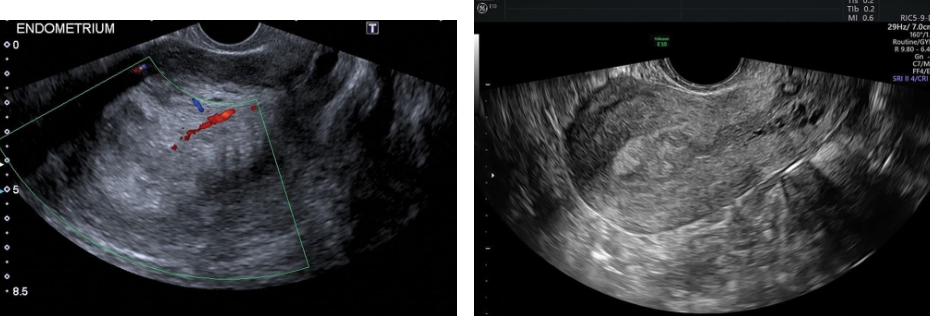
Patient with ________can be asymptomatic, or they may present with uterine
bleeding.
Histologically, polyps are overgrowths of endometrial tissue covered by epithelium.
They contain a variable number of glands, stroma, and blood vessels. Approximately 20% of
endometrial polyps are multiple.
They may be pedunculated, be broad-based, or have a thin stalk.
They typically cause diffuse or focal endometrial thickening and are more frequently seen in
perimenopausal and postmenopausal women.
In menstruating women, they may be associated with menometrorrhagia or infertility.
In postmenopausal women, especially those being investigated for bleeding, the major
differential considerations are hyperplasia, submucosal myomas, or, less commonly,
endometrial carcinoma.
Sonographic Findings
Sonographically, polyps appear toward the end of the luteal phase and are represented by a
hypoechoic or isoechoic region within the hyperechoic endometrium.
They initially may appear as nonspecific echogenic endometrial thickening.
The polyp may be diffuse or focal and may also appear as a round echogenic mass within the
endometrial cavity.
Cystic areas representing histologically dilated glands may be seen within a polyp.
A feeding artery in the pedicle may be identified with color Doppler.
Individual polyps are better visualized when outlined by intracavitary fluid.
Sonohysterography is a valuable technique when transvaginal sonography is unable to differentiate an
endometrial polyp from a submucosal leiomyoma. Color Doppler sonohysterography can be
particularly useful in discriminating polyps from submucosal myomas based on the presentation of
feeding vessels. Polyps present most often with one primary feeding vessel, whereas myomas typically
have multiple microvessels arising from the inner myometrium.
Endometrial Polyps
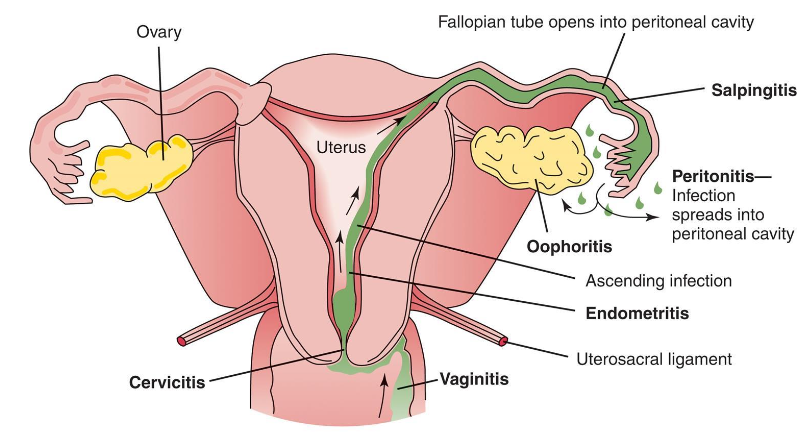
Endometrial thickening or fluid may indicate _______________ ?
………… is an infection within endometrium of the uterus.
It occurs most often in association with PID, in postpartum state, or following
instrumentation of uterus.
In patients with pelvic infection, uterus is conduit for infectious spread to tubes and
adnexa.
Postpartum patients may develop endometritis after prolonged labor, vaginitis,
premature rupture of the membranes, or retained products of conception.
Clinically, patient has intense pelvic pain.
Sonographically, the endometrium appears prominent, irregular, or both, with a
small amount of endometrial fluid.
Pus may be demonstrated in the cul-de-sac as echogenic particles or debris.
Enlarged ovaries with multiple cysts and indistinct margins may be seen secondary
to periovarian inflammation.
Dilation of the fallopian tube shows fluid-filled tubular shapes in a folded
configuration and well-defined echogenic walls.
A thickened tubal wall (5 mm or more) indicates acute disease. These should be
distinguished from a fluid-filled bowel by gentle compression on the pelvic wall to
look for peristalsis or movement in the bowel lumen.
Sonographic findings
Endometrium may appear thick, contain fluid, air or clot or appear
normal.
Endometrium considered normal up to 20 mm.
Measurement of >20 mm should raise suspicion of endometritis,
hemorrhage, or retained products of conception.
Risk for endometritis increases with premature rupture of
membranes, retained clot or POCs and prolonged labor.
As the infection worsens, periovarian adhesions may form and fuse the inflamed tube and
ovary, called the tubo-ovarian complex.
Further progression results in a tubo-ovarian abscess that appears as a complex
multiloculated mass with septations, irregular shaggy margins, and scattered internal echoes.
There can be posterior enhancement and a fluid-debris level. Gas bubbles are present in rare
cases; however, these also are observed in normal postpartum patients.
In the immediate postpartum period, the presence of retained tissue is difficult to distinguish
from inflammatory debris or blood clots.
The sonographic appearance can be similar to that of other adnexal masses, so clinical
correlation is important.
Sonography can also be useful in following the response to antibiotic therapy or in guided
transvaginal aspirations and drainage. If the aspirate is purulent, catheter drainage is used.
Endometritis

Intrauterine synechiae (endometrial adhesions, Asherman syndrome) are found in women with
posttraumatic or postsurgical histories, including uterine curettage. Synechiae can cause infertility
or recurrent pregnancy loss.
Sonographic Findings: Ultrasonography may demonstrate bright echoes within the endometrial cavity
in this condition.
The diagnosis is difficult unless fluid is distending the endometrial cavity. This is best identified
during the secretory phase when the endometrium is more hyperechoic.
Synechiae are more easily observed in the gravid uterus, where they appear as a hyperechoic band
traversing the uterus from anterior to posterior.
Sonohysterography is an excellent technique for demonstrating adhesions and should be performed in
cases of suspected adhesions. Adhesions appear as bridging bands of tissue that distort the cavity or as
thin, undulating membranes that connect from one side of the uterus to the other. Thick, broad-based
adhesions may prevent distention of the uterine cavity. Adhesions can be divided under hysteroscopy.
Synechiae
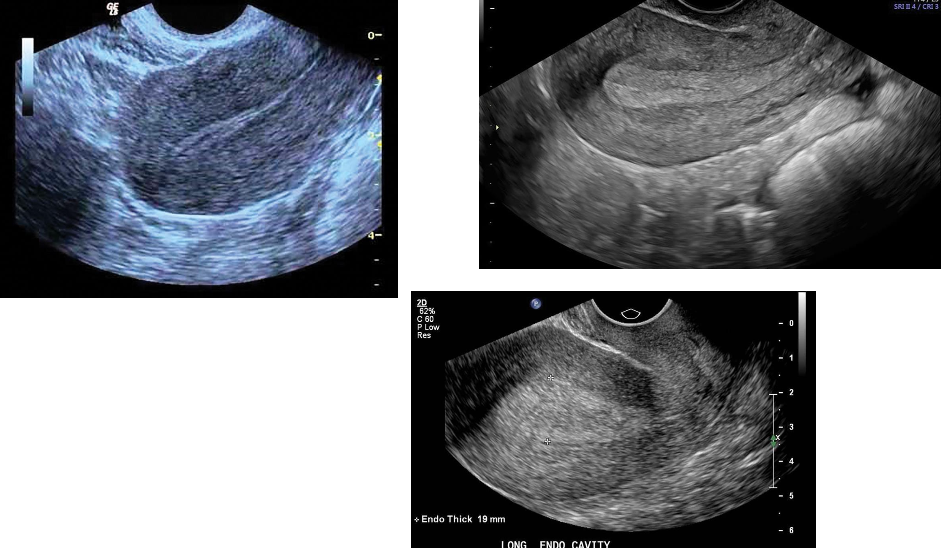
___________is the most common gynecologic malignancy in North America, and its
incidence has been rising.
Most endometrial malignancies are adenocarcinomas occurring in postmenopausal patients.
The most common clinical presentation is uterine bleeding, although only 10% of women with
postmenopausal bleeding will have endometrial carcinoma.
There is a strong association with replacement estrogen therapy.
In the premenopausal woman, anovulatory cycles and obesity are also considered risk factors.
The earliest change of endometrial carcinoma is a thickened endometrium. An abnormally thick
endometrium is also associated with endometrial hypertrophy and polyps.
Although increased endometrial thickness is an early finding in endometrial carcinoma,
enlargement with lobular contour of the uterus and mixed echogenicity are correlated with
more advanced stages of the disease. The risk of malignancy increases with the presence of a
large endometrial fluid collection or clinical symptoms, such as abdominal pain or bleeding.
Endometrial carcinoma may obstruct the endometrial canal, resulting in hydrometra or hematometra.
The level of myometrial invasion (superficial versus deep) also can be detected by transvaginal ultrasonography, although
contrast-enhanced MRI is more sensitive. MRI is also valuable in evaluating extrauterine extension and involvement of
lymph nodes.
Tamoxifen, a nonsteroidal antiestrogen compound, is widely used for adjuvant therapy in premenopausal and
postmenopausal women with breast cancer and has secondary effects on the endometrium.
An increased risk of endometrial carcinoma, hyperplasia, and polyps has been reported in patients on tamoxifen therapy. On
sonography, tamoxifen-related endometrial changes are nonspecific and similar to those described in hyperplasia, polyps, and
carcinoma. Because it may be difficult to distinguish the endometrial-myometrial border in many of these patients,
sonohysterography is valuable.
Sonography may be helpful in staging carcinoma and in distinguishing between tumors limited to the uterus (stages I and II)
and those with extrauterine extension (stages III and IV). Both MRI and CT are useful in staging by demonstrating
lymphadenopathy and distant disease (stages III or IV). Endometrial biopsy is usually required for a definite diagnosis.
Sonographic Findings
Transvaginal examination is helpful in screening for early changes of endometrial hyperplasia or carcinoma
by accurately measuring endometrial thickness.
Sonographically, a thickened endometrium (greater than 4 to 5 mm, and this value varies institution to
institution) should be considered cancer until proven otherwise.
Demonstration of myometrial invasion is clear evidence for endometrial carcinoma.
Transvaginal ultrasonography demonstrates myometrial invasion as thickening and irregularity of the central
endometrial interface with echogenic or hypoechoic patterns combined with infiltration of hyperdense structures
in the myometrium.
Cystic changes within the endometrium are more commonly seen in endometrial atrophy, hyperplasia, and polyps
but can also be seen with carcinoma.
Endometrial masses containing numerous vascular branches with color imaging should also raise the level of
suspicion for carcinoma.
Endometrial Carcinoma
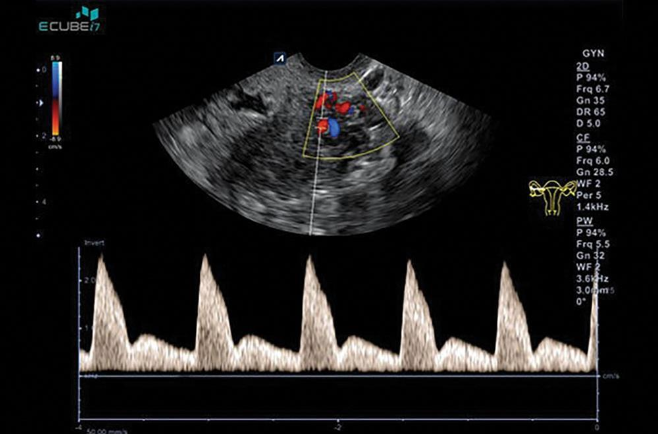
What may help distinguish between benign and malignant endometrial thickening?
Doppler Ultrasonography of the uterine artery
_____________is used to evaluate the resistive index (RI = peak systolic
− end diastolic/peak systolic) or pulsatility index (PI = peak systolic −
end diastolic/mean).
Pulsed Doppler
_____________(RI less than 0.4) has been found in patients with
endometrial carcinoma
Low Resistance flow
______________-(RI greater than 0.5) in normal or benign endometria.
High resistance flow
What are the common Regimens in Menopausal Women?
1. No hormones
2. 3. 4. Unopposed estrogen (usually Premarin); if uterus is present, unopposed estrogen is associated with increased
risk for endometrial hyperplasia or carcinoma.
Continuous/combined estrogen and progesterone (Premarin and Provera):
➢ Combination produces endometrial atrophy after 3 to 6 months.
➢ Usually no risk of endometrial cancer
➢ Women may have “breakthrough” bleeding during month and/or annoying progesterone side effects (i.e., irritability, depression, bloating,
breast tenderness)
Sequential estrogen and progesterone (Premarin first half, then Provera second half of month)
➢ Women have predictable withdrawal bleeding at end of each month.
What are the beneficial effects of ESTROGEN?
Alleviates menopausal symptoms (hot flashes, night sweats, painful intercourse)
Reduces risk of osteoporosis, vertebral and hip fractures
Reduces risk of heart attacks, strokes
What are the beneficial effects of PROGESTERONE?
Produces endometrial atrophy
Reduces risk of endometrial hyperplasia/cancer
What are the Negative effects of the ESTROGEN?
Increases risk of endometrial hyperplasia/cancer
What are the Negative effects of the PROGESTERONE?
Increases risk of breast cancer
Causes irritability, depression, breast tenderness in some women
____________________also occur with ectopic pregnancy,
endometritis, degenerating myomas, and recent abortion.
Sonographic Findings: Transvaginal sonography, with its improved resolution,
sometimes shows tiny endometrial fluid collections not seen on transabdominal
scans.
………………………. (less than 2 mL) are common in women
during the menstrual phase of the cycle. They are seen in postmenopausal
women, especially during the menstrual phase in women taking sequential
hormones.
In a uterus with a fluid collection, the anteroposterior diameter of the fluid should be
subtracted from the endometrial measurement for a true assessment of endometrial
thickness.
Small Endometrial Fluid Collections
should be regarded with suspicion.
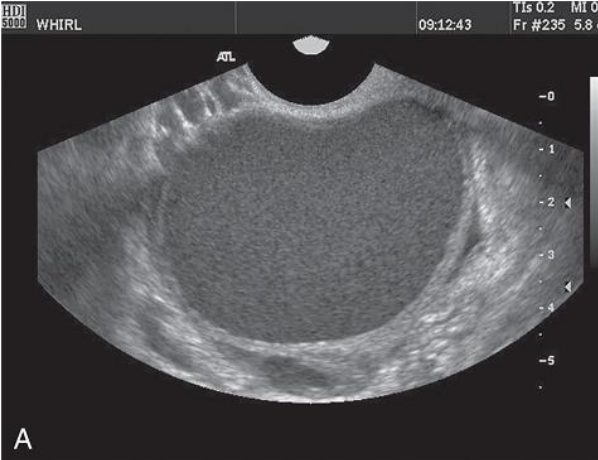
Obstruction of the cervical os results in the accumulation of secretions, blood, or both in the
uterus.
Before menstruation, the accumulation of secretions is referred to as hydrometrocolpos.
Following menstruation, hematometrocolpos results from the presence of retained menstrual
blood.
The obstruction may be congenital, imperforate hymen (most common), vaginal septum,
vaginal atresia, or a rudimentary uterine horn. Hydrometra and hematometra may also be
acquired as a result of cervical stenosis from endometrial or cervical tumors or from post-
irradiation fibrosis.
They may also be caused by uterine, cervical, tubal, or ovarian carcinoma. Hyperplasia and
polyps also cause endometrial fluid collections, so these collections also indicate increased risk of endometrial carcinoma.
However, large amounts of endometrial fluid also are associated with benign conditions,
such as congenital anomalies or cervical stenosis from prior instrumentation or childbirth.
The patient typically complains of abdominal pain and has an enlarged abdominal mass. She
may or may not have vaginal bleeding. The presence of fever suggests infection of the blood
collection.
Laboratory results show an elevated white blood cell count. In simple hematometra, the
uterine cavity returns to normal promptly after dilation and curettage. Pyometra is more
likely to occur with uterine cancer. Abnormal development of the vagina or uterus may
result in a cystic uterine or vaginal collection of mucus in children. When menstruation
begins, the collection consists of blood.
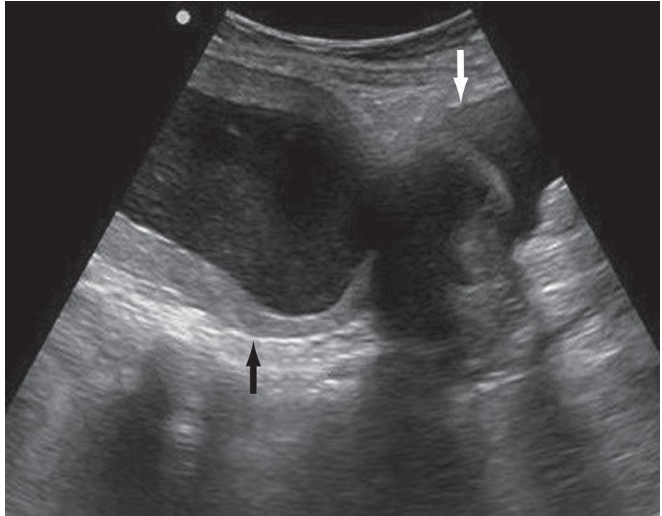
Sonographic Findings: The sonographic picture of large endometrial cavity fluid collections
is that of a centrally cystic, round, moderately enlarged uterus. This may contain echogenic
material if pus or blood is present.
Large Endometrial Fluid Collection