Speech Disorders FINAL Exam
1/118
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
119 Terms
Disfluency Types:
Stuttering
Acquired (neurogenic) Stuttering
Psychogenic Stuttering
Cluttering
Stuttering begins…
In childhood, no known cause
Acquired (neurogenic) stuttering results from…
Brain trauma, disease, meds
Psychogenic Stuttering results from…
Emotional or psychological trauma
Not all disfluency is stuttering, not all stuttering is disfluency
Disfluency Definition
Repetitions, hesitations, and disruptions in the forward flow of speech
Everyone is disfluent sometimes
Stuttering Definition
Abnormally high frequency and/or duration of stoppages in the forward flow of speech
Inner feeling of loss of control
Often accompanied by secondary behaviors
Primary/Core Stuttering Behaviors
Repetitions (sounds/syllables, words, phrases are repeated)
Prolongations (sound is elongated)
Blocks (no sound is produced)
Secondary/Accessory Stuttering Behaviors
Eye aversion
Avoidance
Verbal interjections
Abnormal head or body movements
Circumlocution
Word substitution
Fluency-Enhancing Conditions
Singing or whispering
Speaking in a different voice, accent
Choral reading, talking in unison
Talking when alone, to babies or pets
Speaking to a metronome, AAF
Possible Explanations for Fluency-Enhancing Conditions
Distraction
Altered social dynamics
Rate (slower rate = more fluency)
Different self-monitoring
using speech mechanism differently
Represent situations in which person has stuttered before and associated with embarrassment or shame
Anxious feelings increase stress and resulting muscular tension
Genetic Theory
Stuttering stems from hereditary, genetic component
Twin studies: monozygotic twins have higher concordance than dizygotic twins
Family studies: genes linked to dopamine receptors and lysosomal storage
Genes interact with environmental factors
Genetic Influence
4 genes have been identified that account for ~20% of cases of persistent stuttering
Polygenetic disorder: diabetes, Alzheimer’s, schizophrenia
Diagnosogenic Theory
Behaviors the child exhibits are mostly hesitations and repetitions normally seen in all children
Parents react with increased criticism and punishment
Parents mislabel normal disfluencies as “stuttering” → make child self-conscious → child tries to avoid disfluencies → more negative reactions → stuttering
Etiology of Stuttering
Arises from complex dynamic interactions between internal factors and external conditions
Internal Factors:
Inherited traits, temperament, cognitive abilities, language abilities, information processing mechanisms, speech motor control abilities
External Conditions
Culture, dynamics of home life, child rearing practices, educational experiences, social relationships
Normal Disfluencies
Increase in children around 2 to 3 years
Revisions, pauses, interjections, effortless repetitions of phrases and words
Normal disfluencies persist throughout life: interjections, repeating, revising
Stuttering Characteristics
Sound/syllable, monosyllabic word repetitions
Sound prolongations
Within-word pauses
Tense pauses and hesitations
Blocks
Internal feeling of loss of control
Often effortful/tense
Onset of Stuttering
Between 2 and 4 years in ~95% of cases
Mean age of onset: ~34 months
Development of Stuttering
Usually gradual
Severity often increases as child ages
~50%: at least on physical concomitant (visible tension, irregular breathing, head movements)
Some kids learn to hide it so severity appears to decrease with age
Common speech/language disorder that coexists with stuttering in children
Phonological impairment
Stuttering Impact
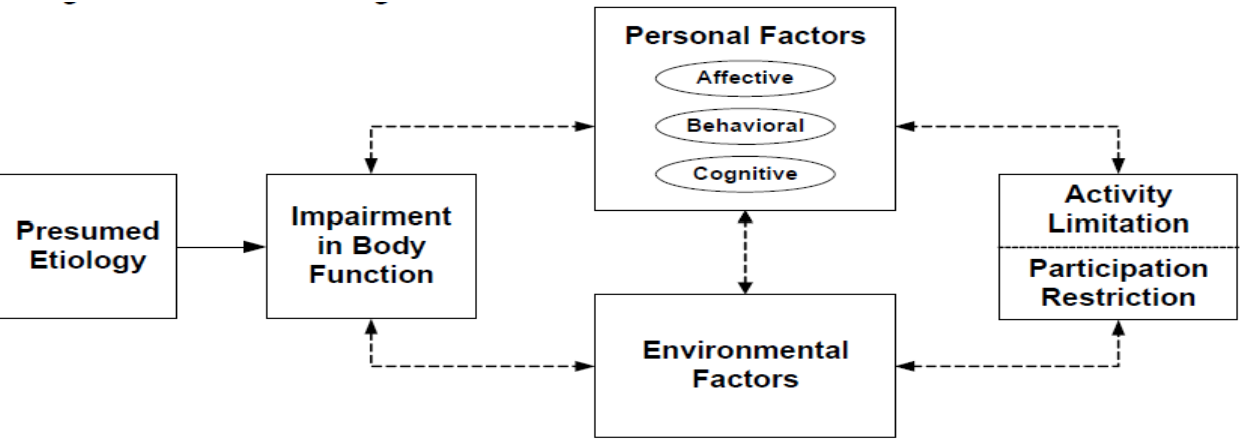
W.H.O.: look beyond disfluencies to client’s personal reaction, environmental reactions, participation restrictions and activity limitations
Can have negative affect on daily activities (school performance, employment, social interactions)
Can profoundly affect an individual’s self-confidence, self-esteem
Common myths about stuttering
People who stutter are more introverted
People who stutter are more anxious
Parents of children who stutter are more anxious
People who stutter have lower intelligence
People who stutter have less self-confidence
People who stutter are more sensitive
Communication with a person who stutters
Maintain normal eye contact
Do not interrupt
Do not finish their words, sentences
Pay attention to what the person is saying, not how they’re saying it
Be aware of how common stereotypes may be influencing your opinion of the person who stutters
Two Main Questions at Onset
Is my child stuttering
Diagnosis: either yes or no
Does my child need treatment
Prognosis: less clear cut, depends on many factors
Evaluation of Stuttering in Preschoolers
Case History: medical history, developmental history, speech and language milestones
More specific questions: when did the stuttering begin? has it changed over time? situations that make stuttering more or less severe; family dynamics; does it run in the family?
Stutter-like disfluencies vs normal disfluencies
Stutter-like:
part-word repetition (“b-but”, “thi-thi-this”)
single-syllable word repetition (“you you you”, “and and”)
dysrhythmic phonation: (“mmmmy”, “cooookie”), blocks (“—toy”), broken words (“o—pen”)
Normal:
interjection ('“um”, “uh”)
revision/abandoned utterances (“Mom ate/Mom fixed dinner”, “I want/Hey look at that”)
multisyllable/phrase repetition (“because, because”, “I want, I want to go”)
Counting Disfluencies
Repetitions of sounds, syllables, or words are counted as one disfluent word
Prolongations of sounds are counted as one disfluent word regardless of the number of iterations
Blocks on a word are counted as one disfluent word regardless of the durations of the block
Unnaturally long pauses are counted as one disfluent word
Revisions are counted as one disfluent word
In reading: the omission, modification, or addition of a word or words is counted as one disfluent word
Fillers and starters are counted as disfluent words (um, uh, etc.)
Preschool Speech Sample
Analysis of child’s speech behaviors
Types of disfluencies
Frequency and duration of disfluencies
Visible/audible secondaries
Bilingualism
Disfluencies can reach 7% when the average bilingual child is 2-4 yrs old
May be inherent to the processing involved in the production of spoken language in bilinguals
Prognosis: Risk Factors
Family History: especially if there are relatives who persisted in stuttering (less risk if family member outgrew stuttering as a child)
Sex: more males become persistent, more females recover and do so quicker
Age at onset: children who begin stuttering before age 3½ are more likely to recover
Time since onset: longer than 6 months → may be less likely to spontaneously recover
Standardized Assessments:
Stuttering is often comorbid with other S/L disorders
Articulation: GFTA-4
Language: PLS-5, TELD-4, TOLD-P
Space out testing and play to minimize fatigue in young children
The International Classification of Functioning, Disability, and Health
Severity Assessment for School-age kids & adults
Perceived by the listener
Frequency, duration, tension of stuttering
Includes observable secondary behaviors
Affective & Cognitive Factors Assessment for School-age kids & adults
Feelings and attitudes about stuttering and communication in general
Quality of Life Assessment for School-age kids & adults
How limiting is the disorder?
School, employment, social relationships, self-image, etc.
Assessing severity in school-age kids & adults
Some clinical relevance because it captures what listeners experience
Provides numerical score or discrete category/level supposedly needed for insurance or educational purposes: but actually not
CAUTION: snapshot in time, observable features only, two clients can have very different stuttering patterns but same severity
Severity DOES NOT predict impact
Overall Assessment of the Speaker’s Experience of Stuttering (OASES)
Provides insights into global impact of stuttering
3 different forms
4 categories
Yields Overall Score and Impact Ratings (mild, mild-moderate, moderate, moderate-severe, severe)
3 different forms of OASES
7-12 yrs
13-17 yrs
18+ yrs
4 categories of OASES
General Information
Your Reactions to Stuttering
Communication in Daily Situations
Quality of Life
Assessing School-age Child
Similar to assessment for preschool-age children
Differences:
Reading sample
Negative emotions and attitudes likely to be stronger
Can ask child, parents, teacher about school experiences
Can talk to child directly about stuttering
Impact of Child’s Environment
Must understand how the child’s family responds to/thinks about child’s stuttering
I.e., family support/motivation
Assessing Child’s Feelings/Attitudes
Child’s comfort level is critical
How concerned is the child about their speech
What does the child know about stuttering
How does the child cope with stuttering
How does the child feel about self as a communicator
School-Based SLP
Collect info from teachers, parents, observations in class and therapy room
May test for concomitant issues as well
IEP team meets to discuss results
Does child’s stuttering meet state’s eligibility criteria?
Is stuttering negatively impacting the child? (academically or socially)
CO Communication Rating Scale:
A stuttering impairment does NOT exist when…
Disfluencies are part of normal speech development
Disfluencies do not interfere with educational performance resulting in a denial of free appropriate public education (FAPE)
Treatment Recommendation
Not all kids who stutter need treatment right now
If negatively impacting child, start therapy!
Parents need to know it’s ok for child to stutter
Child’s level of concern may not match parents’ or teacher’s
If children don’t feel like they need to change, they probably won’t
Types of Stuttering Therapy
Fluency-shaping therapy
Stuttering modification therapy
Stuttering-affirming approaches
Psychotherapeutic approaches
Electronic devices
Parent-directed intervention for preschoolers
Fluency Shaping Therapy Goals
Goal: increase fluency
Focus on slower, fuller breathing from the diaphragm
Slow speaking rate by:
stretching phenomes
slowing phenome or syllable transitions
more frequent pausing
Reduce vocal fold tension at the beginning of words
Reduce articulatory pressure
Fluency Shaping Therapy Results
Result is slow, monotonous, but fluent speech; only used in clinic
After mastering target speech behaviors, speaking rate and prosody are increased until more natural sounding
Fluent speech is transferred to daily life outside the speech clinic
Continue to refine/practice new speech patterns until they stabilize
Fluency Shaping Techniques
Light articulatory contacts/soft starts
Reduces tension in articulators by bringing them together gently and pulling apart slowly
Easy/gentle onsets
Gentle onset of voicing that gradually increases in intensity
Slowing Rate
Pausing/phrasing or slowing phonemes & syllable transitions
Stuttering Modification Therapy Goals
Modify moments of stuttering so they are less tense/briefer
Reduce fear of stuttering while eliminating avoidance behaviors associated with this fear
Assumes most school-age & adult PWS will never be normally fluent speakers, so goal is to be an effective communicator with some level of acceptable stuttering
Stuttering Modification Therapy Desensitization Causes More Control over Stuttering
Disclosing/advertising stuttering, openly talking about stuttering → Bouncing
Voluntary stuttering → Prolongation
Maintaining eye contact → Pullout
Putting self in feared situation → Cancellation
A stutter can be changed before, during, or after it occurs
4 Stages of Stuttering Modification
Identification
Desensitization
Modification
Stabilization
Stages of Stuttering Modification: Identification
Identify stuttering behaviors (core and secondary)
Feelings and beliefs
Learn how speech mechanism works
Stages of Stuttering Modification: Desensitization
Stutter openly, confront fears & avoidances
Stages of Stuttering Modification: Modification
Change how you stutter, do it more easily
Bouncing, prolonging, pull-outs, cancellations
Stages of Stuttering Modification: Stabilization
Generalize skills to the real world
Clients must becomes their own therapists and learn how to handle relapse
Electronic Devices
DAF
FAF
Masking
Rhythm
Electronic Devices to Reduce Stuttering
Changing how a PWS hears their voice usually improves fluency
May correct auditory processing underactivity
3 types of altered auditory feedback
DAF and FAF immediately reduce stuttering about 70-80% without training or therapy
Effects often diminish with time
3 types of altered auditory feedback
Delayed auditory feedback (DAF)
Frequency altered feedback (FAF)
Masked auditory feedback (MAF)
AAF outside the clinic
SpeechEasy: helps some PWS, not helpful for others
Effects tend to face with time
Treatment for Preschool-age Child Goal and Methods
Goal: eliminate stuttering, empower parents
Methods: indirect or direct therapy
Indirect Therapy
Manipulate environment & change how family interacts with child
Decrease factors that maintain/exacerbate stuttering
Increase factors that reduce stuttering
Slower rate
More pauses
Fewer questions
Simplified language
Direct Therapy
Target child’s aberrant speech behaviors, rather than environmental factors
Child alters the way in which he/she speaks
Usually conducted within clinic room by SLP, but parents can also deliver treatment
Effectiveness of Stuttering Intervention
Early diagnosis and treatment is best practice
Full recovery in school-aged children is unlikely
Stuttering decreases 60-80% regardless of therapy used
What is Cluttering?
Perceptually rapid, irregular speech with many disfluencies that is difficult to understand
Disfluencies are typically incomplete phrases, revisions, fillers (usually without tension)
Misarticulations: collapsing or distorting words
Disorganized language
Often poor self-monitoring/awareness
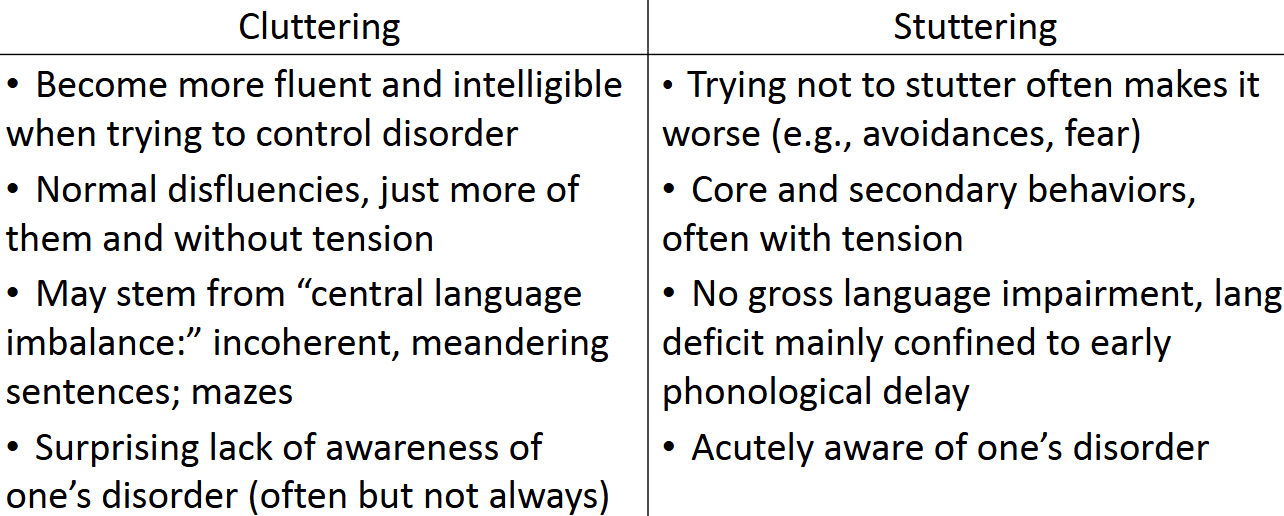
Cluttering vs. Stuttering
Stuttering is primarily a motor speech disorder with a linguistic component
Cluttering sits at the convergence of language formulation and articulatory control
PWC: disorganized, confused, and reiterative speech patterns not seen in PWS
Cluttering vs. Stuttering Table:
Cluttering Facts
Average age of diagnosis is ~8 yrs; language has become complex and lengthy
Common Disorders Co-occurring with Cluttering
Stuttering: 14-32% of PWS show cluttering symptoms
Articulation disorders: different from the cluttering symptoms of omitting phonemes or syllables due to rapid speech rate
ADHS: propensity to hurry, do things quickly
Learning disabilities: likely related to language deficits seen in the speech and writing of PWC
Autism: more research in this area recently
Voice Disorders
Difficultly initiating, maintaining, or controlling voice
Vocal folds don’t vibrate normally
Characteristics of Voice Disorder
Pitch (Frequency): too high, too low
Loudness (Amplitude): too loud, too soft
Voice Quality (Timbre, Complexity): hoarse, breathy, strained
Resonance (how vocal tract modifies sound): hyper/hyponasal, throaty
Classification of Voice Disorders
Functional
Organic
Neurological
Functional Classification
No changes in laryngeal structure
Can be stress or anxiety related (or psychogenic)
Habitual or maladaptive behavior: using your voice wrong
Organic Classification
Structural cause
Laryngeal web, tumors, swelling, etc.
Neurological Classification
Neurological cause
E.g., vocal fold paralysis resulting from conditions affecting the nervous system
Vocal Pathologies
I. Trauma
Behavioral
Mechanical
Chemical/Thermal
Mechanical Trauma from Intubation
Result = Granuloma/Contact Ulcers
Examples of Behavioral Trauma
Speaking during menstrual cycle
Aspirin (drugs)
Intense personality
Vocal Pathologies
II. Unknown Causes
Ventricular Dysphonia: false vocal folds interfere during phonation
Stress/anxiety: can cause Muscle Tension Dysphonia (abnormal muscle activity with unknown cause)
Excessive use/misuse of voice, GERD, learned behaviors after upper respiratory illness
Puberphonia (mutational falsetto)
Vocal Pathologies
III. Masses on the vocal folds
Any mass or lesion along the vocal fold edge can cause glottic closure and cause voice abnormalities
Tumors, polyps, nodules, papilloma, ulcers
Diagnosed by medical team
Will impair voice variably according to location, size, and firmness
Increased bulk
Altered vf shape and tension
Limited vf mobility
Not enough approximation
Compensatory excessive tightness of approximation
Vocal Fold Nodules
Excessive voice use causes swelling, which may result in tissue changes if voice is not rested
Small, callous, sessile, bilateral protuberances on the inner surface of the vocal folds
Can be acute or chronic
Polyps
Benign growth
Acute, focal misuse
Soft, fluid filled sacs
Usually one-sided
May be sessile (closely-attached) or pedunculated (attached by a stalk)
Interfered with VF contact during vibration resulting in breathy voice quality
Differentiate Nodules from Polyps
Location:
P & N: midpoint or anterior
Uni/Bilateral:
P: usually unilateral ; N: usually bilateral
Definition
P: soft blister ; N: callous
Causes
P: acute focal misuse ; N: chronic abuse
Symptoms
P & N: pretty similar
What are Contact Ulcer Granuloma
Inflamed lesions, usually in posterior regions
Sores on mucous membrane of arytenoid(s)
Can be painful
Contact Ulcer Granuloma Causes
Usually GERD
Forceful closure of cartilaginous portion of vocal folds
Intubation trauma
Papilloma
Benign, viral neoplasm/tumor
Stippled mass, like a wart
Caused by exposure to HPV
Juvenile or adult papilloma
May occur in the pharynx, trachea and larynx
Benign, but may be precancerous
Carcinoma
Malignant tumor
Life-threatening
Smoking is a major cause of laryngeal cancer
Risk increases substantially when alcohol is combined with smoking
Voice changes may be an early detection of disease
Edema
Reinke’s edema: swelling (fluid fills the superficial layer of the lamina propria
Translucent, sac-like
Smoking, reflux, chronic vocal abuse
Laryngeal Web
Membrane
Congenital or scar tissue from trauma
Consequences:
Stridor
Hoarseness
Aphonia
Cysts
Glandular duct blockage (glob of fat or fluid-filled growth), contained within membrane
Vocal Pathologies
IV. Neurogenic Voice Disorders
Disruption in structure or function at CNS or PNS level
Dysfunction of Vagus Nerve (Cranial Nerve X)
Neurological Diseases
Parkinson’s disease
ALS
MS
Spasmodic Dysphonia
Disorder affecting motor control of the larynx
Hallmark symptom: Intermittent voice stoppage
Strained voice, pitch breaks, worsens with stress
Thought to be psychogenic at one point: now considered a form of focal dystonia
Involuntary muscular contractions and abnormal postures
Adductor, Abductor, Mixed
Vocal Fold Paralysis
Unilateral, bilateral, adduction, abduction
Bilateral abductor vocal fold paralysis if life threatening and requires prompt management
Normal phonation but may progress to complete respiratory obstruction
Caused by thyroidectomy, neurological disorder (PD, CVA, MS), congenital, etc.
Medialization Thyroplasty
Place implant through thyroid behind vocal fold, fat injections can also be used
Laryngectomy
May only need chemotherapy if caught early on or simpler surgery
Cordectomy
Hemi laryngectomy
Larynx may need to be removed completely if not caught early
Speech After Laryngectomy
Mechanical
Artificial larynx
Surgical
TEP (Tracheo-Esophageal Puncture)
Most frequently used method of alaryngeal speech
Other
Esophageal Speech: air is injected into upper esophagus and released in a controlled manner to create sound source for speech
TEP
Tracheoesophageal puncture
One way valve allowing exhaled air to pass into pharynx. This airstream vibrates the mucosa of the upper PE segment
Similar physiologic principles of normal speech
Efficient air flow source
Natural phrasing and varied voice efforts
When the air source subsides, the valve closes and prevents aspiration of secretions