Autoimmunity & Immunodeficiencies: Principles, Diseases, and Causes in Veterinary Medicine
1/86
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
87 Terms
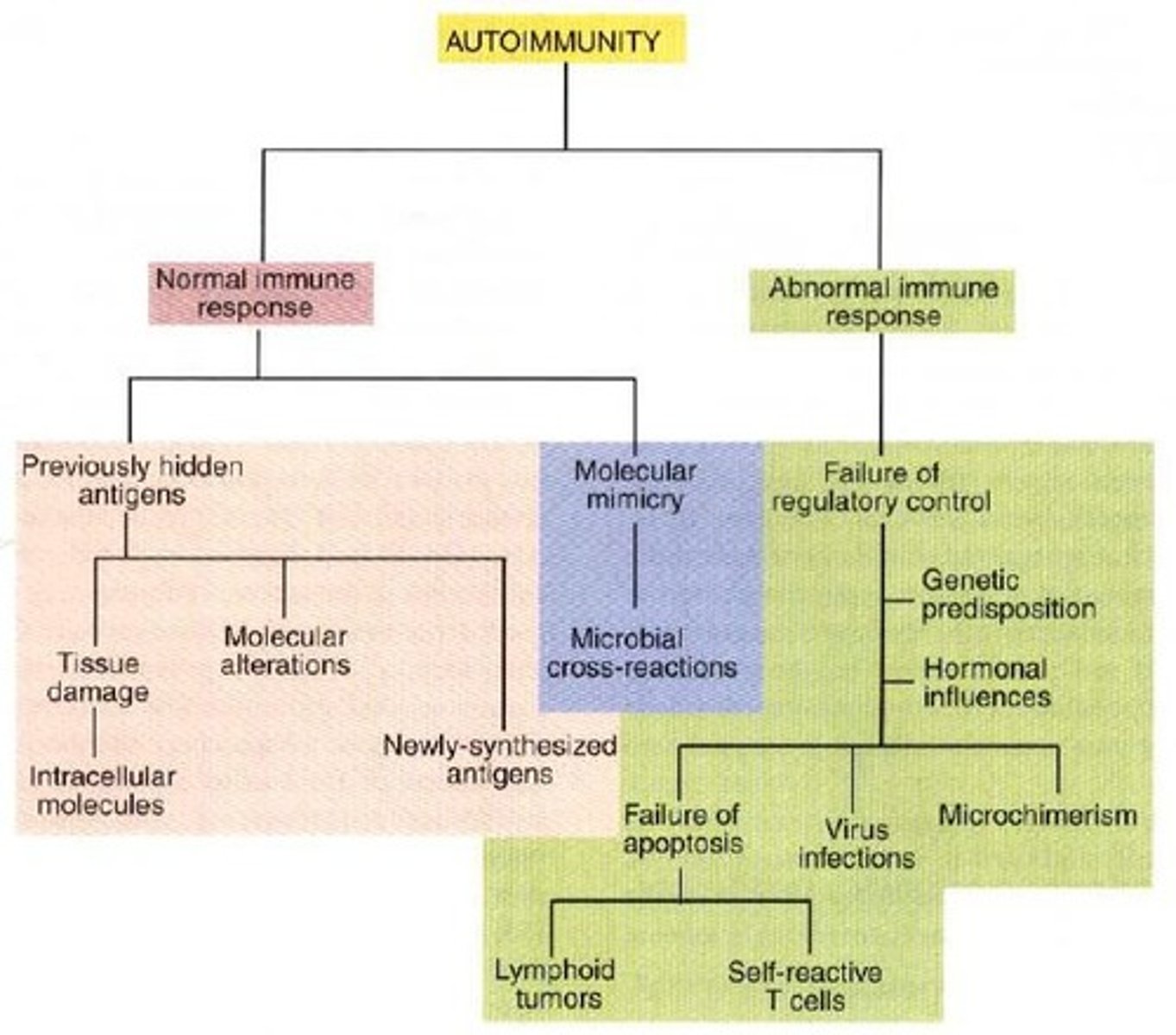
What are the two major categories of autoimmune diseases?
1. Result from normal immune response to an unusual or abnormal antigen. 2. Result from abnormal immune response to a normal antigen (most significant).
What occurs when there is a breakdown in the immune system's tolerance of self?
Autoimmune disease.
What are the key factors that can lead to autoimmune diseases?
1. Aberrant response to a single specific antigen. 2. General defect in the regulation of B- or T-cell functions.
Which gene is most important in influencing naturally occurring autoimmune diseases?
The MHC (Major Histocompatibility Complex).
How can defective thymic selection contribute to autoimmune diseases?
It may lead to the development of autoimmune diseases due to improper immune cell maturation.
What is an example of a dog breed that is unusually prone to autoimmune blood diseases?
Old English sheepdogs.
What happens to hidden antigens after cell damage?
They may be released and trigger an autoimmune response as they encounter antigen-sensitive cells.
What is molecular mimicry in the context of autoimmunity?
It is the sharing of epitopes between an infectious agent and self-antigen, leading to cross-reactivity.
Give an example of a disease caused by molecular mimicry.
Infection with Trypanosoma cruzi can lead to autoantibodies that cause nervous system and heart disease.
What can trigger the production of autoantibodies related to molecular changes?
The development of completely new epitopes on normal proteins.
What is a consequence of failure of regulatory control in the immune system?
A sustained autoimmune response necessary for disease development.
Name an organ-specific autoimmune disease that affects the thyroid.
Hyperthyroidism.
What is an example of a systemic immunological disease?
Systemic Lupus Erythematosus.
What non-specific factor can affect an animal's ability to synthesize immunoglobulins?
Malnutrition.
What are some cytotoxic chemicals that can lead to immunodeficiency?
Corticosteroids, estrogen, and butazolidone.
Why is colostrum important in the context of immunodeficiency?
It provides passive immunity to newborns.
How can environmental contaminants affect immunity?
Heavy metals can suppress antibody production and cell-mediated immunity.
What is a specific factor that can lead to immunodeficiency?
Neutrophil dysfunction and deficiency.
What breed is known for susceptibility to Aspergillus infection?
German shepherd.
What condition is associated with combined immunodeficiency in foals?
Arab foal.
Which dog breeds are particularly susceptible to parvovirus enteritis?
Rottweiler and Doberman.
What effect can vaccination have on immunodeficiency?
It can be associated with malnutrition.
What is the impact of neoplasia on the immune system?
It can cause protein depletion, leading to immunodeficiency.
What can cause a decrease in the number of neutrophils?
Drug therapy, toxins, viral infections (like canine distemper and parvovirus), bacterial infections (due to bacterial toxins depressing bone marrow production), and cyclic neutropenia.
What is cyclic neutropenia and its characteristics?
An inherited condition in humans and greyhounds with a cycle of 10-12 days, lasting about 2-4 days.
What syndrome is associated with defective chemotactic migration in neutrophils?
Chediak-Higashi syndrome, characterized by giant lysosomal granules in cells, normal phagocytic function, and associated with oculo-cutaneous albinism.
What is canine granulocytopathy syndrome?
A condition where neutrophils appear normal and may increase in number but have an enzyme deficiency affecting their ability to kill phagocytosed bacteria; inherited in Irish Setters.
What are the two types of lymphocyte dysfunction?
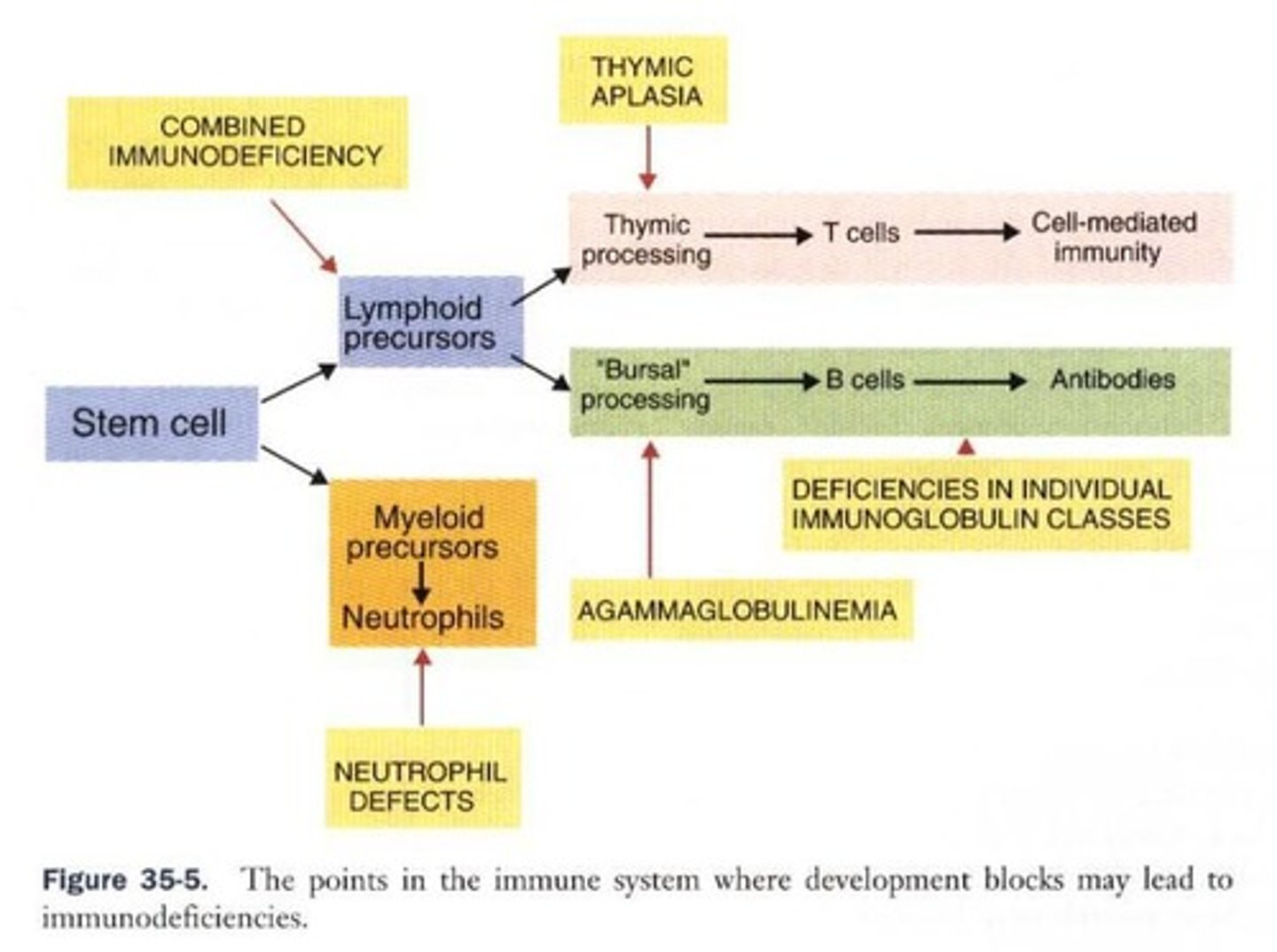
Primary and secondary/acquired.
What is severe combined immunodeficiency (SCID) in Arab foals?
An autosomal recessive condition causing failure to produce functional T and B cells, leading to infections after antibody levels decline.
What is agammaglobulinemia in horses?
A condition characterized by the inability to produce B cells, resulting in a lack of immunoglobulin, with a lifespan of about 18 months.
What is Acquired Immunodeficiency Syndrome (AIDS) in humans?
A disease caused by the HIV virus that suppresses helper (CD4) T cell activity, leading to lymphopenia and opportunistic infections.
What are some infections associated with AIDS in humans?
Opportunistic infections like pneumocystis infection and the development of Kaposi's sarcoma.
What is Feline Acquired Immunodeficiency Syndrome (FAIDS)?
A disease in cats similar to HIV in humans, first reported in 1987, associated with chronic infections of the oral cavity, respiratory tract, and conjunctiva.
What viral conditions can cause lymphoid suppression in animals?
Canine distemper, pestivirus (mucosal disease) in cattle, equine herpes virus, and viruses that cause neoplasms.
What are some other disorders known to be immunosuppressive?
Bone marrow neoplasia and demodectic mange.
What is the main effect of HIV on the immune system?
It suppresses helper (CD4) T cell activity and affects dendritic cells, macrophages, and microglia.
What is the characteristic of lymphopenia in AIDS patients?
A decrease in lymphocyte count, specifically CD4 T cells.
What is hypergammaglobulinemia?
An increase in immunoglobulin levels often seen in AIDS patients.
What is the typical lifespan of a horse with agammaglobulinemia?
About 18 months.
What is the genetic inheritance pattern of SCID in Arab foals?
Autosomal recessive.
What is the role of neutrophils in the immune response?
They are essential for phagocytosis and killing of bacteria.
What is the significance of chemotaxis in neutrophils?
It is crucial for neutrophils to migrate to sites of infection.
What are the clinical manifestations of Chediak-Higashi syndrome?
Photophobia and immunodeficiency due to defective chemotactic migration.
What is the primary cause of infections in SCID foals?
Failure to produce functional T and B cells leading to opportunistic infections.
What type of infections are commonly associated with FAIDS in cats?
Chronic infections of the oral cavity, respiratory tract, and conjunctiva.
What happens to T cell function as disease progression occurs?
There is suppression of T cell function.
What type of dermatitis is suggested by the reaction around mites as disease progresses?
Allergic contact dermatitis.
What is the most common organ-specific autoimmune disease in old cats?
Hyperthyroidism.
What autoantibodies are associated with feline hyperthyroidism?
Autoantibodies to thyroid peroxidase, found in 1/3 of cases.
What is the primary autoimmune mechanism in insulin-dependent diabetes mellitus (IDDM) in humans?
Mediated by autoantibodies against glutamic acid decarboxylase.
What is a significant characteristic of canine insulin-dependent diabetes mellitus?
Associated with pancreatic islet atrophy and loss of Beta cells.
Which dog breed has a familial predisposition to insulin-dependent diabetes mellitus?
Samoyeds.
What cytokines may influence the development of insulin-dependent diabetes mellitus?
Regulatory cytokines IFN-y, IL-12, IL-4, IL-10.
What is the most common cause of blindness in horses?
Equine recurrent uveitis, also known as periodic ophthalmia.
What are the symptoms of acute equine recurrent uveitis?
Blepharospasm, lacrimation, photophobia.
What major autoantigen is implicated in equine recurrent uveitis?
Interphotoreceptor retinoid-binding protein.
What is the pemphigus complex?
A condition caused by the immune system attacking its own skin cells, leading to blistering and pustule formation.
What is the most common form of pemphigus?
Pemphigus foliaceus, causing pustules, crusts, and scaling.
What distinguishes pemphigus vulgaris from other forms?
It can cause blisters in the mouth and on mucous membranes.
What is alopecia areata?
An inflammatory hair loss condition that starts locally and can spread to the entire body.
What immune cells infiltrate hair follicles in alopecia areata?
CD4+ and CD8+ T cells and Langerhans cells.
What type of antibodies are directed against hair follicles in alopecia areata?
IgG antibodies directed against lower hair follicles.
What is the primary characteristic of immune-mediated hemolytic anemia (IMHA)?
Autoantibodies to RBC antigens.
What are common symptoms of immune-mediated hemolytic anemia?
Anemia, pallor, weakness, lethargy, fever, icterus, hepatosplenomegaly.
What genetic predisposition is noted for immune-mediated hemolytic anemia in dogs?
Cocker spaniels and miniature schnauzers.
What are the classifications of IMHA in dogs?
Class I: agglutination at body temp; Class II: IgM-mediated intravascular hemolysis; Class III: IgG1 and IgG4 without agglutination; Class IV: some IgM antibodies cannot agglutinate.
What are cold antibodies and when do they function?
Cold antibodies are antibodies that can only agglutinate red blood cells when chilled, specifically at temperatures around 4°C.
What can happen when blood circulates to extremities and cools sufficiently?
It may lead to agglutination within capillaries, resulting in vascular stasis, blockage, tissue ischemia, and necrosis, particularly severe in winter.
What is Class V mediated by and what is its effect?
Class V is mediated by IgM antibodies that bind RBCs when chilled but do not agglutinate, activating complement and leading to intravascular hemolysis.
What is Myasthenia Gravis and what causes it?
Myasthenia Gravis is a disease of skeletal muscle characterized by abnormal fatigue and weakness after mild exercise, caused by a deficiency of acetylcholine receptors.
Which breeds are known to have an inherited deficiency of acetylcholine receptors in Myasthenia Gravis?
Jack Russel Terriers, Springer Spaniels, and Fox Terriers.
What causes the deficiency of acetylcholine receptors in adults with Myasthenia Gravis?
In adults, it is due to autoantibodies that accelerate degradation of the receptors and block acetylcholine-binding sites.
What is Polymyositis and which dogs are commonly affected?
Polymyositis is a condition that occurs in large dogs such as German Shepherds, characterized by progressive muscle weakness not associated with exercise.
What are some symptoms of Polymyositis?
Symptoms include changes in laryngeal muscle function affecting voice, megaesophagus leading to dysphagia, and aspiration pneumonia.
What is the treatment of choice for Polymyositis?
Corticosteroids.
What is Systemic Lupus Erythematosus?
A complex disease syndrome affecting humans, primates, mice, horses, dogs, and cats, characterized by a variety of symptoms and disease courses.
What are some key features of Systemic Lupus Erythematosus?
Patients develop autoantibodies, changes in T cell function, defective phagocytosis, impaired apoptosis, multiorgan inflammation, and oncogene expression.
What is the hallmark of Systemic Lupus Erythematosus?
The hallmark is the presence of autoantibodies against different nuclear structures, including nucleic acids and ribonucleoproteins.
What is Rheumatoid Arthritis and how does it manifest in dogs?
Rheumatoid Arthritis is an erosive polyarthritis that manifests in dogs with chronic depression, anorexia, pyrexia, and lameness, especially after rest.
What joints are primarily affected by Rheumatoid Arthritis?
It mainly affects peripheral joints, which show symmetrical swelling and stiffness.
What are the consequences of Polymyositis related to the esophagus?
Megaesophagus may lead to dysphagia and result in aspiration pneumonia.
What type of antibodies are found in Polymyositis?
Patients may have antinuclear antibodies or antibodies to sarcolemma.
What are the common symptoms of Myasthenia Gravis in affected animals?
Abnormal fatigue and weakness after mild exercise.
What is the effect of autoantibodies in Myasthenia Gravis?
They block acetylcholine-binding sites and trigger complement-mediated damage.
What is a significant symptom of Polymyositis related to voice?
Changes in laryngeal muscle function lead to a change in voice.
What is the relationship between temperature and the function of cold antibodies?
Cold antibodies agglutinate red blood cells only when the temperature is sufficiently low, specifically around 4°C.
What are the systemic effects of Systemic Lupus Erythematosus?
It can cause multiorgan inflammation and a wide variety of symptoms due to autoantibodies.