MODULE 11. OTHER GRAM NEGATIVE RODS
1/135
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
136 Terms
History and current status Vibrio cholera
-haiti, india, pandemics
Dates back to alexander the great (356 BC)--> “scourge of antiquity”
Disease is endemic in sections of India and Bangladesh
7 pandemics since 1817
Most recent in 1960-70s involving africa, western europe, phillipines, parts of southeast asia
Haiti outbreak: followed earthquake in 2010 (lasted 8 years), spread rapidly through displacement camps, already area of concern, infected almost a mil, killed 10,000
Lab diag: Vibrio cholerae
gram stain and morph
culture media
oxidase
lactose
Gram negative rod, comma-shaped
growth on simple culture/agar media; media specific for vibrio cholerae is also available
Oxidase positive (enterics are ox neg)
lactose negative (like intestinal pathos)
Vibro genus: causative agents of ___
2 important strains
how to distinuish and what serotype is in both pathogenic strains
which one is responsioble for most cases, which one is in india
Vibro genus: causative agents of cholera
Contains important intestinal pathogens of man such as vibrio cholerae which causes epidemic asiatic cholera
There are two strains/biotypes of vibrio Cholera distinguished by phenotypic markers and O (somatic) antigens→both have O1 serotype
Vibro cholerae (strain El Tor)--1st ID in El Tor Egypt
milder form of disease, patients can be asymptomatic
bacteria survives in the body longer than classical strains, allowing carriers to infect a great number of people
responsible for most cholera cases globally
biotype that caused cholera and Haiti after 2010 earthquake
Vibrio cholerae (classical)
relatively rare globally, except in India and Bangladesh (current endemics)
source V. cholera
2 carriers
how easy is it to ID in chronic carriers and why
Source= man is the only known host
human carrier serves as the source
carrier sheds bacteria and feces, contaminates food and water supplies
there are two types of carriers:
convalescent= those recovering from disease who shed bacteria for up to a year
chronic= those who no longer have disease but still carry back bacteria for years
maybe asymptomatic
these individual store bacteria in the gallbladder
gallbladder intermittently sheds bacteria which can make it difficult to identify these individuals
unpredictable release
Transmission: V. cholera
2 risk foods
detremental conditions (3—why one is not suff to prevent infection)
Fecal oral route
ingestion of contaminated food or water such as fruits and vegetables grown in sewage rich soil that are then ingested without prior cooking
eating raw oysters as well
detrimental conditions:
desiccating/drying, sunlight, acid conditions kill vibrio, however, microbial dose causing infection is so great (1 mil organisms) that losing some bacteria due to stomach acid is not sufficient to prevent infection
Pathogenesis V. cholera
location, syms
complications result from what (3 following conditions)
how much fluid loss
relation to toxin
Ingestion in multiplication after ingestion, bacteria multiply rapidly in the intestine
production of enterotoxin
bacteria produce powerful enterotoxin which acts on the intestinal lining causing massive fluid and electrolyte loss
fluid loss can be up to 20 L day or 5 gallons
voided fluid contains high amounts of Na, K, Cl, and bicarbonate (buffer sys)=>electrolytes
Enterotoxin, not the bacteria itself, causes pathogenic condition→toxic cond
in the large intestine, bacteria multiply rapidly, toxin from bacteria penetrates cells of intestinal wall, toxin prevents intestine from absorbing water from digested food; diarrhea and dehydration as result
symptom=severe vomiting and diarrhea can be abrupt on set with characteristic rice water stools which help in diagnosis of the disease
without prompt rehydration, death can occur within hours after onset of symptoms
severe infection=symptoms can be vomiting and profuse diarrhea, moderate to severe hypovolemic shock (low volume fluids), rice water stools→treat with oral rehydration soln (ORS)
complications= Result from massive loss of essential electrolytes due to severe dehydration and diarrhea
hypovolemic shock
metabolic acidosis
Since bicarbonate is buffer system in the body, when bicarbonate decreases acid condition develops, hypokalemia can follow (K+ loss can affect cardiac function)
State the treatment administered to counteract the effects of the V. cholera enterotoxin.
-% mortality treatment and not
1 antibi
immunity/ vacination
Treatment:
Salt solution, intravenous fluids, antibiotics
and unprepared communities, death rates can be as high as 50%, with treatment only 1 % mortality
Rehydration is the first priority treatment, then prompt fluid in electrolyte replacement causes rapid Improvement in the patient
antibiotics such as tetracycline lower the bacterial load which lowers the amount of enterotoxin released, reduces fluid and electrolyte following administration, eliminate bacterial concentration and bile of the gallbladder thereby eliminating the carrier state
Immunity, prevention, control:
After resolution of infection, immunity is long-lasting for most people
single-dose vaccines are available for travelers to areas where cholera is common
oral cholera vaccine (OCV) is available to prevent disease spread– limitation of this vaccine is a limited protection in children
proper sanitation and hygiene is the best way to reduce large numbers of infected people
Campylobacter:
Causative agents of what
species of interest
sporatic events or epi/pandemics
affects how many anually
Causes 5 to 10% of all diarrhea cases in the US
most human illness is caused by one species, C. jejuni
virtually all cases occur as isolated, sporadic events, not large outbreaks
around 15 cases out of 100,000 people are diagnosed annually– in many cases go undiagnosed or unreported
estimated to affect over 1 million people annually
Source of C. jejuni
resoviors in animals/ env
Lower animals, such as dogs and cats
people have acquired infection from infected stool of sick pet
birds carry C. jejuni without becoming ill
Reservoirs: Several environmental reservoirs can lead to human infection:
colonization of GI tract of chickens leading to high numbers of C. jejuni– bacteria passes through Chickens in a flock through fecal oral route, humans consume contaminated animal products such as unpasteurized milk or meat
C. jejuni can enter water supply / infect humans directly via drinking water
C. jejuni invades epithelium of human intestine, causing inflammation and diarrhea
81% supermarket chickens
Transmission C. jejuni
way to red
how many organisms casue infection
ingestion of food as well as poultry and unpasteurized dairy products, or contaminated H2O
most cases are associated with handling raw poultry or eating raw or undercooked poultry meat
freezing reduces the number of campylobacter present in raw meat because it kills the bacteria (unlike with salmonella)
one way to become infected is to cut poultry meat on a cutting board that is porous and allows liquids to get into the board itself, and then use the unwashed cutting board to prepare vegetables or other raw / lightly cooked foods
a very small number of campylobacter organisms ( <500) can cause illness in humans
even one drop of juice from raw chicken meat can cause an infection in a person
Clinical infection from C. jejuni
symps
self limiting or not?
incubation
symps=Fever, cramps, bloody diarrhea ( indicates campylobacter is an invasive pathogen that infiltrates the lining of the intestine where blood capillaries rupture / are injured)
ulceration occurs at the mucosal surface of the intestine
Self-limiting
2 to 10 day incubation period
treatment of C. jejuni (1 antobi)
erythromycin is preferred antibiotic
Helicobacter pylori:
Causative agent of ___
what caused ulcers before discovery
who discovered and story
% ulcers regoc to be caused by H. pylori
Leading cause of peptic ulcers and chronic gastritis in America
mechanism for pathogenesis: motility, urease activity, association with gastric mucosal cells are all important violence factors
before 1982 when this bacterium was discovered, spicy foods, acid, stress, lifestyle we're considered causes of ulcers
majority of patients were given long-term medications without hope for permanent cure
patients reduced acid content, coded the stomach, reduced pain
Relieved ulcer-related symptoms, healed gastric mucosal inflammation, may have healed the ulcer, but did not treat the infection
Barry J. Marshall and J. Robin Warren won nobel prize in 2005
Skeptics claimed that bacteria could not withstand the harsh acidic environment of the upper digestive tract, so to disapprove this criticism Marshall ingested H. pylori, making himself violently ill with severe gastritis, and then resolved symptoms with antibiotic treatments
80 to 90% of ulcers are now recognized to be caused by H. pylori
source of H. pylori and % that harbors
location
% asymp
primary role of transmission
More than 50% of the population globally harbors age H. pylori in the upper GI tract
85% of infected people never experience symptoms– why remains unknown
many people become infected as children, parents and siblings seem to play a primary role in transmission
Transmission H. pylori (2)
person to person by saliva
equal contamination of food / water
manifestations H. pylori (2 countries common—50%)
long term infect leads to __ fold inc risk of dev (2):
do most ppl have symps?
Most infected people never suffer symptoms
It is common in countries such as Columbia and China where h.pylori infects over half of the population in early childhood
Some adults and children suffer from chronic active and persistent gastritis due to h. Pylori
long-term infection leads to two to six-fold increased risk for developing:
gastric cancer– second most common cancer worldwide
mucosal associated lymphoid (MALT) lymphoma
clinical diag of H. pylori: Endoscope and biopsy
diag from biopsy accomplished by ___test (dep on what rxn)
how fast is result
Endoscopy and Associated biopsy is the reference method for diagnosis
“Go to method” that other methods are compared to if there is a new one discovered
during endoscopy, biopsy specimens of stomach and duodenum are obtained
H. pylori diag from biopsy is accomplished by:
Biopsy urease test (urease pos–releases urease in stomach–only source therefore ID)
color metric test based on ability of h.pylori to produce urease
rapid test result of tissue from biopsy
histologic stain of tissue and culture to identify the bacteria present in the tissue
gold standard of diagnostic tests
clinical ID: Urea breath test H. pylori
role of labeling and how to track
what is released from patient with label
In this test, patient is given either 14C- labeled urea to drink
h.pylori metabolizes the urea rapidly and label carbon is released as 14-CO2 in the patient's expelled breath
This can be used to determine whether h. pylori is present
gold standard test for H. pylori
Endoscope and biopsy
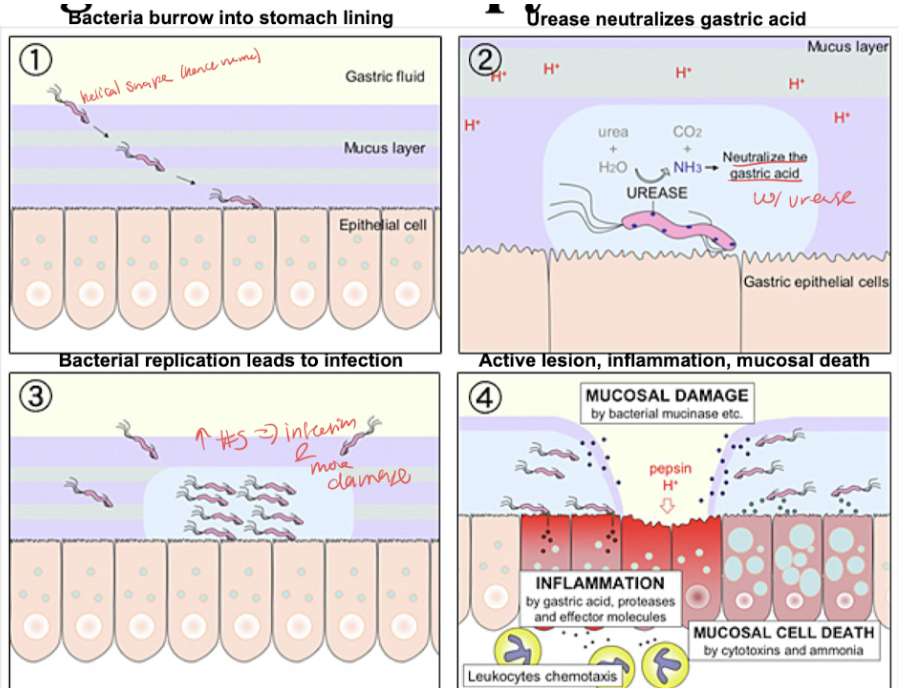
Progression of infection H. pylori
Bacterial burrow into stomach lining, urease neutralizes gastric acid with urease, bacteria replication leads to infection and more damage, active lesion inflammation and mucosal death
Serum antibody test (blood) H. pylori clinical ID
what antibody
compare ease of use to breath test
definitive?
Serological testing measure of specific IgG (takes while to develop but massive effect– “memory” for years)
Simpler assay than breath test
IgG antibodies have reactivity against H. pylori
Determines if a person has been infected
If antibodies are present, then the person has or had the infection–that could be current or 10 yrs ago (not very definitive)
Sensitivity and specificity of these assays range from 80-90%
H. pylori Stool antigen test clinical ID
Antigen detection is accurate, noninvasive test for direct detection of H. pylori antigens in stool (bac on antigen therefore yes or no answer for current status of infect)
Antigen detection=active infection
Definitive test of choice for diag and treatment monitoring
of 4 H. pylori clinical ID test, which one best?
Endoscope and biopsy
Urea breath test
Serum antibody test (blood)
Stool antigen test bc ID active infection
treatment of H. pylori
2 antibi
2 for symps
Amoxicillin and tetracycline
Antacid or proton pump inhibitor to help alleviate ulcer related symptoms (abdom pain and nausea)
Heal gastric mucosal inflam
prevention H. pylori
% younger and older people
spread via (2)
The exact way h.pylori infects someone is still unknown.
it may be passed from person to person through direct contact with saliva, vomit, or feces.
it may also be spread through contaminated food and water.
for this reason it is wise to wash hands thoroughly eat food that has been prepared properly and drink water from a safe clean source
According to the nih, 20% of people affected are younger than 40 years old, 50% are older than 60 years old
rates are higher in developing countries
most people with H.pylori infection never have symptoms; why this is remains unclear
Both campylobacter and helicobacter lab diag:
gram stain and morph (___ shape)
agar req
temp
CO2
fermentation
oxidation
catalase
Gram negative rods, curved S shaped
No growth on blood or macConkey agars
Campy agar is formulated for campylobacter growth– has 10% blood and antibiotics in it ( regular blood agar is 5% blood so this bacteria needs more nutrition)
microaerophilic:Requires high CO2 environment to grow because killed by O2 content of ambient air
prefers 42° C temperature, Which is higher than most bacteria
biochemical ID: nonfermentative, oxidase-positive, catalase positive
Pseudomonas
Source:
species of interest
do most cause disease
transmission—where/what is main source of infect
Found in soil, water as natural habitat–widespread in nature
Most pseudomonas species do not infect man
Those that do usually cause severe infections and are diff to treat
Species most freq associated with human disease is P. aeruginosa
P. aeruginosa Is found nearly everywhere and may be harbored in nearly any site in the medical environment such as Hospital water systems, Dental water lines
P. aeruginosa Transmission is in contaminated equipment (IV fluids, water, soap may be vehicles for transmission; easily spread from Patient to Patient via hospital personnel; best way to reduce spread in hospitals is to always use aseptic technique when working with patients and handling equipment)
Burkholderia
species of interest
disease and mortality rate
risk groups
symps and latency/ relapse cycle
Responsible for life-threatening human disease, Meliodiosis (Whitmore’s disease), which is characterized by pneumonia and multiple abscesses with a 40% mortality rate
bacterium found in the soil and water in tropical areas of Southeast Asia
Vietnam War veterans had exposure to this microbe, probably due to extensive exposure to what soils and surface water
high risk groups include farmers, laborers, indigenous groups and Adventure Travelers locations such as vietnam, thailand, Northern australia, Mexico
5 to 20% of agricultural workers have antibody to it meaning they have been exposed at some point in their life
can remain latent / no symptoms for a long time, up to several years, until relapse / recurrence of infection occurs
appears to be a relapse since the recurring infection is due to reactivation, not reinfection
thus, not encountering the organism again, only the organism is being harbored in the body
Burkholderia pseudomallei disease presentation
predisposing factors
clinical response
1 symp
transmission
chronic course (3 diseases)
Old age and a lower immunity predisposition tend to be the primary populations of infection
clinical response to therapy is usually slow, relapses are common
disease presentation: infection where an abscess forms and leads to aggressive granulomatous disease caused by:
ingestion or inhalation of contaminated dust
Soil contamination of abraded skin
Further abscess formation in lungs and other viscera
overwhelming and rapidly fatal septicemia can occur
chronic course resembles:
tuberculosis with pneumonia, multiple abscesses, osteomyelitis
One recent case in the us, long process to cure patient
Differentiate Pseudomonas from Enterobacteriaceae in relation to the fermentation of carbohydrates and media used for this differentiation.
on basis of fermentation, O2 req, glucose use, pigments
Pseudomonas lab diag:
Aerobic gram neg rods
Nonfermentative (15% of all GNR are nonferm)
Do not utilize glucose by ferm
Special media are needed to ID nonferm
Most freq isolated nonferm in clinical setting
Producer of pigments
Pyocyanin, fluorescein
Discuss the characteristic pigmentation and fluorescence of Pseudomonas aeruginosa; include appearance (color) of the pigment, what causes pigment production.
Producer of pigments: pyocyanin, fluorescein
Characteristic blue-green color (pyocyanin)
Fluorescent under UV
Occurs in vitro and in vivo (how first ID pyocyanin in wounds in 1850 french military–P. aeruginosa)
Takes E so not sure function (other than pyocyanin as a virulence factor)
Relate the susceptible/resistant nature of P. aeruginosa to antimicrobial therapy.
3 virulence factors—enzyme, 2 tox, invasion and biofilm prod
antibiotic rez
Determinants of pathogenicity (virulence factors)
proteases
Proteolytic necrotizing enzymes: hemorrhagic tissue destruction
corneal tissue destruction in eye infections
toxins
Pyocyanin
kills competing microbes and why it can become the predominant organism at a given site
generates reactive oxygen species such as H2O2 and superoxide anion
and activates catalase, and enzyme that breaks down H2O2 to become less toxic
endotoxin A: Necrotizing activity at site of colonization
hemolysins–RBC Hb lysed
contributes to invasiveness, especially in pneumonia (CF patients– leading cause of death; biofilm production p. Aeruginosa was first biofilm to be ID)
Antibiotic rez of p. Aeruginosa:
Intrinsic resistance to many antibiotics and acquired resistance to some
because of this resistance, it becomes a dominant organism present in the diseased area after other microbes are limited by the antimicrobial therapy
multiple resistance to drugs
Describe the types of patients that are more susceptible to Pseudomonas aeruginosa infections
risk groups
2 disease states
mortality if systemic
why leukemia patients are high risk
Clinical infection:
P. aeruginosa Infections usually occur in people with altered host defenses such as:
burn patients ( High incidents)
patience with malignant diseases
patients receiving Interventional treatments ( respirators, catheters, ventilators→ CF patients)
can in fact nearly any tissue or body site:
lesions or septicemia
lesions May spread via the bloodstream causing septicemia or systemic infection with high mortality up to 80%
eye infections of the corneal tissue may result in loss of vision in the eye
highly susceptible states such as leukemia patients, burn patients, CF patients with lung infections
leukemia patients: p. aeruginosa is the second most common cause of septicemia and Leukemia patients behind e coli, the most common
the major defense a leukemia patient has against p. aeruginosa is his or her own innate immunity– specifically phagocytosis ( when leukemia patients become severely leukopenic (dec WBC), they become highly susceptible to fatal infection
State the major host defense mechanism against Pseudomonas aeruginosa. (treatment)
2 topical antimic, or the oral antimic family (how admin too)
when infection is localized and external, treatment with topical antimicrobials such as polymyxin b or colistin is effective
use these antibiotics with some caution since each is toxic to the kidneys and thus is only used topically
if much necrotic tissue is present, it must be the debrided before topical treatment is effective ( burn patients)
abscesses must be drained if infection is under skin / abscesses by being lanced or getting a needle aspartate which can be used in cultures (burn patients)
multiple resistance to drugs
Methods used for administration of antimic:
topical for burns, wounds, eyes
systemic by ingestion or injection routes of administration
treatment consists of intensive antimicrobial therapy since P. aeruginosa tends to be highly resistant to antimicro
specific choice of antibiotic must be based upon the history of p. aeruginosa sensitivity in the community (antibiograms from location–changes)
Treatment of systemic pseudomonas Infection frequently consists of a combination strategy (penicillin and aminoglycoside)
This lowers the concentration needed of either to thus lower the benefit to risk ratio
When parenteral therapy needed, aminoglycosides such as tobramycin or gentamicin are used
parenteral= not through the alimentary canal (GI tract)-->IV admin
Contrast with eternal–”involves the alimentary canal” (esophagus, stomach, and intestine)-->oral admin
Penicillins such as carbonicillin, ticarcillin, piperacillin can also be used
Prevention and control:
A heptavalent vaccine has been developed for burn patients, proven effective in lessening incidents of infection
Describe the morphology of organisms of the genus Hemophilus when Gram stained and media req.
Small gram negative rods (coccobacilli)
characterized by requirement for specific growth factors that are found in blood (hemophilus means blood loving)
Very fastidious for growth
4 Hemophilus Species of importance:
H. influenzae
H. aegyptius
H. ducreyi
Gardnerella vaginalis (H. vaginale)
Describe the specific growth factors (X-factor, V-factor) required by organisms from the genus Hemophilus (i.e. what are they and from what source might they be obtained?).
Lab diag:
Requires nutritional factors directly supplied by Blood chocolate agar and the addition of V factor (NAD) and X factor (hemin=iron complex derived from hemoglobin)
Most organisms don't need both factors, but can grow on
Antibody reactivity
On a quad plate (used to ID hemophilus)
H. influenzae= no growth on NAD or hemin only, growth on hemin and NAD on regular media, and growth on blood media
State which growth factors are necessary for the growth of H. influenzae.
Blood chocolate agar and the addition of V factor (NAD) and X factor (hemin=iron complex derived from hemoglobin)
requirement for specific growth factors that are found in blood (hemophilus means blood loving)
Differentiate the type of meningitis caused by H. influenzae (that is, nonepidemic) and by Neisseria meningitidis (that is, sporadic or epidemic).
H. influez sero typing
most common cause of meningitis in kids
2 clinical infect
immunity in infants
Latex agglutination tests (test for what and how works)
H. influenzae sero typing:
Stereotyped into six groups utilizing capsular antigens for the typings of A-F
H. influenzae type B is the most common cause of acute bac meningitis in infants and children (seldom have detectable levels of bac antibody)
Non-epidemic—sporatic
Clinical infection H. influenzae:
Meningitis:
most serious disease produced by this bacteria is acute non-epidemic bacterial meningitis
type B is the most common cause
occurs in children from 3 months to 6 years of age– elderly individuals are also susceptible
disease progression: respiratory distress during period of bacterial invasion, followed by positive CSF culture, CNS deficits may result after recovery
Acute bacterial epiglottitis:
Occurs mostly in children between 2 to 7 years of age
infected epiglottis becomes swollen and may lead to closing off of the airway, which necessitates a trichotomy
septicemia May develop and be fatal
immunity: transplacental for infants aged 0 to 6 weeks after which time natural immunity May begin to develop– since and beginning stages, not substantial enough to prevent infection
Latex agglutination tests for causative agents of meningitis:
pos= agglitination from An-Ab reaction
helpful when time is of essence
Prevalence of H. influenza and N. meningitidis:
Neiserria in young, hemophilus in older adults, strep pneumo most overall
State the source, means of transmission and treatment/prevention of H. influenzae.
vaccine—what type does it protect against
source= humans are only known reservoirs
30% normal adults have in upper resp tract (not lungs)
transmission= human to human
Inhal of infected droplets from clinically active cases, convalescent (recovering), or chronic human carriers
treatment= ampicillin and chloramphenicol
Prevention: Hib vaccine
Protects against H. influenzae type B
An important cause of childhood meningitis and cause of bacterial pneumonia in children
estimated to cause 3 million cases annually
resistant to phagocytosis by alveolar macrophages, probably due to capsule
macrophages are white blood cells that perform phagocytosis and reside in specific locations, they are the first two ID invasion of a pathogen and raise alert to send out mediators/cytokines to recruit neutrophils
several different Hib vaccines are on the market, these vaccines are now part of routine childhood vaccination programs and more than 20 countries including the US
State the disease commonly caused by Hemophilus aegyptius. and bacillus name
differenciation
clinical infection (1)
epidemic? if so at what level
treatment
Koch-weeks bacillus
Differenciation:
H. aegyptiusNeeds to be differentiated from h.influenza serologically since both have the same culture and biochemical characteristics
Confirm suspicion that takes into account location ( eye= aegyptius, respiratory/csf = influenza)
Clinical infection:
Conjunctivitis ( pink eye)
can be at epidemic levels in kids
Treatment:
local administration of ophthalmic antibiotic solution
State the type of disease caused by Hemophilus ducreyi and identify the characteristic symptom of initial infection.
bacillus name
clinical infection (1, symp)
transmission
Chancroid bacillus
Clinical infection:
Venereal (STD) disease: chancroid
Initial infection causes formation of soft chancre (painful ulcerative sore on genitalia that bleeds easily if scraped)
Accounts for 10% of all venereal diseases
Transmission: direct contact (highly contagious)
Define and identify clue cells and state the disease associated with their presence.
what bac and disease is associated with these
% significant of infection
characteritsic appearnece of norm vs infect
Classification: was gardnerella vaginalis until became Hemophilus vaginale w/ DNA seq
Clinical infection:
Venereal transmission that is associated with vaginitis
Does not invade tissue–grows in vaginal secretions
ID:
Clue cells (if present indicate Hemophilus vaginale)=Squamous epithelial cells with adhered masses of gram-negative pleomorphic rods
normal vaginal cultures have lots of squamous epithelial cells which have more cytoplasm than a nuclear component
if more than 20% of the epithelial cells in a direct exam our clue cells, then significant for bacterial vaginosis
normal epithelial cells have a defined cell edge, flu cells have lack of a defined cell Edge due to bacterial adherence to the cell which obscures the borders
Describe the morphology of B. pertussis when Gram stained./ lab diag
O2 req
media
growth rate
sample collect
sero typing? if not what pref
Lab diag:
Gram neg rod
Strict aerobe
Req selective enrichment media w/ 15-30% blood (Bordet-Genou medium that is potato glycerol blood agar)
Slow grower: 2-5 days at 37 dec C
Current samp collect: nasopharyngeal sample on dacron/rayon swab (cotton doesn’t work)-->asses with PCR for fast turn around or fluorescent antibody test
Past method was cough plate (patient coughs directly onto bordet-gengou plate which is incubated and assessed for growth
Sero typing:
Bordella contains specific capsular (K) antigens–however, sero tests have not been stanardized or approved
Lack of association between serum antibody levels and protective pertussis immunity makes result diff to interp
Not used→instead PCR
Select another name for Bordet-Gengou medium and state the major component it supplies as a requirement for the culture of B. pertussis.
B. pertussis req selective enrichment media w/ 15-30% blood (Bordet-Genou medium that is potato glycerol blood agar)
State the common name given to the disease caused by B. pertussis.
toxin released, 3 steps of infect
transmission
Clinical infection: pertussis/ whopping cough
Following inhal of infected droplets via nose/mouth
Organism multiplies (infect estab) w/in the resp tract w an incubation period that varies from 5-21 days
After mult, organism aggregates on bronchial and tracheal lining and toxins are released
Exotoxin release causes bad adherence to cells and cytotoxicity and cell necrosis
3 stages of whooping cough
3 stages:
Catarrhal: most highly infectious period, lasts 7-14 days, upper resp involvement, mild cold like symptom, mild cough, sneezing, slight fever, runny nose
Paroxysmal: where name comes in; lasts 1-6 weeks, cough is paroxysmal (sudden intensification of symptoms) or spasmodic (sudden but transitory airway constriction)
Series of coughs so close together and forceful that the person cannot take a breath between coughs
At the end of the coughing spasm, person grasps for breath, which sounds like a whoop
Coughing may be so intense and severe that vomiting follows coughing episode
Young infants usually do not whoope–but may have anoxia (low O2), cyanosis, seizures, encephalopathy
Convalescence: lasts >1 mo, less severe and less freq paroxysms
Bordetella parpertussis
Another pathogenic species of bordetella that causes similar illness to whooping cough, but less common
source, mode of transmission (3), toxin (1), major symp, major complication (2) of B. pertussis
A. Source: usually children who pass among themselves, adults are reservoirs, major source is indiv w unregoc mild pertussis (misdaig with bronchitis, allergy, or walking pneum–symps not bad and have for mo)
B. Mode of transmission: inhal or direct contact w discharges from resp mucous memb of infected person, coughing aerosolized bac thereby transmit to sus indiv
C. Toxin production: Exotoxin release causes bac adherence to cells and cytotoxicity and cell necrosis
D. Major symptom: cough is paroxysmal (sudden intensification of symptoms) or spasmodic (sudden but transitory airway constriction)
Series of coughs so close together and forceful that the person cannot take a breath between coughs
At the end of the coughing spasm, person grasps for breath, which sounds like a whoop
Coughing may be so intense and severe that vomiting follows coughing episode
Young infants usually do not whoope–but may have anoxia (low O2), cyanosis, seizures, encephalopathy
E. Major complication
CNS disorders due to the anoxia have been associated with the disease
Encephalopathy
coma after anoxic episode
secondary infection: and the ears, sinuses, respiratory tract
secondary infection → Bronchopneumonia that can be severe → death
treatment and sus (usually performed or not) of B. pertussis
Treatment:
Erythromycin
susceptibility is not usually performed because of the characteristics slow growth of the organism
supportive treatment administered if needed like fluid and electrolyte management, and oxygen therapy to avoid anoxia
Describe the type of immunity provided by the DTP series (diphtheria, tetanus, pertussis).—vac and booster
active immunity
immunizations for diphtheria, tetanus, pertussis
DTap:Vaccine given to Children less than 7 years of age
TDap: booster immunization given at age 11 for continued protection because of pertussis reemergence
average duration of protective antibody titers following vaccination is 12 years, only a small percent of adults are immune to pertussis regardless of Prior vaccination history
reports indicate that 85% of all non-immunized children develop whooping cough in this percent is drastically decreased by vaccination
Describe the morphology of organism from the genus Brucella when Gram stained.
Gram neg rods found intracellular in macrophages
State the term given to the clinical condition associated with infection with organisms from the genus Brucella.
(one animal one human)
incidence
origin of bac
The genus Brucella is made up of bacteria that are intracellular parasites involving lower animals and are transmittable to man
Importance:
Causes contagious abortion and lower Ani 1-3 weekmals by brucella abortus
causes brucellosis or undulant fever and humans
fever is undulant = rise and fall like a wave
caused by brucella melitensis
Incidence:
Worldwide Wisconsin and mexico, africa, india, and Europe
Other names for brucella is multifavor, Crimean fever, Gibraltar fever which are named after the location
source, transmission (main way and 4 mechs), incubation, symps—unique one, treatment and prevention of brucella (melatensis) diseases
dissem or loc, intact or not in phagocytes, localized in what 2 RES locations
how long do symps last
what CNS symps can occur that are unsual
A. Source Infected animals or secretions like milk; animals may recover quickly but excrete bacteria for varying lengths of time in their milk
B. Mode of transmission
Ingestion– contaminated milk or milk products
consumption– insufficiently cooked meat from infected animal
direct contact– at risk populations are dairy men, farmers, veterinarians
inhalation– rare but has occurred in research lab workers
C. Incubation period 1-3 weeks
D. Major symptoms clinical infection begins with direct contact or ingestion
To initiate infection bacteria enters through the skin ( direct contact) or are ingested, disseminated through lymphatics and bloodstream, remain intact within phagocytes– especially macrophages– where they are protected from antibodies and other host defense mechanisms as well as antibiotics, may cause abscess formation and infected tissue, localized in the spleen and bone marrow
nonspecific manifestations: weakness, fatigue usually manifested late in the day, chills, sweating or night sweats, general malaise, anorexia, weight loss, abdominal pain, headache
intermittent fever commonly associated with undulant fever (unique)= undulating characteristic is probably related to endotoxin release
sometimes mental depression and increased nervousness
symptoms last 3 months to a year normally, but chronic brucellosis May last up to several years with relapses
complications: arthritis, endocarditis, neurological disorders
Treatment and prevention:
Tetracycline and or rifampin, alternative is choramphenicol
antibiotics: intercellular localization of bacteria May contribute to antimicrobic inefficiency or ineffectiveness
control animal infections( and meat from infected animals), pasteurized milk and milk products
Discuss the febrile agglutination test used in the laboratory identification of Brucella infection: include statement of antigens or antibodies in the patient’s serum for which you are testing, cross-reactivity of the test, diagnostic use and importance.
BSL level
ideal specimins
diag based on convalescent/acute Ab
titer inc to diag
Lab diag:
Gram negative Rod found intracellularly and phagocytes, or tissue
slow growing bacteria: may take up to 30 days to grow
BSL level 3
ideal specimens collected depending on symptoms: blood if fever, bone marrow, liver biopsy, lymph node aspartate, abscess exudate
serological test for antibody detection ( recommended by CDC)
febrile glutination test provides rapid results
detects presence of glutens or antibodies present in patient serum
panel of tests that rule in / out different diseases such as brucellosis, Rickettsial infections, salmonellosis, toleremia
besides test panels for several different bacteria, there are brucella specific agglutination tests: basis of the reaction=
Serum containing specific Ab from patient + brucella antigen on plate→agglutination upon combination (from Ab-An reaction)
Diagnosis based on acute and convalescent antibody;
During encounter one, first response is IGM that begins eliminating the antigen, secondly in the convalescent stage IGG will protect the body longer term and lead to Total elimination of bacteria ( in acute sample IGM will be high IGG will be low, and convalescent sample IGM will be low, IGG will be high)
during encounter two, IGM will not have a major defense but IGG will show increasing amounts and ultimately lead to faster recovery
Serum antibody titers during the disease progression must have a fourfold rise or greater between the acute and convalescent phase
acute and convalescent serum samples are the norm for diagnosis and the only test a hospital can do with such slow Growers that are BSL level 3
State the technical name and the common name given to the disease caused by Francisella tularensis.
Francisella tularensis is the causative agent of tularemia or rabbit fever
Describe the morphology of F. tularensis when gram stained.
and type of disease caused to whom
Gram neg rod found intracellular in macrophages (like brucella)--Acute infectious disease of wild animals, especially rabbits and ground squirrels
source, transmission (3), symps and incubation, progression, treatment and prevention of tularemia
in what cases is mortality higher
A. Source: Rabbits, rodents reservoirs
B. Mode of transmission
Ingestion of infected meat or contaminated water
inhalation of aerosols containing F. tularensis
Direct contact: most common mode of transmission in the US
handling contaminated animals or infected carcasses
bites of insects vectors
predominantly in the Midwest
Recent case in 1984 involving Native Americans where they were able to treat all patients
C. Major symptoms
Disease progression:
incubates 2-10 days
Bacteria invades tissue, infects most cell types primarily macrophages– entry into macrophages occurs by phycocytosis
harbors and macrophages by sequestering in the phagozone, breaks out of phagozone into the cytosol where it rapidly proliferates
infected macrophage undergoes apoptosis which releases bacteria that initiate new rounds of infections
Regional lymph glands become infected, drain into lymph nodes or bacteria enter the bloodstream
because cytosis and bloodstream and just bacteria and cycle starts again, this is how bacteria spread systemically
Symptoms:
sudden fever– febrile disease
Chills, headache, exhaustion, back pain, Progressive weakness leading to incapacitation for 6 months
Treatment and prevention:
Streptomycin
without antimicrobic treatment, fatality rate is 5 to 15% unless there are pneumonic or septic conditions which increases rate to 30 to 60%
avoid infected animals, wash hands often and well after handling infected animals or contaminated carcasses, cook food thoroughly and be sure to drink water from safe source, use insect repellent containing Deet to prevent insect bites, be vaccinated if there's High exposure to infected sources ( animal handlers, laboratory personnel)
Name and describe the 7 clinical types of tularemia.
which three from direct contact, which two with higher mortality
Ulceroglandular (direct contact): 40 to 80% of all cases and predominant way of transmission, cutaneous / surface level ulcer develops at site of infection, regional lymph nodes become swollen and painful ( lymphadenopathy) due to bacterial transport by macrophages
Oropharyngeal infection: pharyngitis, tonsillitis, swelling of lymph nodes– can be due to ingestion
Oculoglandular (direct contact): . purulent conjunctivitis, similar to ulceroglandular except that conjunctiva is a primary site of infection, usually results from rubbing eyes with contaminated fingers
Glandular (direct contact): Regional lymphadenopathy ( swollen lymph nodes) with no skin lesions ( no ulcers)
pneumonic (Fatality rate without antimicrobics is 30 to 60%, with treatment is less than 2%): severe form of disease, pleuropulmonary disease with aerosol inhalation
Ultimately: septicemic ( fatality rate without antimicrobics is 30 to 60%, with treatment is less than 2%): said septicemia, diarrhea, vomiting, May rapidly lead to shock, DIC, ARDS or acute respiratory distress syndrome, death
typhoidal: focus of infection and mouth, throat, GI tract, systemic illness with fever with toxemia in liver, spleen, can be do to ingestion of bacteria
Explain why laboratories forward cultures of suspected cases of tularemia to reference labs.
BSL
techniques to ID (4) — which two are the main ones
growth req
specimen selection
fold inc in titer test to diag
Lab diag:
PCR is technique usually used
organism detection and identification:
growth on blood agar and chocolate agar– very fastidious, small and sparse growth on plates
48 to 72 hours
specimen appropriate for culture is symptom dependent: ulcer biopsy ( advancing edge, which is where the progression at wound is evident and where higher number of organisms causing infection are present), lymph node aspartate, or other like blood, csf, throat swab
BSL level 3
serological test for antibody detection
most commonly used lab ID to test
elevated serum antibody titer of francisella tularensis antigen ( for folder greater change in titer) and a patient without history of tularemia vaccination in conjunction with compatible clinical presentation is a probable case of tularemia
determined by ELISA or agglutination reactions
Describe the morphology of P. multocida when Gram stained.
optimal specimen (2)
2 other lab diag tests
Gram negative rod
optimal specimen source is symptom dependent: exudate from lesion/needle aspartate, or blood if fever is present
cultural and biochemical identification
State the source (2) and mode of transmission (3) of P. multocida.
source= cats, dogs
transmission= licks, bites, scratches
80% of cat bite infections have____, and it is also part of normal flora
highly pathogenic for ___, which are natural hosts
is the bacteria mentioned above common in well managed pets?
Highly pathogenic for animals which are natural hosts
uncommon and well-managed and properly cared for animals
normal flora of a dog's mouth has greater than 60 bacterial species (much like man)
80% of cat bite infections have P. multocida
How organisms are introduced→ many organisms can be source of infection, some are more pathogenic than others
Pasteurella ___ is the only species that infects man and is transmitted from animal to man via animal bites or scratches (dogs and cats all have potential to transmit but not all do)
multocida
disease name of infection with P. multocida.
clinical infections (2)
complications (3—one esp if deep bite)
treatment (2 antibi and 2 clinical prevention actions—don’t what)
disease= pasteurellosis
Clinical infection= cellulitis and abscess formation at the sire
complications= sepsis, meningitis, osteomyelitis (esp if bit is deep and thus more likely it will hit an artery or vein and get into bloodstream)
treatment=
Clean wound and avoid suturing if possible ( can make region unable to be washed and less reachable by topical antibiotics, thus wound gets worse)
initiate antibiotics such as penicillin or tetracycline ASAP
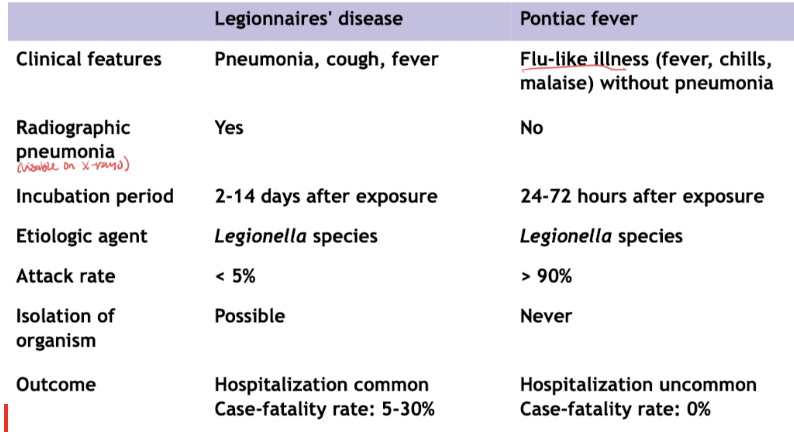
lab diag of legionella pneumophila: gram stain, mechanism of evading host defense
clinical diag: compare legionnaires disease vs pontiac fever (which one radiographic pneumo, hospitalization, higher fatality rate, pneumo-related)
Lab diag:
Gram negative rod
able to enter, survive, multiply within host cells– especially macrophages and neutrophils ( our phagotic cells now protecting from detection as for microbes and thus prevents phagocytosis)
Clinical diag:
radiographic pneumonia ( visible in x-ray)= Legionnaires disease; hospitalization is common and fatality of 5-30%
Pontiac fever= flu like illness without pneumonia
State the source (primary source, tolerance for what, op temp, greatest concern locations) and mode of transmission of Legionella.
source=
Water supplies, especially in water holding bats
Legionella has a tolerance for chlorine and therefore can gain entry into water supplies (usually used to decrease bacterial numbers)
Water systems which maintain water temperatures between 20 to 50° C are conducive to growth of legionella, particularly where there are opportunities for formation of biofilm layers on surfaces
of greatest concerns are:
cooling water towers of air conditioning systems, heat exchangers, supplies of portable tap water and shower water, hot water systems, evaporative condensers, whirlpools, humidifiers
transmission= Primarily inhaled of infected water droplets/aerosolized sized particles ( air conditioner)
Case study: when ID “Legionnaires disease”
risk pops, epidemic locations now (4)
First recognized as disease after an outbreak at the Bellevue Stratford Hotel in Philadelphia during the summer of 1976 where the 58th annual Convention of American lesion was held and many developed symptoms and died.
evidence exists that prior epidemics and deaths have been caused by Legionella
epidemics continue to occur in are often associated with hotels, cruise ships, hospitals, supermarkets
populations of risk are: people with pre-existing respiratory disease, diabetes, renal disease, malignancy, elderly or immunocompromised, heavy smokers or drinkers ( all of which were a large population of the hotel in 1976)
Clinical infection of legionellosis (2 of varying degrees, asymp possible? 2-15% ___-acquired pnemo, range of symps)
from mild upper respiratory tract infections to pneumonia
causes 2 to 15% community acquired pneumonia
asymptomatic affections can occur
legionellosis is associated with two clinically and epidemiologically distinct illnesses:
Legionnaires disease ( predominant)-- fever, myalgia, cough, pneumonia
Pontiac fever– a milder illness than legionnaires with no pneumonia
treatment of legionellosis
Erythromycin or erythromycin/rifampin combination
most common transmission mode of F. tularensis
direct contact
3 direct contact clinical forms of tularemia and what makes each of them distinct from the others
granular (no ulcers)
ulceroglandular (most cases)
oculoglandular (conjunctival)
2 injestion forms of tularemia
typhoidal
oropharyngeal
is susceptibility testing usually done on B. pertussis? why?
no bc characteristic slow growth (2-5 d)
avg duration of protective Ab titers of B. pertussis
12 yrs
causative agent of brucellosis and common name of disease
undulating fever
B. melitensis
B. melitensis is transmitted indirectly mostly via
secretions contam, like milk
most common lab ID test for F. tularensis
sero tests/ Ab titer elevation and ELISA or agg rxns
primary transmission mode of P. multocida
dog or cat bite/scratch; can be lick too
optimal specimens for gram (-) rods tend to be ___ dep
symptom
why is legionella found in its source
water supplies—bc chlorine tol and 20-50 deg C op temp for growth
Legionella disease type that is worse and which is most common:
Legionnaires’ disease
pontiac fever
Legionnaires’ disease—worse bc pneumo
pontiac fever—more common
is isolation possible in legionnaires disease or pontiac fever
legionnaires disease
which legionella disease incubates for 24-72 hrs instead of 2-14 days
pontiac fever
sero typing for B. pertussis is done on what basis; is it often used?
K (capsular) antigens but not used bc of lack of association w/ serum Ab levels to inc protective immunity thus makes diff to interp results
what bac releases endotoxin in waves that lead to rise and fall of fever
which bac releases exotox to adhere to cells
Brucella melitensis
Bordetella pertussis
what stage of whooping cough is most contagious
catarrhal (stage 1)
stage and 2 hallmarks of whooping cough “cough”
paroxysmal (stage 2)
paroxysmal and spasmodic
how does H. influenzae type B evade alveolar macrophage phagocytosis
encapsulation
koch-weeks bacillus
H. aegyptius
chancroid bacillus
H. ducreyi
what helps ID H. vaginale and why
clue cells; found in vag secretions bc don’t invade tissue
what bac req most % blood (15-30) of the bac we have seen
name of media used
B. pertussis
Bordet-Gengou medium
H. influenzae uses antigens from where to serotype
capsule
most common cause of acute bac meningitis in children, and is it epidemic?
influenzae type B
not epidemic
what is causative agent of ulcers
H. pylori
definitive test of choice for H. pylori
stool antigen test
what bac is urease pos (can be used to ID)
H. pylori
what long-term infection leads to 2-6x risk for gastric and lymphatic cancer
H. pylori
what 2 GI infections do ppl mostly remain asymp (underreport)
H. pylori and C. jejuni
El Tor vs Classical V. cholerae
which one occurs globally
which one was involved in Haiti
which one has worse symps
which one has most carriers
which one occurs globally—T
which one was involved in Haiti—T
which one has worse symps—C
which one has most carriers—T