neuro exam 3
1/207
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
208 Terms
___________ is the white coating of the eyes.
a. iris
b. cornea
c. choroid
d. sclera
d.
What does the ciliary body produce?
aqueous humor
____________ is the crystal clear portion that let light in.
a. iris
b. cornea
c. choroid
d. sclera
b.
_________ is located between lens and cornea and is a circular opening of it is called the pupil.
a. iris
b. cornea
c. choroid
d. sclera
a.
___________ is between retina and the sclera, and contains connective tissue and blood vessels to provide nutrition to the eye.
a. ciliary body
b. cornea
c. choroid
d. sclera
c.
What is the measurement of fluid pressure inside the eye? What is the avg in adults?
IOP—> ~15mmHg in adults
What is the only modifiable risk factor for glaucoma?
elevated IOP
What drugs increase IOP?
anticholinergics (ex: oxybutynin, tolterodine, benztropine, antihistamines, tricyclic antidepressants)
chronic glucocorticoid therapy (topical and systemic)
topiramate
Explain how aqueous humor is produced, flows, and recycled?
idk how imp
produced in ciliary body
circulates around lens—> to pupil—> to anterior chamber
flows out anterior chamber into trabecular meshwork (80-85%)
other 15-20% of humor drains by uveoscleral pathway
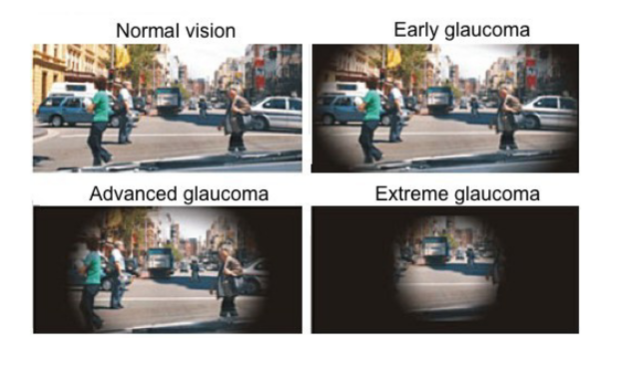
If not managed, what may glaucoma progress to?
blindness
Angle refers to the filtration angle between the iris and the cornea.
What’s the difference between open and closed-angled glaucoma?
basically—> key difference is how fluid drains from the eye
open: slowed exit of aqueous humor through trabecular meshwork—> slowly develops over time
think—> like a slowly draining sink
closed: iridocorneal angle completely closed—> flow stopped—> rapid/painful pressure increase
think—> like putting a stopped in a sink and blocking it
List the medications used for glaucoma tx:
b-blockers
a2 agonists
prostaglandin analogs
rho kinase inhibitors
carbonic anhydrase inhibitors
cholinergics
List the beta-blockers used for glaucoma tx:
are they selective or non-selective?
betaxolol- b1 selective
carteolol- nonselective
levobunolol- nonselective
timolol- nonselective
What are the advantages/disadvantages to using betaxolol for glaucoma tx?
advantage—> b1 selective, so less likely to cause pulmonary ADRs
disadvantage—> less efficacious because b2 receptors are predominant in the eye
MOA of b-blockers used for glaucoma tx:
blocks aqueous humor production
aqueous humor production is through activation of what receptors in what pathway?
through activation of b receptor Gs-cAMP-PKA pathway
List the a2 agonists used for glaucoma tx:
apraclonidine
brimonidine
a2 agonists bind to pre/post synaptic a2 receptors to cause what effects?
presynaptic: decrease NT release= decrease IOP
postsynaptic: stimulate Gi pathway= decrease cAMP= decrease aqueous humor production
ADRs of a2 agonists used for glaucoma?
idk how imp
CNS depression
ocular/skin allergy
List the prostaglandin analogs used for glaucoma tx:
latanoprost
bimatoprost
travoprost
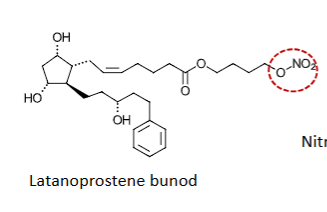
latanoprostene bunod
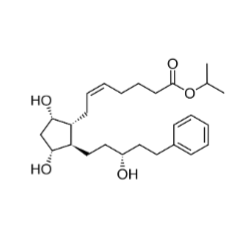
What is the MOA of prostaglandin analogs?
What type of receptor does it bind to? ionotropic? g-coupled?
What effects are seen?
PGF2a analogs—> bind to PGF receptors
PGF2a receptors are GPCRS
effect the Gq- PLC-IP3- Ca2+ pathway
effects:
altered ciliary muscle tension—> increases outflow
digestion of extracellular matrix that impedes outflow—> increases outflow
Latanoprostene bunod has what group on its structure to increase outflow?
nitric oxide donating group
ADRs of prostaglandin analogs:
darkening of iris
increase length/# of eyelashes
What drug is a rho kinase inhibitor? MOA and effects?
drug: Netarsudil
MOA: inhibits rho kinase (which regulates the cytoskeleton of the trabecular meshwork) —> increases outflow
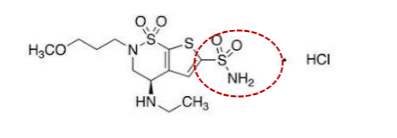
List the carbonic anhydrase inhibitors used for glaucoma tx:
which is systemic?
dorzolamide
brinzolamide
acetazolamide—> systemic, barely used/tolerated
What role does carbonic anhydrase play in aqueous humor production?
catalyzes the formation of carbonic acid from H20 and CO2
carbonic acid needed to make bicarbonate (HCO3-)
bicarb is ESSENTIAL for aqueous humor production
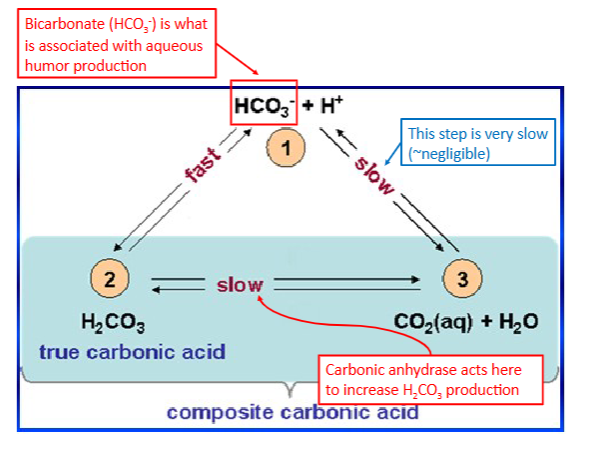
Inhibiting carbonic anhydrase leads to ___________ aqueous humor production.
a. increase
b. decrease
b.
ADRs of topical and systemic carbonic anhydrase inhibitors:
topical: sulfa allergy, burning, blurred vision
systemic: sulfa allergy, rash, ataxia, confusion, loss of appetite, n, kidney stones, hematologic toxicity
List the cholinergic agents used for glaucoma tx:
pilocarpine
carbachol
What is the MOA and ADRs of cholinergic agents?
MOA: direct agonists—> activate muscarinic receptors and cause contraction of iris sphincter and ciliary muscle
results: iris—> miosis—> increases drainage of fluid—> decrease IOP
ciliary muscles relax—> lens thickens
ADRs: pupil constriction, HA
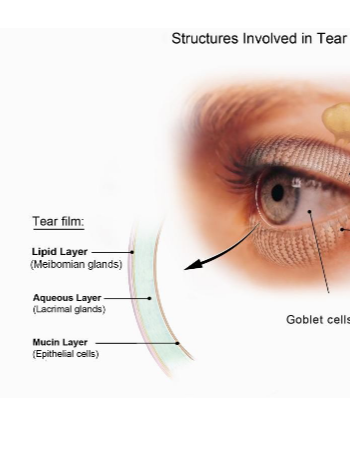
What are the 3 layers of a tear?
oil layer—> prevents evaporation
aqueous layer—> nourishes cornea, conjunctiva, eyelids, eyes in general
mucous layer—> binds water from aqueous layer to keep eye wet
Describe ocular lubricants:
admins?
designed to do what?
many admin: gels, alcohols/polymers, mineral oil
designed to lubricate cornea/conjunctiva, enhance tear activity, and reduce fricition
What medication can be used for chronic dry eye disease?
cyclosporine
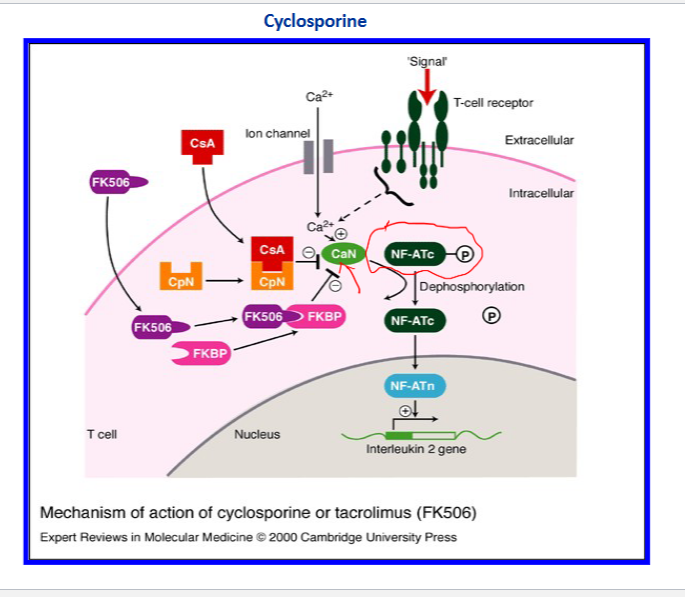
Define each of the following terms:
cyclophilin
calcineurin
nuclear factor of activated T-lymphocytes (NFAT)
immunophilin
cyclophilin- cytoplasmic receptor protein (CpN)
calcineurin- a phosphate (CaN)
nuclear factor of activated T-lymphocytes (NFAT)- intracellular protein which requires translocation from cytosol to nucleus
immunophilin- cellular protein that has strong affinity towards an immunosuppressant and forms complex
What is the MOA of cyclosporine?
cyclosporine forms complex with cyclophilin (cytoplasmic receptor protein)
complex then binds to calcineurin (a phosphatase)
this inhibits calcineurin-mediated dephosphorylation of NFAT (nuclear factor of activated T-cells)
then inhibits the next step of calcineurin-catalyzed dephosphorylation which is required for translocation to nucleus
ultimately inhibits NFAT from synthesizing interferons
PRACTICE:
What class of drugs should not be considered if the patient has a sulfa allergy?
a. beta-blockers
b. a2 agonists
c. carbonic anhydrase inhibitors
d. rho kinase inhibitors
c.
What is dementia?
defines the loss of cognitive functioning (thinking, remembering, reasoning) and behavioral abilities that interfere with a person’s daily life and activities
Does mild cognitive impairment (MCI) warrant a dementia diagnosis?
no! not everyone with MCI will develop dementia (about 15% do)
What is vascular dementia (VaD)?
how to reduce risk?
treatment?
refers to any dementia that is primarily caused by cerebrovascular disease or impaired cerebral blood flow
reduce risk—> antihypertensives, antithrombotic therapy
treatment—> cholinesterase inhibitors, memantine
What is frontal lobe dementia?
any current cure?
neuropathologically and clinically heterogeneous disorder characterized by focal degeneration of the frontal and/or temporal lobes
no current “cure”—> tx aimed at s/sx relief
What is the most common pathology of dementia and is defined as a gradual progressive dementia?
Alzheimer’s Disease
Early Onset Alzheimer Disease (EOAD) is age < ____.
Late Onset Alzheimer Disease (LOAD) is age ≥____.
EOAD is age <65
LOAD is age ≥65
What is the exact etiology of AD?
exact is not known!!! several genetic/environmental factors and hypothesizes
Which genes are most strongly associated with Alzheimer's disease risk, and what biological processes do they influence?
APOE and ABCA7—> most substantial heritable contributor to genetic risk
role: lipid metabolism
TREM2, CLU, and PICALM
role: implicated in amyloid plaque formation, tau pathology, neuroinflammation
What are the key genetic mutations associated with dominantly inherited Early-Onset Alzheimer's Disease (EOAD) and Late-Onset Alzheimer’s Disease (LOAD)
EOAD
dom inherited alterations in chromosomes 1,14, 21 that impact amyloid precursor protein (APP)
LOAD
APOE*4 allele (one copy/heterozygous less risk then two copies/homozygous)
What is Apolipoprotein E (APOE)?
fxn?
binds to what?
APOE*4 allele is associated with what?
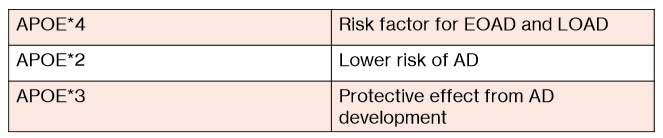
Difference between APOE*4, APOE*3, APOE*2?
APOE—> a fat-soluble transporter
responsible for transporting cholesterol in the blood/brain and interacts with b-amyloid binds to NFTs
APOE*4 allele associated with modified clearance and increased deposition of Ab in AD
APOE*4- risk factor for EOAD and LOAD
APOE*2- lower risk of AD
APOE*3- protective effect from AD development
What is one gene that actually reduces the risk of AD/ EOAD development?
A673T (a rare APP mutation)
PRACTICE:
Genetic susceptibility to late-onset AD is primarily linked to which of the following?
a. apolipoprotein E4 genotype
b. presenilin gene mutations
c. amyloid precursor protein mutations
d. apolipoprotein E2 genotype
a.
T/F: the exact pathophysiologic mechanisms of AD are unknown.
true—> there are signature lesions made of amyloid plaques and NFTs in the brain’s cortical areas and medial temporal lobe structures tho
What is the amyloid cascade hypothesis of AD?
imbalance of what?
results in?
what’s unknown about it?
imbalance between the production and clearance of b-amyloid peptides
results in accumulation/aggregation—> plaque formation—> AD development
unknown if presence of ab is the primary pathology or changes are a marker of an alternate pathology
What are tau proteins?
What are NFTs?
How are NFTs correlated with dementia?
tau proteins provide structural support (to microtubules)
NFTs are composed of abnormally hyperphosphorylated tau proteins (microtubules now can’t fxn properly)
NFT density tends to correlate with severity of dementia
what is one of the most prominent neurotransmitter defects in AD?
cholinergic abnormalities (aka loss of acetyl choline)
What is the cholinergic hypothesis in AD?
BASICALLY—> a theory that loss of cholinergic neurons and neurotransmitter dysfunction (e.g., acetylcholine) contributes to cognitive/memory impairments in AD
What are the main limitations/flaws of the Cholinergic Hypothesis?
Cholinergic neurons are just one of many pathways damaged in AD.
cholinergic cell loss is a secondary consequence of AD pathology
What do cholinergic therapies do in AD?
minimize/ improve symptoms
Explain what the inflammatory mediator hypothesis for AD is.
BASICALLY—>proposes that chronic brain inflammation plays a key role in Alzheimer’s disease
β-amyloid has direct neurotoxicity AND triggers an immune response that indirectly damages neurons.
Inflammation represents a failed attempt to clear amyloid.
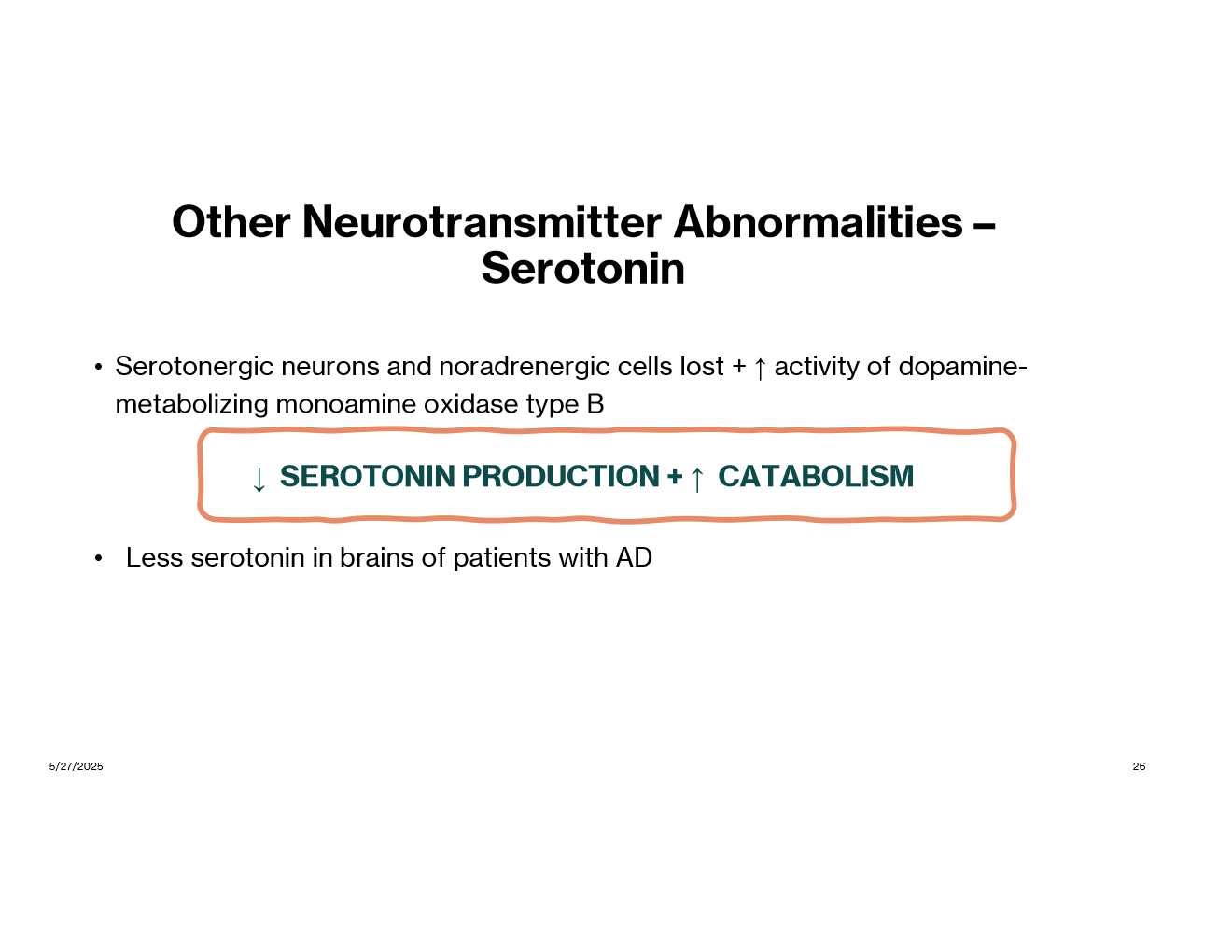
In addition to acetyl choline, what neurotransmitter abnormalities have been seen in AD?
glutamate
serotonin
There is a causal association between what disease and incidence of AD?
CV and vascular disease (ex: high cholesterol, HTN)
vascular disease may accelerate amyloid deposition and reduce clearance of amyloid b
With what stage of AD does functioning fluctuate from day to day?
a. mild
b. moderate
c. severe
b.
What are some cognitive symptoms of AD?
memory loss
aphasia (impaired communication)
circumlocution, anomia
apraxia (can’t sequence movements)
agnosia
disorientation
impaired executive fxn
What are some functional symptoms of AD?
inability to care
eating, toileting, bathing, dressing
What are some neuropsych symptoms of AD?
depression
hallucinations, delusions
behavioral disturbances
aggression
uncooperativeness
wander
repetitive manners
Screening for AD is done at what age regardless of symptoms?
mini-Cof or MoCA is rec at age 65 regardless of symptoms
What are the 4 screening assessments available for AD?
(idk how imp)
mini-mental state examination
montreal cognitive assessment
mini-cog
saint louis university mental status exam
What are the 2 categories of biomarkers in AD?
which is early changing versus late changing?
what do they help do? diagnose?
FYI: Biomarkers are measurable substances or processes in the body that indicate normal or abnormal conditions
Core 1 (early-changing)
includes b-amyloid and T1
help identify presence of AD
Core 2 (later-changing)
includes T2 biofluid and tau PET
help confirm AD diagnosis
What is the definitive diagnosis for AD?
is a clinical diagnosis!!!! (looks at symptoms, history, cognitive tests, imaging)
What is the goal of pharm therapy in AD?
tx cognitive difficulties symptomatically and preserve pt. function for as long as possible
Current AD treatments ______ seem to prolong life, cure AD, or halt/reverse processes of the disorder.
a. do
b. do not
b.
List all the pharm options for cognitive symptoms of AD:
just an overview, don’t memorize
cholinesterase inhibitors
Donepezil, Rivastigmine, Galantamine
NMDA receptor antagonists
Memantine
cholinesterase inhibitor + NMDA receptor antagonist
Donepezil + memantine
anti-amyloid monoclonal antibody (mAb)
Donanemab
Lecanemab
What is the indication of cholinesterase inhibitors?
1st line for mild-moderate AD
Name the cholinesterase inhibitors:
donepezil
rivastigmine
galantamine
What are the ADRs of cholinesterase inhibitors in general?
dizzy
syncope
bradycardia
atrial arrhythmias
sinoatrial and AV block
MI
n/v/d
anorexia
weight loss
ADRs specific to donepezil?
peptic ulcer disease
GI bleeding
insomnia
vivid dreams/ nightmares
ADRs and Counseling points with Rivastigmine?
ADR: allergic dermatitis
admin: take with food
MOA of each of the following:
donepezil
rivastigmine
galantamine
idk how imp
donepezil- specifically/reversibly inhibits acetylcholinesterase
rivastigmine- psuedo-irreversible inhibitor of butyrylcholinesterase and acetylcholinesterase
galantamine
ADR and counseling points of Galantamine?
ADR: serious skin reactions
admin: take with meals
MOA of Memantine:
uncompetitive antagonist of the NMDA glutamate receptor
ADRs and counseling points with Memantine (Namenda)?
ADRs: HA, confusion, dizzy, hallucinations, constipation
admin: can take w/ or w/out food, can open capsule and sprinkle contents on applesauce
Combination therapy is done for what kind of AD?
moderate-severe
Namzaric is a combination of what 2 drugs?
donepezil + memantine
What drugs are anti-amyloid monoclonal antibodies used in AD?
Donanemab
Lecanemab
What is the main ADRs assoicated with Donanemab and Lecanemab?
ARIA (amyloid-related imaging abnormalities)
infusion related rxns
How often is each anti-amyloid mAb dosed?
Donanemab- q 4 weeks
Lecanemab- q 2 weeks
Contraindications to taking anti-amyloid mAbs?
homozygous for APOE e4 allele
When is pharm therapy for neuropsychiatric symptoms started?
is tx permanant or temporary?
when nonpharm has failed!!
temporary tx
If an antidepressant must be used in AD, what is the DOC? what antidepressant should be AVOIDED?
SSRIs (sertraline, citalopram) most common used in AD
AVOID Tricyclic antidepressants (anticholinergic activity)
What is the BBW on antipsychotics?
increased mortality in elderly patients with dementia related psychosis
What antipsychotics can be considered in AD?
aripriprazole
risperidone
olanzapine
quetiapine
Brexipiprazole is FDA approved for ________________________.
agitation with dementia
Suvorexant is approved in patients with mild-to-moderate AD for what?
insomnia
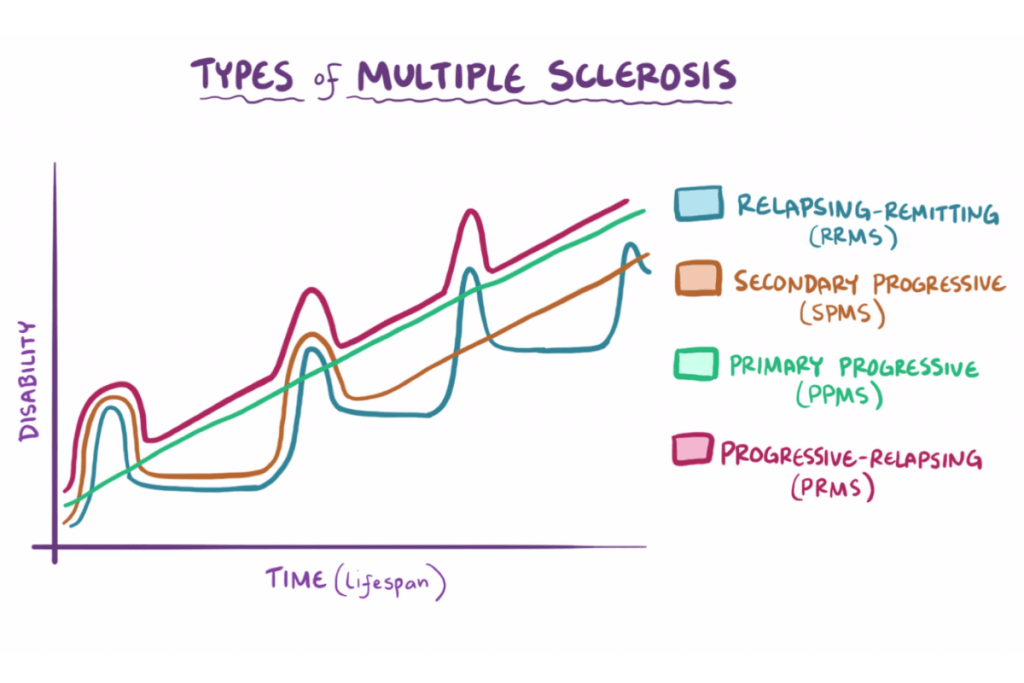
Understand the categories of multiple sclerosis and the MS patient population that are affected by each category
relapsing-remitting MS (RRMS)
temporary periods called “relapses”
attacks followed by period of remission
~85% of pts.
primary progressive MS (PPMS)
symptoms get worse with no remission period
~10% of pts.
secondary progressive MS (SPMS)
slowly worsening of symptoms and fxn
50% of pts. with RRMS convert to SPMS within 10-20
progression-relapsing (PRMS)
rare (~5% of pts.)
worsens from onset of 1st symptom
What are some lab tests for MS?
CSF analysis
MRI
optic neuritis
gadolinium
What does the Gadolinium test identify?
contrast agent to identify new lesions and disruption of the BBB
Answer the following about Interferon-B 1b drugs:
Betaseron | Avonex | Plegridy | |
Dose | XXXXXXXXXX | ||
Frequency | |||
ROA |
Betaseron | Avonex | Plegridy | |
Dose | 250 mcg | 30 mcg | XXXXXXXXX |
Frequency | every other day | once weekly | every 2 weeks |
ROA | SQ | IM | SQ |
Which medication was the first oral DMT and its contraindications?
Fingolimod (sphingosine-1-phosphate receptor agonist)
C/I:
Class Ia and III anti antiarrhythmic agents
What medication needs genetic testing for CYP2C9 polymorphisms?
Siponimod
Which medication has a black box warning for hepatotoxicity and teratogenicity?
Teriflunomide
What medications have a lifetime cumulative dose?
Cladribine
Mitoxantrone
What is the treatment of Pseudobulbar Palsy (aka emotional outbursts, dysphonia, dysphagia)?
Nuedexta (dextromethorphan and quinidine)
What medication should be used cautiously if a patient is depressed?
IFN and natalizumab