lecture 3-Pathophysiology
1/34
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
35 Terms
Physiology
The biological discipline that describes processes or mechanisms operating within an organism.
Pathology
The medical discipline that describes conditions typically observed during a disease or damaged state. Describes the abnormal or undesired condition.
Pathophysiology
Is a convergence of pathology with physiology. Seeks to explain the functional changes that are occurring within an individual due to a disease or pathologic state. (>can be described as a disruption to homeostasis)
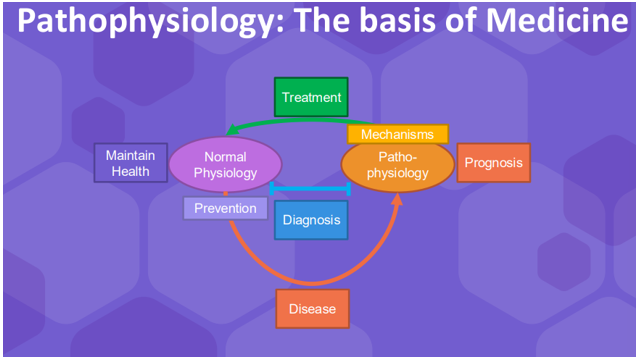
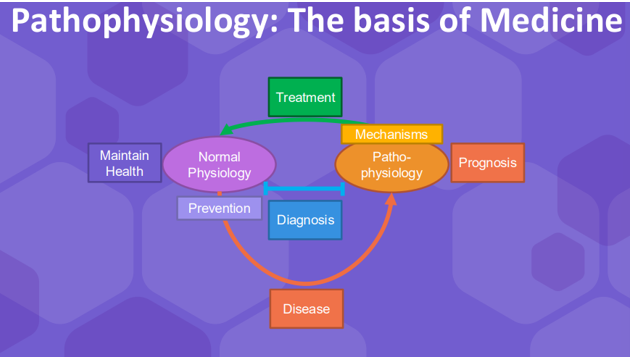
Describe the diagram
The diagram shows how we go from normal physiology to pathophysiology.
Disease links them
In medicine if we want to maintain normal physiology this is about maintaining normal health (keeping healthy, healthy eating etc.).
When we have disease, looking at the pathophysiology path provides us with what known as a prognosis (what can see what effect its going to have)
The thing that separates normal physiology and pathology is where diagnosis comes in. You have to understand normal physiology and pathophysiology in order to diagnose properly
Treatment is understanding the pathophysiology and normal physiology so you can return to the other.
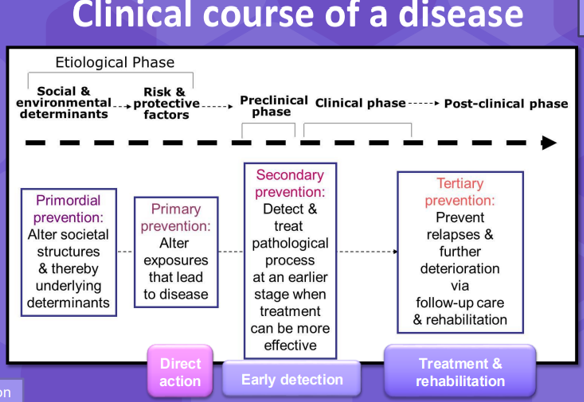
Describe the Clinical course of a disease
To start with it is good to prevent disease
The pre-clinical phase: where you get exposed to the pathogen, you get the onset of disease if you don’t control the pathogen but you don’t actually have any symptoms in this phase.
The clinical phase: where you have symptoms appearing
>Diagnosis occurs quite far on as you can only really accurately diagnose an illness at the end of the illness which is one of the problems in medicine. Treatment is also towards the end.
>The prognosis is saying what the effects or outcomes of the disease.
Diagnosis: 3 clinical separations when making a diagnosis
Symptoms, Presentation, Signs
Diagnosis: Symptoms
Feelings: Headache, feeling hot, generally unwell
All of these are used together to diagnose. Usually the diagnose a syndrome first.
Diagnosis: Presentation
Location/ Timeline: Acute(all of a sudden) vs Chronic
systematic(affecting all your systems) vs local
What happens after you have diagnosed a syndrome?
If you have a syndrome you don’t need to be diagnosed with something, you can be treated right away for what it could be.
The specific teats are done to see what it is (you usually treat people before the tests)
From the specific tests you can diagnose a disease and have specific treatments
Describe Primordial prevention, Primary prevention, Secondary prevention, Tertiary prevention
Example (MRSA sepsis)
Primordial prevention: New hospitals, better staff training, change policies
Primary prevention: Clean wards, isolate patients
Secondary prevention: Prophylactic antibodies (>Prophylactic antibiotic are given even when the person doesn’t have an infection because the chances of having an infection after surgery are high)
Tertiary prevention: Patient monitoring- labelled potentially immunosupressed
Common clinical terms: Aetiology (Etiology)
study of causation or origination of a disease
Idiopathic
relating to or denoting any disease which arises spontaneously or for which the cause is unknown
Iatrogenic
Relating to illness caused by medical treatment (e.g from chemo)
Nosocomal
disease originating in a hospital (MRSA)
Multifactorial
Involving or dependent on a number of factors, especially genetic or environmental factors
Risk factor
A factor when present increases the likelihood of disease
Pathogenesis
Development or evolution of the disease, from initial stimulus to manifestation of disease
Pathogens
agent of disease: virus, bacteria, fungi, environmental, multifactorial
Systems disease
Systems diseases can be broken down into multiple components
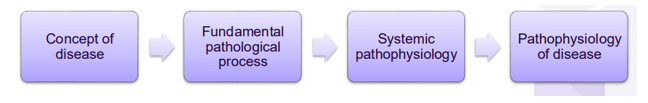
Concept of disease
What is this? E.g. infection, the concept is infection is a pathogen coming in and doing something
Fundamental pathological processes
How is the infection getting there, where does it go, what is it doing?
Systemic pathophysiology
How is it affecting those symptoms
Pathophysiology of disease
The combination of all the components
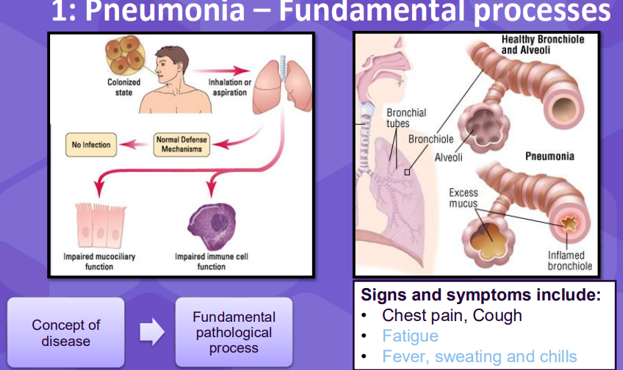
Fundamental processes- Pneumonia
>Concept of disease = there’s an infection in the lung
>Fundamental pathological process = you have to have inhalation of the pathogen e.g. bacteria normally its cleared by your defence mechanisms but for some reason it gets not your lung and affects the cells in the lung, impairing the cells that make mucus for instance and therefore breaking that barrier a little bit, or could cause extra mucus to be produced (image top right). When you get this sort of thing you can start to explain some of the symptoms.
>Systemic pathophysiology = You have an issue with your lung, you impaired gas exchange which causes hypoxia, which then affects multiple tissues in your body, but then has an impact of your heart. This dysfunction then, (you can go through multiple strategies as shown below) can cause heart failure.
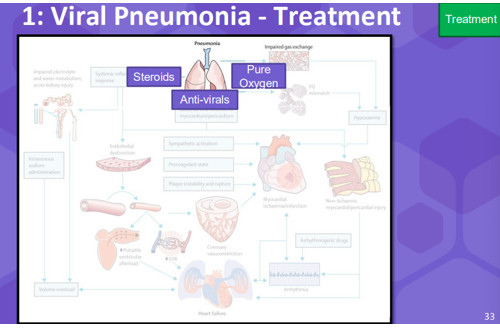
Viral Pneumonia- Treatment
We can treat it by blocking everything that leads to this bad outcome see image below. We block off all these pathways to the ultimate thnig that will kill you which is heart failure. This is why its important to understand the whole disease progression.
>You can give steroids, antivirals or and giving pure oxygen helps the lungs recover.
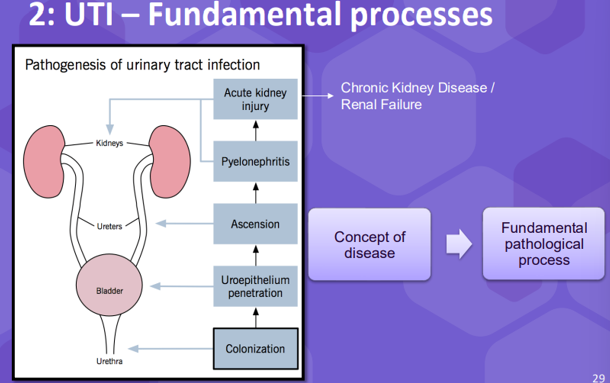
Fundamental processes-UTI
The concept of disease is that your getting an infection.
>Its an infection that probably starts in the bladder and then gets eventually to the kidneys which is the worst stage f the disease.
>Process (in diagram)
> Colonisation = Bacteria penetration into the bladder, it ascends the ureter and then eventually causes acute kidney injury which can result in chronic kidney disease.
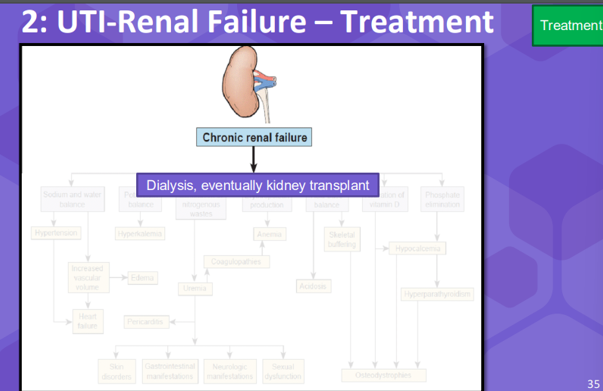
>When we look at the systemic pathophysiology of having a problem with your kidneys can result in many other health issues e.g. , see diagram above.
>Treatments for kidney disease are dialysis or a kidney transplant if it gets worse.
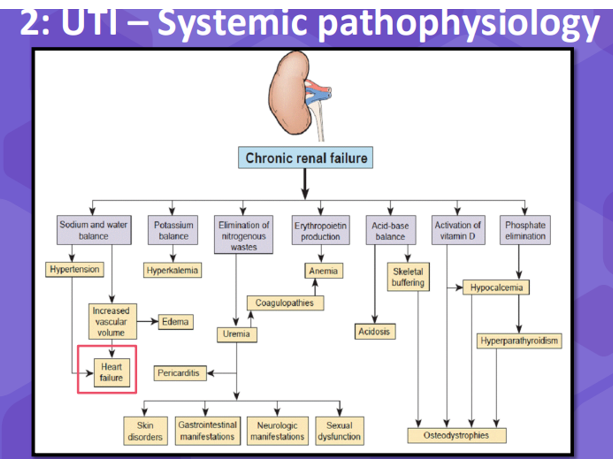
UTI-Renal Failure- Treatment
Treatment for renal failure is dialysis but if the kidney is too damaged then you require a kidney transplant. This is why its important that when you start getting this bladder infection you treat the disease before it ever gets or to treat the pathogen before it ever gets to the kidney.
Cellular stress and damage
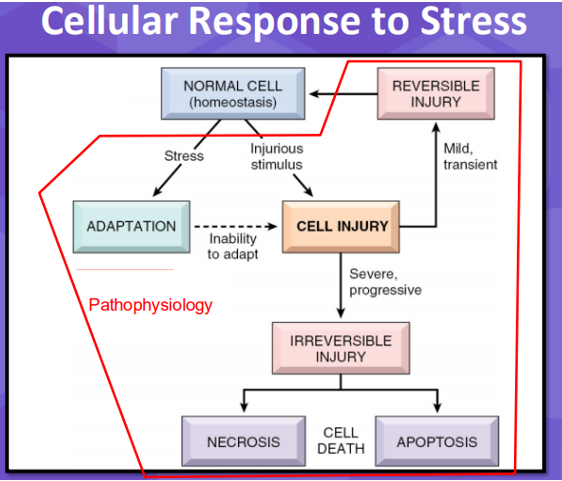
Mechanistic examples- Cellular response to stress
Cells respond to stress in different ways. Usually when a cell is stressed out it can adapt to that stress and adapt back when the stress is gone, but when its unable to adapt to maintain that, that’s when you get an injury. That can be mild which is reversable or irreversible and you can get apoptosis. When talking about cells pathophysiology includes all of this (anything that an imbalance in homeostasis).
Causes of cell stress / damage:
· Physical - heat or radiation
· Metabolic - lack of oxygen or glucose
· Chemical Agents
· Microbial Agents: Virus & Bacteria
· Immunologic Agents: Allergy, autoimmune disease, general immune response (cause damage through our cells through the action of our own immune system)
· Genetic factors: Such as sickle cell anaemia
Example of cell damage: Hypoxic ischemic brain injury
>Sudden lack of oxygen to the brain for some reason causes your brain cells to react
· Demyelination (cells aren’t able to maintain myelination of neurones)
· Endothelial degradation (blood brain barrier starts to break down)
· Lactic acidosis (cells produce lactic acid)
· Mitochondrial atrophy (mitochondria start dying)
· Clotting
Example: Neutrophil cytotoxicity
>Neutrophils are cells that would eat things like bacteria and they can also eat viruses.
Collateral damage caused by:
· Neutrophil Extracellular Traps – autoimmune amplification
>Neutrophils sort of spring load their own DNA and shoot them out of the cell at rapid velocity and these are called nets because it was almost like a net that captures bacteria. The chromatin is negatively charged so it will bind non-specifically to different things e.g. bacteria. As well as the net neutrophils release:
· Release of: ❖Toxic granules (proteases – eat (>proteins) cells)
❖Reactive oxygen species (cell bleach) >These don’t just damage bacteria but every other cell around them.
· Pyroptosis > a type of programmed cell death characterized by inflammation and cell lysis, the cell essentially explodes and releases all its content out. The cell will be reacting with the bacteria and just explodes. When the cell explodes it releases lots of different granule content… toxic granules, cell bleach, proteases, things called cell damage associated molecular patterns which activate other immune cells.
Example of cell damage: Aristolochic acid
Aristolochic acid (AA) was present in some Chinese Herbal Medicine (Pre-2000)
Kidney Nephropathy
- AA Causes cell cycle arrest in kidney cells via microRNA/ Reactive Oxygen Species
- Necrosis > caused cells to die
Liver Cancer
- Metabolites of AA directly cause DNA mutations
- Stress Response >cells adapted rather than died
Cell stress adaptations:
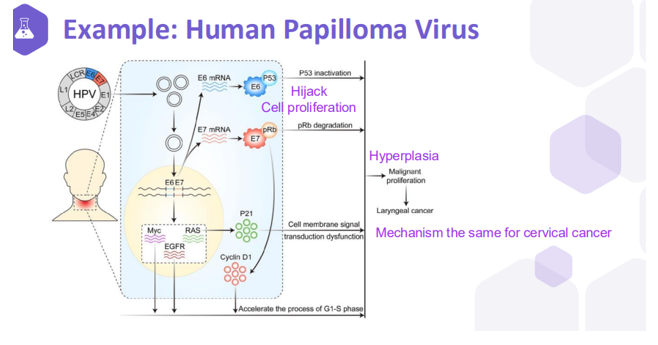
Hyperplasia - increase in number of cells in response to a stimulus. e.g. hyperplasia caused by the human papilloma virus (HPV)
Example of hyperplasia: Human Papilloma virus
The HPV virus causes hyperplasia, an enhancement of proliferation of cells. When you get more proliferation of cells you get more chances for a mutation to occur, therefore you could get cancer.
>Explaining the diagram: The viral infection causes cells to proliferate more, they hijack cell proliferation because when a cell proliferates it increases its metabolic rate which is beneficial for a virus to be able to divide. This generates more cells but because of this you have more of a chance for error and therefore more of a chance of cancer.
Cell stress adaptations
· Hyperplasia - increase in number of cells in response to a stimulus. e.g. hyperplasia caused by the human papilloma virus (HPV)
· Hypertrophy - increased size of cells, that results in an increase in size of the affected organ. e.g. high blood pressure causing heart hypertrophic cardiomyopathy
· Atrophy - decrease in the size of an organ due to a decrease in cell size and/or number. e.g. muscle atrophy in starvation
· Metaplasia – a cell type is replaced by another cell type. e.g. squamous metaplasia alteration caused by smoking, endothelial to mesenchymal