Neuro 10, 23- Neuro Pharmacy (Alzheimer's, Neuropathy, Migraines, Parkinson's, Tremors, Seizure Pharmacy)
1/58
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
59 Terms
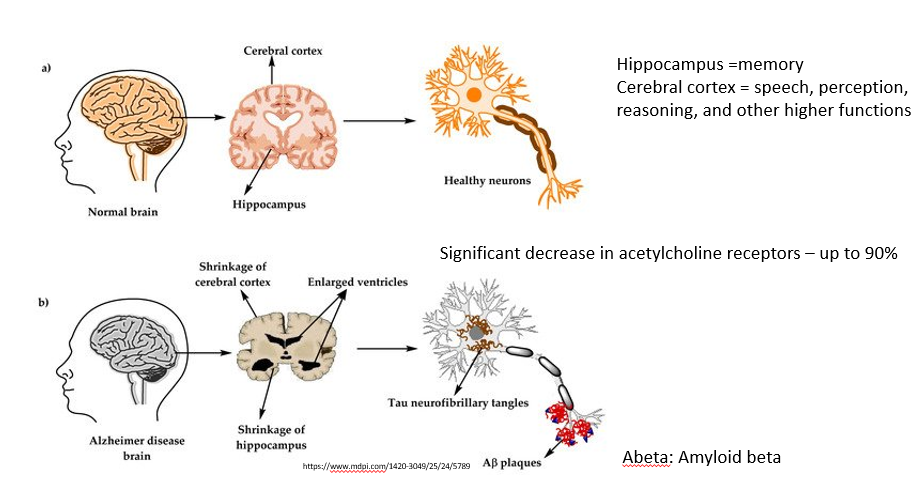
Describe the changes in the brain parenchyma, neurotransmitters, and neurons in Alzheimer’s disease.
Shrinkage of cerebral cortex and hippocampus (which are important for higher functions such as speech, perception, reasoning; and memory, respectively)
and
significant decrease in Ach receptors (up to 90%)
and
tau protein tangles and amyloid beta plaques on neurons (see image)
State the drug class and MOA of the following drugs:
(Aricept, Exelon, Razadyne are the brand names)
Cholinesterase inhibitors - prevent breakdown of acetylcholine and enhance transmission by cholinergic neurons
What should you consider in a patient who is taking Donepezil for mild dementia and tiotropium for COPD?
Donepezil is a cholinesterase inhibitor, which increases the amount of acetylcholine, while tiotropium is an anticholinergic which decreases the effect of acetylcholine - so combining them is not recommended as they have opposite effects
don’t combine anticholinergics with cholinesterase inhibitors (donepezil, rivastigmine, galantamine)
NMDA receptor antagonists, such as memantine (Namenda) can be used to treat moderate to severe symptoms of…
Alzheimer’s disease
Namenda/Memantine is an NMDA receptor antagonist that helps prevent overstimulation of the NMDA receptor. It is indicated for what disease…
moderate to severe symptoms of Alzheimer’s disease
Aducanumab and Lecanemab are two examples of DMT for what disease…
Alzheimer’s (technically mild cognitive improvement or mild dementia)
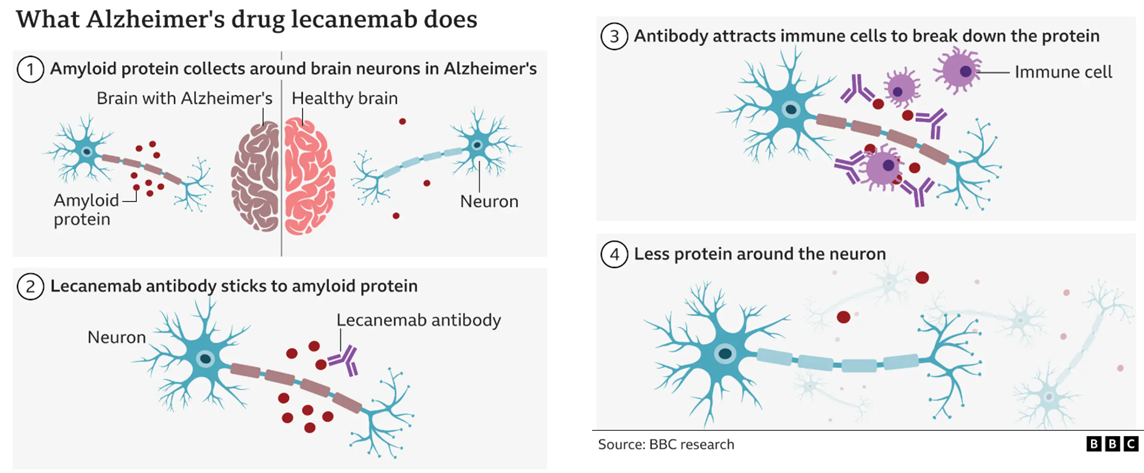
Death from amyloid related imaging abnormalities (ARIA) - E (edema) or H (hemorrhage) is a risk of amyloid beta-directed antibodies.
What genotypes are at a higher risk of this AE?
How do you monitor for this condition?
ApoE genotypes are at a higher risk; must test genotypes prior to therapy.
MRI testing is needed throughout this therapy to test for ARIA
What are the two first line agents for neuropathic pain?
antiepileptics (such as pregabalin or gabapentin) and antidepressants (SNRIs and TCAs; duloxetine, venlafaxine, amitriptyline)
What are the two second line agents for neuropathic pain?
lidocaine patch and capsaicin
true or false - opioids are effective for neuropathic pain
false
how long would you expect a medicine for neuropathic pain to take effect?
it may take 8-12 weeks; if no response, try combo therapy
True or False - butalbital compounds such as fioricet and fiorinal can be prescribed as first-line therapy for mild to moderate migraines.
False; they aren’t recommended as first line.
They can lead to tolerance/dependence and overuse headache
Why might you use metoclopramide (Reglan) or Prochlorperazine (Compazine) in someone with a migraine?
these antiemetics treat the nausea associated with migraine
T or F - Antiemetics metoclopramide and Prochlorperazine can cause akathisia
true
A 34-year-old patient presents with a history of episodic migraines and is prescribed almotriptan for acute migraine relief. Which of the following best describes the mechanism of action of almotriptan?
A) Inhibition of serotonin (5-HT) receptors, leading to vasoconstriction and inhibition of neuropeptide release from trigeminal nerves.
B) Inhibition of prostaglandin synthesis, reducing inflammation and pain in the head and neck.
C) Blocking of dopamine receptors in the chemoreceptor trigger zone, reducing nausea associated with migraines.
D) Inhibition of calcitonin gene-related peptide (CGRP) receptors, preventing neurogenic inflammation.
E) Stimulation of GABA receptors, enhancing inhibitory neurotransmission and decreasing neuronal excitability.
A) Correct: Almotriptan is a 5-HT1B/1D receptor agonist (a type of triptan) that works by stimulating serotonin receptors. This results in vasoconstriction of cranial blood vessels and inhibition of neuropeptide release from trigeminal nerves, which helps relieve migraine symptoms.
B) Incorrect: This describes the mechanism of NSAIDs (e.g., ibuprofen, naproxen), which inhibit cyclooxygenase (COX) and reduce prostaglandin production, decreasing pain and inflammation.
C) Incorrect: This describes the mechanism of metoclopramide, which is an antiemetic that works by blocking dopamine receptors in the chemoreceptor trigger zone, helping to reduce nausea in migraine sufferers.
D) Incorrect: This describes the mechanism of erenumab and other CGRP receptor antagonists, which block calcitonin gene-related peptide (CGRP), a neuropeptide involved in migraine pathophysiology. CGRP inhibitors are a newer class of drugs for migraine prevention, not acute treatment.
E) Incorrect: This describes the mechanism of benzodiazepines (e.g., diazepam), which enhance GABA activity and have sedative and anticonvulsant effects, but they are not used to treat migraines directly.
a patient receives a new prescription for carbamazepine (Tegretol). What intervention should be made?
a - warn her not to withdraw this drug abruptly
b - recommend that she take this medication at bedtime with meals
c - teach her family to assist by maintaining a seizure frequency chart
d - ensure that genetic testing for HLA-B1502 is performed
d
Carbamazepine is an anticonvulsant used to treat epilepsy and trigeminal neuralgia, but it carries a risk of serious cutaneous reactions like Stevens-Johnson syndrome (SJS), especially in individuals of Asian descent.
HLA-B1502 is a genetic marker that identifies patients at higher risk for severe reactions to carbamazepine. Genetic testing for HLA-B1502 is recommended before initiating carbamazepine therapy, particularly in patients of Asian ancestry, to assess this risk.
You are taking care of a patient on valproic acid (Depakene). What is the most common adverse effects of this medication?
a - increased risk of infection
b - reddened, swollen gums
c - nausea, vomiting, and indigestion
d - central nervous system depression
Correct Answer: C) Nausea, vomiting, and indigestionExplanation:
Valproic acid is a widely used antiepileptic drug (AED) and mood stabilizer. While it can cause a range of side effects, the most common adverse effects are gastrointestinal (GI) symptoms such as:
Nausea
Vomiting
Indigestion (dyspepsia)
These GI side effects are often seen in the early stages of treatment and may be alleviated by taking the medication with food or adjusting the dosage.
Other Options:
A) Increased risk of infection:
This is not a common side effect of valproic acid. However, valproic acid can rarely cause bone marrow suppression, which can affect white blood cell count and increase susceptibility to infections, but this is not a typical or common adverse effect.B) Reddened, swollen gums:
Gingival hyperplasia (swelling and redness of the gums) is more commonly associated with phenytoin (another antiepileptic drug) than with valproic acid. It is not a major adverse effect of valproic acid.D) Central nervous system depression:
CNS depression (drowsiness, dizziness, confusion) can occur with valproic acid, especially at higher doses, but it is not the most common side effect. The GI symptoms (nausea, vomiting, indigestion) are more frequent and are often more bothersome in the early stages of treatment.
Which medication can cause a metabolic acidosis? pH 7.32 paCO2 33, HCO3 20
a primidone
b lamotrigine
c lacosamide
d topiramate
Topiramate (option D) is the medication most commonly associated with metabolic acidosis. The lab values suggest a primary metabolic acidosis, which is consistent with topiramate's potential to cause this disturbance due to its carbonic anhydrase inhibition effect.
what is the goal of pharmacologic therapy in the treatment of Parkinson’s disease?
to balance cholinergic and dopaminergic activity in the brain
A patient with Parkinson’s disease who has been positively responding to drug treatment with levodopa/carbidopa (Sinemet) suddenly develops a relapse of symptoms. What is the explanation for this reaction?
this could be the on/off or the wearing off symptoms
adjusting the dose/timing could help; Parkinson’s is one of those diseases where you can dose more frequently based on symptoms
A patient with Parkinson’s disease is prescribed pramipexole (Mirapex) along with his levodopa/carbidopa (Sinemet). Which symptom is most likely a manifestation of an adverse effect of these drugs when given together?
a - diarrhea
b - dyskinesia
c - wheezing
d - headache
Dyskinesia
What counseling should you give to a patient who is newly prescribed a triptan for their migraines?
can cause a sensation of chest tightness and pressure
may also cause mild vertigo, malaise, fatigue, tingling
AVOID IN PATIENTS WITH CAD, Hx of MI, and uncontrolled HTN
teratogenic
don’t take more than recommended dose in 24h as it can make Sx worse
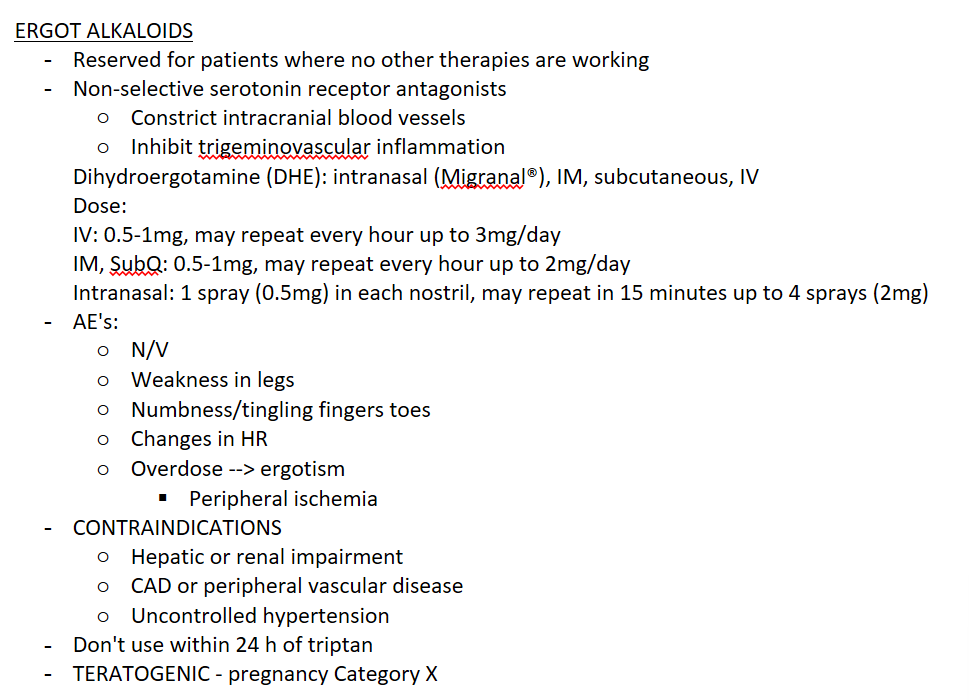
when are ergot alkaloids, such as Dihydroergotamine (DHE) indicated?
treatment for migraines when no other therapies are working
What are you worried about with ergot alkaloid overdose?
ergotism - peripheral ischemia and other neurologic symptoms
TRUE OR FALSE - DHE can be used to treat refractory migraine in a pregnant woman with hypoalbuminemia and GFR <50 mL/min, and hypertension.
FALSE; ergot alkaloids (Dihydroergotamine) are contraindicated in pregnancy, hepatic and renal impairment; also contraindicated in CAD and uncontrolled hypertension.
True or False - in order to get coverage for ubrogepant or rimegapant (CGRP Antagonists), patients often have to fail two triptans
true
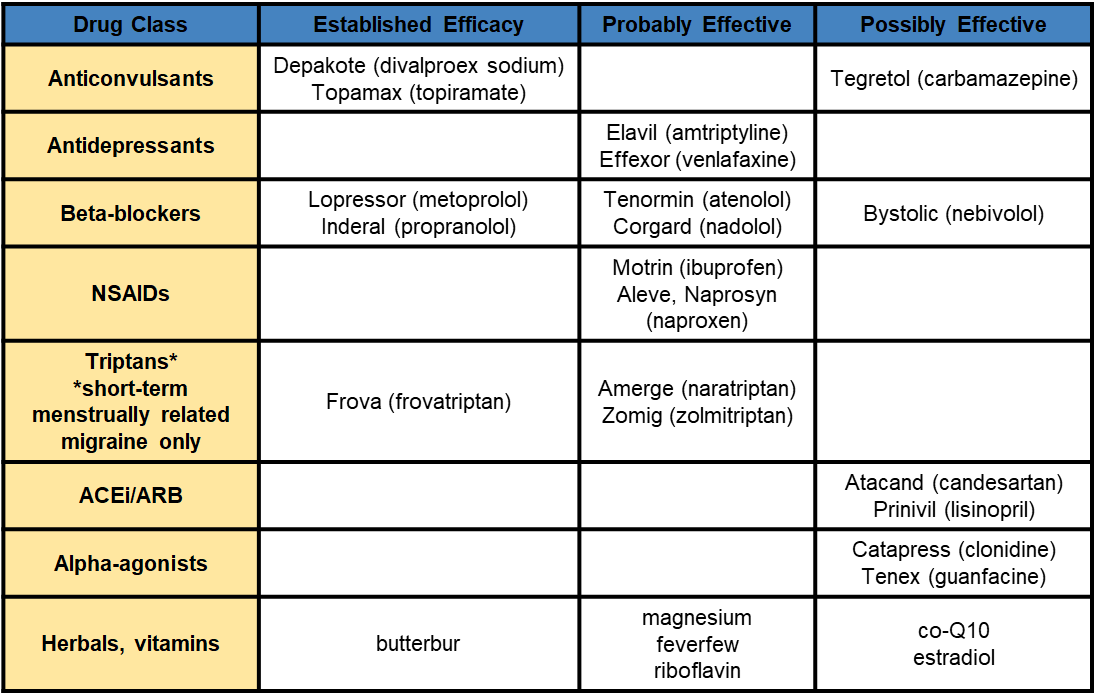
What do these drugs have in common when it comes to treating migraines: Depakote, Topamax, metoprolol, propanolol, frovatriptan, butterbur?
They all have established efficacy as migraine prophylaxis
NOTE: CGRP Antagonists, such as Ubrogepant or Rimegepant can also be used as migraine prophylaxis. they’re only dose about once a month; however, patients generally have to fail other therapies to get these
why is levodopa combined with carbidopa in treatment of Parkinson’s disease?
it helps to decrease peripheral metabolism of levodopa, so that more of it can enter the brain
Dopaminergic agents such as levodopa/carbidopa are first line for Parkinson’s disease. When are anticholinergics given? Give two examples of anticholinergics that are used for Tx of PD.
anticholinergics are used more frequently in younger patients, and for milder symptoms. They only help with tremor and rigidity.
Cogentin (Benztropine) and Artane (Trihexyphenidyl) are two anticholinergics used to treat PD
Why is the COMT inhibitor tolcapone rarely used?
it’s hepatotoxic
(other COMT inhibitors entacapone and opicapone aren’t hepatotoxic)
What is the purpose of adding on entacapone to levodopa/carbidopa? what are some suspected AEs?
similar to carbidopa, it decreases peripheral metabolism of levodopa helping more of it to enter the brain.
AEs: orthostatic hypotension, orange urine, GI symptoms
Which of the following medications are NOT adjunctive treatments to levodopa/carbidopa in the management of Parkinson's disease?
A) Amantadine
B) Pramipexole
C) Entacapone
D) Olanzapine
A) Amantadine:
Incorrect. Amantadine is an adjunctive treatment to levodopa/carbidopa, used for early-stage Parkinson’s disease and to manage levodopa-induced dyskinesias.B) Pramipexole:
Incorrect. Pramipexole is a dopamine agonist, often used as an adjunct to levodopa to help manage motor fluctuations and early-stage Parkinson's disease.C) Entacapone:
Incorrect. Entacapone is a COMT inhibitor used as an adjunct to levodopa/carbidopa to prolong the effect of levodopa and manage motor fluctuations.D) Selegiline:
Correct. Olanzapine is an atypical antipsychotic and is not typically used as an adjunct to levodopa in Parkinson's disease. While it can be used to treat psychosis, it has significant dopamine-blocking effects that can worsen motor symptoms- an especially undesirable AE in Parkinson’s disease patients.
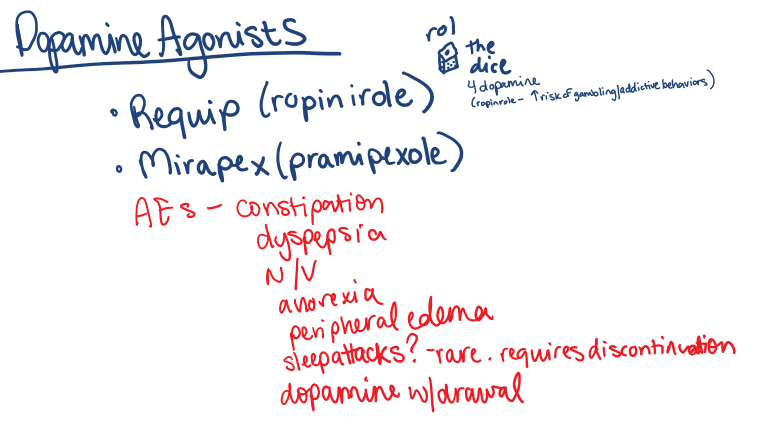
A patient is being treated for Parkinson’s disease and reports that they recently got into gambling, and have spent half of their life savings at the casino. They are taking a drug which increases dopamine and puts them at risk of developing addictive behaviors. Which of the following drugs is likely responsible for this sudden change of behavior?
a - Selegiline
b - Levodopa/Carbidopa
c - Ropinirole
d - Istradefylline
c - Ropinirole
“Rol the dice” for dopamine
Which two of the following drugs can help to reduce off time and reduce wearing off of Parkinson's disease treatments?
A) Pramipexole
B) Safinamide
C) Entacapone
D) Ropinirole
B) Safinamide and C) Entacapone
This setup offers a mix of treatments, with Safinamide and Entacapone being the correct answers for reducing off time and wearing off in Parkinson’s disease management.
A) Pramipexole:
Incorrect. Pramipexole is a dopamine agonist used to help manage Parkinson’s disease symptoms, but it is not specifically used to reduce off time or wearing off effects related to levodopa therapy.
B) Safinamide:
Correct. Safinamide is an MAO-B inhibitor that can help to reduce off time and wearing off effects when added to levodopa therapy. It works by both inhibiting dopamine reuptake and modulating glutamate activity, helping to extend the effect of levodopa.
C) Entacapone:
Correct. Entacapone is a COMT inhibitor that works by prolonging the action of levodopa, helping to reduce off time and wearing off effects. It is often added to levodopa therapy to enhance its efficacy.
D) Ropinirole:
Incorrect. Ropinirole is a dopamine agonist that is used in the management of Parkinson’s disease, but it does not specifically address off time or wearing off. It is used in early or advanced stages, often as an adjunct, but does not target the wearing off effect of levodopa.
Why must apomorphine be administered by a specialty pharmacy?
it has a high risk of profound emesis; to counteract this, trimethobenzamide must be administered 3 days prior to initiating drug- and it must be continued for at least the first two months of therapy.
It can also cause orthostatic hypotension and must be monitored at 20, 40, 60 min after dosing.
note: avoid 5-HT3 receptor antagonists as they also increase the risk of hypotension
Which two antipsychotics do you prefer to treat psychosis in patients with PD?
a - Clozapine
b - Quetiapine
c - Olanzapine
d - Haloperidol
e - Pimavanserin (Nuplazid)
b - Quetiapine (Seroquel) and e - Pimavanserin
Pimavanserin (brand name Nuplazid) is an atypical antipsychotic specifically approved for the treatment of Parkinson's disease psychosis (PDP). Unlike other antipsychotics, it does not block dopamine receptors and therefore has a low risk of worsening motor symptoms in Parkinson's disease.
clozapine can be used but has some bad AEs like agranulocytosis; onlanzapine and haloperidol can worsen motor symptoms (lead to extrapyramidal symptoms)
Your PD patient is concerned about cognitive decline and wants to try Rivastigmine. What should you counsel them on?
it may help, but it also could worsen their tremor
True or False - Modafinil can be used to treat fatigue in PD, as well as sleep problems.
True; for sleep, it helps to improve patient’s wakefulness during the day, which can improve their sleep-wake cycle
T or F - Ritalin can be used to treat fatigue in PD
true
Which two medicine classes work best for tremors?
beta blockers and anticonvulsants (i.e. propanolol and primidone)
Which of the following drugs is NOT typically used to improve tics?
a) Haloperidol
b) Risperidone
c) Clonidine
d) Sertraline
e) Botox
f) Guanfacine
Correct answer: d) Sertraline
Explanation: Sertraline, an SSRI, is not typically used to treat tics, while haloperidol, risperidone, clonidine, guanfacine, and botox are more commonly used in tic management.
why should you avoid using phenytoin/fosphenytoin in the elderly/adolescents?
risk of osteomalacia/osteoporosis due to abnormal vit D metabolism
why are you concerned about a patient who is both on phenytoin and warfarin at the same time?
these drugs are protein bound, and it’s not clear which will out-compete the other for binding…
which of the following anti-seizure meds do you need to check CBC monthly for the first year (due to a risk of agranulocytosis or leukopenia)?
A) Phenytoin
B) Gabapentin
C) Carbamazepine
D) Levetiracetam
E) Valproate
C - carbamazepine
phenobarbital is a (drug class?), therefore we are concerned about abuse and drowsiness.
barbiturate
TRUE OR FALSE - Levetiracetam and Valproate are both considered broad spectrum anti-convulsants.
true; valproic acid can be used for all types, and levetiracetam can be used for focal seizures, generalized tonic-clonic seizures, and myoclonic seizures, (as well as refractory absence seizures)
What AEs are you concerned about when dosing either lamotrigine, zonisamide, or carbamazepine (not together just in general)- that will lead you to titrate the dose up slowly?
rash - SJS/TENS
Why do you want to titrate Lacosamide slowly?
to avoid dizziness
Lacosamide can make ur head spin like loco
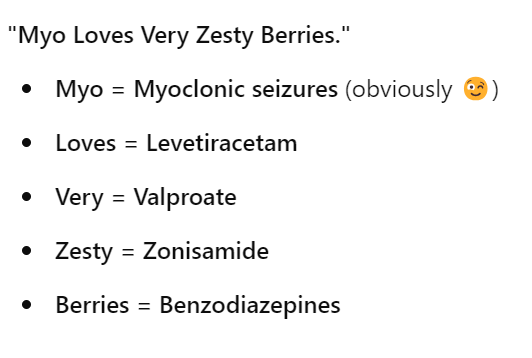
What four drugs can be used to treat Myoclonic seizures?
levetiracetam, valproate, zonisamide, benzos
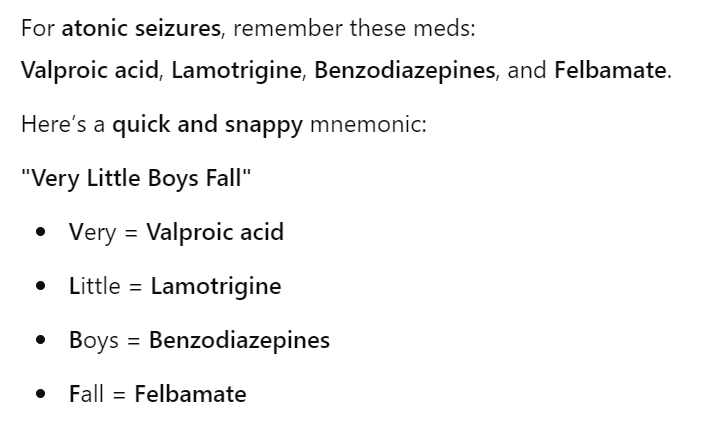
what drugs can be used for atonic seizures?
very little boys fall
“Valproic acid, Lamotrigine, Benzodiazepines, Felbamate”
which drugs can be used for absence seizures?
Very = valproate
Careless = clonazepam (NOT CARBAMAZEPINE- which is used for focal or tonic-clonic seizures)
Little = Lamotrigine
Egos = Ethosuximde
Totally = Topiramate
Zone Out = what someone with an absence seizure does NOT ZONISAMIDE
Phenytoin, and what other common anti-seizure med, are protein bound?
Valproate
what class of drugs are lorazepam, midazolam, and diazepam- and WHY do you usually reserve them for acute management of actively seizing patients?
benzodiazepines - because of risk of tachyphylaxis
(effectiveness decreases with prolonged use)
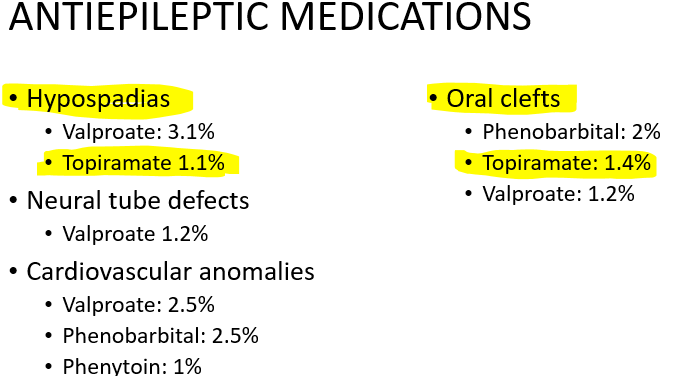
Which anti-seizure meds should you avoid during pregnancy (and prior to conception) due to risk of birth defects?
valproic acid, phenytoin, phenobarbital, and topiramate
What is our treatment goal in Traumatic Brain Injuries?
manage CPP by decreasing ICP (increased ICP leads to decreased cerebral perfusion) AND avoid hypotension
how we do this:
vasopressor/NS to avoid hypotension (which will lead to less cerebral perfusion/less mean arterial pressure)
decrease ICP : hypertonic fluids, mannitol, decompressive craniectomy
Decrease cerebral oxygen demand - sedation and analgesia
What three things do we want to manage in order to prevent the CPP from becoming dangerously low? (<50 mmHg can lead to ischemia)
vasopressor/NS to avoid hypotension (which will lead to less cerebral perfusion/less mean arterial pressure)
decrease ICP : hypertonic fluids, mannitol, decompressive craniectomy
HOWEVER, don’t give mannitol to a hypotensive patient, or to a patient with kidney disease
Decrease cerebral oxygen demand - sedation and analgesia
Which IV fibrinolytic would you use to treat an acute ischemic stroke?
A) Warfarin (Anticoagulant)
B) Alteplase
C) Tenecteplase
D) Clopidogrel (Antiplatelet)
C - Tenecteplase
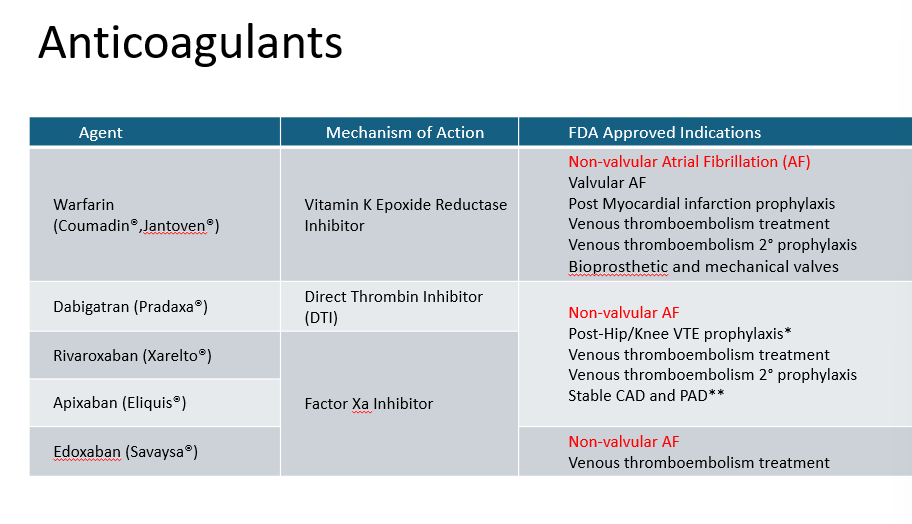
what type of drug do you want to use in a patient with A-fib to prevent stroke?
anticoagulant (can use warfarin or DOAC)
Delirium isn’t generally treated pharmacologically, unless a patient is severely agitated and may harm themselves- in which case, you can prescribe what drugs?
antipsychotics such as haloperidol, quetiapine, olanzapine