Pathogenesis (How Microbes Cause Disease)
1/18
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
19 Terms
What is pathogenesis?*
A biological mechanism or mechanisms that leads to disease
What is pathogenicity?
The ability of an organism to cause disease
What is Virulence? What are pathogenic determinants? *
Degree of pathogenicity
Attributes of bacteria or viruses that enable or enhance their ability to cause disease
What is an Infection?*
The invasion of the host by disease-causing microorganisms

How does a microorganism cause disease?*
Virulence Factors*
Must gain access to a host
Adherence to host cells
Penetrate/evade immune response
Damage host cells and tissue
Exotoxins
A-B toxins, membrane-disrupting toxins, superantigens, and genotoxins
Exit portals
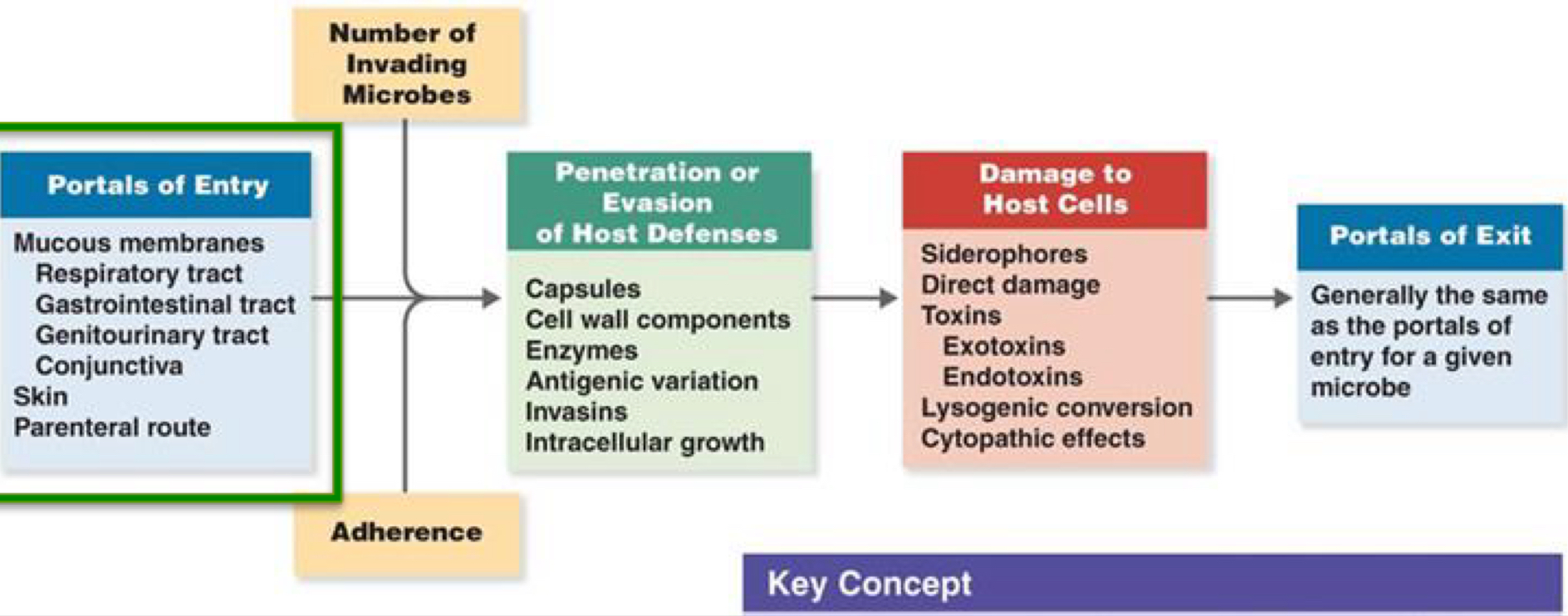
Adherence*
Means by which pathogens attach themselves to host tissue
Necessary for pathogenicity
Surface molecules on pathogens that bind to receptors on host cells are called adhesins
Glycoproteins or lipoproteins
Usually binds to sugars on host cells like mannose
Adhesins include:
Pili
Capsules
Cell wall components
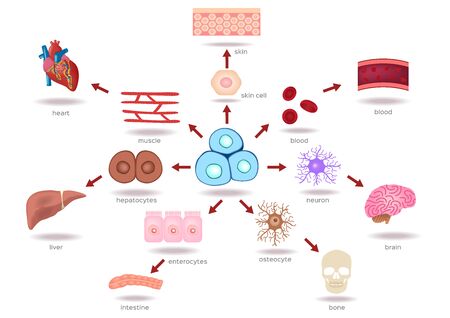
Penetration into Host Cell*
Bacteria attach to host cells by using adhesins
Produce surface proteins called invasins that promote bacteria entering into host cell
Evade Immune Responses/Defenses*
Capsules*: Escape phagocytosis
Cell wall components:
M protein* -
Cell wall of S. pyogenes
Mediates attachment and helps evade phagocytosis
M - mutants are unable to avoid phagocytosis and can’t survive in host
Opa protein* -
Outer membrane of N. gonorrhoeae
Attachment/internalization by host cells
Inhibit T cell proliferation and activation
Mycolic Acid* -
Mycobacterium tuberculosis, waxy cell wall allows it to avoid digestion by phagocytosis and can multiply inside phagocytes
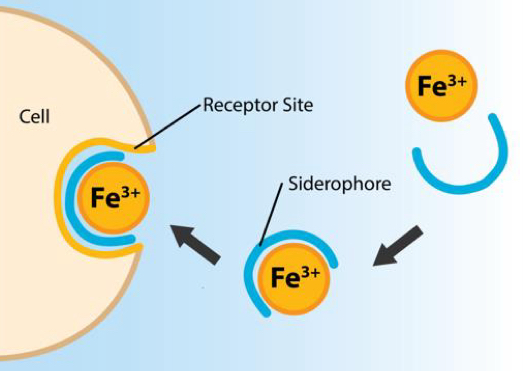
How Bacterial Pathogens Damage Host Cells*
Using host nutrients
Siderophores* - sequestering iron away from host proteins, like hemoglobin
Direct interaction with iron-transport protein
Causing direct damage in the area of infection
Uses host cells as a source of nutrients and produces waste products
Inducing hypersensitivity - damaging body cells, too high of a temp.
Producing toxins
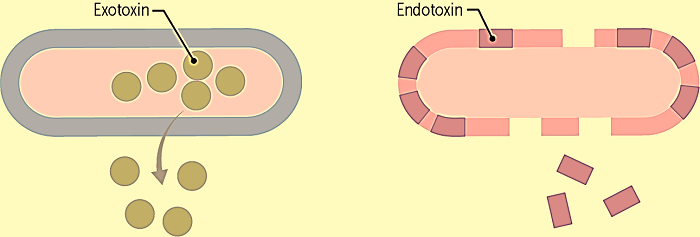
Exotoxins* -
Proteins produced inside a pathogen that is secreted into surrounding or released by lysis
Genes often carried on plasmids or phages
Work by affecting particular aspects of host cells and/or host metabolic pathway
Endotoxins* -
Lipid proteins (lipid A) of lipopolysaccharides that are part of the outer membrane of gram (-) bacteria. These are released when bacteria die, and the cells lyse
Exotoxins Continued*
Diseases caused by bacteria that produce exotoxins are often caused by the exotoxin itself, not the bacteria
The body produces antibodies against toxins called antitoxins
Exotoxins inactivated by heat or chemicals called toxoids can be used to vaccinate to stimulate antitoxin production
Tetanus and diphtheria vaccines
Types of Exotoxins:
A-B toxins -
Most exotoxins
A is the active part, B is the binding component
diphtheria toxin, cholera toxin
Membrane disrupting toxins -
Cause lysis of host cell by disrupting their plasma membrane
Aids bacteria escape from sacs within phagocytes
hemolysins, leukocidins
Superantigens -
Provoke a very intense immune response
Nonspecifically stimulates proliferation of T cells
Release enormous amounts of cytokines
Fever, nausea, vomitting, shock
S. aureus
Genotoxins -
Damage DNA
Causes mutation and may lead to cancer
Portals of Exit*
Respiratory Tract
Coughing, sneezing
Gastrointestinal tract
Feces, saliva
Genitourinary tract
Urine, vaginal secretions
Skin
Blood
Biting arthropods, needles/syringes

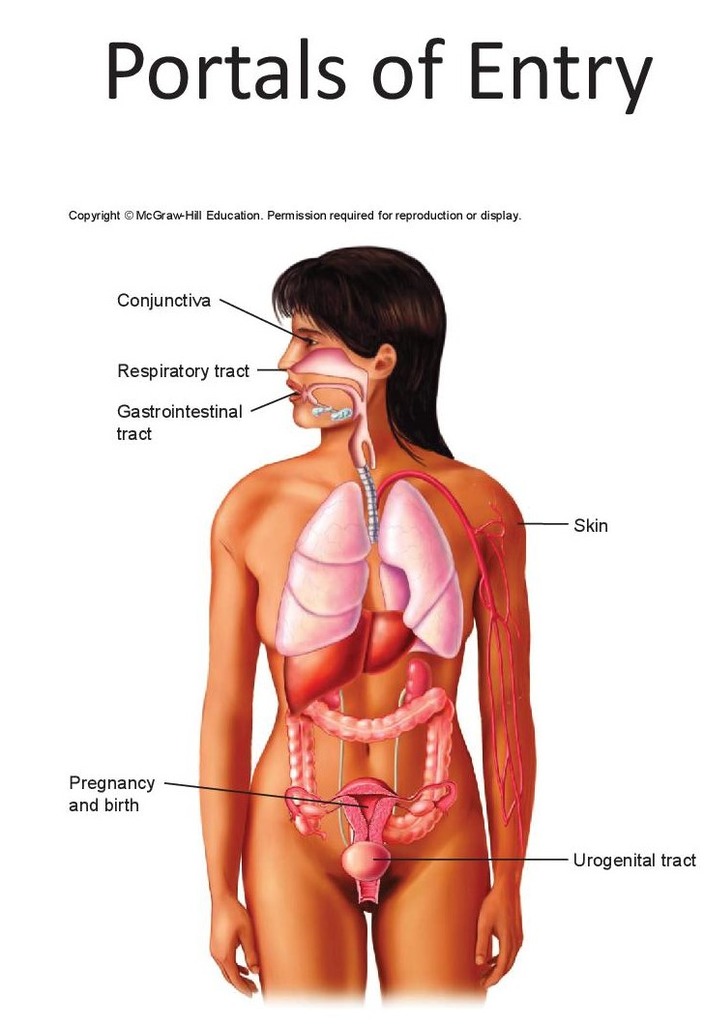
Portals of Entry*
Mucous Membranes
Gastrointestinal tract
Respiratory tract
Genitourinary tract
Conjunctiva
Skin
Unbroken = Impenetrable, to most organisms
Some microbes can gain access through openings in the skin such as hair follicles
Parenteral route
Directly deposited into the tissue beneath the skin or mucous membrane due to cuts, injections, bites, and surgery
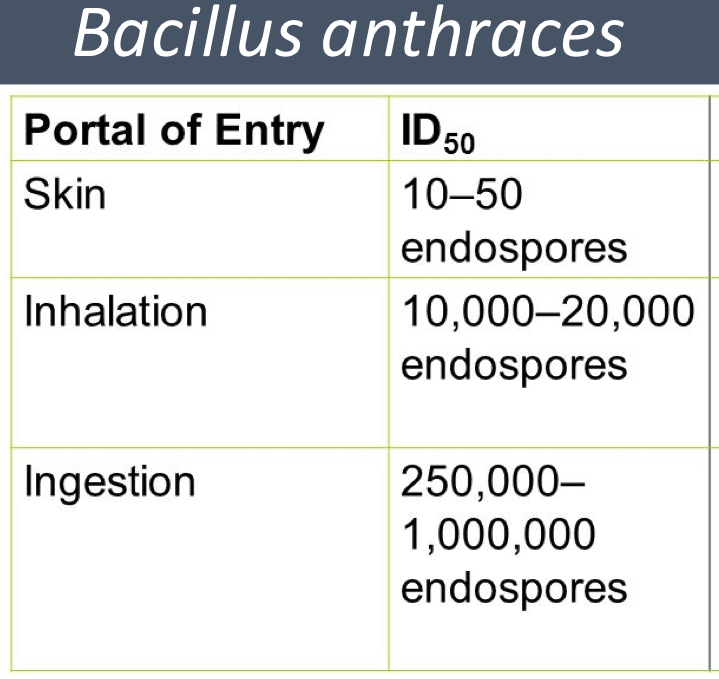
Numbers of Invading Microbes
Generally, if only a few microorganisms enter, not much happens
The more that get in = better chance of causing disease
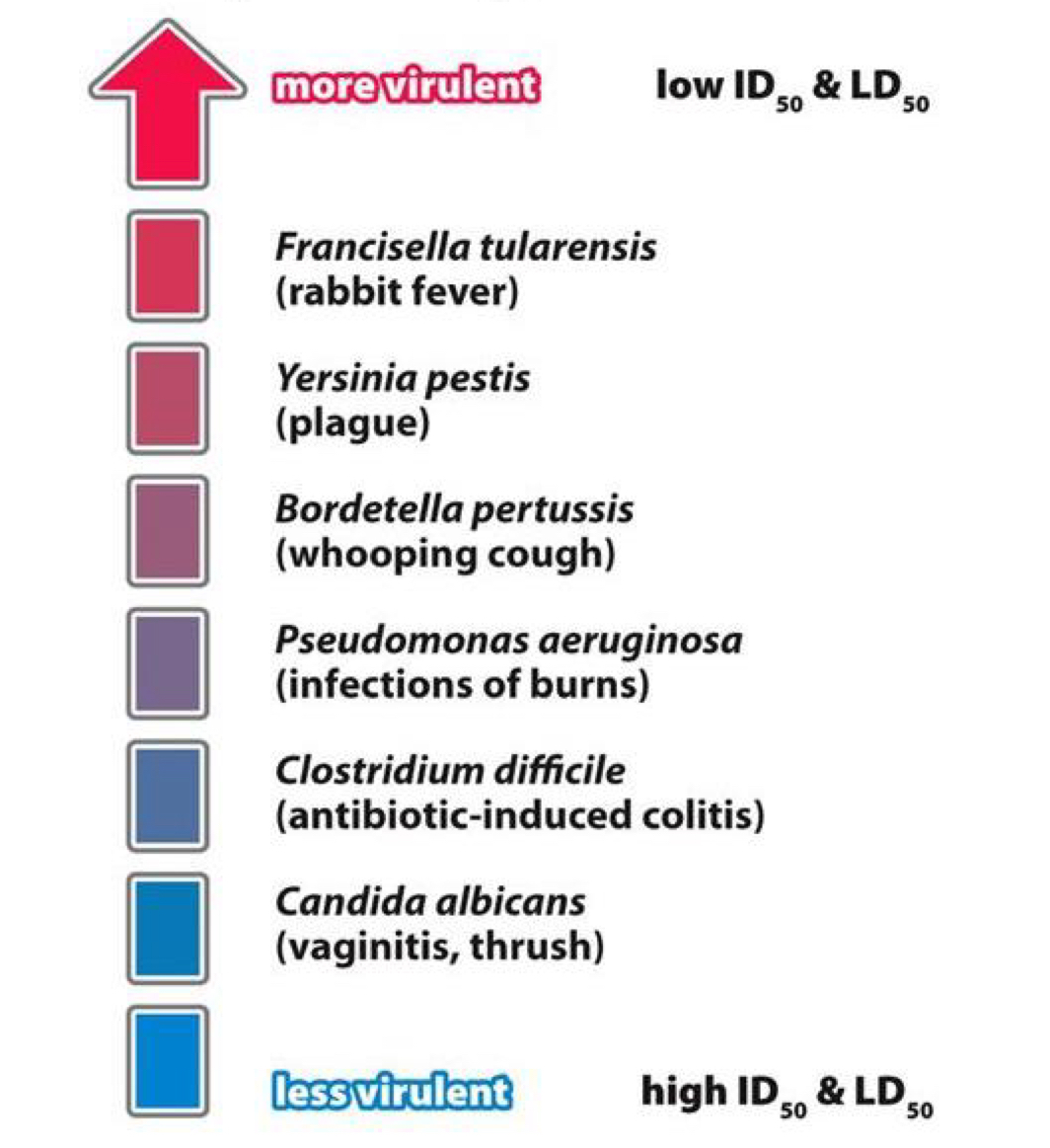
We measure these to determine the virulence of pathogens
Quantitatively: ID50 and LD50
ID50*
The dose that causes disease in 50% of the population
Used to compare relative virulence under defined conditions
LD50*
The dose that kills 50% of the population within a certain time
Usually, toxic agents
Botulism toxin
Shiga toxin
Defined conditions
Lower # = more toxic
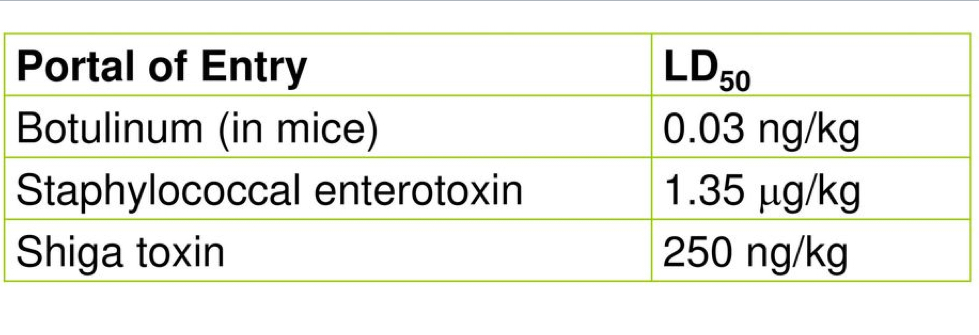
ID50 & LD50 (Virulence)*
Enzymes/Exoenzymes
Bacteria produce exoenzymes that aid in virulence
Coagulase - Clot Fibrinogen in blood, may protect bacteria from phagocytosis + other cellular defense mechanisms
Kinases - Breaks clots formed by the body to isolate and contain bacteria and allow it to extend infection
IgA Protease - Chops/cleaves up antibodies
Collagenases - Breaks down connective tissue of muscles and tissues, facilitating the spread of the bacteria
Act over and over again, so small amounts are harmful
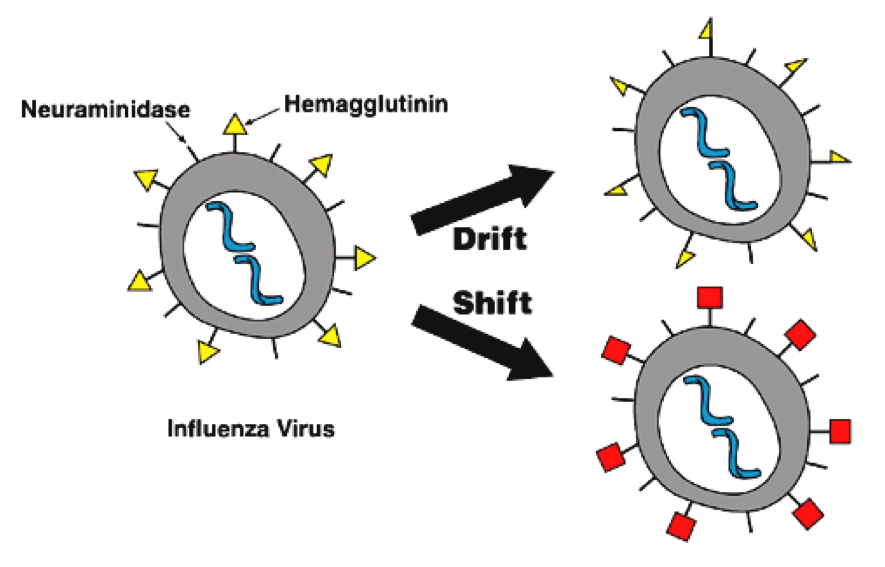
Antigenic Variation
Pathogens can alter their surface proteins by a process called antigenic variation
By the time the body mounts an immune response, the pathogen has already altered its antigen
Influenza virus
N. gonorrhoeae
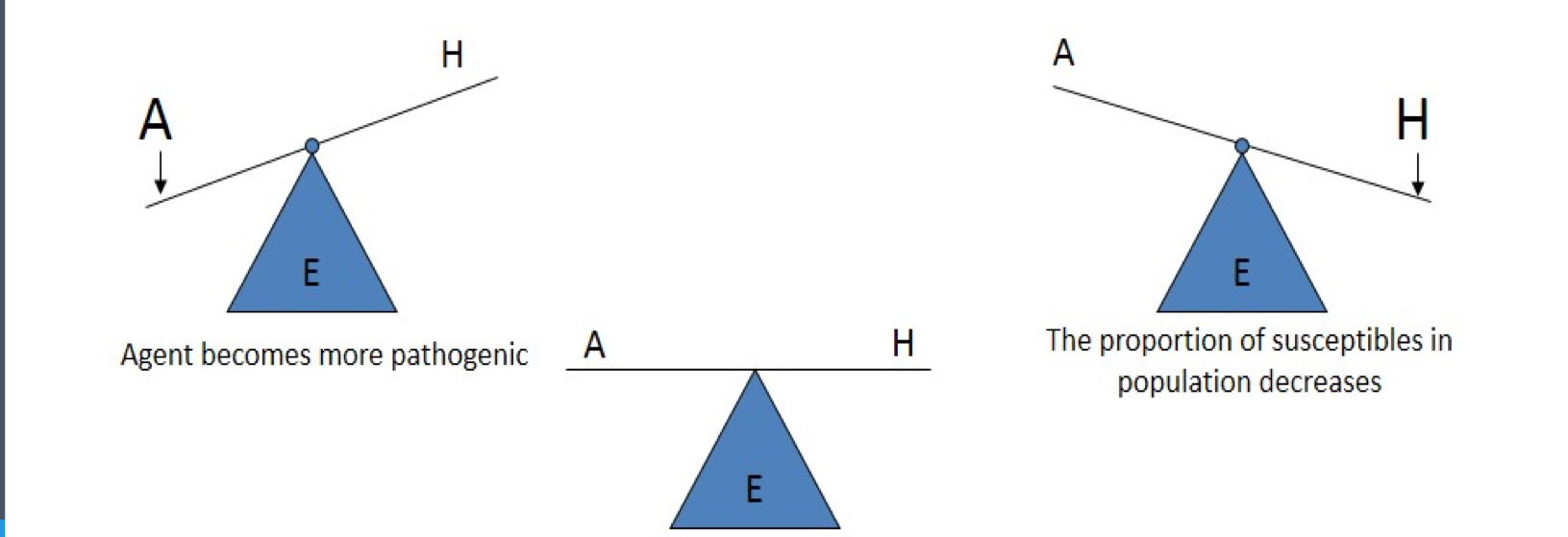
Etiology*
The Triad
Disease agent
Susceptible host
Environment that brings host and agent together
Out of balance = get disease
Disease results from the interaction between the agent and susceptible host in an environment that supports transmission of the agent from a source to that host