BIOMETRICS and NUTRITION
1/85
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
86 Terms
Fasting plasma glucose normal:
<100 is normal;
Body Mass Index (BMI)
Underweight:
<18.5
Body Mass Index (BMI) Normal/Healthy Weight:
18.5-24.9
Body Mass Index (BMI) Overweight:
25.0-29.9
Body Mass Index (BMI) Obese
≥30.0
Waist Circumference
Elevated cardiometabolic risk women:
Women ≥35 inches (88 cm)
Waist Circumference
Elevated cardiometabolic risk men:
Men ≥40 inches (102 cm)
Blood Pressure (mmHg)
Normal:
<120 systolic / <80 diastolic
Blood Pressure (mmHg)
Elevated:
120-129 systolic / <80 diastolic
Blood Pressure (mmHg)
Hypertension Stage 1:
130-139 systolic or 80-89 diastolic
3 multiple choice options
Blood Pressure (mmHg)
Hypertension Stage 2:
≥140 systolic or ≥90 diastolic
Lipid Panel (mg/dL)
Total Cholesterol: desirable
<200 desirable
LDL (“bad” cholesterol) Optimal:
<100 optimal for most people (some guidelines say <130 is near‐optimal; <70 may be a target for people at high risk)
HDL (“good” cholesterol) Men:
Men: >40 (higher is better)
HDL (“good” cholesterol) Women:
Women: >50 (higher is better)
3 multiple choice options
Triglycerides:considered normal
<150
Fasting plasma glucose prediabetes:
100-125
Fasting plasma glucose diabetes:
≥126 is diabetes (diag)nostic
Normal Hemoglobin A1C:
<5.7%
Prediabetes Hemoglobin A1C:
5.7%-6.4%
Diabetes Hemoglobin A1C:
≥6.5%
Body Composition
Body fat percentage values vary by age, gender, and reference source. For most women:
Healthy range (women): roughly 18–28%
Body Composition
Body fat percentage values vary by age, gender, and reference source. For most men:
Healthy range (men): roughly 10–20%
Physical Activity Guidelines (though not exactly a “biometric,” coaches are generally expected to know them)
For healthy adults, at least 150 minutes/week of moderate‐intensity aerobic activity, or 75 minutes/week of vigorous aerobic activity, plus muscle‐strengthening exercises on 2 or more days per week.
Resting heart rate: typical range
60-100 beats per minute in adults (lower for some highly fit individuals).
Metabolic Syndrome Criteria:
Three or more [waist circumference Men: ≥102 cm (≥40 inches) Women: ≥88 cm (≥35 inches)], [blood pressure Systolic blood pressure (SBP): ≥130 mmHg / Diastolic blood pressure (DBP): ≥85 mmHg] [triglycerides, ≥150 mg/dL (1.7 mmol/L)] [HDL Men: <40 mg/dL (1.03 mmol/L) / Women: <50 mg/dL (1.29 mmol/L)], and [fasting glucose ≥100 mg/dL or on medication for elevated glucose) heightened cardiovascular/metabolic risk.
High-Sensitivity C-Reactive Protein (hs-CRP)
Though less standard in basic panels, hs-CRP is sometimes mentioned as a marker of inflammation and cardiovascular disease risk. You should be aware that elevated CRP (>3.0 mg/L) may indicate higher risk, but coaches do not interpret or diagnose from these labs.
Bone Density Screenings (DEXA Scan):
Osteoporosis risk and bone health can appear in exam scenarios. NBHWC coaches would not diagnose from DEXA results but should know bone density screenings are advised in older adults (e.g., women ≥65 years old or those at risk).
Physical Activity Readiness:
Standard risk stratification or readiness questionnaires (such as PAR-Q+) can be part of a coach's knowledge in exercise contexts (though the emphasis is often on whether to refer for medical clearance if risk factors are high).
Mammograms (Breast Cancer Screening) Starting Age:
Historically, many guidelines suggested age 40 or 50 as a start point. Recently, some recommendations have shifted to encourage most women to begin at age 40.
Mammograms (Breast Cancer Screening) Frequency:
Usually every 1 to 2 years once screening has begun.
Mammograms (Breast Cancer Screening) Ending Age:
Often continued until about age 74, but may be individualized after discussion with a healthcare provider.
Cervical Cancer Screening (Pap Smear / HPV Test)
Ages 21–29: A Pap test every 3 years, assuming normal results. HPV testing is not routinely recommended as a standalone test in this younger group.
Ages 30–65: EitherPap test every 3 years, orPap test plus HPV co-testing every 5 years, orHPV test alone every 5 years (depending on the latest guidelines and available tests).
Over 65: Some guidelines say women may discontinue cervical screening if they have had several consecutive normal tests and no high-risk history.
After hysterectomy: Screening may be discontinued if the hysterectomy was for benign reasons and there is no cervical cancer history, but only with provider confirmation.
Colorectal Cancer Screening
Starting Age: Often age 45 (recently updated from 50 by USPSTF for average-risk adults), though some organizations still list 50.
Frequency and Method:Colonoscopy every 10 years (often considered the “gold standard”).Other methods (such as fecal immunochemical test annually, stool DNA test every 3 years, or flexible sigmoidoscopy every 5 years) are also accepted in certain guidelines.
Ending Age: Often age 75 for routine screening, but may be individualized up to age 85 depending on overall health.
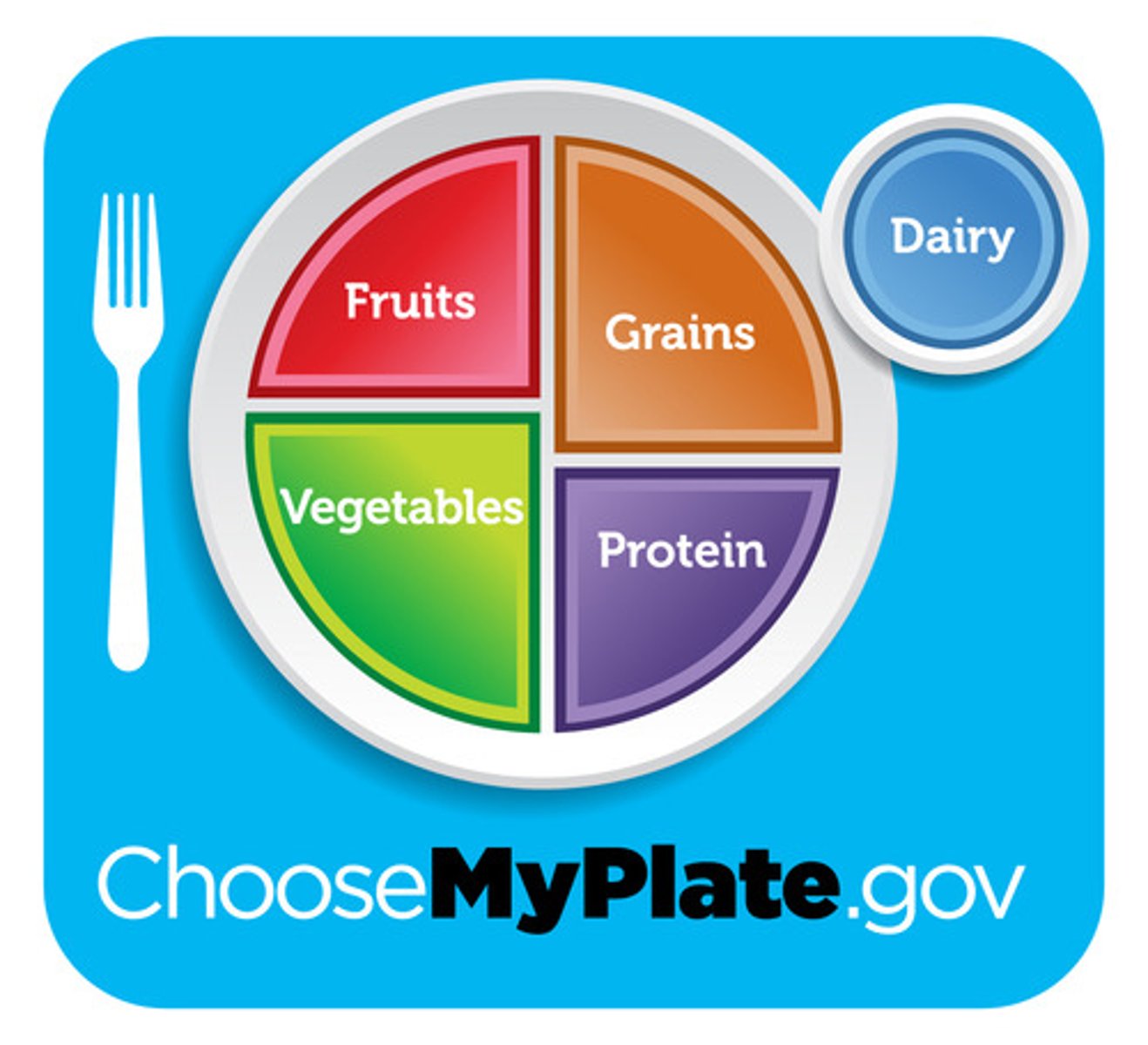
MyPlate Five Core Food Groups.
Fruits, Vegetables, Grains, Protein, and Dairy
Roughly half your plate is
fruits and veggies (slightly more veggies than fruits).
50% Fruits & Vegetables
25% Grains
25% Protein
My plate proportions
Fruits Recommended Amount:
~2 cups per day for many adults.
What Counts as a Cup?1 cup fresh/frozen/canned fruit1 cup 100% fruit juice½ cup dried fruit
What counts as a cup of fruit?
1 cup fresh/frozen/canned fruit
1 cup 100% fruit juice
½ cup dried fruit
Vegetables Recommended Amount:
~2½ cups per day for adults
What counts as a cup of vegetables?
1 cup raw or cooked vegetables
1 cup vegetable juice (100%)
2 cups raw leafy greens = 1 cup of vegetables
Grains Recommended Amount:
~6 "ounce-equivalents" (oz-eq) per day for many adults.
What counts are 6 ounce equivalents of grains?
What’s an Ounce-Equivalent?
1 slice bread
1 cup ready-to-eat cereal
½ cup cooked pasta or rice
½ cup cooked oatmeal
Protein Recommended Amount:
~5½ oz-eq per day for many adults.
What’s an Ounce-Equivalent of protein?
1 oz lean meat, poultry, or fish
1 egg
¼ cup cooked beans or tofu
1 Tbsp peanut butter
½ oz nuts or seeds
MyPlate Advice Healthy Fats and Oils
MyPlate doesn't emphasize oils as a formal "food group" but recommends moderate use of plant-based oils (e.g., olive, canola) and limiting saturated/trans fats.
Typical daily allowance might be ~5-6 teaspoons of oil for an adult (depending on total calories).
MyPlate on added sugars, sodium and saturated fats:
Limit Added Sugars, Sodium, and Saturated Fats
Aim for <10% of daily calories from added sugars.
Aim for <10% of daily calories from saturated fat.
Keep sodium intake under 2,300 mg/day (and even lower if recommended by your healthcare provider).
Key Features of this nutrition style:
Emphasizes fruits, vegetables, legumes, whole grains, nuts/seeds, and olive oil (as the primary fat).
Moderate intake of fish and poultry; limited red meat.
Uses herbs/spices for flavor instead of excess salt.
Encourages moderate consumption of dairy (often yogurt or cheese) and red wine (optional, typically with meals). Associated with reduced risk of heart disease, certain cancers, Type 2 diabetes, and cognitive decline.
Mediterranean Diet
Key Features of this nutrition style:
Focuses on fruits, vegetables, whole grains, low-fat dairy, lean protein (fish, poultry, beans).
Low in saturated fat, cholesterol, and total fat.
Encourages reducing sodium intake, typically aiming for <2,300 mg/day (some guidelines recommend 1,500 mg/day for hypertension).Shown to help lower blood pressure, improve heart health, and support weight management.
DASH Diet (Dietary Approaches to Stop Hypertension)
Key Features of this nutrition style:Centered on foods of plant origin (fruits, vegetables, grains, legumes, seeds, nuts).May or may not include animal products; e.g., vegetarian (may include eggs/dairy) vs. vegan (excludes all animal products).
Evidence:Potential benefits for cardiovascular health, weight management, and lowering risk of some chronic diseases if well balanced.
Plant-Based Eating Patterns
Exercise Guidelines for Special Populations
Older Adults (≥65 years)
Similar baseline recommendations: 150 minutes/week of moderate‐intensity, plus 2+ days of strengthening exercises.
Include balance exercises (tai chi, single‐leg stands, heel‐to‐toe walks) to reduce fall risk.
Modify intensity based on individual capability; some older adults may perform short bouts of activity multiple times daily.
Emphasize low‐impact, joint‐friendly exercises if they have arthritis or other mobility issues.
General Physical Activity Guidelines for Healthy Adults
Aerobic Activity
Minimum: 150 minutes of moderate‐intensity aerobic exercise per week (e.g., brisk walking, light cycling, water aerobics)or75 minutes of vigorous‐intensity aerobic exercise per week (e.g., running, interval training, competitive sports).
This can be spread out over the week (e.g., ~30 minutes of moderate activity 5 days/week).
Incremental approach: When clients find it daunting to start at 150 minutes, encourage small increments (e.g., 10–15 minutes per session) and gradually build up.
Muscle‐Strengthening Activity
At least 2 days per week focusing on major muscle groups (legs, hips, back, abdomen, chest, shoulders, arms).
Exercises may include bodyweight moves (e.g., squats, push‐ups), resistance bands, or free weights/machines.
Aim for 8–12 reps per set to near fatigue; 1–3 sets, depending on fitness level.
Exercise Guidelines for Special Populations
Pregnant & Postpartum Individuals
In the absence of contraindications, at least 150 minutes moderate‐intensity aerobic activity per week.
Avoid supine exercises after the first trimester and activities with high risk of falling or abdominal trauma.
Watch for signs of overexertion; hydration and adequate caloric intake are crucial.
Encourage postpartum resumption of exercise gradually, as medically advised.
Exercise in Chronic Conditions (e.g., diabetes, heart disease, arthritis)
May need modifications or specialized programs.
Typically aim for 150+ minutes/week of moderate activity, with additional emphasis on safety and physician clearance.
Low‐impact aerobic activities (e.g., walking, swimming) and gentle strength work can be beneficial.
A supervised exercise program or rehabilitation program may be indicated if risk factors are present.
Improves cardiovascular endurance, helps manage weight, reduces blood pressure, boosts mood and energy.
Examples: walking, jogging, cycling, swimming, dancing.
Cardio (Aerobic) Training
Builds and preserves lean muscle mass, supports bone density, aids functional fitness (activities of daily living).
Can help with weight management and body composition (higher muscle mass).
Resistance/Strength Training
Enhances range of motion, may reduce musculoskeletal injuries, and improve posture.
Examples: yoga, static stretching, foam rolling (myofascial release).
Flexibility & Mobility Work
Important for fall prevention, agility, coordination, especially for older adults but also beneficial for all ages.
Could be integrated into daily routines or as part of specialized classes.
Balance Training
Recommended Sleep Durations
Adults (18–64 years):
Typically 7-9 hours of quality sleep per night is recommended.
Recommended Sleep Durations Older Adults (65+ years):
Generally 7-8 hours, though some might need slightly more or less.
Common Sleep Disruptors
Screen Time & Light Exposure:Electronic devices emit blue light that can suppress melatonin production, disrupting circadian rhythms.
Caffeine & Stimulants:Consuming coffee, tea, soda, or energy drinks late in the day can interfere with the ability to fall asleep.
Stress & Anxiety:Racing thoughts at bedtime, job/family worries, or poor stress management can hinder quality sleep.
Inconsistent Schedules:Bedtimes and wake times that vary widely from day to day (e.g., shift work, staying up late on weekends) can disrupt circadian rhythms.
Normal Weight
18.5 - 24.9
Obese
≥30
Overweight
25 - 29.9
Stage 1 Hypertension
130-139 / 80-89 mmHg
Normal blood pressure
<120 / <80 mmHg
Stage 2 Hypertension
≥140 / ≥90 mmHg
Ideal LDL cholesterol level
<100 mg/dL
Borderline High triglyceride level
150 - 199 mg/dL
Total cholesterol level of 210 mg/dL category
Borderline High (200 - 239 mg/dL)
Fasting glucose range for Prediabetes
100 - 125 mg/dL
A1c level indicating Diabetes
≥6.5%
Fasting glucose of 98 mg/dL classification
Normal (<100 mg/dL)
Waist circumference cutoff for high CVD risk
Men >40 inches, Women >35 inches
Risk factors needed to diagnose Metabolic Syndrome
3 or more
One of the five Metabolic Syndrome risk factors
High BP (≥130/85),
High Triglycerides (≥150 mg/dL),
Low HDL (<40 men, <50 women),
High Fasting Glucose (≥100 mg/dL),
Abdominal Obesity
High blood pressure reading
≥140 / ≥90 mmHg
Healthy HDL level
≥60 mg/dL
Obese Class 3 (Severe Obesity) category
≥40
What is the Minimum Aerobic Activity Recommended for adults?
150 minutes of moderate‐intensity aerobic exercise per week (e.g., brisk walking, light cycling, water aerobics) or 75 minutes of vigorous‐intensity aerobic exercise
Which of these exercise guidelines is NOT included Exercise Guidelines for Special Populations Pregnant & Postpartum Individuals
Aim for 8–12 reps per set to near fatigue; 1–3 sets, depending on fitness level.
3 multiple choice options
Which of these exercise guidelines is NOT included General Physical Activity Guidelines for Healthy Adults
Include balance exercises (tai chi, single‐leg stands, heel‐to‐toe walks) to reduce fall risk.
3 multiple choice options
Key Principles of the DASH Diet: Increase:
Fruits and vegetables (rich in potassium).
Whole grains, beans, nuts, and seeds.
Low-fat or fat-free dairy products.
Lean proteins like fish, poultry, and plant-based sources.
Key Principles of the DASH Diet: Limit:
Sodium intake to 1,500-2,300 mg/day.
Saturated fats (e.g., fatty meats, full-fat dairy).
Sugary beverages and sweets.
Anti-Inflammatory Diets: Managing Inflammation and Arthritis
Increase Anti-Inflammatory Foods:
Omega-3 fatty acids from fatty fish (e.g., salmon), flaxseeds, walnuts.
Colorful fruits and vegetables rich in antioxidants (e.g., berries, spinach).
Whole grains like quinoa and brown rice.
Limit Pro-Inflammatory Foods:
Refined carbohydrates (e.g., white bread).
Processed foods high in trans fats or added sugars.
Diabetes: Balanced Carbohydrate Management
Key Principles:
Focus on Low-Glycemic Foods: Include whole grains, non-starchy vegetables, legumes, and lean proteins to stabilize blood sugar levels.
Carbohydrate Monitoring: Spread carbohydrate intake evenly across meals to avoid blood sugar spikes.
Healthy Fats: Incorporate sources like avocados, nuts, seeds, and fatty fish to support heart health.