Diseases and Disorders of the Vulva and Vagina
1/83
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
84 Terms
What is the spectrum of conditions that cause vaginal or vulvar symptoms that present with itching/irritation, burning/ +/- pain, and abnormal discharge?
vulvovaginitis
What is the normal vaginal bacteria and what is its pH?
lactobacillus, <4.5
What are the MCC of vulvovaginitis?
BV, trich, candidiasis
What is the bacteria that causes BV with a shift of pH above normal?
gardnerella vaginalis
What is the MCC of vaginitis and the MC vaginal infection?
BV
A pt presents with malodorous "fishy" discharge, that is watery, thin, and gray-white in color. The wet prep showed "clue cells" --- what is the likely dx and how are you treating this patient?
BV
tx: topical or oral metronizadole
What is the Amsel criteria for the diagnosis of BV?
1. Homogenous, non-clumping vaginal discharge
2. Amine (fishy) odor when potassium hydroxide solution is added to vaginal secretions
3. presence of clue cells (greater than 20%) on microscopy
4. Vaginal pH greater than 4.5
What bacteria causes candidiasis?
candida albicans
What are some predisposing factors for vulvo candidiasis?
diabetic, pregnancy, obese, immunocompromised, steroid use, recent ABX use, personal practices
A pt presents with itching, burning, and dysuria. Upon PE you see bright red mucosa with a thick white curd like "cottage cheese" like discharge. On Wet prep you find hyphae and spores. --- What is the likely dx and treatment?
vulvovaginal candidiasis
tx: "-AZOLE"
How are you treating a pregnant patient for volvo candidiasis?
topical "-azole"
A pt presents with vulvar itching, burning, and copious frothy discharge that has a rancid odor. Upon PE you see erythematous petechiae "strawberry patches". On wet prep you see motile flagellated protozoan --- what is the likely dx? and how are you treating?
trich
Tx (including pregnant): Metronidazole PO
What can occur with diminished estrogen levels?
atrophic vaginitis
A pt presents with complaints of decreased vaginal lubrication, dryness, itching, burning, dyspareunia. Upon PE you see thinning of pubic hair and vaginal mucosa that is smooth, thin, and friable, with loss of rugae and petechiae-- what is the likely dx and how are you treating?
atrophic vaginitis
tx: Topical or oral estrogen therapy (premarin )
- topical if women if uterus is intact
What is usually found in postmenopausal women that does NOT usually involve the vagina and presents as "onion skin" or cigarette paper parchment like with hypopigmentation?
Lichen Sclerosus
A pt presents with complaints of chronic vulvar itching, dyspanuria, and "onion skin" or cigarette paper like. On PE you see severe anatomic landmarks that are lost and there if fusion of the normal labial and periclitoral folds and skin that is hypopigmented. ---- what is the likely dx and how are you treating it?
Lichen Sclerosus
tx: high dose topical steroids (Clobetsol)
What is the diagnostic testing for lichen sclerosus?
biopsy- "hyalinized glassy dermis"
What is the tx for lichen sclerosus?
high dose topical steroids (clobetsol)
What presents as an "itch that rashes" usually with diffusely reddened areas and leather appearing and patients usually have a history of itching or burning that is relieved by scratching or rubbing with a washcloth-- a biopsy is not warranted?
lichen simplex chronicus
What is the tx for lichen simplex chronicus?
benadryl or atarax
- if not relieved in 3 mo then BIOPSY
What is a rare autoimmune skin condition that involves keratinized and mucosal surfaces (including the vulva and the vagina)?
lichen planus
A pt presents with chronic vulvar burning and/or itching, insertional dyspareunia and profuse vaginal discharge. Upon PE you see whitish lacy bands of keratosis with "wickham striae" and multiple shiny flat - purple, planar, polygonal, pruritic, papules---- what is the likely dx?
lichen planus
What is the diagnostic testing for lichen planus?
biopsy to confirm
What is the tx for lichen planus?
vaginal steroid suppository or topical steroids
What is an inherited condition that will present with slightly raised, round/oval pink plaques, silver scale on erythematous base, + Auspitz sign (bleeding when scale is removed) and can be treated with topical steroids?
psoriasis
What is acute and chronic inflammation of vestibular glands w/ reoccuring pain and long lasting (Premenopausal > post)?
localized volvodynia
A pt presents with new onset insertional dyspareunia, unable to have intercourse, pain with tampon insertion, and sitting. Upon PE you obtain a "positive swab test" and see small, reddened, patchy areas. --- what is the likely dx?
localized volvodynia
What is the tx for localized volvodynia?
variety (topical lidocaine, changing or eliminating environmental factors, temporary abstinence, KY jelly or topical cortisone)
Surgical removal of vestibular glands
What occurs due to inflammatory blockage of sebaceous glands, small, smooth, nodular masses arising from the inner surfaces of the labia major and minora and contains a cheesy material?
sebaceous or inclusion cyst
What presents usually located bilaterally at 4 and 8 oclock on posterior lateral vaginal orifice, aid in lubrication of the vagina?
Bartholin cysts/abscesses
What is the tx for a small mass <3cm cyst/abscess?
cyst- sitz bath/warm compresses
abscess- I&D
What is the tx for a small mass >3cm cyst/abscess?
I&D both, culture, catheter placement, +/- abx
A pt presents with complaints of a "fullness sensation". Upon PE you see unilateral swelling-- what is the likely dx?
cyst
A pt presents with complaints of pain/tender to palpation and pain especially when sitting and walking. Upon PE you see Unilateral welling with erythematous mucosa and purulent discharge----- what is the likely dx?
abscess
What is a chronic condition of follicles in the area of sweat glands and can lead to scarring, draining, and fistula formation?
hidradenitis suppurativa
What is the treatment for hidradenitis suppurativa?
antibiotics, laser & light therpay, biologic therapies, surgery, anti-androgens
Surgical Exicison
What occurs when the genital plate canalization is incomplete and hymen is closed-- leading to obstruction of blood when menses occurs?
imperforate hyman
What is the tx for imperforate hyman?
hymenotomy
What is the term for early superficial changes to the skin covering the vulva (premalignant condition!!)?
VSIL (vulvar squamous intraepithelial lesion)
What are some RFs associated with VSIL?
HPV, smoking, immunosuppression
What classification of VSIL is low grade and usually has benign manifestations of the skins reaction to an HPV infection and occurs most often in condyloma acuminata?
LSIL
What is the treatment for LSIL?
self limited will resolve within a year or 2 and not treated unless symptomatic
What classification of VSIL is high grade and the intraepithelial neoplasms have potential to progress to invasive vulvar carcinoma -- associated with SCC?
HSIL
What classification of VSIL has the highest risk of progressing to SCC and is associated with lichen sclerosus?
differentiated VIN
A pt presents with vulvar pruritis or soreness, chronic irritation, burning/tingling, dyspareunia, and development of a raised mass. Upon PE you note localized lesions that are well isolated and raised with a rough texture and the vulva and perineal body is hairless. --- what is the likely dx?
VSIL
What is the diagnostic tool for VSIL?
colposcope (biopsy)
What is the tx for VSIL?
Wide excision or laser ablation
Topical Nonsurgical tx- F-FU, Imiquimod, Phototherapy
What is not common but is typically associated with adenocarcinoma in or around the lesion adn can present with: intense itching and pain with fiery red background mottled with whitish hyperkeratotic areas?
pagent disease of the vulva
What is the dx for pagent disease of the vulva?
clinical! -- biopsy
What is the tx for pagent disease of the vulva?
wide excision or vulvectomy
What typically occurs AFTER menopause Btwn ages 70-80 and 90% of them are SCC?
vulvar cancer
A 75yo F pt presents with complaints of vulvar pruritis, pain, burning, and slight bleeding. Upon PE you see red and white ulcerative lesions with a lump that arises in posterior 2/3rd of labium majora. --- what is the likely dx?
vulvar cancer
What is the dx and tx for vulvar cancer>?
biopsy and excision!
What makes up 85-90% of vulvar cancers as usually appears as a growth but can also be an ulcer OR can present as a sore that wont heal?
squamous carcinoma
What type of vulvar cancer lies deeper and is usually only detected by palpation?
adenocarcinoma
What type of vulvar cancer is the MC-non SCC of the vulva?
vaginal melanoma
What type of vulvar cancer presents as pigmented (brown or black), skin tag, or a raised irritated area?
vaginal melanoma
What type of vulvar cancer presents as a grape like mass protruding from the introitus of typically pediatric patients?
sarcomas
What are the diagnostics of vulvar cancer?
biopsy MULTIPLE areas
Colposcope for visualization
What is the tx for vulvar cancer?
conservative excision for unifocal lesions
- large tumors (>2cm) vulvectomy and node dissection
What type of cyst occurs on the outer aspect of vaginal canal, small, cystic in structure and usually asymptomatic?
garter duct
What type of cyst occurs on the posterior lower vaginal surface often from imperfect approximation of laceration or episiotomy?
inclusion
What can occur in the upper 1/3rd of the vagina and is caused by HPV or after irradiation of cervical cancer in women >50yo?
VAIN (vaginal intraepithelial neoplasia)
What is usually asymptomatic in a patient and found accidentally on a pap smear in women >50yo?
VAIN
What is the tx for VAIN -1?
watch
What is the tx for VAIN- 2?
laser, local excision, radiation, chemical treatments
What can present with unusual vaginal bleeding, watery or foul-smelling discharge, mass, plaque, ulcer, pelvic pain, and constipation and has 80-90% SCC?
vaginal cancer
What are some RFs associated with Vaginal cancer?
increasing age, VAIN, HPV, DES exposure, multiple sex partners, early first intercourse, smoking, HIV
What are some RFs associated with pelvic support defects?
pregnancy and delivery, genetic predisposition, parity, menopause, advancing age, prior pelvic surgery, CT disorders, obesity, chronic constipation, excessive straining, atrophic changes
What type of pelvic support defect is described:
uterine hernation into the vagina, appears smooth
uterine prolapse
What type of pelvic support defect is described:
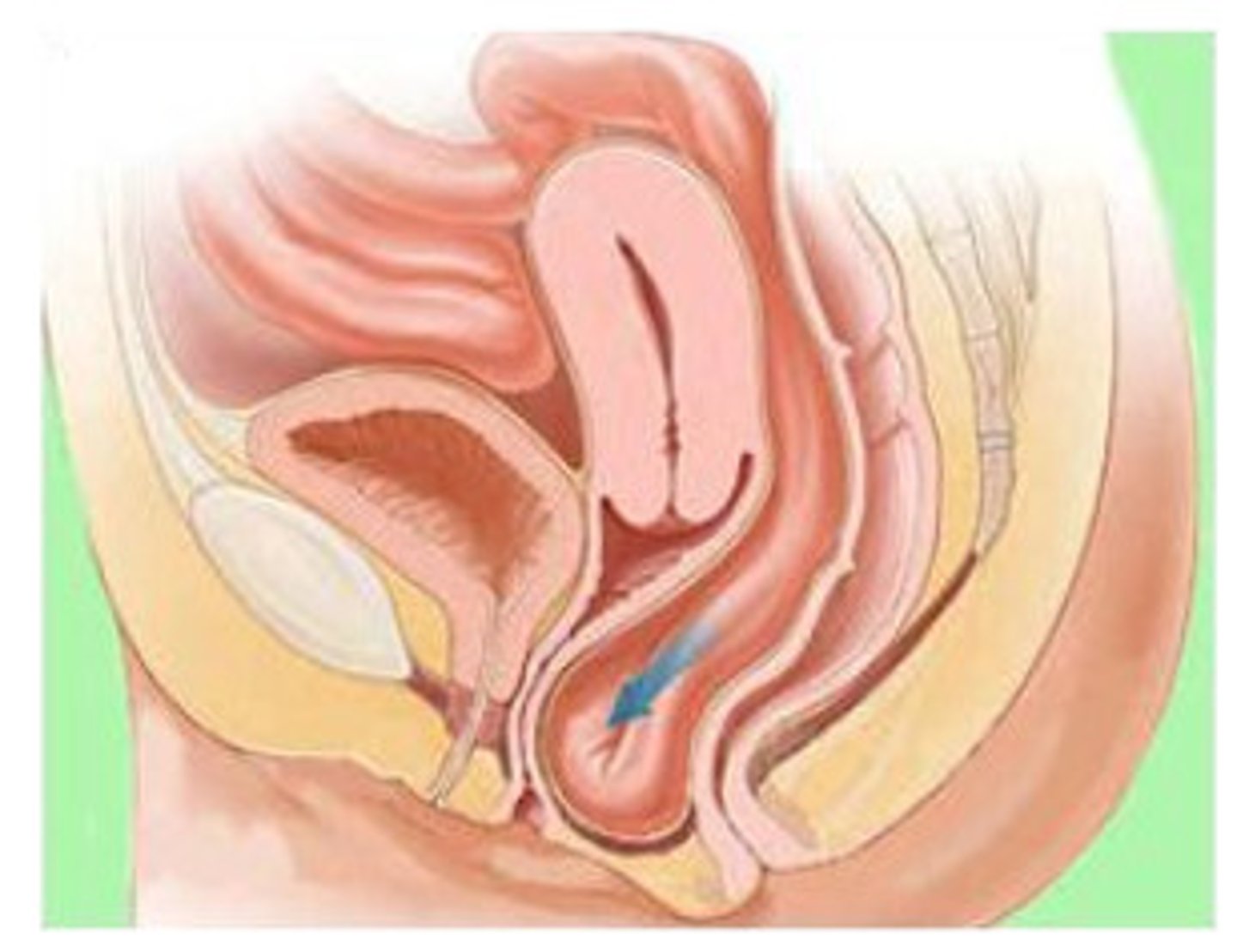
Anterior herniation of the bladder into the vagina with rugae appearance
Presents with: Urinary incontinence
cystocele (bladder)
What type of pelvic support defect is MC?
cystocele
What type of pelvic support defect is described:
herniation of the terminal rectum into the POSTERIOR vagina
rectocele
What type of pelvic support defect is described:
vaginal vault hernia containing SI
enterocele
What type of pelvic support defect is described:
sagging/prolapse of urethra following detachment of the bladder neck from pubic symphysis with childbirth
urethrocele
What stage of pelvic organ prolapse is described:
No prolapse. The cervix (or vaginal cuff, if the patient has had a hysterectomy) is at least as high as the vaginal length
stage 0
What stage of pelvic organ prolapse is described:
The leading part of the prolapse is >1 cm above the hymen.
stage I
What stage of pelvic organ prolapse is described:
The leading edge is ≤1 cm above or below the hymen.
stage II
What stage of pelvic organ prolapse is described:
The leading edge is >1 cm beyond the hymen, but less than or equal to the total vaginal length.
stage III
What stage of pelvic organ prolapse is described:
Complete eversion
stage IV
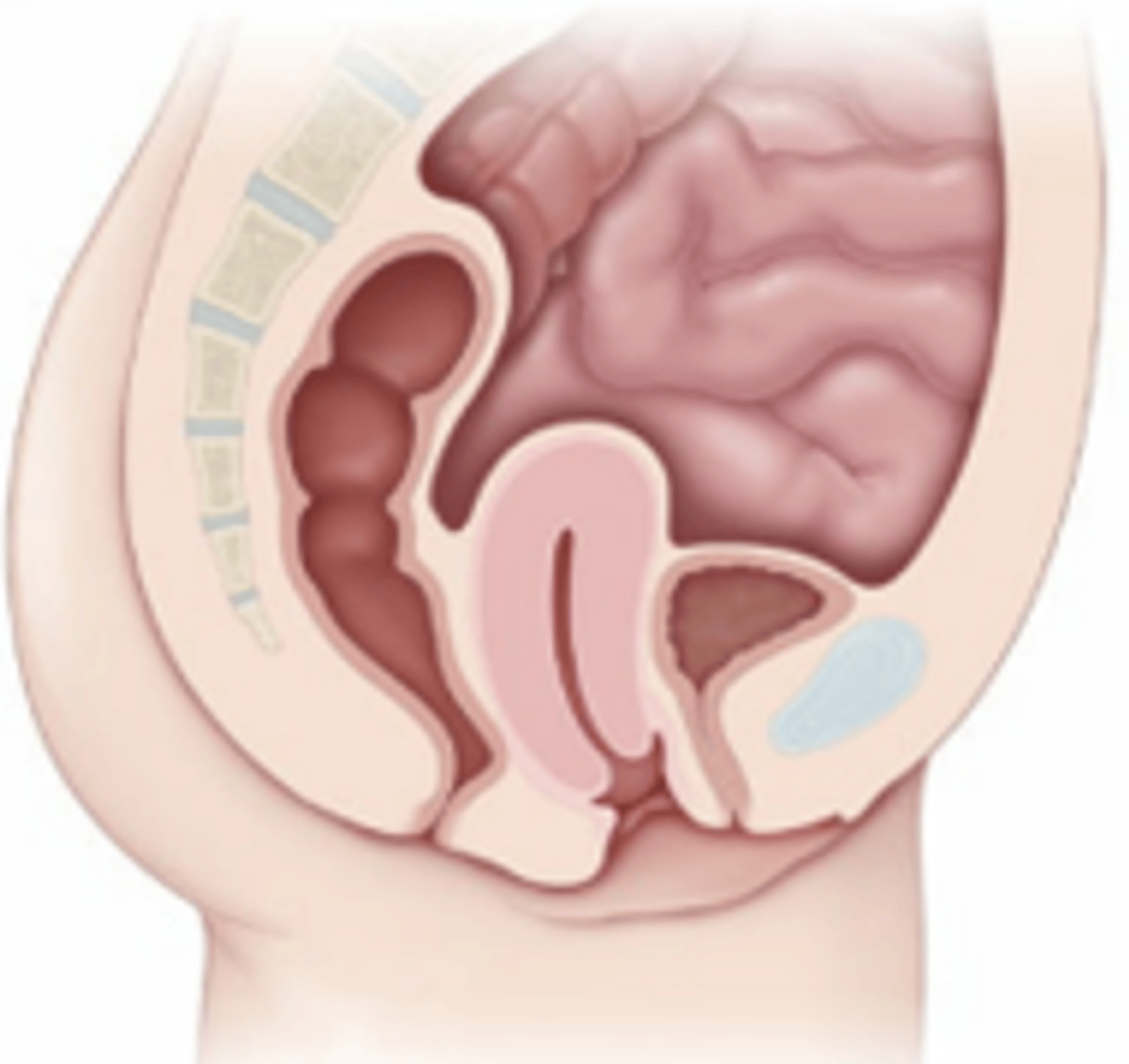
uterine prolapse
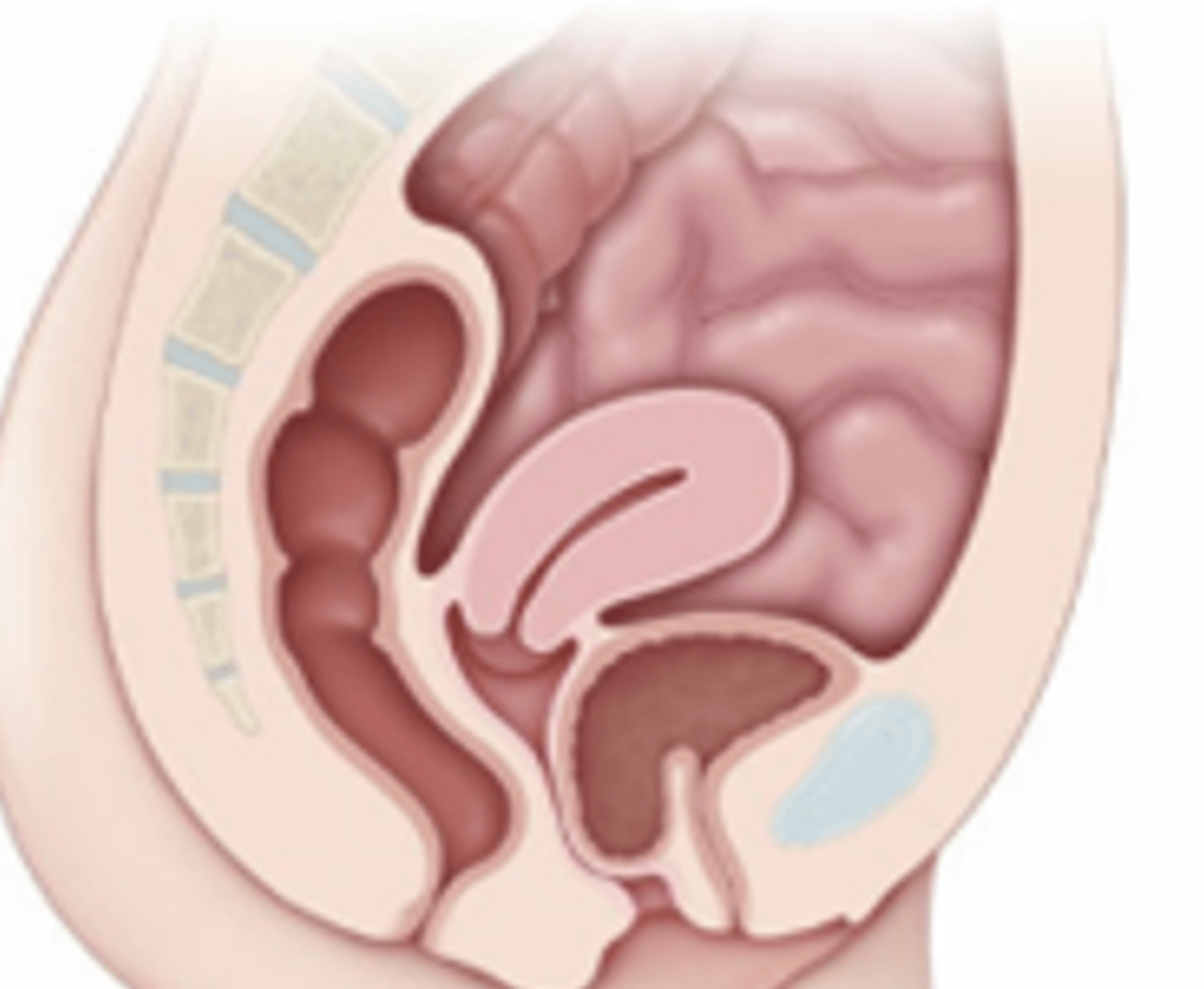
cystocele
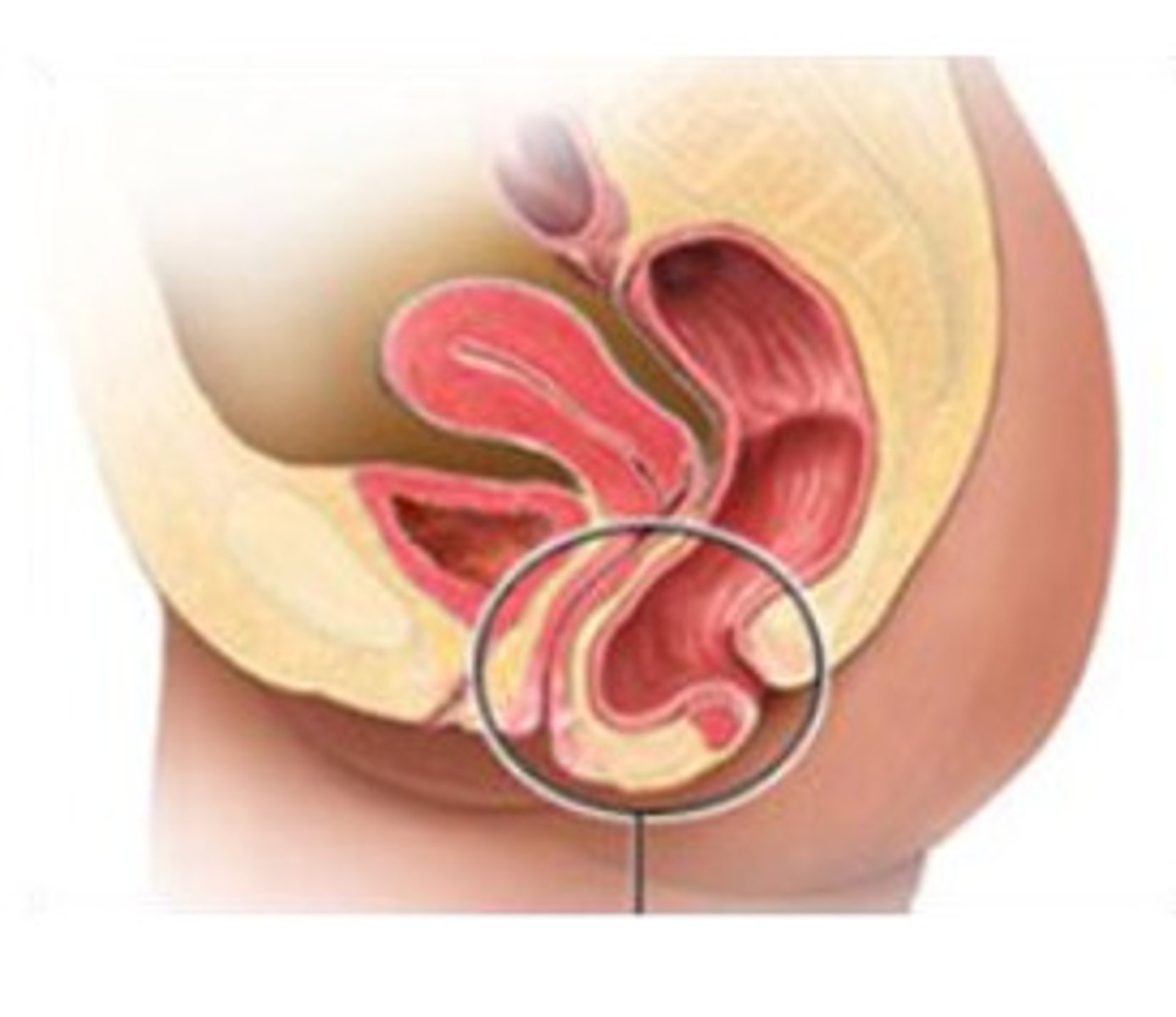
rectocele
enterocele