Muscular System (L4-6)
1/103
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
104 Terms
Describe the different types of Muscle
What are they? What are their characteristics?
Hint: which are straited/non striated; voluntary/involuntary
Skeletal
Voluntary, Striated
Cardiac
Striated, Involuntary
Smooth
Non-Striated
Involuntary
What does it mean to be voluntary? Involuntary?
Voluntary means we choose to move it;
Involuntary is automatic and occurs without our input
What does it mean to be striated? Unstriated?
striated has long/thin parallel streaks
unstriated lacks these lines

Which is striated, unstriated, and cardiac?
STRIATED || UNSTRIATED || CARDIAC
Does voluntary or Involuntary muscle use more ATP
Voluntary
What are the defining traits of skeletal muscle fiber / cells (5)
• It contains many mitochondria.
• It is multinucleated.
• It has special structures called Transverse tubules (T tubules).
• It has myofibrils and sarcomeres.
• It has specific terms for some of the intracellular structures
ex: Sarcolemma = Plasma membrane
Sarcoplasm = Cytoplasm
Sarcoplasmic reticulum = Smooth ER
Sarcolemma =
Sarcoplasm =
Sarcoplasmic reticulum =
Why do these new names exist??
Plasma membrane
Cytoplasm
Smooth ER
they are more developed / specialized, but are somewhat similar
Controlled contraction of muscle allows:
1) Purposeful movement of the whole body or parts of the body
2) Manipulation of external objects
3) Propulsion of contents through various hollow internal organs
4) Emptying contents of certain organs to the external environment
Humans are ____% muscle with ____ having more skeletal muscle than the opposite sex
~50
men
What muscle type has intercalated disks?
what do they do?
cardiac
connect the cardiac tissue
Light muscle is only ____; whi;e dark is mainly ______
Actin
Myocin
What does the mitochondria do for muscle fiber
It provides energy / ATP
What does the Neuromuscular Junction (NMJ) do?
It is a specialized synapse/connection where motor neurons/nerve cells communicate with muscle fiber causeing a signal that results in contraction via an efferent signal from the brain
How does the NMJ signal to initiate contraction?
1) an Action Potential (AP) travels down the motor neuron’s axon and reaches the presynaptic terminal / boutin
2) AP causes Depolerization in the terminal
→ causes voltage gated Calcium channels to open in the terminal
→ Calcium ions enter the neuron
3) Calcium ions fom Acetylcholine (ACh) in the synaptic cleft
4) ACh diffuses across the cleft; binding to ACh receptors on the posthaptic pathway
→ binding causes calcium to flow into the muscle fiber
5) the membrane depolarize (end plate potential) and if end plate potential reaches the threshold sodium channels
6) If thresh holds open, AP enters the muscle fiber
→ AP spreads from. muscle fiber to muscle fiber membrane into the T Tubules
→ enters the sarcoplasmic reticulum
→ activates more CA channels
→ CA enters the muscle fiber cytosol
7) CA enters muscle fiber cytosol
8) Muscle Contraction occurs via the Cross Bridge Cycle
→ Calcium binds to the troponin and moves tropomyosin
→ exposes the actin binding site
→ cross bridge starts
what is end plate potential
a localized depolarization of the muscle fiber membrane at the neuromuscular junction
When does muscle contraction stop
ACh is broken down by Acetylcholinesterase is the cleft
Muscle contraction requires what nutrient/ion
Calcium
explain the cross bridge cycle
1) Energization of the myosin head
→ myosin head has ADP and Pi from a broken down ATP
→ If no Calcium is introduced, muscles remain at rest
→ If calcium is present it proceeds to step 2
2) Excitation → Myosin head // cross bridge binds to the Actin
→ Requires calcium be present to open tropomyosin and reveal the binding site
2.5) Cross Bridge closed the Pi but not the ADP
3) Power Stroke
→ head ‘bends back’ due to the Pi leaving
→ ADP detatches
→ Power Stroke does not move myosin, ONLY the actin
4) Contraction occurs
5) New ATP binds and is broken down into ADP and Pi
→ cycle repeats
what is the cross bridge
the attachment point where myosin heads bind to the actin filament
Order of the parts of the muscle
Muscle
Muscle fiber and Connective Tissue
Myofibril
A bands and I bands
Sacromere
Z line, M line, H Zone
Thick Filament (myosin)
Thin Filament (actin)
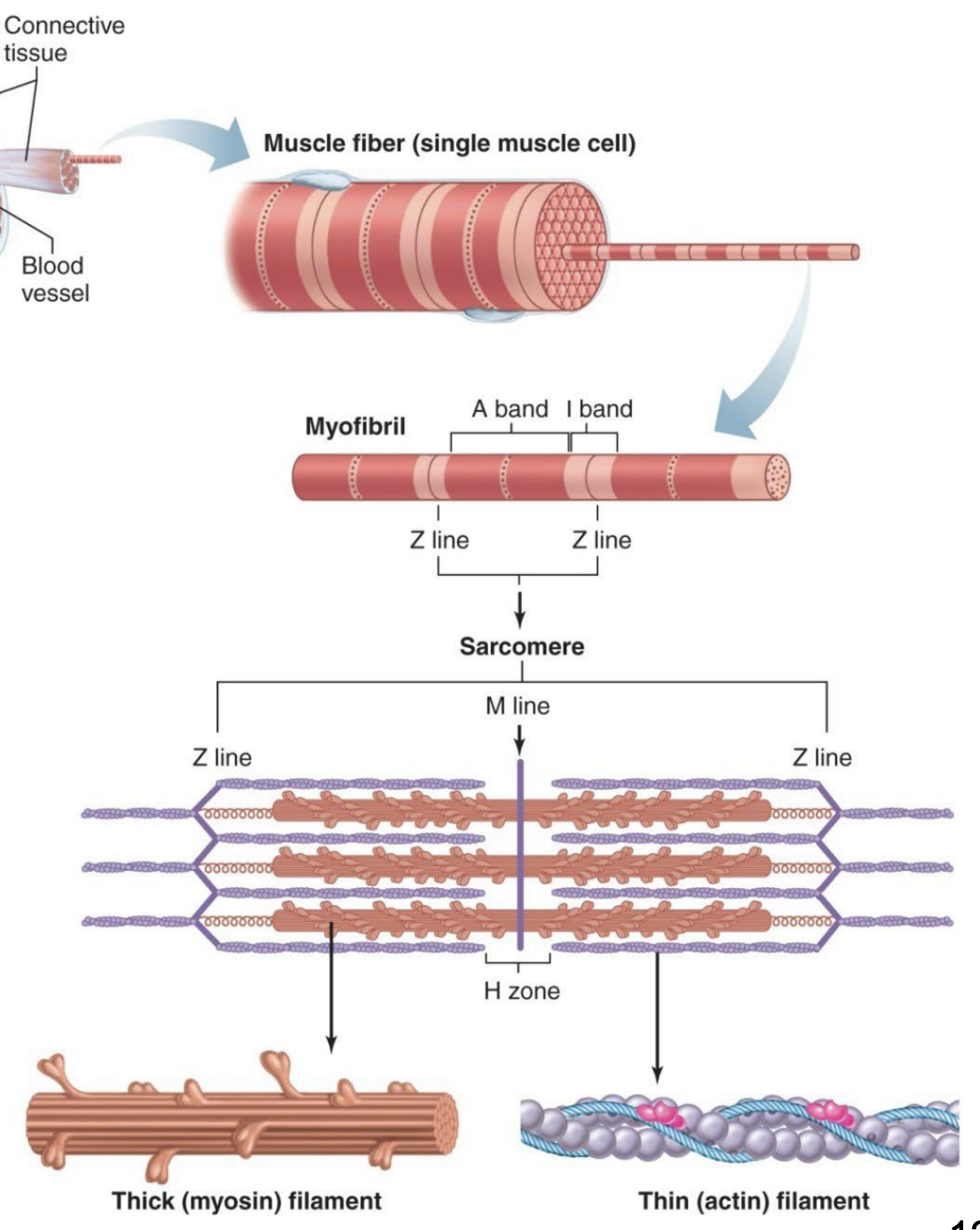
Muscle
population of elongated muscle fibers held together by connective tissue and connected at either end by tendons.
Myofibril
elongated, cylindrically-shaped contractile elements composed of a population of sarcomeres connected end-to-end.
Every myosin is surrounded by ____ actin
every actin is surrounded by ____ myosin
6
3
sacromere is the region between
two Z-Lines
Z lines are in the middle of
I bands
A bands are the area between
two I bands
M lines are in the middle of
A bands
sacromere are made up of what?
Thick and thin filiment
(myosin and actin)
Muscles are made of _______, which are made of ________
muscle fibers
myofibril
I bands cover 2 parts of _____
sacromeres
What are T-Tubules
T Tubules are an extension of the the membrane throughout / within the muscle cell
Sarcoplasmic Rheticulum surrounds what two things
T Tubules and Myofibrils
Is there myocin in the I band
No, only the A band
Sarcomere
the smallest unit of a muscle cell containing all of the elements necessary for contraction.
- Composed of interdigitating and partially-overlapping thick and thin filaments.
What is Titin and what does it do
Connexts to the Z line to hold myosin in lace
Helps maintain sarcromere structure
Thick filiments are assemblies of _____
myosin
Myosin
cytoskeletal protein composed of two interwoven subunits, each with a long tail and a globular head region.
myosin head-actin binding site
specialized region of the myosin head capable of binding to actin
myosin ATPase
specialized region of the myosin head capable of ATP hydrolysis
the three parts of troponin and what they do
Troponin I → Inhibits interaction bw actin and myosin
Troponin T → tropomyosin binding site (helps with contraction)
Troponin C → Calcium Binding
Thin Filament
specialized assemblies of three proteins, actin, tropomyosin and troponin, arranged to form an elongated double helical strand.
Actin
Globular cytoskeletal protein linked to form two long chains arranged in a double helical strand.
Tropomyosin
pairs of threadlike filamentous proteins that lie alongside the groove formed by the actin helix.
Troponin
protein complex composed of three subunits, one that binds to actin, one that binds to tropomyosin, and one that binds Ca+. Multiple copies of this complex_are bound to the strands of actin and tropomyosin
What happens during muscle contraction
(what change in size)
1) Sarcomere shortens Thick filament Thin filament
2) H zone becomes shorter
3) I band becomes shorter (since actin binds to myosin)
4) A bands maintains the same width
5) Individual actin and myosin fibers maintain a constant length
Myosin cytoskeleton looks like
two interwoven parts with a head and tail
each head has actin bind site and myosin ATPase site
G actin vs F actin
G is monomer
F is filiment
what does ATPase do
Site can do ATP hydrolosis and break ATP to get energy for muscle contraction
What are foot proteins and where can you find them
AKA ryanodin receptor
Span the gap b/w lateral sacs and T-Tubules
help w muscle contraction and play a role in excitation-contraction coupling
What do T Tubules hold
Calcium
What happens when T Tubules depolerize
they activate Dihydropyridine receptors → open Ca channels in foot protein/lateral sacks
What is the functional unit of skeletal muscle
Sacromere
defines boundary of sarcomere; site where thin filaments attach
Z Line
made up of thick filaments along with portions of thin filaments that overlap
A Band
lighter area within middle of A band where thin filaments do not reach
H Zone
extends vertically down middle of A band within center of H zone
M Line
consists of remaining portion of thin filaments that do not project into A band
I Band
muscle fiber traits
A single skeletal muscle:
- multinucleated
– large, elongated, and cylindrically shaped
– fibers extend entire length of muscle
Dihydropyridine Receptor
receptor proteins in the transverse tubule membrane that come into contact with the foot proteins. They are voltage dependent and gate the change in permeability of the foot proteins to Ca++.
Dihydropyridine receptor is located in the
membrane of the T tubule
Ryanodine receptor is located in the
membrane of the S.R.
Excitation-Contraction Coupling:
Muscular contraction occurs when the thick and thin filaments within a sarcomere slide past one another.
The sliding action is mediated by a complex sequence of chemical reactions called the power stroke
Muscle fibers are composed of:
myofibrils
thick filament =
thin filament =
myosin
actin
during contraction what gets smaller and what stays same
thick and thin move in so:
sarcomere shorten
H, I shorten
A stays same size
Actin and myosin stay same size
Muscle Mechanics
whole muscles are groups of muscle fibers bundled together by connective tissue and attached to bones by tendons
Motor Unit and key traits
A motor neuron and all of the muscle fibers it innervates
1) One motor neuron innervates multiple muscle fibers
2) When a motor neuron is activated, all of the muscle fibers it innervates are stimulated to contract simultaneously
3) muscle fibers innervated by a given motor neuron are distributed throughout the muscle (AKA, it allows for evenly distributed contractions)
Motor Unit Recruitment:
the process of increasing the number of motor units that participate in muscle contraction.
weak contraction → ______ motor units
strong contraction → ______ motor units
few (1 goes, but not 2 or 3)
many (more and more, its a spectrum)
T/F
The number of muscle fibers per motor unit and the number of motor units per muscle vary widely, depending on the specific function of the muscle
true
more fine / delicate (dexterity) movements have _____ fibers +example
fewer muscle fibers
Fingers
Broad, powerful movemines have ______ muscle fibers + example
more
Legs
Muscle Tension
depends not only on the number of motor units recruited and on the tension developed by each contracting fiber
4 factors influence the extent to which tension can be developed in a fiber
1) The frequency of stimulation.
2) The length of the fiber at the onset of contraction
3) The extent of fatigue
4) The thickness of the fiber
What keeps muscle tension within a set possible range (in humans, not in a lab)
bones
what is a twitch
The mechanical response of a muscle fiber to a single action potential
Twitches occur when…
a bigger twitch occurs when…
there is a small AP spacing
There is not enough time for muscle to relax
there is less and less time between AP
what is tetanus and when does it occur
- a smooth, sustained contraction of maximal strength
- three to four times stronger than a single twitch
- prevents function at max strenght
it occurs when there is VERY LITTLE time between between end and start of AP //
Occurs if muscle fiber is stimulated so rapidly that it does not have a chance to relax between stimuli
Motor Unit Recruitment
recruitment of X-number of motor units for various muscle contractions (more units, bigger contraction, more force on load)
MUR is the recruitment of more motor proteins
asynchronous recruitment
recruit in pairs for contraction
ex: 2 and 4 work together, and 1 and 3 work together
prevents fatigue
Twitch summation
the increase in tension accompanying repetitive stimulation of a muscle fiber (twitches build)
→ AP is shorter than the twitch
→ Results from sustained elevation of cytosolic calcium upon repetitive stimulation
→ causes tetanus
explain the Length Tension Relationship
fiber tension depends on lenght
→shorter muscle is less optimized
→loger muscle have more tension
→Bones limit muscle shortening and help maintain tension
Methods of Muscle Metabolism (In Order) + explain
Creatine Phosphate
- provides a reserve of high energy phosphate for synthesis of ATP
- excess ATP generated by glycolysis and oxidative phosphorylation, is converted to creatine phosphate / stored by muscle cells as reserve
Oxidative Phosphorylation
- aerobic metabolism of glucose and fatty acids.
uses myoglobin from the muscle
-Oxygen from ETC usually
Glycolosis
- anaerobic metabolism of glucose.
The biproduct, excess pyruvic acid, is converted to lactic acid that is removed by the bloodstream.
Creatine Phosphate EQ
creatine phosphate + ADP <-> creatine + АТР
describe Fatigue
inability of muscle to maintain tension.
Can result from muscle fatigue or neuromuscular fatigue.
Muscle fatigue + influencing factors
exercising muscle can no longer respond to stimulation with the same degree of contractile activity.
1) depletion of glycogen reserves.
2) local increases in inorganic phosphate from ATP breakdown
must replenishment of muscle glycogen and creatine phosphate following intense activity
Neuromuscular fatigue
inability of the NMJ to synthesize ACh rapidly enough to sustain chemical transmission of AP's from the motor axon to the muscle cell.
No contraction occurs
Central fatigue
when the CNS no longer adequately activates motor neurons
Excess post-exercise oxygen consumption (EPOC)
the need for elevated O2 uptake during recovery from exercise.
Types of skeletal muscle
Type 1 (slow oxidative)
Type 2A (fast contract)
Type 2b (very fast contract)
describe type 1 skeletal muscle
slow oxidative
slow contraction and reliance on oxidatve phosphorylation for ATP. - high in mitochondria, blood supply, and myoglobin
describe type 2a skeletal muscle
fast contract
fast contraction and reliance on oxidatve phosphorylation for ATP.
- high in mitochondria, blood supply, and myoglobin.
describe type 2b skeletal muscle
very fast contraction and reliance on glycolysis forATP.
- low in mitochondria, blood supply, and myoglobin
- high in muscle glycogen.
smooth muscle
muscle fibers are located in the walls of hollow organs and tubes such as blood vessels and the intestines. Not Striated
Have dense bodies
where do dark bodies attatch
filiments
smooth muscle has tropomyosin but not _____
troponin
key traits of smooth muscle
not straited
involuntary
mononucleated
dense bodies
tropomyosin no troponin
calmodulin
NO T TUBE
Multi-unit smooth muscle plus examples
smooth muscle cells that are activated by neuronal input (neurogenic).
Examples: (1) walls of large blood vessels
(2) large airways to the lungs
(3) muscles of the eye that adjust the lens
(4) iris of the eye
(5) at the base of hair follicles (“goose bumps")
Single-unit smooth muscle plus example
smooth muscle cells capable of generating pacemaker activity that are coupled into a functional syncytium by gap-junctions.
Examples:
(1) walls of the digestive tract
(2) walls of the reproductive tract
(3) walls of the urinary tract
(4) walls of small blood vessels
Pacemaker Potential
Gradual depolarization until threshold is reached
NOT AP