PHAR 100 - Module 1
1/93
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
94 Terms
drugs
any substance received by a biological system that is not for nutritional purposes
pharmacology
science of drugs including their uses, effects, and modes of action
Influence of poison: Curare
Used as poison: indigenous people of the amazon used to dip their bows in it because it caused paralysis and death
Used as a drug: used by anesthesiologists to relax a muscle during surgery
influence of poison: ergot
Poison: poison fungus that grows in bread and killed a bunch of people in the medieval times
drug: used to prevent migraines because it constricts blood flow
Drugs acting on the brain: Reserpine and Chlorpromazine
discovery: the extracts of a rauwolfia plant were used by Indian medicine to reduce anxiety and blood pressure
therapeutic uses: chlorpromazine is preferred to be used for mental patients that reserpine because its easier to dose it correctly. Converts anxious tense people into calm people
Drugs acting on the brain: Lysergic and diethylamide (LSD)
discovery: a Swiss pharmaceutical was trying to make products from ergot
contribution to pharmacology: the discovery of the psychedelic effects of LSD supported the idea that some mental illnesses might be due to chemicals in the brain
Drugs acting on the brain: Anesthetics
Nitrous Oxide (laughing gas): a chemist was giving demonstrations in the 1840s, and this one man was on the gas and gashed his leg but felt no pain. a dentist in the crowd started using it for patients
Ether: similar properties to laughing gas
1. drug discovery
- identify a target (receptor)
- once a compound is found that binds well to a receptor, its effects on the molecular, cellular, and animal level are tested
- if it shows promise, it'll go on to the pre-clinical trial
2. Pre-clinical studies
- IS IT SAFE AND EFFECTIVE?
- this testing happens before any testing on humans
-Toxicology studies and Pharmacological studies
Toxicology studies
- a pre-clinical study
- determines if the drug has any adverse effects on other organs
- all drugs are toxic at some level
-expensive and can take up to 6 years
Pharmacological studies
- a pre-clinical study
- determines the detailed mechanisms of the new drug
3. Clinical trial: Initial Steps
to test on humans, the following is requires:
- show proof that it was safe from testing on animals
- methodology of the proposed clinical trial is required
- your drug needs to be evaluated by other scientists
4. Phase 1 Clinical Trial
-conducted on healthy people
- carefully evaluates the effect of the drug
- tests dosages and tolerability
-doesn't assess the efficacy
5. Phase 2 Clinical Trial
- conducted on the people with the disease the drug aims to fix
- tests if the drug is effective on treating that disease
- paying careful attention to the safety of the drug
6. Phase 3 Clinical Trial
- test the drug on a large # of people
- longest clinical trial stage
- done in multiple cities to keep it diverse
- most expensive part off drug trials
-determines safety and effectiveness
Target Population (Phase 3 Clinical Trial)
- a group who the drug is meant for
Study populations (Phase 3 Clinical Trial)
- randomized allocation makes sure there is an equal chance of being in the control or treatment group (ensures diversity)
Treatment group (Phase 3 Clinical Trial)
will get the new drug on trial
Control group (Phase 3 Clinical Trial)
will get the placebo drug or the gold standard drug
Inclusion/Exclusions Criteria (Phase 3 Clinical Trial)
the criteria of people that can be included in the study
- effected: diseases, age, gender
consent (Phase 3 Clinical Trial)
the participants have to sign a document agreeing to any risks
Placebo (Phase 3 Clinical Trial)
a replica drug that doesn't actually have any active ingredient
Gold Standard (Phase 3 Clinical Trial)
the best treatment for the disease the medical community has
- its unethical to withhold treatment if its available so the gold standard drug is used if available, if not, a placebo is used
Blinded assessment (Phase 3 Clinical Trial)
neither the investigator nor the patient knows the groupings (double blind). stops any bias or expectations
outcome (Phase 3 Clinical Trial)
the results should be reliable and consistant
Compliance (Phase 3 Clinical Trial)
-how the patient took the drug
- any unused pills are returned and counted
Quality of life (Phase 3 Clinical Trial)
-hoping the drug will improve quality of life
Result analysis (Phase 3 Clinical Trial)
the experimental drug must be compared to the control group using stats.
7. Health Canada Review
- the results of the trial are reviewed
- if the drug is deemed effective and the toxicity is acceptable, it gets approved
8. Manufactoring
Generic Vs. Name Brand
- name brand is when there is a patent on the drug (patents starts in the pre-clinical trials and lasts 20 years, 8-10 of those are used during the trials)
Bioavailability Studies
- compares the blood levels after taking the name brand and the generic brand. They should be bioequivalent
- there are strict rules so drugs made are bioequivalent and that the generic brand is as effective as the name brand drug
Bioequivalent
2 drug products, generic and name brand, which have the same active ingredient and give similar blood levels
9. Phase 4 Post-approval Trials
- keeping surveillance on the drug to make sure there isn't any risks developing
Advertising Techniques
1. Before and after- show a sick person using the drug to get healthy
2. fear- putting fear into someone and then giving them a drug to fix it
3. offering an easy solution - showing how easy it is to fix a disease
4. catch the audiences attention- eye catching ads
5. using trusted authorities- like celebrities and doctors endorsing it
6. discredit other drug manufacturers and praise your own
Drug Targets- Receptors
Receptor is a protein molecule on the surface of a cell that regulates the organism
- receptors in the body are bound to and activated by endogenous ligands ( like hormones and neurotransmitters)
- location of the receptor determines where the drug acts and if its beneficial or detrimental
Drugs and Receptors
-drugs mimic or block the effect of endogenous ligands at the receptor
- antagonist (stops response)
-agonist (stimulates response)
- like a lock and key
Antagonist
drug that bonds to the the receptor and stops the response
(key fits but cant open lock)
Agonist
drug that binds to the receptor and stimulates a response
(key fits and opens lock)
dose-dose relationship
- the intensity of the effect of the drug increases with higher doses
- a threshold exists (a certain # of receptors need to be activated to see a response, once threshold is reached, small dose increases cause big increases in response)
- our bodies have a maximal effect where increasing the drug will have no further effect
dose response curve
- the y axis: the effect of the drug (0-100%)
- the x axis: the dose of the drug plotted using log scale
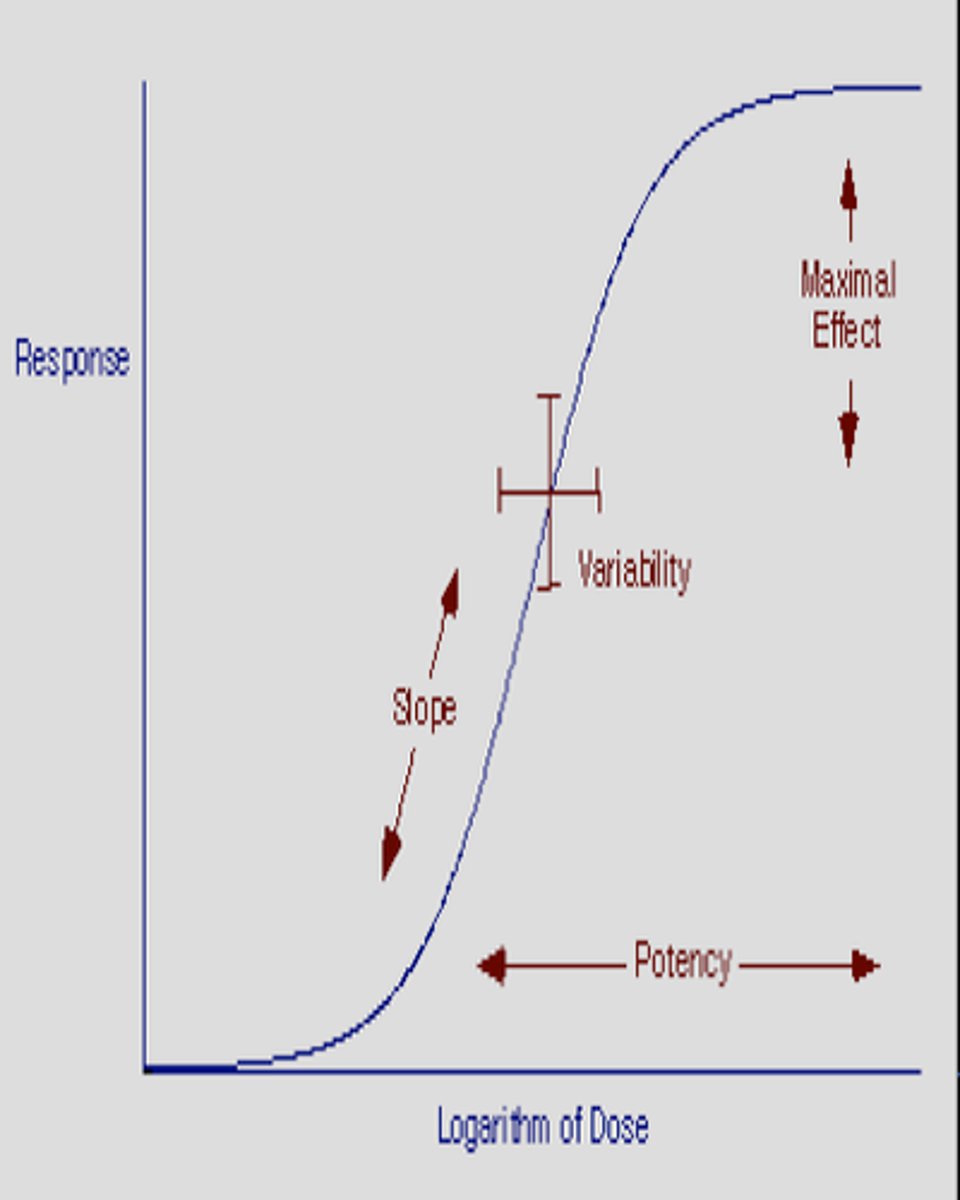
Dose response curve: threshold of effect
- administering the drug and nothing happens
- you need a certain amount of drug to get enough receptors to make a response
Dose response curve: when you reach the threshold
- after reaching the threshold, when you increases the dosage, the response increase is linear
- small dose increase = large response change
Dose response curve: Reach max effect fo the drug
- the response plateaus
- the Maximum response is reached, and no more response will happen
Dose response curve: ED 50
- you can use the graph to see what dose will give you 50% of your response
- its the dose of drug thats effective in 50% of people
efficacy
the maximum pharmacological response that can be produced by a drug in that biological system
- the amount needed of the drug doesn't matter
- what matters is the max effect that the drug can make
- more important that potency because it helps decide what drugs to use for certain levels of pain
potency
the dose of a drug required to produce a certain magnitude response (usually 50% response)
- ex. If drug A is more potent than drug B. less dosage is required to reach the same response
- its easy to adjust the dosage (potency), whats important is if you're getting the pain relief you need (efficacy)
- the more potent the drug is, the less dosage you need (good because then you'll have less adverse effects)
on an efficacy, potency, and dose response curve
- the taller the curve goes, the efficacy is it
- the closest the curve is the the left side of the graph, the more potent it is
therapeutic range
the zone between when the drug has no effect, and when its getting to toxic concentrations
Pharmokinectics
the movement of the drug into, through, and out the body
ADME
(administration), absorption, distribution, metabolism, excretion
-the 4 major processes that determine the drug concentrations in the blood
Administration
routes of administration:
1. Topical administration (skin+lungs)
2. Enteral Administration (gastrointestinal)
3. parenteral administration (bloodstream)
1. topical administration
- on the skin
- through the skin
-inhalation
1. topical administration: on the skin
- treats mild to severe skin conditions (acne, eczema)
onset of action: rapid to slow (depends on organ)
bioavailability: 5-10%
1. topical administration: through the skin
- transdermal drug delivery (drug on skin absorbs into general circulation in the body. delivers drug supply for days and bypasses the enzymes of the stomach, intestine, and liver)
disadvantages: expensive and can cause irritation at the administration site
onset of action: rapid to slow (depends on organ)
bioavailability: 5-10%
1. topical administration: Inhalation
- inhaled drugs through the lungs
-gaseous anaesthetics are inhaled through the lungs for a whole body effect
- drugs for lung disease can be inhaled
advantages: for local effect, dosage is small (avoids toxicity)
disadvantages: requires proper use by patient
onset of action: rapid to slow (depends on organ)
bioavailability: 5-10%
2. enteral administration: mouth
- very common (90% of drugs taken this way)
advantages: convient and cheap. non-invasive and patient can administer it themselves
disadvantages: variability in absorption due to differences in patients
first pass effect: passes through the liver before getting to the blood. there are enzymes in the liver that decrease the amount of active drug
onset of action: slow (0.5-1 hour)
bioavailability: 5-10%
2. enteral administration: rectum
- can be systematic or for local effects
-used for patients who are vomiting or for people in a coma
-digestive stomach enzymes are bypassed
disadvantages: not all drugs are available as suppositories. Absorption is slow, incomplete, and caries
onset of action: slow and incomplete
bioavailability: 30-100%
2. enteral administration: sublingual and buccal
sublingual- under tongue
buccal- in cheek
advantages: stomach, and liver enzymes are bypasses
disadvantages: can be swallowed, and then the drug would act as if it was taken orally
under tongue:
onset of action: rapid (1-2 mins)
bioavailability: 30-100%
in cheek:
onset of action: intermediate (3-4 mins)
bioavailability: 30-100%
3. parenteral administration: intravenous
- drug goes directly into the blood
advantages: can be used for drugs that don't get absorbed well (as long as it is able to be made into a water solution)
disadvantages: response is immediate, intense, and irreversible (risky), it costs a lot of money, and it has to be made in a sterile place
onset of action: 15-30 seconds
bioavailability: 100%
3. parenteral administration: intramuscular
- drug injected deep in a muscle
- volume is limited to 5-10mL in an adult
onset of action: 10-20 minutes
bioavailability: 75-100%
3. parenteral administration: subcutaneous
-drug is injected into the deepest layer of the skin
- drug modification can be modified to control the timing of the release of the drug
onset of action: 15-30 minutes
bioavailability: 75-100%
Bioavailability
- the fraction of an administered dose that reaches systematic circulation (blood) in active form
- intravenous is 100% bioavailable because its straight into the blood
ADME: Absorption
- the movement of the drug from the administrative site into the blood
- for a drug to be absorbed, it has to be able to cross biological membranes
ways for drugs to pass through membrane: diffusion through aqueous pores
- water soluble, small molecules
- pass through membrane by dissolving in the aqueous fluid surrounding the cell, and passing though small openings
- diffuses from high to low concentration (passive)
ways for drugs to pass through membrane: diffusion through lipid
- MOST IMPORTANT
- biological membranes are made up of a lipid bilayer and proteins
-pass through membranes by dissolving in the lipid part of the membrane
- diffuses from high to low (passive)
ways for drugs to pass through membrane: active (carrier mediated) transport
-drugs bond to carrier proteins, drug gets moved across membrane
- can be passive or active transport
ADME: Distribution
- the movement of the drug from the blood to the other tissues and the site of activation
(most drugs reach all the tissues and organs anyways)
-the concentration of the drug as the site of distrubution are in equilibrium with its concentration in the blood
- if the concentration in the blood drops, the drug will diffuse from the distribution site to the blood to keep equilibrium
- the rate at which drugs distribute depends on the blood flow to that organ (more blood flow, the quicker the drugs get there)
ADME: Metabolism
BIOTRANSFORMATION
- conversion of a drug into a different chemical compound to be eliminated (bioavailability)
- drugs have to be water soluble to leave the body through the kidney
-most biotransformation occurs in the liver, but some also happens in the intestines, lungs, skin, etc.
Metabolism: metabolites
- metabolites are the product of metabolism
biotransformation reactions
phase 1: add or unmask a functional group on the drug so that phase 2 reactions can add a large, water-soluble molecule (like adding a handle)
- makes drug water-soluble for kidney
phase 2: add a large water soluble molecule to the product of phase 1
- males it able to be excreted by the kidney
metabolism: p450
- a family of enzymes that breaks down most clinical drugs
- found in most tissue, but in high concentration in the liver
MOST BIOTRANSFORMATION HAPPENS IN THE LIVER
- if you take more than 1 drug, the p450 enzymes might not be able to break down the drug, and therefore the drug wouldn't leave the body and there would be increased toxicity in the body
ADME: Excretion
-moving the drug and metabolites out of the body
Excretion: Kidney
- eliminates majority of the drugs
- if the drugs are water soluble enough, they'll be peed out
-lipid soluble drugs can be reabsorbed form the kidney back into the blood
Excretion: GI tract
- excreted by the GI tract after biotransformation in the liver
Excretion: Lungs
- gaseous can be exerted by lungs (ex. alcohol and anesthetics)
Excretion: Breast milk
- its a minor route of elimination, but the baby can get a therapeutic or toxic level of drugs from the breast milk
Excretion: Saliva and Sweat
- drugs of abuse can be found in the sweat of a user
Variation in drug response
- different people respond to different doses of drugs due to:
- an influence at any stage of ADME
- genetic factors
- environmental factors
-disease
-altered physiological states
-presence of other drugs
Variation in drug response: genetic factors
- genetic variability exists in the receptors and how the body handles drugs
Variation in drug response: environmental
- certain exposure to chemicals cab increase biotransformation enzymes in the liver (and the drugs would be eliminated more quickly)
Variation in drug response: Disease
disease will alter how your body handles drugs (ex. liver will metabolize drugs slower)
Variation in drug response: altered physiological states
age of patient: drugs have a stronger effect on old people because they have reduced liver and kidney function so the elimination of drugs is slowed down
pregnancy: 2 patients are receiving the drugs
Variation in drug response: other drugs present
- if multiple drugs are taken, the one drug can change the effect of the other
adverse effects
effect produced by drugs that was not the intended effect
Examples of adverse effects: Extension of therapeutic effects
- too much drug is in the blood
Examples of adverse effects: Unrelated to main drug action
- effects that are unexpected/unrelated to the intended action of the drugs (like a side effect)
Examples of adverse effects: Allergic reactions
- mediated by the immune system
- antigen-antibody combo starts an adverse effect that can be mild or severe
Examples of adverse effects: drug depended and addiction
- unwanted physiological and psychological effects of the drug
Examples of adverse effects: Teragenisis
- drugs cause defects in a developing fetus
Examples of adverse effects: adverse biotransformation reactions
- drug is converted to a chemically relative metabolite that can bond to tissue and cause damage
predicting adverse drug reactions
- a drugs can appear to have little/np adverse effects until later
because:
- the toxic reaction may be rare
- the reaction may only occur after long use
- the effect is not detectable in animals
- toxic effect maybe be unique to the Tim period (ex. pregnant woman)
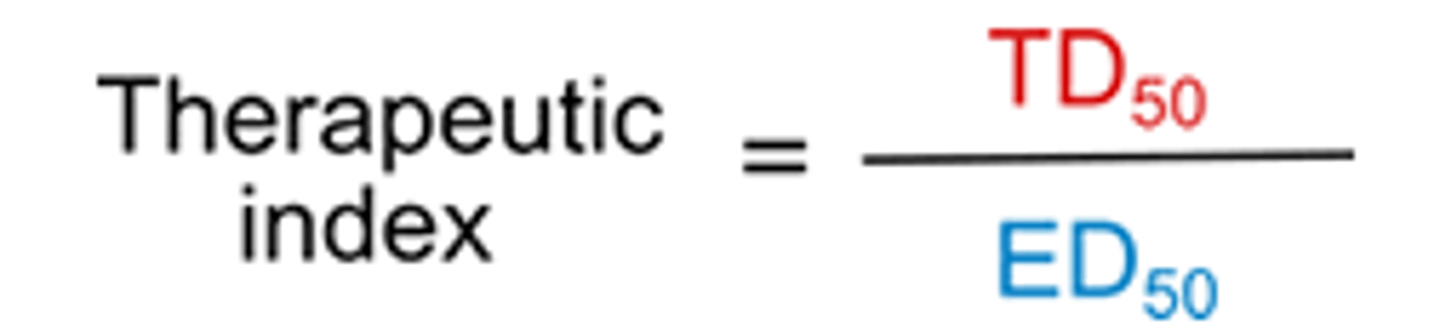
Assessing Drug Toxicity
measured using therapeutic index
therapeutic index
-tells you how safe a drug is
- high T=safer, low T=more toxic
TD50: the dose of drug thats toxic to 50% of the population
ED50: dose of the drug that is effective to 50% of the poulation
Drug-drug interactions
- when 1 drug changes the effect of another drug in the body
absorption: a drug can increase intestinal movement, causing another dug to be pushed through the intestine quicker (no time to absorb)
metabolism: a drug can block the inactivation of a second drug in the liver, causing increasing blood level and effects of the second drug
excretion: a drug can make it easier to excrete the second drug, decreasing blood level and the effects of the second drug
Drug-Food Interactions
Tyramines:
-found in ages cheese and is broken down by enzymes in the liver call MAO
- can raise blood pressure
- there is a type of antidepressants that inhibit MAO and if they eat tyramines while on this drug, it won't break down the blood raising effects
grapefruit:
- alters the absorption of some drugs because the grapefruit inhibits the enzymes that break down drugs in the GI
- more active ingredient in the blood can lead to overdose of more effects