Perfusion NRS 325
1/136
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
137 Terms
perfusion definition
refers to blood flow through the circulatory system for optimal cellular activity
perfusion attributes
central perfusion
tissue perfusion
ischemia
a reduced blood flow and oxygen supply to the heart muscle, often caused by narrowed or blocked coronary arteries from plaque buildup
infarction
a part of the heart muscle is dying because its blood supply is suddenly blocked, usually by a blood clot in a coronary artery
Anoxia
a complete lack of oxygen supply to the heart muscle
Hypoxia
low levels of oxygen in your body tissues
Hypoxemia
there is an abnormally low level of oxygen in the blood, which can lead to a lack of oxygen supply to the heart and other organs
Hydrostatic
the force exerted by blood pushing against the walls of the heart chambers and blood vessels
Oncotic
the force created by proteins, primarily albumin, within the heart's blood vessels that pulls water into the capillaries, counteracting the pressure that pushes fluid out
perfusion scope
excessive perfusion —> decreased perfusion
Normal Physiological Process: Central Perfusion
Force of blood movement generated by cardiac output
Requires adequate:
Cardiac function
Blood pressure
Blood volume
Normal Physiological Process: Tissue or Local Perfusion
Volume of blood that flows to target tissue
Requires:
Patent vessels
Adequate hydrostatic pressure
Capillary permeability
Oncotic/colloidal pressure
Pulmonary Arteries
the only artery that carry oxygen-poor blood from the right side of the heart to your lungs
Remember: arteries usually go away
preload def from class
volume when ventricles are at rest
volume to start off with
pre load definition
volume of blood in ventricles at end of diastole (end diastolic pressure)
pre load increase in
hypervolemia
regurgitation of cardiac valves
heart failure
after load def from class
how much pressure to push out
how hard to push
after load definition
resistance left ventricle must overcome to circulate blood
after load increases in
hypertension
vasoconstriction
An INCREASE in afterload means
increase in cardiac workload
The equation of cardiac output
CO= SV x HR
Arterial End net filtration pressure
+ 10 mm Hg
fluid exit capillary
Mid capillary net filtration pressure
0 mm Hg
no net movement of fluid
Venous end net filtration pressure
-7 mmHg
fluid re-enters capillary
Risk Factors: Impaired Central Perfusion
Occurs when cardiac output is inadequate.
Reduced cardiac output results in a reduction of oxygenated blood reaching the body tissues
If severe, associated with shock (hypoperfusion)
If untreated, leads to ischemia, cell injury, and cell death
Risk Factors: Impaired Tissue Perfusion
Associated with loss of vessel patency or permeability, or inadequate central perfusion
Results in impaired blood flow to the affected body tissue
Leads to ischemia and, ultimately, cell death if uncorrected
TYPES OF individual risk factors
age related change
smoking
obesity
family history (genetics)
risk factor: age related change
Myocardial efficiency decreases, SA node decreases control, increased risk for left ventricular heart failure, blood vessel stiffening (resistance
risk factor: smoking
Vasoconstriction
risk factor: obesity
Relationship with chronic illness: Diabetes, hypertension, high cholesterol
risk factor: family history (genetics)
High cholesterol, atherosclerosis, history of chronic illness, history of hypertension
Common Diagnostic Tests
CK-MB
Troponin
C-Reactive Protein
Potassium (Serum)
Serum lactate
Cholesterol: HDL, LDL, Triglycerides
Coagulation Labs
MORE Common Diagnostic Test
Electrocardiogram (ECG/EKG)
Cardiac stress tests
Exercise or pharmacological test
Radiographic studies
Chest x-ray, ultrasound, arteriogram, echocardiogram
Basic EKG (parts of an EKG)
Note the normal waveforms and measurements:
P wave (atrial depolarization)
PR interval (slight atrial repolarization)
QRS (ventricular depolarization)
ST segment
T wave (Ventricular repolarization)
This all happens in about 1 second!
P wave
atrial depolarization
PR interval
slight atrial repolarization
QRS
ventricular depolarization
T wave
Ventricular repolarization
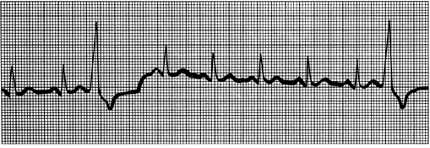
Basic EKG Interpretation: 4 basic questions
Rate – normal, brady, or tachy
Rhythm – regular or irregular
Is there a P for every QRS?
Is the QRS normal or wide?
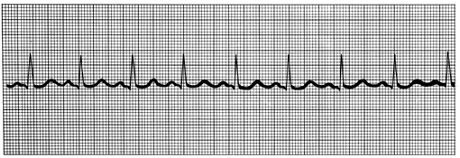
Normal Sinus
(Normal)
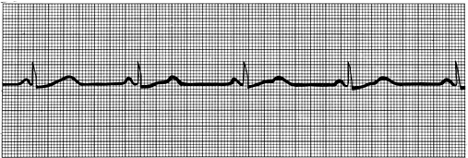
Sinus bradycardia
(rate is too slow)
sinus tachycardia
(rate is too fast)
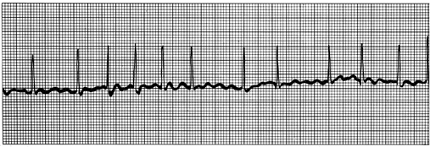
atrial fibrilation
Irregular atrial signaling
(no P wave)
Decreased CO, increased risk of clotting
premature ventricular contraction
Occasional irregular beat
(d/t ventricular signaling)
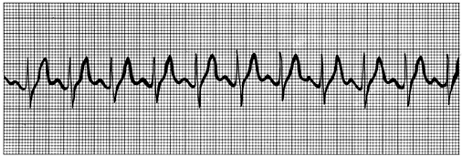
Ventricular Tachycardia
Can be sustained or nonsustained
Sustained = Emergency
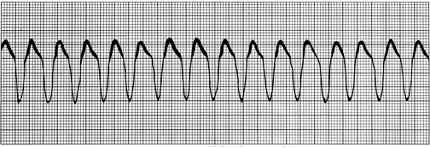
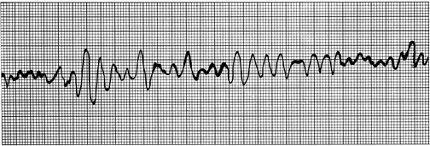
Ventricular Fibrillation
No identifiable rhythm
Sustained = Emergency
Perfusion clinical management: Primary prevention
Smoking (causes vasoconstriction) and nicotine cessation
Nutrition
Exercise
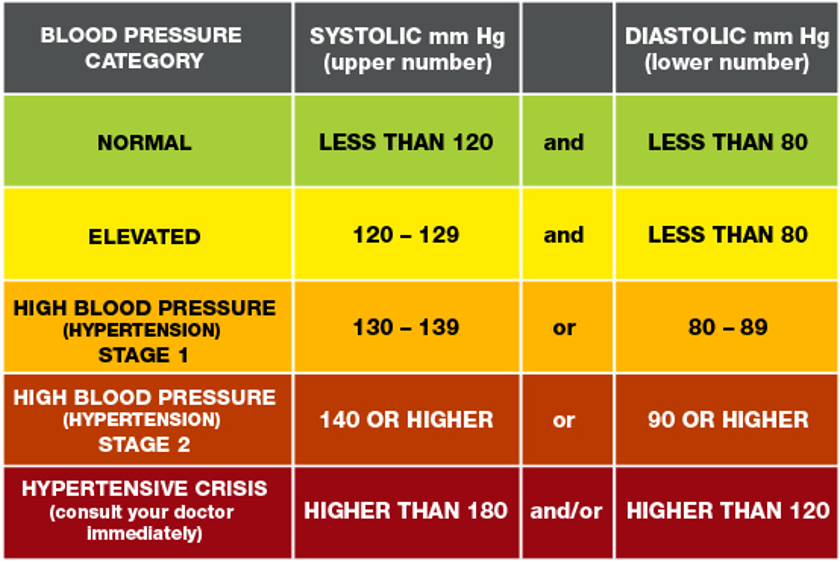
Perfusion clinical management: Screening
Blood pressure screening
Lipid screening (HDL, LDL, Cholesterol, Triglycerides)
Perfusion Clinical Management: Collaborative Interventions
Treatment strategies depend on underlying condition
The most common strategies include:
Diet modification and smoking cessation
Increased activity (Cardiac reconditioning)
Inpatient
Immediately out-patient
Long term home management
Positioning
Activity level
Pharmacotherapy
Clinical Exemplars: Pregnancy and Fetal perfusion
Increased blood volume, with decreased return
Changes in hydrostatic pressure and blood pressure
Problems with maternal perfusion can impact placental (fetal) perfusion
Perfusion Clinical Exemplars: Birth
Monitor for signs of hemorrhage in birthing parent
Rapid changes in heart at birth
Assess newborns HR, BP, SpO2, heart sounds
Some transient cyanosis around mouth, hands, and feet is not uncommon in the first 3-4 days of life
Perfusion Clinical Exemplars: Infants and Children
Typically, perfusion problems
related to a congenital defect
Infants:
Poor feeding
Poor weight gain
Failure to thrive
Dusky color
Toddlers and children:
Squatting and fatigue
Developmental delay
Failure to hit milestones
Clinical Exemplar: Infants
Poor feeding
Poor weight gain
Failure to thrive
Dusky color
Clinical Exemplar: Toddlers and children
Squatting and fatigue
Developmental delay
Failure to hit milestones
Atrial Septal Defect
mixing of blood
Usually not detected till preschool years
What is an Atrial Septal Defect?
there is a mixture of rich oxygenated and oxygenated blood due to a hole in the septum
insufficient circulation and increased work load (Increase CO)
Tetralogy of Fallot
4-5 defects
Infants develop hypoxia and cyanosis
What is the Tetralogy of Fallot?
a hole in the ventricles
mixture of oxygenated and deoxygenated blood
overriding aorta
Transposition of the Great Arteries
The pulmonary artery and the aorta are transposed
this is life threatening at birth.
What is Transposition of the Great Arteries?
the heart is ONLY pumping DEOXYGENATED blood
PFO is what is keeping the baby alive
allows a little bit of oxygen for the baby to survive
Clinical Exemplars: Adults
Myocardium less efficient and less contractible
SA Node decreases control
Left ventricular slight hypertrophy
Vessels become stiffer
Clinical Exemplars: Shock
Impaired tissue perfusion to the entire body
Results in inadequate cellular oxygenation and life-threatening cellular dysfunction.
Clinical Exemplars: Types of Shock
hypovolemic
cariogenic shock
obstructive shock
disruptive shock
septic shock
neurogenic shock
anaphylactic shock
hypovolemic shock
(Intravascular volume loss – absolute or relative)
hemorrhage= absolute and relative = fluid shift
Cardiogenic Shock
Pump failure
Obstructive Shock
Physical obstruction
Distributive shock
Systemic vasodilation
septic shock
infection
Neurogenic Shock
Spinal Cord Injury
Anaphylactic Shock
Widespread hypersensitivity AKA anaphylaxis
TYPES OF Clinical Exemplars: Classes of Shock
early, compensatory, decompensated, refractory
early class of shock
Something causes a decrease in Mean Arterial Pressure (MAP) – (This stage is rarely detected!)
compensatory class of shock
Body starts to compensate for a lack of MAP.
Changes to HR, BP, peripheral perfusion, mental status noted
decompensated class of shock
Body no longer compensating for lack of perfusion
Notable changes in assessment indicating WORSENING perfusion
refractory class of shock
Irreversible. Results in death of cells, tissues, organs
Clinical Exemplars: Atherosclerosis, Angina
Notice:
What does Atherosclerosis do to perfusion?
What is the difference between: Stable and Unstable angina
What does ST-Segment elevation look like on an ECG?
What does Atherosclerosis do to perfusion?
blocking or decrease flow to tissues and/organs by narrowing or hardening the arteries
Angina
chest pain
stable angina
has a regular pattern
rest and medications usually help
unstable angina
random pattern
pain usually doesn’t go away with medications
what does ST-segment elevation look like on an ECG?
ST raised in baseline
plaque in the coronaries
ischemia or infraction
Pharmacotherapy: Impaired Perfusion
RAAS suppressants
(ACEIs and ARBs)Adrenergic antagonists
(beta and alpha)Calcium channel blockers
Organic nitrates
Digoxin
Statins
Vasopressors
Cause vasoconstriction to increase blood pressure
Used in certain types of shock, critical care settings
RAAS Suppressants: ACE-I & ARBS
Angiotensin-Converting Enzyme Inhibitors (ACEIs) “prils”
enalapril
lisinopril
Angiotensin II Receptor Blockers (ARBs) “sartans”
Losartan
Valsartan
Treatment of:
High Blood pressure
Heart Failure symptoms
(excess fluid volume)Reduce risk of MI, stroke
Slow progression of diabetic
nephropathy
Angiotensin-Converting Enzyme Inhibitors (ACEIs) “prils”
enalapril
lisinopril
Angiotensin II Receptor Blockers (ARBs) “sartans”
Losartan
Valsartan
Types of treatment for RAAS Suppressants: ACE-I & ARBS
High Blood pressure
Heart Failure symptoms
(excess fluid volume)Reduce risk of MI, stroke
Slow progression of diabetic
nephropathy
RAAS Suppressants: ACE-I & ARBS —> Assessment
Is the med appropriate?
Assess blood pressure / Cardiac Assessment
Treat High Blood pressure
Treat Heart Failure symptoms (excess fluid volume)
Reduce risk of MI, stroke
Slow progression of diabetic nephropathy
RAAS Suppressants: ACE-I & ARBS —> Caution
Contraindicated in: Pregnancy; history of angioedema; renal artery stenosis
RAAS Suppressants: ACE-I & ARBS —> Effects
dehydration
RAAS Suppressants: ACE-I & ARBS —> Implementation/Patient teaching
Drug interactions:
Concurrent use of drugs that lower BP can cause exaggerated hypotension
Concurrent use of potassium-sparing diuretics and potassium supplements can cause exaggerated hyperkalemia
Concurrent use of lithium may result in lithium toxicity
Concurrent use of NSAIDs may reduce effectiveness of ACE inhibitor
RAAS Suppressants: ACE-I & ARBS —> Evaluation
Did it work?
Consider why was this patient taking the med?
HTN: BP is lower
CHF: less symptoms of fluid volume overload
Diabetic Nephropathy: is kidney function better?
TYPES OF RAAS Suppressants: Planning, Implementation
1st dose
cough
hyperkalemia
Angioedema
RAAS Suppressants:
Planning, Implementation —> 1st dose hypertension
ACEI: Yes
ARB: No
Nursing Interventions: Monitor, ensure safety
RAAS Suppressants:
Planning, Implementation —> Cough
ACEI: Yes
ARB: No
Nursing interventions: Monitor, Problem?
RAAS Suppressants:
Planning, Implementation —> Hyperkalemia
ACEI: Yes
ARB: Yes
Nursing Interventions: Avoid with other meds that raise K+, and salt substitutes
RAAS Suppressants:
Planning, Implementation —> Angioedema
ACEI: Rare
ARB: Even more rare
Nursing Interventions: Monitor Emergency!!
SNS Activation stimulates
alpha and beta receptors
Beta Blockers – “olol’s”
Non-cardioselective (Block beta 1 AND 2)
Propranolol
Cardioselective (Block beta 1 only)
Metoproplol
Treatment of:
High blood pressure
Heart failure symptoms
Angina pectoris
Dysrhythmias (which type?)
Non-cardioselective (Block beta 1 AND 2)
Propranolol