PTE 743: exam 3
1/133
Earn XP
Description and Tags
GBS, ALS, post polio syndrome, and spinal cord injuries
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
134 Terms
what is Guillain-Barre Syndrome (GBS)?
a rare neurological disorder where the body's immune system mistakenly attacks the peripheral nerves, causing inflammation and damage
aka “demyelinating inflammatory polyradiculoneuropathies”
what type of paralysis does GBS lead to?
flaccid paralysis
bc the nerve roots and peripheral nerves are attacked
what autoimmune illnesses can lead to GBS?
respiratory and gastrointestinal illnesses
list examples of toxic and metabolic causes that can lead to GBS.
diabetes
alcohol abuse
chronic exposure to heavy metals
in GBS, which part of the nervous system does the immune system attack?
the myelin sheath
ultimately damages the axons thus disturbing the action potentials
what’s the key difference between GBS and MS (multiple sclerosis)?
GBS: damage to myelin sheath of the peripheral axons
MS: damage to the myelin sheath of the central nervous system
how would impairment level testing results differ between GBS and MS?
GBS: results in LMN signs and symptoms
MS: results in UMN signs and symptoms
what are the signs and symptoms of a UMN?
weakness, paralysis, mild atrophy
hypertonia, spasticity
hyperreflexia
pos babinski sign
clonus
what are the signs and symptoms of a LMN?
weakness, paralysis, profound atrophy
hypotonia, flaccidity
hyporeflexia
fibrillations and fasciculations
describe the motor impairments seen with a diagnosis of GBS.
varies from mild weakness of distal LE musculature to total paralysis of peripheral, axial, facial, and extra-ocular musculature
describe the clinical presentation of GBS.
rapidly evolving, symmetrically (bilaterally) ascending weakness or flaccid paralysis
can involve children and adults
GBS travels distal to proximal in the onset of muscle weakness, but what is the exact progress?
begins in the feet and only starts in the hands when the weakness reaches the thighs
what would make a therapist suspicious that a patient may have GBS?
patient presents with limited foot clearance, leg heaviness, general LE weakness, and not feeling right
T or F: patients presenting with onset of pain not associated with a known injury or stress and complain of paresthesias and vibratory or decreased DTRs should be assessed for GBS.
T
of patients who develop GBS, ____ require assisted ventilation due to paralysis or weakness of intercostal and diaphragm muscles and ____ develop cranial nerve involvement (primarily facial muscle weakness).
30%
50%
GBS can also affect the autonomic nervous system with 50% of patients reporting issues. what are some examples of these clinical presentations?
low cardiac output
cardiac arrhythmias
fluctuations in BP
peripheral pooling of blood with poor venous return
urinary retention
describe the sensory symptoms reported with GBS.
stocking and glove pattern
describe the prognosis for a patient with GBS.
may experience max. paralysis in first 1-2 days → disease progresses for 3-4 weeks → shows gradual recovery of strength 2-4 weeks post-plateau of progression → 80% become ambulatory within 6 months of onset of symptoms
15% of GBS patients show persistent residual deficits in function. where do therapists see this at?
weakness in ankle dorsiflexors (specifically tib ant), foot, and hand intrinsics
what should a patient with GBS do to prevent unexpected rapid onset of respiratory failure?
should be hospitalized and may be intubated
what are the two key factors when performing a motor evaluation on a patient with GBS?
test muscle strength and ROM as specifically as possible (helps track progression)
avoid fatigue in a single session
how could one help with respiratory and dysphagia dysfunction associated with GBS?
increase ventilation
decrease oxygen consumption
control secretions
improve exercise tolerance
dysphagia = see a SLP
T or F: wrapping limbs snuggly with elastic bandages to provide continuous light pressure can reduce hypersensitivity experienced by a patient with GBS.
T
how do patients with GBS prevent contractures and decubitus ulcers?
positioning program
pressure relieving mattress
mild continuous stretching
orthotics
when can a patient with GBS progress with a standing program?
when respiratory and ANS are no longer unstable and patient can tolerate moving to a tilt table
may experience issues with hypotension due to prolonged immobility
what benefits to preventing secondary complications may be obtained by using a tilt table in the early stages of GBS recovery?
improved lung function
increase weight bearing through LEs
challenges tolerance to upright position
what is the biggest risk when changing the posture of a patient with GBS?
the movement can trigger orthostatic hypotension
always monitor vitals!
therapists should provide ROM at least 2x per day to patients with GBS. what are three modalities to help ROM?
continuous passive massage
soft tissue massage
heat!!
T or F: when diagnosed with GBS, strength is lost and gained in an ascending pattern.
F; strength returns in a descending pattern
exercise will not hasten or improve nerve regeneration in a patient with GBS, so what’s the point?
exercise maintains musculoskeletal system in the optimal “ready” state, prevents overwork, and paces recovery process
what are the recommendations for exercising a patient with GBS?
short periods of non-fatiguing exercises
increase activity level only if patient improves and there is no deterioration after 1 week
return to relative bed rest if decrease in function or strength
focus on strengthening for function!
what is amyotrophic lateral sclerosis (ALS)?
a degenerative, terminal disease affecting upper and lower motor neurons causing a massive loss of anterior horn cells of the spinal cord and loss of motor cranial nerve nuclei in the lower brain stem and an eventual hardening of the ventral and lateral column of the spinal cord as the nerves are degenerating and are replaced by fibrous astrocytes
describe the mixture of upper and lower motor neuron deficits that a patient with ALS will experience.
UMN deficits seen below the levels of lesion
descending pathways cannot modulate movement → spastic paralysis, hyperreflexia, and pos pathological reflexes
LMN deficits seen at the level of lesion
damaged reflex arc at the anterior horn → flaccid paralysis, hyporelfelxia, and muscle atrophy
T or F: ALS is the most common form of motor neuron disease affecting mostly females aged 50-70 years old.
F; males are 2x more likely to get ALS than females
what are the two most common symptoms leading to an ALS diagnosis?
fatigue
weakness (although its not evident to patient until has loss of function)
describe the pattern of weakness seen in a patient with ALS.
motor loss typically moves from distal to proximal
flexors weaker than extensors!
bulbar signs/symptoms common later in disease progression
a patient presents with tongue fasciculations and weakness, facial weakness, dysphagia, and dysarthria after finding out 2 weeks ago that he has ALS. what is his prognosis like?
poor :( a rapid progression with an early death
these are bulbar signs
80% of patients with ALS show early clinical signs of pyramidal tract dysfunction. what are the 3 signs of this dysfunction?
hyperreflexia in the presence of muscle weakness and atrophy
spasticity with resistance to PROM testing
pos babinski or hoffman reflex
T or F: there is no single laboratory test available to confirm diagnosis of ALS but creatine phosphokinase levels are usually found to be elevated.
T
what does an EMG show when done on a patient with ALS?
spontaneous fibrillations and fasciculations with giant unit spikes with voluntary activity
why are nerve conduction velocity tests usually within normal limits in the early stages of ALS?
ALS is not a demyelination disease so nerve velocity is relatively fine; its only affected when muscle weakness is significant
what are the two criteria/circumstances for a definitive diagnosis of ALS?
patient must show 1) UMN and LMN signs in 3 spinal regions or 2) UMN and LMN signs in 2 spinal regions with bulbar signs present
what happens when neurons are damaged (in ALS patients)?
neurons become hyper-excitable → release excessive amounts of glutamate → leading to damage and death of motor neurons
when a patient with ALS complains of spasms, what is the best way to manage that?
relieve with stretching or increase in movement or medication such as Baclofen
why might pain medications not be the best course of management for a patient with ALS?
due to the compromised respiratory function, care must be used when prescribing and dosing medication, as opioids can suppress respiration
manipulating food in the mouth and the ability to articulate sound through speech become huge problems for patients with ALS. what are the cranial nerves associated with these functions?
CNs 5 (motor portion), possibly 7, 9, 10, and 12
why is the loss of swallowing a big concern for patients with ALS?
it increased the risk of aspiration therefore increasing the risk of aspirational pneumonia
in regards to dysphagia and dysarthria, what are some common signs of both seen in patients with ALS?
drooling and chocking
inadequate breath volumes
abnormal breathing speed and cadence
reduced speaking volume and compromised speech
stroke patients may also have problems with drooling or manipulating food in their mouths. how is it different from a patient with ALS?
stroke: the motor and/or sensory loss is unilateral → the drooling and pocketing of food in the mouth occur on just one side
ALS: the motor and/or sensory loss is bilateral
what are some clinical signs of progressive respiratory failure?
tachycardia
changes in sleep pattern with daytime sleepiness
difficulty concentrating, mood swings
morning headache
dyspnea (difficulty breathing) with exertion or lying supine
hypoventilation
increased use of auxiliary respiratory muscles
physical therapy goals must be based on ALS patient’s goals and ultimately optimize health. list some examples of goals?
maintain max independence and positive quality of life for as long as possible
maintain max muscle strength within limits of disease
prevent and minimize secondary complications of disease (contractures, ulcers, thrombophlebitis, infections)
what are the two therapeutic balance of activity goals for patients with ALS?
prevent disuse atrophy
prevent overuse injury
what is post-polio syndrome (PPS)?
a condition that affects individuals who have previously had polio, causing a new onset or worsening of muscle weakness and other symptoms due to the deterioration of motor neurons in the spinal cord that were damaged by the polio virus
post-polio syndrome appears around how many years after acute onset?
35 years
what are the features of a lower motor neuron disease such as polio?
asymmetry in signs and symptoms
atrophy of muscles
loss of balance
secondary scoliosis
contractures of plantarflexors, hip flexors, and paraspinals on one side
picture of motor units of a patient with polio and PPS

how would patients with polio eventually be able to move if recovery was not complete?
via compensation by using assistive devices, braces, and/or altered movement patterns
what might be the long-term effects of partial or complete paralysis for a patient with polio?
muscle atrophy (LMN)
joint contractures and loss of muscle length (hypomobility)
hypermobility where joints are not supported by musculature
what are the two primary impairments a therapist would suspect to find based on the pathogensis PPS?
flaccid muscle paresis
paralysis
what are the secondary impairments a therapist would suspect to find based on the pathogensis PPS?
excessive or limited ROM
a unique type of fatigue!
deep muscle/joint pain
new muscle weakness
when treating a patient with PPS, why would a therapist not want to use cyrotherapy as a modality?
patient likely has cold intolerance from reduced muscle contraction and poor circulation→ poor perfusion
to receive a definite diagnosis of PPS, a patient must present with the onset of two new symptoms and have a history of paralytic polio. what are these symptoms?
excessive fatigue
muscle or joint pain
muscle atrophy
cold intolerance
*all of these must be beyond the normal expectation for aging
what is the prognosis of PPS?
its a slow degenerative/progressive condition that relates to the severity of the original deficits of the patient’s polio case
there is no single medical treatment for PPS, but studies have found some treatments that help. what are they?
IV immunoglobulin to reduce pain, improve muscle strength, and improve overall quality of life
surgeries such as arthrodesis or tendon transfers
describe the difference in disease atrophy and disuse atrophy in cases of PPS?
disease-condition atrophy: primary condition of PPS and therapy cannot really help or control
disuse atrophy: secondary condition to PPS and therapy can help with
what are the two types of pain a patient with PPS might experience?
diffuse muscle pain: increased with activity and decreases with rest, unaffected by meds or modalities
specific to body part: usually affects parts of body more affected by original polio diagnosis, but can occur elsewhere
how would a therapist’s treatment plan differ for the two types of pain experienced by a patient with PPS?
diffuse muscle pain: pacing or changing of activities, non-fatiguing functional activities, more frequent rest periods
specific to body part: relative rest, postural awareness, massage, maybe compensatory methods
T or F: abnormal fatigue is the most common and most debilitating symptom of PPS.
T
often occurs later in the day and may not seem related to activity or to improve with rest
muscle weakness can be seen in both the affected and unaffected extremities of a patient with PPS. why?
compensatory movements with unaffected extremity can lead to overuse
what are some other associated signs with new muscle weakness?
fasciculations
muscle cramps
muscle atrophy
elevated muscle enzymes in blood
what is a key question physical therapists must ask ourselves when treating patients with PPS?
I said to myself, “self, is this patient’s weakness due to overuse OR disuse?”
answer requires a thorough exam to precisely determine the cause
what are the treatment goals for overuse weakness?
slow the rate of progression by decreasing workload on muscle and perform non-fatiguing functional activities
what are the generalized treatment factors for disuse weakness?
begin and progress slow
give frequent rests and monitor for fatigue
submax resistance is recommended at a low to mod intesity
monitor muscle ache and tenderness
50% of patients with PPS report sleep disturbances. why is that a problem?
it can lead to pain, stress, hyperventilation, and/or obstructive apnea
T or F: patients who overcame polio as a child are considered lazy now because of the extreme disadvantages they experienced early in life.
F; they are actually super motivated and have trouble slowing down because they are used to working hard to overcome challenges
SUB: a patient reports progressive weakness starting in his feet, which ascended over a few days to involve his legs and now affects his arms. he was hospitalized one week ago when he became unable to walk and started experiencing mild difficulty with breathing. he reports tingling in hands and feet but denies pain.
PMH: no prior neurological issues but had a flu-like illness ~10 days before weakness started.
Strength: 2/5 BLE, 3/5 BUE (MRC scale)
Reflexes: absent in all extremities
Sensation: decreased light touch and proprioception in distal extremities
Cranial Nerves: intact
Respiratory: VC mildly reduced; under observation by pulmonary team
DX?
GBS
SUB: a patient reports increasing difficulty with speech and swallowing over the past 6 months. in the last two months, she's begun to notice weakness in her hands and legs, as well as frequent tripping and muscle cramping. fatigue is worsening, particularly in the afternoon. she is still living independently but requires increasing help from her husband.
PMH: hypertension (controlled), no prior neurologic issues
Strength: B UE 4-/5, B LE 3+/5 (distal > proximal weakness)
Tone: mild spasticity noted in lower extremities
Reflexes: hyperreflexia in knees, positive Babinski bilaterally
Speech: dysarthria; communication board used occasionally
Swallow: mild dysphagia noted by SLP
Sensation: intact
DX?
ALS
SUB: a patient reports increasing fatigue, new-onset muscle weakness in both legs, and difficulty walking long distances over the past year. he also notes muscle and joint pain in his shoulders and knees, and frequent tripping, especially in the evening. no recent illness or injury. he fears losing independence and has started limiting activities due to fatigue.
PMH: polio at age 8; recovered functional ambulation with LLE residual weakness
DX?
PPS
what is a spinal cord injury (SCI)?
occurs when the spinal cord is damaged
damage can result in a range of functional losses, including paralysis, altered sensation, and autonomic dysfunction, depending on the severity and location of the injury
what are the main causes of SCIs?
MVA
falls
violent acts
sports injuries
what are the leading causes of death for a patient with a SCI?
pneumonia- bed ridden for long periods of time
pulmonary emboli- DVT risk increases
septicemia- blood infection (sepsis) from UTIs
what protects the spinal cord?
dura mater, vertebral bodies, and spinous processes
what’s the difference between tetraplegia and paraplegia?
tetraplegia: impairment or loss of motor and/or sensory function due to damage of cervical segments of spinal cord, affecting UE, LE, and trunk
paraplegia: impairment or loss of motor and/or sensory function due to damage of thoracic or lumbar segment of spinal cord, affecting trunk and LE
how do physicians differentiate between a complete or an incomplete spinal cord lesion when making a diagnosis?
the patient will have total loss of sensory and motor function in the lowest sacral segments (S4-S5) if its a complete SCI
incomplete SCI: partial presentation of sensory and/or motor below neurological level and at S4-S5
what is spinal shock?
flaccid paralysis and absence of all spinal cord reflex activity below level of lesion; occurs 30-60 mins after spinal trauma and can last up to 24+ hours
T or F: associated injuries can occur with/ alongside the SCI location and can vary depending on SCI level.
T
T or F: we must test visual, somatosensory, and vestibular systems with SCI patients too.
T
incomplete spinal cord lesions chart
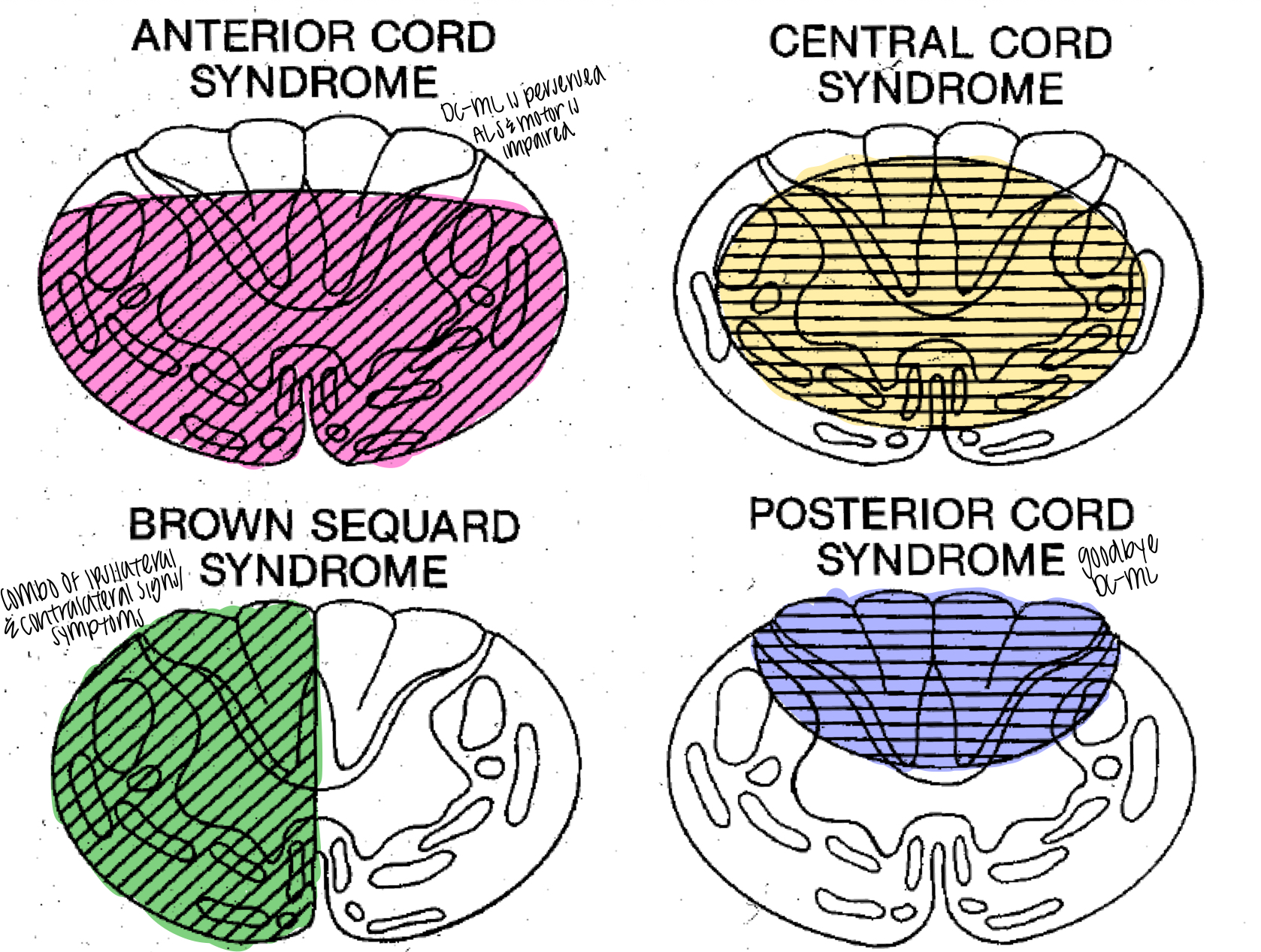
describe the factors that make up anterior cord syndrome.
occurs from a flexion injury
motor function and pain/temp sensation lost bilaterally below impaired segment
poor prognosis for return of bowel/bladder, hand function, and ambulation
pos babinski
describe the factors that make up central cord syndrome.
results from hyperextension injuries of the C spine and causes bleeding into the central gray matter
results in more impairment of function in UE than LE
majority of incomplete lesions
prognosis varies between patients: 77% ambulate, 53% bowel/bladder control, and 42% hand function
describe the factors that make up posterior cord syndrome.
less common SCI
results from compression by tumor or infarction of the posterior spinal artery
loss of proprioception, stereognosis, 2-point discrimination, and vibration sense below level of lesion
describe the factors that make up Brown-Sequard syndrome.
½ cord is injured, likely from penetrating injuries
ipsilateral loss of motor and position sense and contralateral loss of pain and temp sensation
prognosis is good: nearly all ambulate, 80% regain hand and bowel control, and 100% have bladder control
presents similar to a stroke patient
describe the factors that make up conus medullaris syndrome.
injury to caudal end of cord, around L1
often bilateral presentation; depending on UMN and LMN based on lesion site
often affects LE function, genitals, and bowel/bladder (non-reflexive)
describe the factors that make up cauda equina syndrome.
occurs with injuries at or below L2
LMN lesion, usually incomplete lesion
results in flaccid paralysis with no spinal reflex activity present
what are the early goals when treating patients with SCI?
reduce cord compression and edema
fix gross malalignment and focus on stabilization
fracture stabilization
which bodily systems should be reviewed with a SCI patient?
cardiopulmonary, integumentary, musculoskeletal, neuromuscular, urogenital, psychological, gastrointestinal, and endocrine
we listed many reasons why a patient with a SCI may experience a pressure ulcer during lecture, but which one is the biggest risk?
patient cannot feel if she/he has pressure on one area for too long
what type of wheelchair back support is most appropriate?
biangular/curved
what is the best pressure relief when sitting in a wheelchair? (2 answers)
boards answer: push up off chair with C7 or below SCI
Dr. Shaw’s answer: shift weight/ readjust sitting posture
what are the recommended time frames/durations for push up pressure relief?
hold for 90 secs, performed every 30 minutes while sitting