Chapter 9 & Ch 11 - Muscles and Muscle Tissues & Nervous Tissue and Muscles
1/56
Earn XP
Description and Tags
KNR 181 - Micheal Torry's Session M, W, F Overview
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
57 Terms
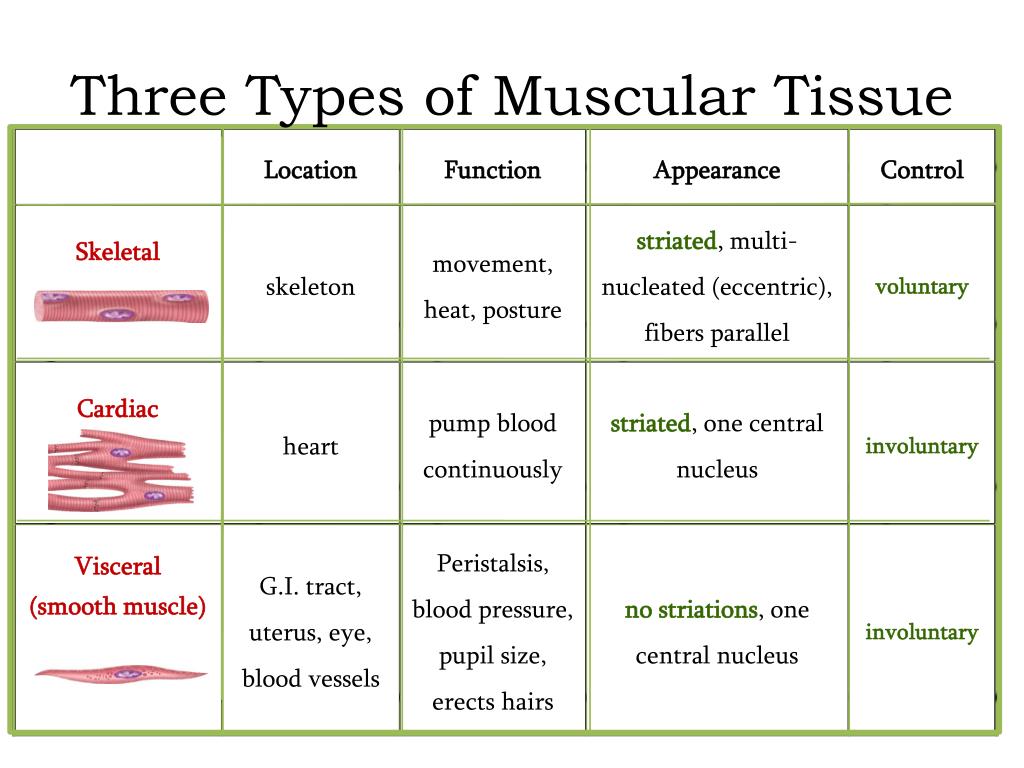
What are the three types of muscle tissues and how are they different in structure?
Skeletal muscle -
attaches to bone, skin, or fascia
Striations; light & dark bands visible with scope
Voluntary control of contraction & relaxation
Considered voluntary because it is the only under our conscious control. Skeletal muscle is often activated by reflexes.
Contracts rapidly but tires easily and must rest after short period (compared to your heart which doesn’t get tired).
Can exert tremendous power and is adaptable force needed to pick up a paperclip vs. a heavy dumbbell
Cardiac muscle -
Occurs only in the heart
Striated tissue
Involuntary contraction
Makes up the walls of the chambers
Contracts without stimulation from the nervous system (intrinsic rhythm set by SA node)
But can be manipulated and controlled by the nervous system (sympathetic response) in times where we need heart to speed up
Smooth muscle -
Found in the walls of hollow visceral organs
Smooth, urinary bladder, respiratory passages
Functions to force substances through body passages
Elongated, non-striated tissue
Slow, sustained, involuntary contraction
Action/Myosin present but not myofibrils composing sarcomeres
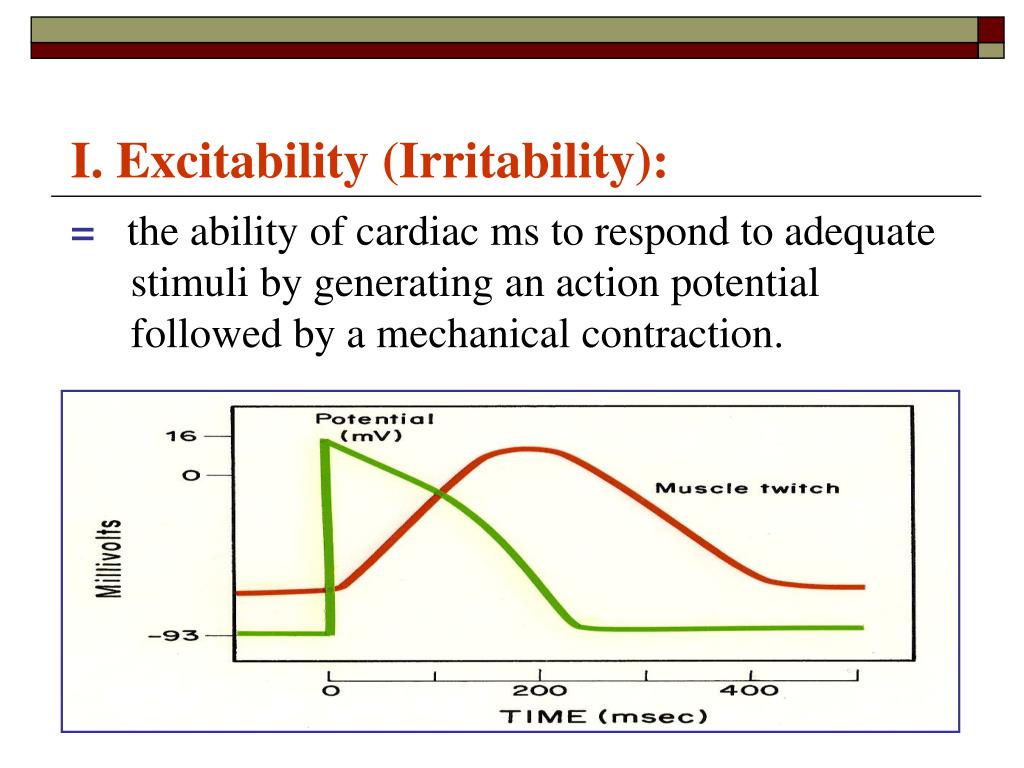
define excitability
ability to receive and respond to stimulus (muscles respond to neurotransmitter presence/signals contraction)
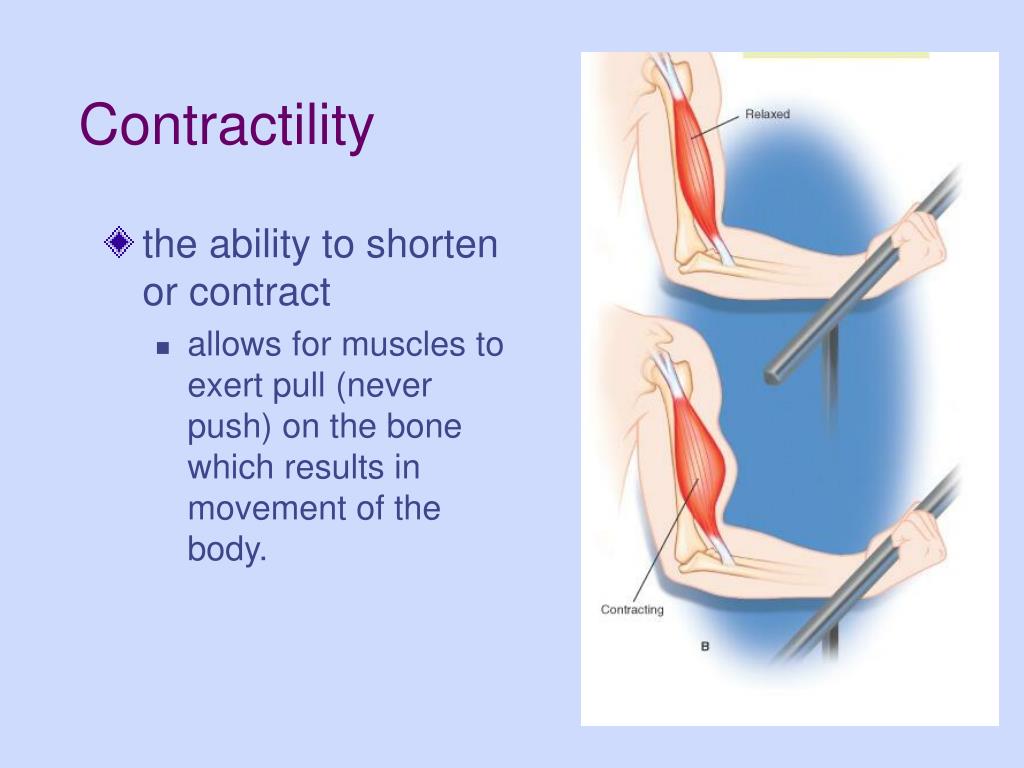
define contractibility
ability to shorten forcibly upon stimulation (sets muscles apart from other tissue types)
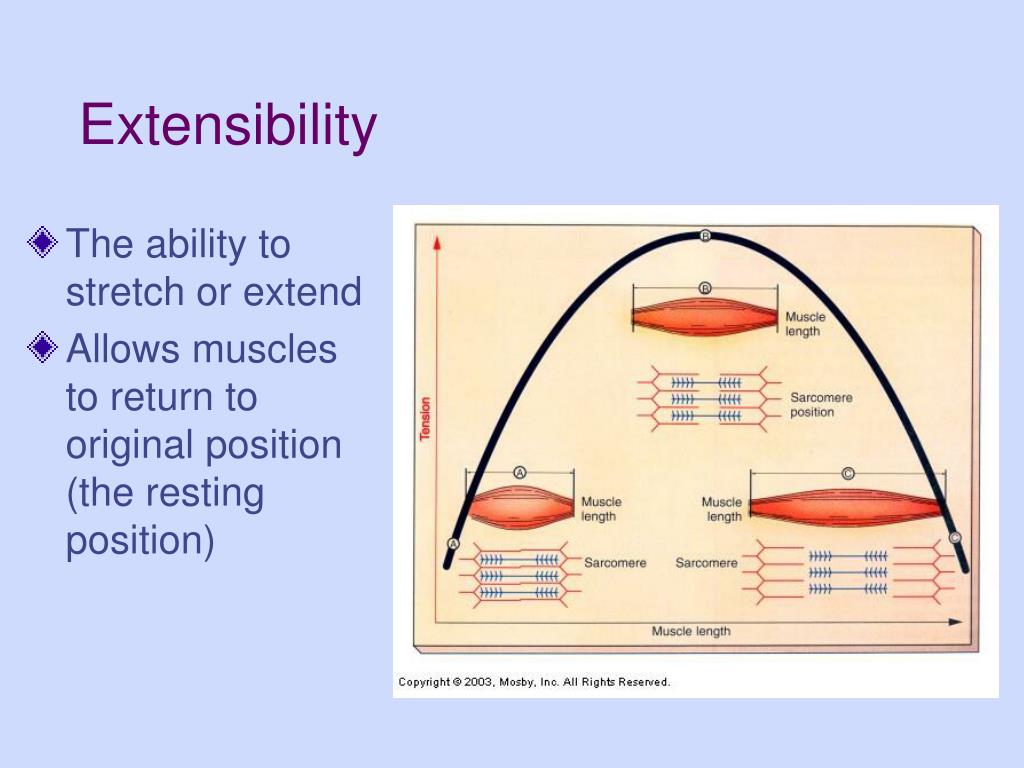
define extensibility
ability to be stretched/lengthened can stretch beyond their resting length when relaxed
define elasticity
ability to return to a resting length after elongation (recoil, resume resting length)
What are the four main functions of muscle?
1) Produce movement - locomotion and manipulating environment
2) Maintain posture - rarely aware of muscles contracting now to maintain our body posture (upright) Function continuously
3) Joint stabilization - most important stabilizing factor is muscles/tendons that cross the joint
4) Produce heat - through contraction which plays a role in maintaining body temperature
Describe the nerve and blood supply for muscle?
One nerve, one artery and one or more veins serve each muscle. These structures all enter or exit near the central part of the muscle and branch profusely through its connective tissue sheaths.
Each skeletal muscle fiber is generally innervated by one nerve ending.
Skeletal muscle = an organ
Muscle tissue
Nervous tissue
Connective tissue
Richly supplied with blood vessels
Muscle capillaries
Oxygen supply; waste removal
Blood - contracting muscles need energy and require continuous delivery of oxygen and nutrients. Muscle cell produces wastes (CO2 and lactate) which must be removed through veins or else contraction could be compromised.
Capillaries of muscles are long, and winding allow muscle to change lengths and straighten when muscles are stretched.
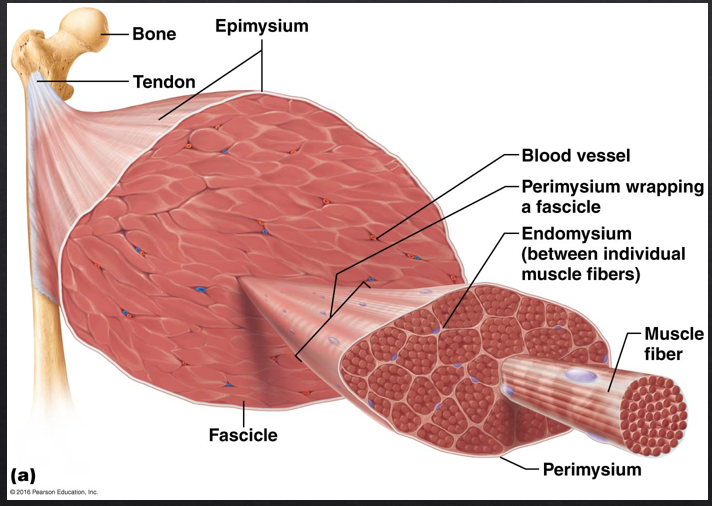
What are the three components of connective tissue of the muscle and what muscle structures do they protect/surround?
Supports and reinforces the muscle organ
Epimysium: “outside the muscle”
Overcoat surrounding the entire muscle of dense irregular connective tissue
Sometimes it blends with the deep fascia that lies between neighboring muscles or the superficial fascia deep to the skin
Perimysium: “fascicles” “resembles bundle of sticks”
Surrounds fascicles (bundles of muscle fibers)
around the muscle
Each fascicle is a layer of dense irregular connective tissue
Endomysium: “within the muscle”
Surrounds individual muscle fibers
Is a wispy sheath of connective tissue
It consists of fine areolar connective tissue
Holds things together so that muscles don’t burst out during strong contractions
Define origin and insertion of muscle?
Origin
Typically, the “less” moveable bone
Usually proximal
Insertion
Moveable bone
Usually distal to the origin
Usually done through (indirect attachments)
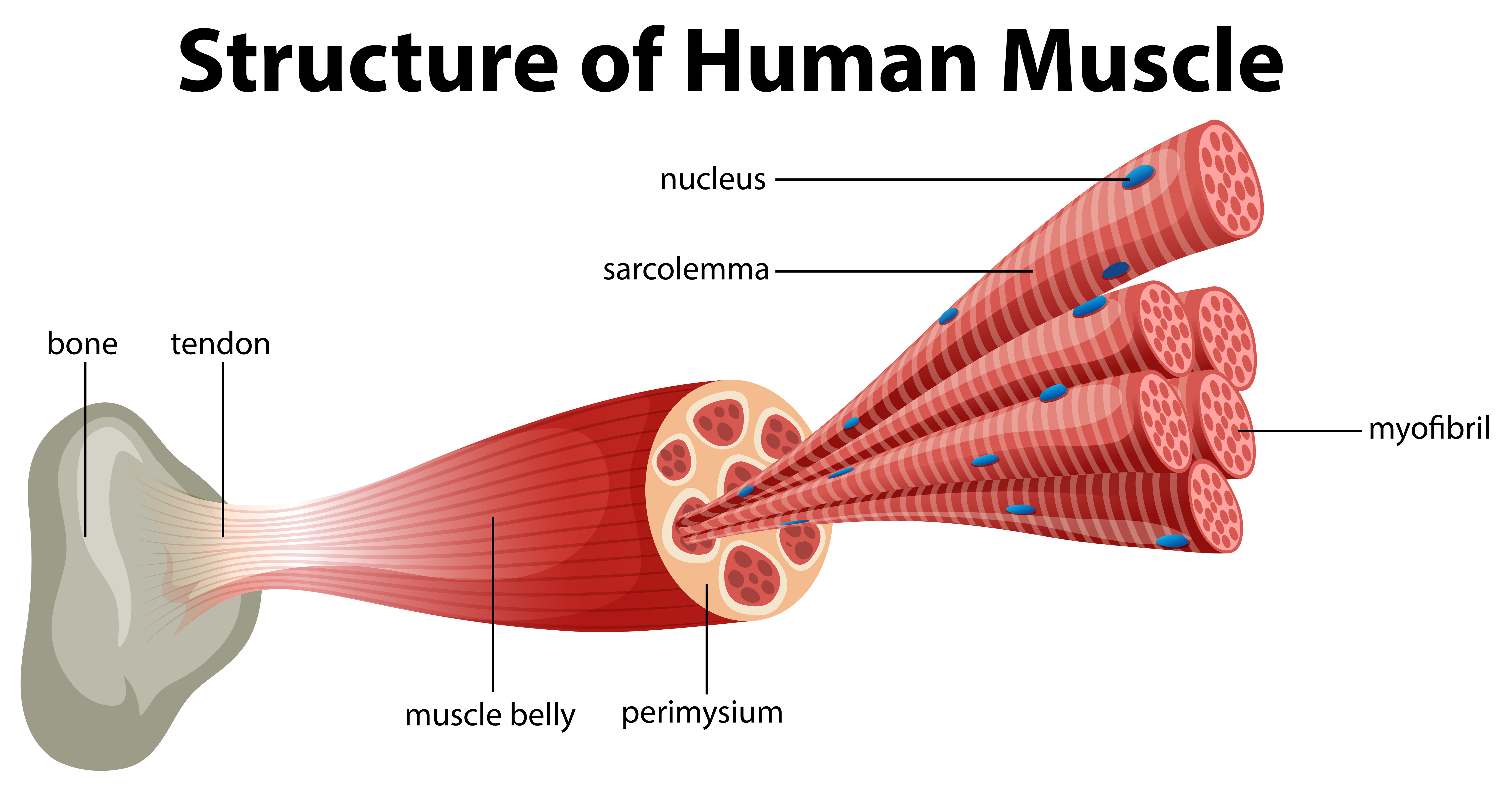
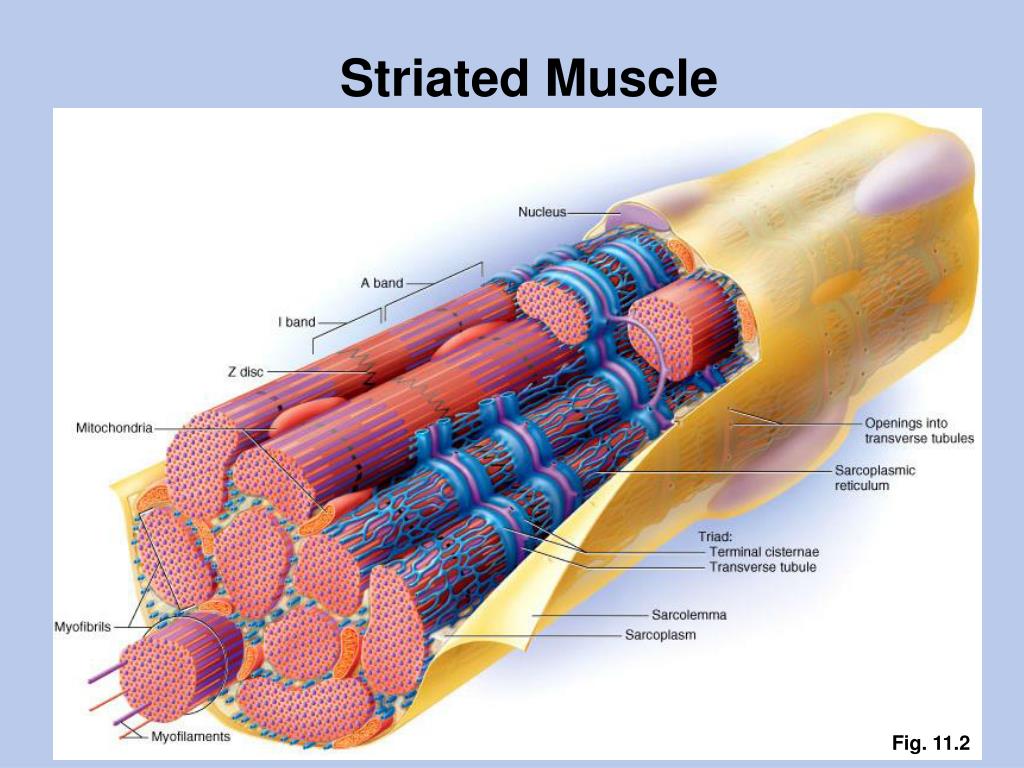
What is the organization structure of muscle (from whole muscle to myofilament)
Muscle (organ) - a muscle consists of hundreds to thousands of muscle cells, plus connective tissue wrappings, blood vessels, and nerve fibers
Connective Tissue Wrappings - covered externally by the epimysium
Fascicle (a portion of the muscle) - a fascicle is a discrete bundle of muscle cells, segregated from the rest of the muscle by a connective sheath
Surrounded by perimysium
Muscle fiber (cell) - a muscle fiber is an elongated multinucleate cell; it has a bonded (striated) appearance; surrounded by endomysium
Myofibril (complex organelle composed of bundles of myofilaments)
appears banded
Rodlike contractile elements that occupy most of the muscle cell volume. Composed of sarcomeres arranged end-to-end
Sarcomere (a segment of myofibril)
A sarcomere is a contractile unit, composed of myofilaments made up of contractile proteins.
Thin (actin) filament
Thick (myosin) filament
Myofilaments (extended macromolecular structure)
Thick filaments contain bundled myosin molecules; thin filaments contain actin molecules (plus other proteins). The sliding of the thin filaments past the thick filaments produces muscle shortening.
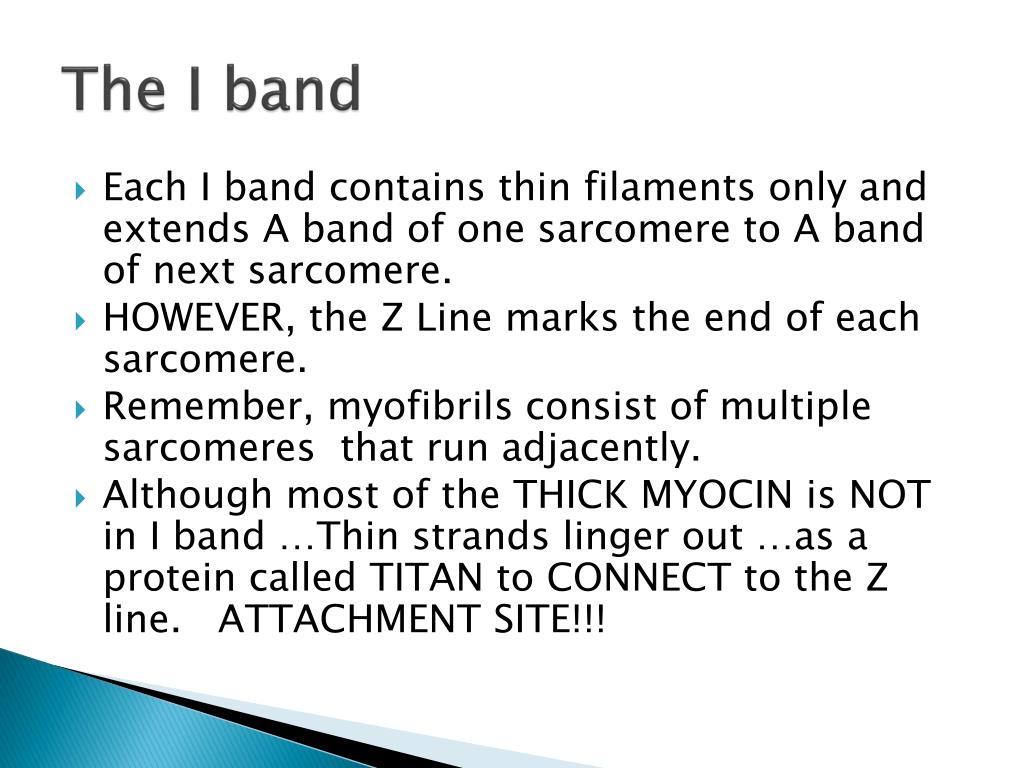
Describe the regions of the striations in skeletal muscle. What makes up each region of the bands of striated muscles?
Sarcomere - The smallest contractile and functional unit of a muscle fiber.
It extends in the region between two successive Z-discs.
Sarcomeres are aligned end-to-end to form a myofibril.
Alternates light and dark bands.
Thin filament (actin) - Extend across the entire length of the ‘I band’ and partially into the ‘A band’
Anchored by the ‘Z discs’
Remember z disc to Z disc is one sarcomere
Thin filaments are made of actin, troponin, & tropomyosin
The myosin-binding site on each actin molecule is covered by tropomyosin in relaxed muscle
Thick filament (myosin) - Extend across the entire length of ‘A band’
Each molecule resembles two gold clubs twisted together
Each thick filament is surrounded by 6 thin filaments
Myosin heads will [later] form cross bridges with the thin filaments
Myofilaments = even small structures
A band - Dark band; overlapping thick & thin, filaments
I band - Light band; only contains thin (blue) filaments
H zone - The midsection of an A band; contains an M-line
Z disc (line) - The “ends” of the sarcomere
Midsection of the I band
M line- formed by protein myosin, place where myosin thick filament tails are connected
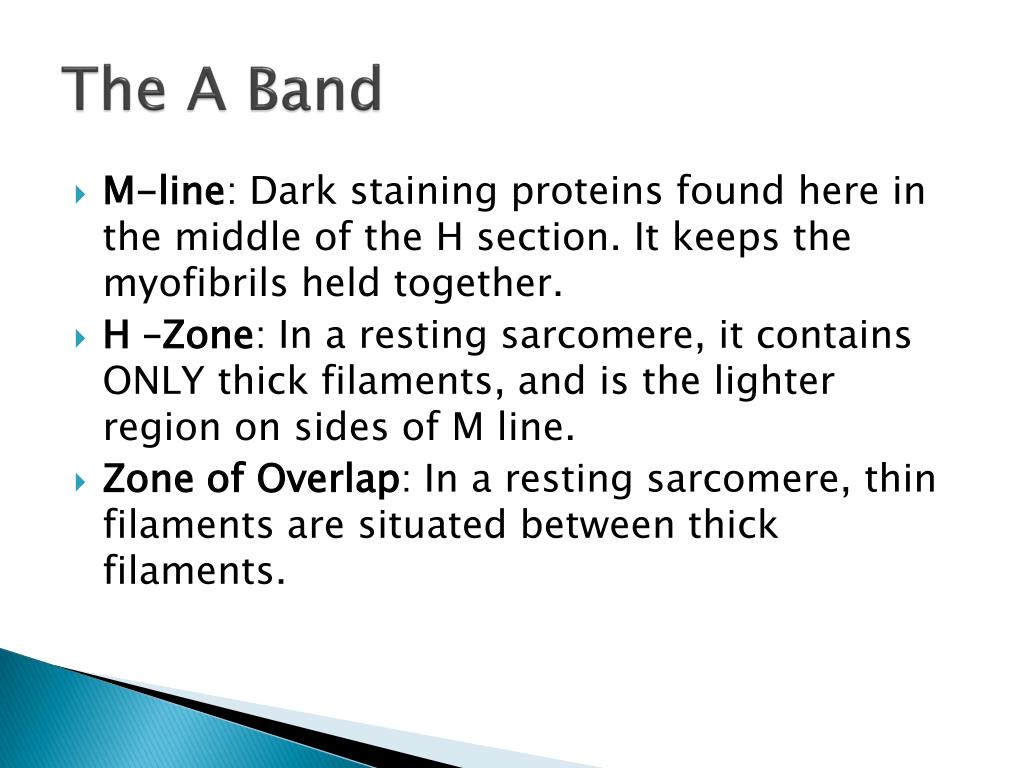
What comprises the A and I bands specifically?
Striations- are the overlapping arrangement of myofilaments and the repeating series of dark and light bands, which are evident along the length of each myofibril.
The intact muscle fiber, the dark ‘A’ bands, and light ‘I’ bands are nearly perfectly aligned, giving the cell its straited appearance.
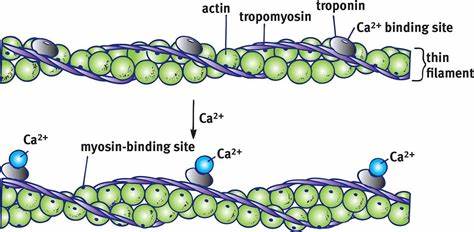
What are thick and thin filaments? What do troponin and tropomyosin do?
Two main types of myofilaments:
Thick filaments
Contain and are called myosin.
They extend across the entire length of ‘A band’
Each molecule resembles two gold clubs twisted together
Each thick filament is surrounded by 6 thin filaments
Myosin heads will [later] form cross bridges with the thin filaments
Thin filaments
Contain and are called actin
Extend across the entire length of ‘I band’ and partially into ‘A band’
Anchored by the ‘Z discs’
Remember z disc to Z disc is one sarcomere
Thin filaments are made of actin, troponin, & tropomyosin
The myosin-binding site on each actin molecule is covered by tropomyosin in relaxed muscle
Both troponin and tropomyosin help control the myosin-actin interactions involved in contraction.
Describe the molecular composition of thick and thin filaments.
Thick filaments
During contraction, they both form cross bridges and swivel around their point of attachment, acting as motors to generate force. Myosin itself splits ATP (acts as an ATPase) and uses the released energy to drive movement.
Contains about 300 myosin molecules bundled together, with their tails forming the central part of the thick filament and their heads facing outward at the end of each molecule
Thin filaments
Actin has kidney-shaped polypeptide subunits, called globular actin or G actin. Each G actin has a myosin-binding site (or active site) to which the myosin heads attach during contraction.
What is the sarcolemma?
the plasma membrane of a muscle cell
What are T-tubules and sarcoplasmic reticulum?
T-tubules -
channels that go into muscle cells and glue electrical impulses, release Ca2+, trigger muscle contraction
Sarcoplasmic Reticulum -
A system of tubular sacs similar to smooth ER in non-muscle cells that surround each myofibril (like the sleeve of a shirt) and stores Ca2+ in a relaxed muscle and later releases Ca2+ triggering muscle contraction
What is a sarcomere?
The smallest contractile unit of a muscle fiber (the functional unit)
The region between two successive Z-discs
Sarcomeres are aligned end-to-end to form a myofibril
What is the sliding filament theory and what are the six molecules essential for sarcomere contraction?
Thick and thin don’t change length, and the theory suggests that striated muscles contract through the overlapping of actin & myosin filaments, resulting in a shortening of the muscle fiber length.
The six molecules are:
Actin, Myosin, Trophonin, Tropomyosin, Calcium ions (Ca2+), and ATP
What is and what are the steps in excitation coupling (see page 293)?
series of events that link the action potential of the muscle cell membrane to muscular contraction
Step 1: The action potential (AP) propagates along the sarcolemma and down the T-tubules
Step 2: Calcium ions are released. Transmission of the AP along the T-tubules of triads causes the voltage-sensitive tubule proteins to change space. This shape change opens the Ca2+ release channels in the terminal cisterns of the sarcoplasmic reticulum (SR), allowing Ca2+ to flow into the cytosol.
Step 3: Calcium binds to troponin and removes the blocking action of tropomyosin. When Ca2+ binds, troponin changes shape, exposing myosin-binding sites on the thin filaments
Step 4: Contraction begins: Myosin binding to actin forms cross bridges and contraction (cross bridge cycling) begins, at this point, E-C coupling is over.
What is cross bridges?
form and break several times during a contraction, acting like tiny ratchets to generate tension and propel the thin filaments toward the center of the sarcomere
Formed between actin and myosin filaments
How does the sliding filament theory work - Describe the key events that lead to a cross bridge being formed?
Myosin binding sites attach to myosin binding sites on actin filaments which form cross bridges
thin filaments are pulled to the M-line
I bands shorten on the inside
contract together when you flex
z discs come toward each other
What is the neuromuscular junction and define ACh role in it?. Link the stages listed in Fig 9.7 to the pictures on page 290.
Neuromuscular junction - is the region where the motor neuron contacts the skeletal neuron. It consists of multiple axon terminals and the underlying junctional folds of the sarcolemma
ACh - (acetylcholine) - when a nerve impulse reaches a neuromuscular junction, it releases ACh. Upon binding to sarcolemma permeability leads to membrane potential.
What is a motor unit?
one somatic motor neuron & all the skeletal muscle cells (fibers) it stimulates
How are motor units recruited?
based on the motor unit size with smaller units recruited first
Motor units must be smaller (less fibers/nerve)
Easily excitable motor units – smallest muscle fibers (get activated first)
What is temporal summation?
two identical stimuli (electrical shocks or nerve impulses) are delivered to a muscle in rapid succession, the second twitch will be stronger than the first. On a myogram, the second twitch will appear to ride on the shoulders of the first
2nd contraction occurs before the 1st contraction is completely relaxed (Refractory period is only 5-10ms) muscle is already partially contracted, more calcium is being released (because another AP been generated) muscle tension produced during the second contraction is greater than the first. Essentially the contractions are summed or added together.
Define unfused/incomplete tetanus?
Stimulus is applied at an increasingly faster rate; relaxation time between twitches become shorter & shorter; increased Ca2+ presence in muscle
Results in a sustained but quivering contraction
Higher stimulation frequency results unfused tetanus
Define fused/complete tetanus?
Stimulus application to increase, maximal muscle tension is reached.
Results in a smooth, sustained contraction plateau
Infrequent in the real word; ‘superhuman strength’, situations
At even higher stimulus frequencies there is no relaxation at all between stimuli. This is fused (compete tetanus)
How is muscle force graded using the size principle of recruitment – see figures 9.13 and 9.14?
Muscle contractions can be graded in several ways:
1) Changing the frequency of the stimulus
2) Changing the strength of the stimulus
3) Motor unit size & recruitment
4) Fiber type
Regardless of what option is selected, the overriding principle that our body will select is based on the conservation of energy
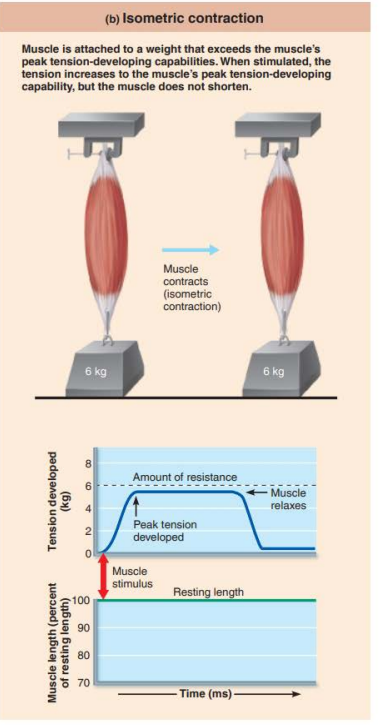
Describe the difference between isometric, concentric, eccentric contractions.
Concentric contraction = a muscle shortens to produce force and movement
Eccentric contractions = a muscle lengthens while maintaining force and movement
Isometric contraction = (same measure) no movement occurs
Tension is generated without muscle shortening
Maintain posture & support objects in a fixed position
What is the role of ATP in muscle contraction?
The role of ATP is that it supplies energy to move and detach cross bridges, operate the calcium pump in the SR, and operate the Na+, -K+ pump in the plasma membrane.
Because ATP is the only energy source used directly for contractile activities, it must be regenerated as fast as it is broken down if contraction is to continue.
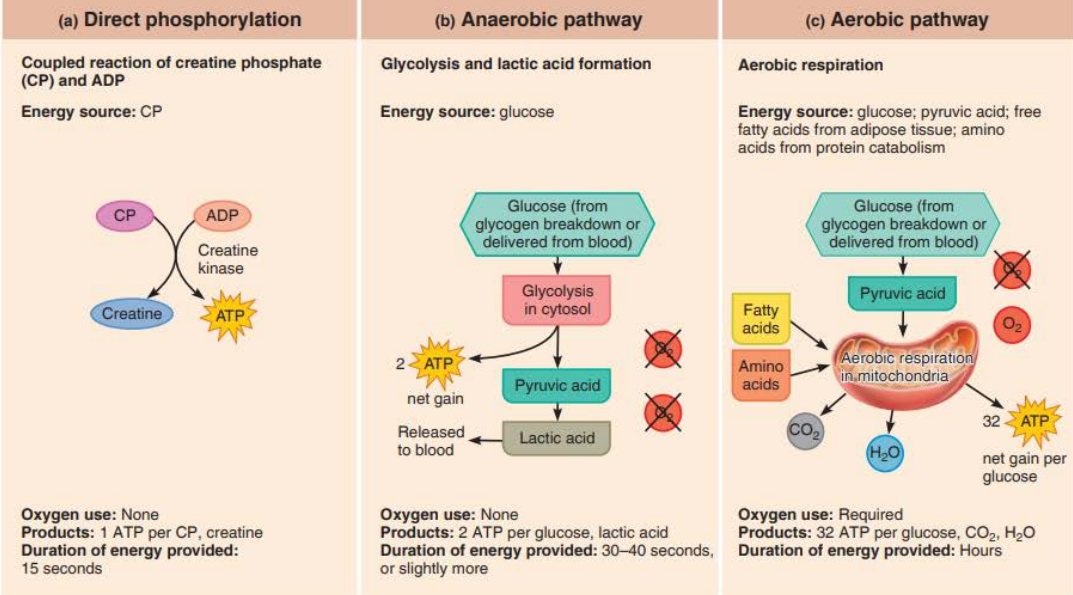
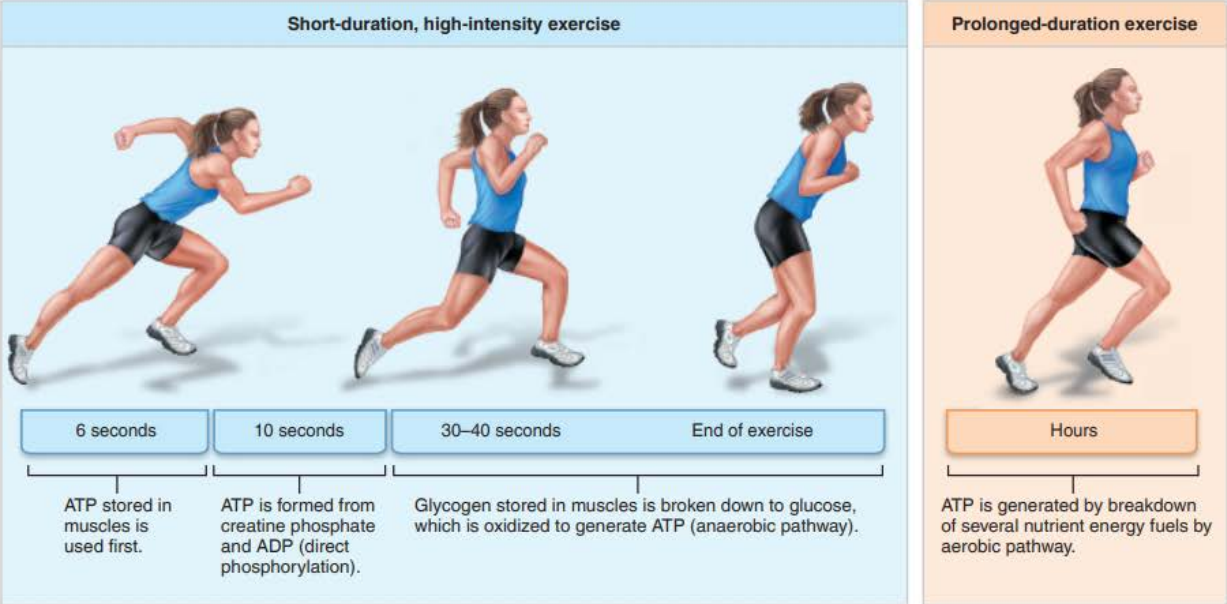
Describe major steps in direct phosphorylation, anaerobic pathway, aerobic pathway – figures 9.16 and 9.17.
Direct Phosphorylation
Coupled reaction of creatine phosphate (CP) and ADP
Energy source: CP
Oxygen use: NONE
Products: 1 ATP per CP, creatine
Duration of energy: 15 seconds
A unique high-energy molecule stored in muscles is topped to regenerate ATP while other metabolic pathways adjust to the sudden high demand for ATP
The fastest pathway
Anaerobic Pathway
Glycolysis and lactic acid formation
Energy source: glucose
Oxygen use: NONE
Products: 2 ATP per glucose, lactic acid
Duration of energy: 30-40 seconds
Aerobic Pathway
Energy source: glucose; pyruvic acid; free fatty acids from adipose tissue; amino acids from protein catabolism
Oxygen: Required
Products: 32 ATP per glucose CO2, and H2O
Duration: Hours
The slowest pathway
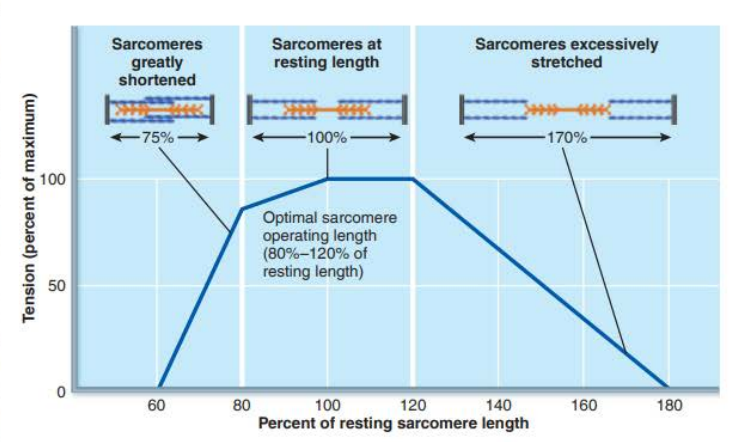
Describe length tension relationship of sarcomeres in skeletal muscle – figure 9.19.
Depends on the number of myosin cross bridges that are attached to actin
Number of muscle fibers recruited
More motor units, more force
Size of muscle fibers
Greater the cross-sectional area the more force it can produce
Hypertrophy - Regular resistance exercise increases muscle force by causing muscle cells to increase in size.
Frequency of stimulation
The higher the frequency, the more force (wave summation)
Degree of muscle stretch
Provides for optimal overlap of actin/myosin
80-120% of resting length
Increases & decreases reduce the ability to generate tension
What are slow fibers and fast fibers?
Slow twitch (slow oxidative) - which moves more slowly but helps to keep you moving longer
Red in color (lots of mitochondria, myoglobin, & blood vessels)
Resist fatigue, and sustained contractions to maintain posture
Endurance specialists relying on aerobic metabolism
Fast twitch (fast oxidative) - which helps move faster, but for shorter periods
Pink in color (lots of mitochondria, myoglobin, & blood vessels)
Spilt ATP at a very fast rate; contract quickly
What are oxidative fibers and glycolytic fibers?
Oxidative fibers -cells that rely mostly on the oxygen-using aerobic pathways for ATP generation
Glycolytic fibers - these fibers primarily create ATP through anaerobic glycolysis resulting in less ATP per cycle. As a result, they fatigue more rapidly. (Quick, but tire out faster)
Understand how skeletal muscles differ from smooth and cardiac about the presence of myofibrils, t-tubules, regulation of contraction, site of calcium regulation, speed of contraction, and metabolism.
Body of Location (Smooth) - unitary muscle in walls of hollow visceral organs (other than the heart); multi-unit muscle in intrinsic eye muscles, airways, and large arteries
_____
Prescence of myofibrils
Cardiac - Yes, but myofibrils are of irregular thickness
Smooth - No, but actin and myosin filaments are present throughout; dense bodies anchor actin filaments
________
Presence of T-tubules
Cardiac - Yes; one per sarcomere at Z disc; larger diameter than those of skeletal muscle
Smooth - No; only caveolae
________
Regulation of contraction
Cardiac - Involuntary; contraction initiated by intrinsic pacemaker cells; regulated by autonomic nervous system, hormones, and stretch
Smooth - Involuntary; initiated by intrinsic pacemaker cells (in unitary muscle) or autonomic nerves (in multi-unit muscle) regulated by local chemicals, hormones, and stretch
Site of calcium regulation
Cardiac - Troponin on actin-containing thin filaments
Smooth - calmodulin in the cytosol
_____________________________________________________
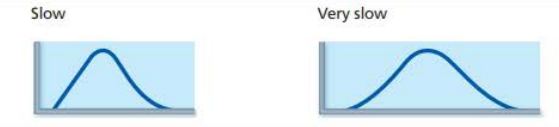
Speed of Contraction
Cardiac - Slow
Smooth - Very Slow
___________________________________________________
Metabolism
Cardiac - Aerobic
Smooth - Mainly aerobic
Define muscular dystrophy
Refers to a group of genetic diseases that cause progressive weakness and degeneration of skeletal muscles.
trouble using arms
trouble walking
frequent falls
How does muscular system help: integumentary system, endocrine system, digestive system.
Integumentary System
Muscular exercise enhances circulation to skin and improves skin health
Skin protects the muscles by external enclosure; helps dissipate heat generated by the muscles
Endocrine System
Growth hormone and androgens influence skeletal muscle strength and mass; other hormones help regulate cardiac and smooth muscle activity
Digestive System
Physical activity increases gastrointestinal motility; skeletal muscle forms the voluntary sphincter of the anus
Digestive system provides nutrients needed for muscle health; liver metabolizes lactic acid
CH 11
Understand the biology of addiction
the dopamine you get from the drug makes you want to keep doing it, once you don’t have it you keep it doing it the same way so addiction
Define sensory input, integration, motor output of the nervous system
Controls and integrates all body activities that maintain life
Three “overlapping” functions:
Sensory input - Sensory receptors monitor internal/external changes
Integration - Process and interpret the input information
Motor output- Responds to the change
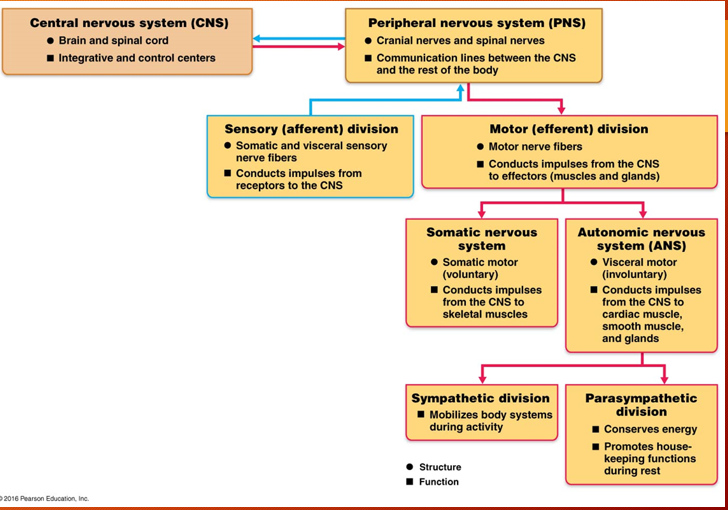
What is the major organization and what are the major divisions of the CNS and PNS – Figure 11.3
Central Nervous System (CNS) – occupies the dorsal body cavity. Interprets sensory input and dictates motor output based on reflexes, current conditions, and experience
Brain
Spinal Cord
Peripheral Nervous System (PNS) – outside of CNS, consists of nerves that extend from the brain and spinal cord and ganglia
Spinal nerves – carry impulses to and from the spinal cord
Cranial nerves - carry impulses to and from the brain
Ganglia – collections of neuron cell bodies
Functional divisions of the Peripheral Nervous System (PNS) include:
Sensory (afferent)
Transmits signals/input towards the CNS
Motor (efferent)
Transmits signals away from the CNS
Two motor divisions:
Somatic nervous system – skeletal muscles, voluntary
Autonomic Nervous System (ANS) – involuntary, cardiac muscle, smooth muscle, and glands
The ANS itself has two branches:
Sympathetic Nervous System: Prepares the body for “fight or flight” responses.
Parasympathetic Nervous System: Promotes relaxation and conserves energy.
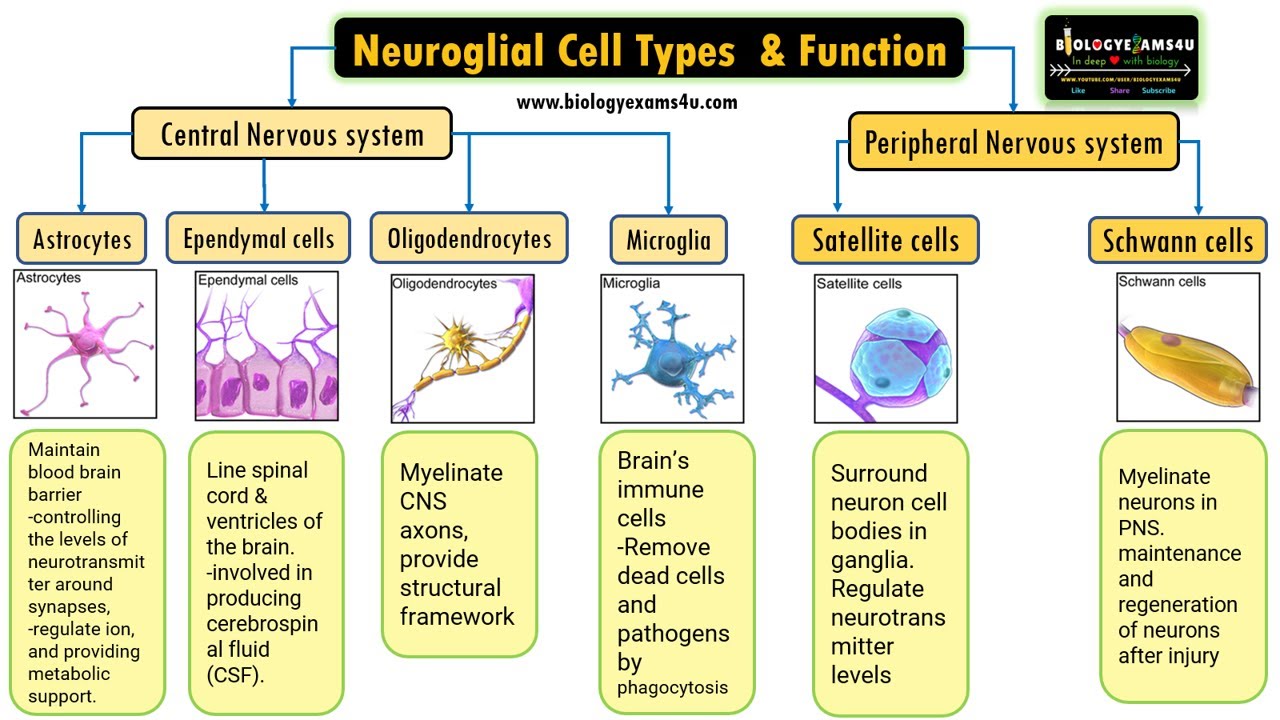
What are the functions of the neuroglia in the CNS; astrocytes, microglial cells, ependymal cells, oligiodendrocytes
Astrocytes
Functions:
Star-shaped
Most abundant
Hold neurons in place
Link neuron with capillary
‘Mop up’ leaked potassium ions and recapture and recycle neurotransmitters
Microglia
Thorny processes
Monitor the health of neuron(s)
Phagocytize microorganisms or neural debris after injury
Protective role is important because the immune system has limited access to the CNS
Ependymal cells
“Wrapping garment”
Line cavities of the brain and spinal cord
Cilia-movement of cerebrospinal fluid in cavities
Can be squamous or columnar, and many are ciliated
Line the central cavities of the brain and spinal cord
Cilia help circulate CSF
Oligodendrocytes
Wrap CNS nerve fibers
Wrap their processes around CNS neurons
Produce covering called myelin sheath
What are the functions of the neuroglia in the PNS; satellite cells, schwann cells
Satellite cells – named for their moon-like appearance
Function similar to astrocytes of the CNS
Supporting/bracing/communication between neurons and nearby capillaries
Schwann cells
Similar to oligodendrocytes of the CNS
Surround and form myelin sheaths around peripheral nerve fibers
What are neurons and what are their major structural components – Figure 11.3
Neurons (nerve cells) = structural units in the nervous system
Receive/transmit messages in the form of nerve impulses
Three characteristics of neurons
Extreme longevity
Amitotic - lost their ability to divide
High metabolic rate - need abundant supplies of O2 and glucose
Axon - Transmits signals away from the cell body
Cell body- Spherical nucleus: biosynthetic center (control center) houses normal organelle located in cell cytoplasm to make proteins and other chemicals
Dendrites- Receive signals entering the cell body
Lots of Rough ER (called Chromatophilic substance)
Most cell bodies are located in the CNS where they are protected by the bones of the skull and vertebral column
Clusters of cell bodies in the CNS = nuclei
Clusters of cell bodies in the PNS = ganglia
What is myelination of the PNS, how does it form and why is it important?
Myelination - is a crucial process in the nervous system PNS
Refers to the formation of a myelin sheath around neuronal axons
Myelin sheaths are composed of lipids & proteins and has a whitish appearance
It consists of many concentric layers of plasma membrane, creating a protective covering around the axons
Schwann cells play a crucial role
They wrap around large-caliber axons forming the myelin sheath
Schwann cells insulate axons, allowing for rapid conduction of nerve impulses
The smallest-diameter axon are nonmyelinated.
These nonmyelinated axons are covered by the long extensions of adjacent glial cells
What is myelination of the CNS called, why is it important?
can greatly increase the speed of signals transmitted between neurons
Oligodendrocytes – from myelin sheaths
White matter:
Regions in brain/spinal cord containing dense collections of myelinated fibers
Gray matter:
Regions of CNS containing mostly cell bodies and unmyelinated fibers
Multiple Sclerosis (MS)
An acquired inflammatory demyelinating disorder affecting the CNS
What are the functions of the sensory afferent neurons?
transmit impulses from sensory receptors in the skin or internal organs toward or into the CNS
bringing sensory information from the outside world into the brain
detecting and responding to external signals
virtually all sensory neurons are unipolar, and their cell bodies are located in sensory ganglia outside the CNS
What are the functions of the motor efferent neurons?
carry impulses away from the CNS to the effector organs (muscles & glands) of the body
Motor neurons are multipolar
Expect for some neurons of the autonomic nervous system, their cell bodies are located in the CNS
What are ion channels; what are ligand gated channels, voltage gated channels, mechanically gated channels?
Ion channels - which allows ions to pass through channel pore including sodium, potassium, calcium, and chloride ions to pass through the impermeant lipid cell membrane
Ligand-gated channels - (chemically gated channels) - open when the appropriate chemical (in this case a neurotransmitter) binds
Voltage-gated channels - open & close in response to changes in the membrane potential
Mechanically gated channels - open in response to physical deformation of the receptor (as in sensory receptors for touch and pressure)
What is the sodium potassium pump and what does it do – pg 400
is a transmembrane protein pump that transports sodium & potassium ions across the cell membrane
The pump uses ATP to move 3 sodium ions out of the cell and two potassium ions into the cell
this creates a concentration gradient of sodium & potassium ions which helps, establish the resting membrane potential of cells, especially neurons
What is a neuron membrane potential – Figure 11.8; how does it change in depolarization, hyperpolarization and what is the physiology of this potential?
the potential difference between an electrode inside a neuron and the ground electrode in the extracellular fluid is approximately -70mV (inside negative)
Depolarization - is a decrease in the membrane potential. The inside of the membrane becomes less negative (moves closer to zero) than the resting potential.
Hyperpolarization - is an increase in membrane potential: the inside of the membrane becomes more negative (moves farther) than the resting potential.
A resting (non-signaling) neuron has a voltage across its membrane called the resting membrane potential. Is determined by concentration gradients of ions across the membrane and by membrane permeability to each type of ion.
What is salutatory conduction; why is it important?
Saltire = ‘to leap’ (30 times faster)
AP’s generated at gaps in myelin sheath
They appear to jump rapidly
Myelin prevents almost all charge from leaking from the axon and allows the membrane voltage to change more rapidly
Saves energy by decreasing the use of sodium-potassium pumps in the use of sodium-potassium pumps in the axonal membrane. It also increases the speed of conduction, allowing the organism to react and think faster.
What are the three axo- synapses – fig 11.16
Axodendritic synapses - are the most common types of synapses
They occur between the axon terminal of one neuron and the dendrite of another neuron
Allow for communication & signal transmission between neurons
Axosomatic synapse - occurs between the axon terminal of one neuron and the cell body soma of another neuron
These synapses can influence the overall excitability of the post-synaptic neuron
Play a role in regulating neuronal firing and maintaining homeostasis
Axoaxonic synapse - between the axon terminal of one neuron and the axon of another neuron
These play a regulatory role by modulating neurotransmitter release
They can enhance or inhibit the release of neurotransmitters from the pre-synaptic neuron
Axoaxonic synapses are found throughout the CNS, including in the hippocampus, cerebral cortex, and stratum in mammals
How does ACh work across NMJ synapses? Pg 410 and Fig 11.3
ACh crosses the synaptic gap and binds to ACh receptors tightly clustered on the surface of the muscle fiber; this leads to the endplate potential (EPP) which initiates the muscle action potential that results in muscle contraction
Reabsorbed & recycled ready to transmit another chemical message
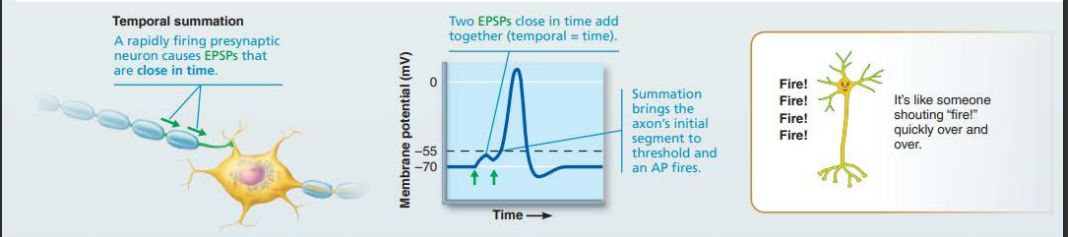
What is temporal summation?
A rapidly firing presynaptic neuron causes EPSPs that are close in time.
From Table 11.3, pg 419-420 - What are neurotransmitters and what are the major functions of the following neurotransmitters:
Glutamate
Dopamine
Serotonin
Histamine
Endorphins
Norepinephrine
Epinephrine
ACh
Neurotransmitters - are your body’s chemical messengers. They play a crucial role in transmitting signals from nerve cells to target cells, which can be other nerve cells, muscle cells, or glands cells.
Cell body: Vital for producing neurotransmitters and maintaining nerve cell function
Axon: Carries electrical signals along the nerve cell to the axon terminal
Axon terminal: where the electrical message is converted to a chemical signal using neurotransmitters
Glutamate: generally excitatory; direct action (dedicated to learning & memory)
Dopamine: feel good or motivational drive
Serotonin: mainly inhibitory; stabilizing mood, and plays a role in sleep, appetite, nausea, and migraine headaches
Drugs that block its uptake relieve anxiety and depression.
Histamine: excitatory or inhibitory depending on receptor type bound; accelerating heart rate, and acting as the brain, spinal cord, and uterus
Endorphins: generally inhibitory; relieve pain, reduce stress
Norepinephrine (NE): excitatory or inhibitory; increasing alertness, arousal, and attention
Epinephrine: or adrenaline is a hormone and a neurotransmitter that boosts your heart rate, blood pressure, and energy in stressful situations
ACh: acts at two classes of receptors: nicotinic and muscarinic
regulates the levels of other neurotransmitters in the brain
What is a neurotoxin and what is neuropathy?
Neurotoxin - substance that is poisonous or destructive to nervous tissue, eg. botulinum & tetanus toxins
Neuropathy - any disease of nervous tissue, but particularly degenerative diseases of nerves