NAPLEX: Pediatric conditions
1/118
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
119 Terms
neonate is classified as
0-28 days
infant is:
1 month-12 months
toddler is:
1-2 years
a child is:
2-12 years
Adolescent is:
13-18 years
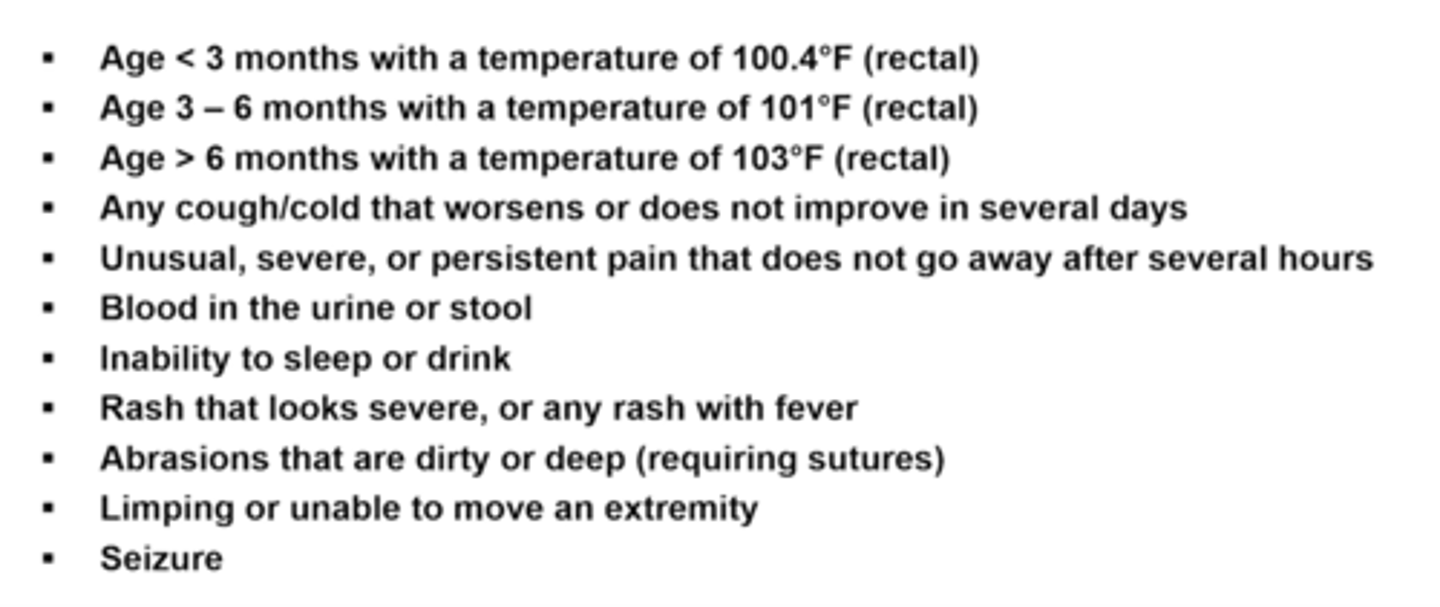
Seek urgent care with a child <3 months when
a temp. of 100.4F/38C (rectal)
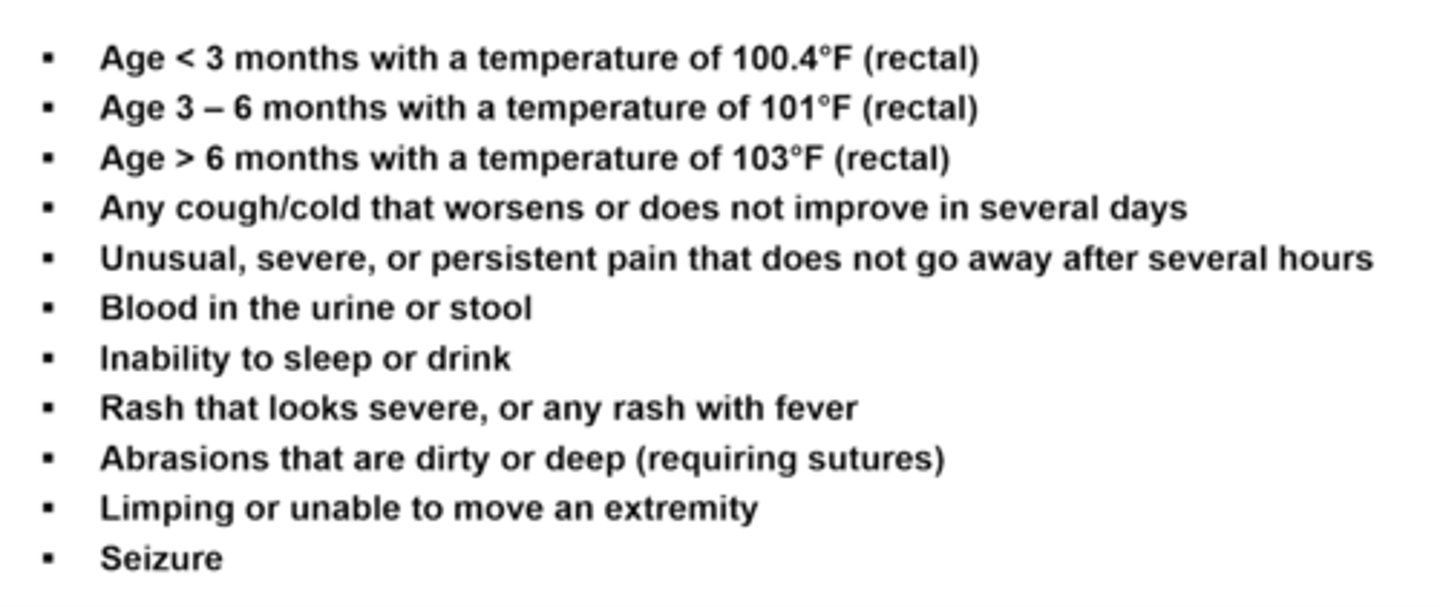
seek urgent care w/ age 3-6 months when
temp 101F/38.3C (rectal)
seek urgent care >6 months when
temp. 103F/39.4C (rectal)
Seek urgen care for a child any age when:
cough/cold worsening not improving for several days
unusual persistent pain not going away several hours
blood in urine or stool
inability to sleep or drink
rash that looks severe or any rash with fever
abrasions/cuts dirty or deep (requiring sutures)
limping/unable to move extremity
seizure
T/F: A household spoon can be used to measure medication
False: Never, oral syringes preferred, dosing cups can be used too
A newborn's general condition is assessed with an_____
A lower score indicates
apgar score
lower score requires more medical care.
newborns:
apgar score of <7 means
medical distress, immediate medical intervention needed (eg, resuscitation)
Standard meds given at birth include
vitamin K to reduce bleed
erythromycin opthalmic to prevent conjunctivitis
hepatitis B vaccine
light therapy for jaundice if needed
low apgar scores in pre-term infants are usually due to:
immature lung and heart development
Drugs that can be used to cause the ductus arteriosus to close
NSAIDS like indomethacin or ibuprofen
work by blocking PGs that keep PDA open
preterm baby conditions + treatment
patent ductus arteriosus (PDA) - NSAIDs to close
persistent pulmonary htn of newborn - supp care, inhaled NO
resp distress syndrome - surfactant (curosurf, infasurf)
NSAIDs are avoided in the third trimester of pregnancy because they can
cause the PDA to close prematurely
NSAIDS for closing the PDA must be administered within ____ of birth
14 days
Persistent Pulmonary Hypertension of the Newborn (PPHN) may be linked to
in utero SSRI exposure
Respiratory distress syndrome is caused by
a deficiency of surfactant production in lungs (not fully developed)
Most babies born <35 weeks gestation will receive _____ immediately after birth or within first few days of life due to under-developed lungs
surfactant
Surfactant names can be recognized with
Surf or -actant in the name
Aspirin and salicylate-containing products (bismuth subsalicylate) cannot be used in patients <_____ years old including infants due to
<16
Reye's syndrome
acetaminophen dosing for infants
10-15 mg/kg/dose every 4-6 hours
max 75mg/kg/day
T/F: An infant can safely take pepto bismol since they don't appear to be sick
False. don't recommend salicylates for patients <16, it may not be apparent they are recovering from a viral illness and its use is associated with Reye's syndrome
T/F: Acetaminophen infant drops and children's suspension are the same concetration
true - to help reduce dosing errors
ibuprofen drops and suspension are supplie din different dose strengths for infants and children!!!
Age to avoid ibuprofen: <___
due to risk of _____
<6 months
risk of nephrotoxicity
ibuprofen dosing for infants
5-10 mg/kg/dose every 6-8 hours
Medication for infants experiencing intestinal gas
simethicone drops
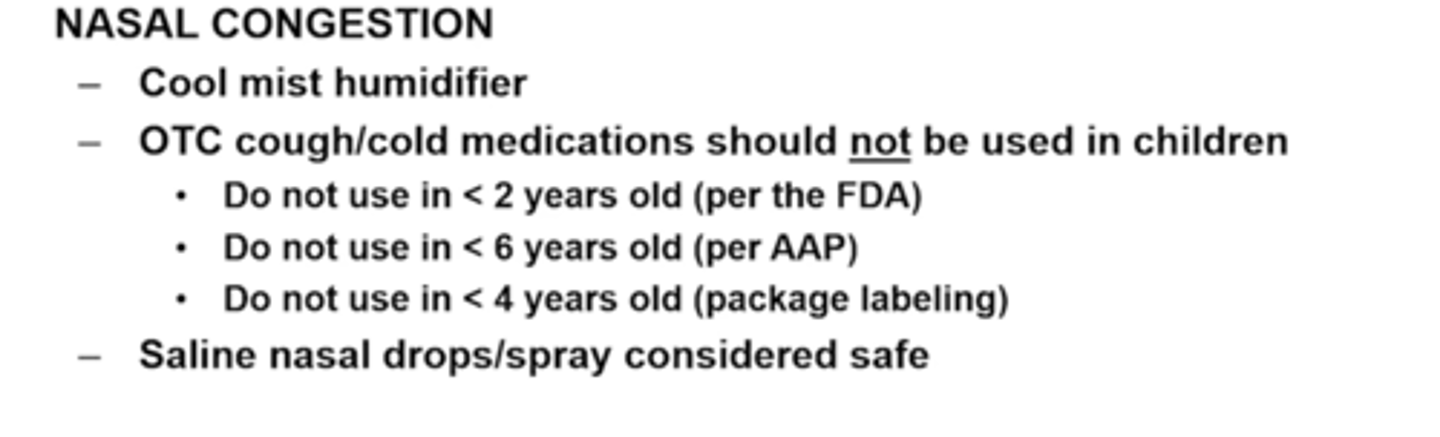
non-pharm suggestions for nasal congestion
cool-mist humidifier near bedside can help reduce, esp. in winter
sit in the bathroom while a hot shower creates steam (avoid burning skin)
gently suction with saline drops/spray to loosen mucus
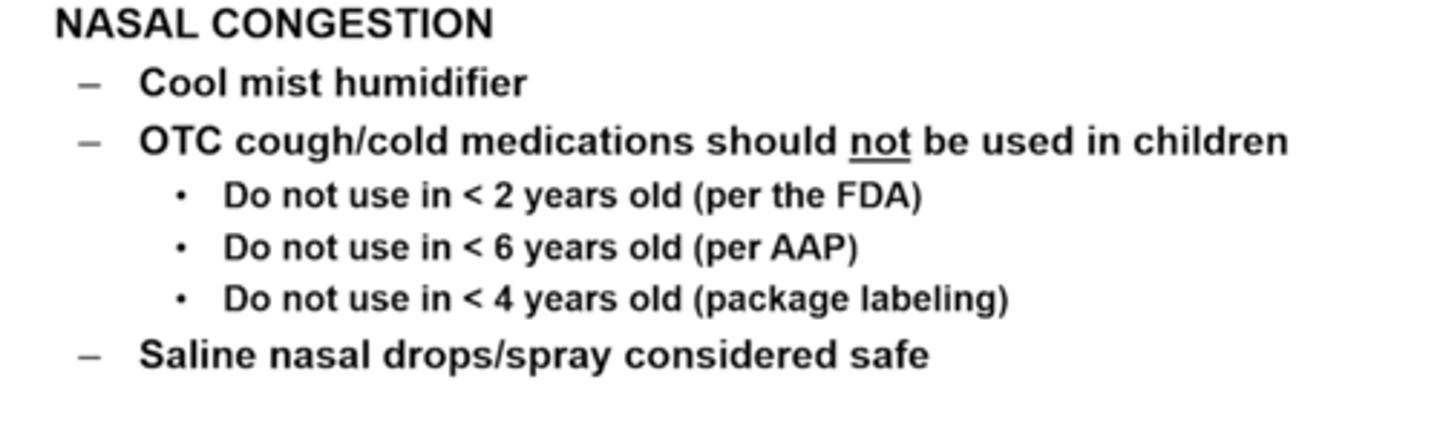
T/F: Most OTC cough and cold medications are available for children <2 years old
False: THE FDA DOES NOT RECOMMEND OTC COUGH AND COLD MEDS TO CHILDREN <2 years old
Treatment of intermittent constipation in children
Miralax (polyethylene glycol 3350) - takes a while
prunes
glycerin suppositories (pediatric size, OTC) for quick relief)
if ongoing, see a pediatrician
miralax should not be used in infants <_____ old
____ can be used instead
<6 months old
glycerin
Oral rehydration solutions for diarrhea
pedialyte and enfamil enfalyte
Antidiarrheal medication _____ is not recommended, risk of reye's syndrome
bismuth subsalicylate
loperamide is not recommended for OTC use in children
Acetaminophen (children's tylenol/infant's fever reducer) dosing (and max/day)
10-15 mg/kg dose every 4-6 hours
(max 75 mg/kg/day
ibuprofen (infants' advil/motrin, children's suspension) dosing, max, and age indication
5-10 mg/kg/dose every 6-8H
(max 40mg/kg/day)
6 months+ indication
concentration of children's tylenol
160mg/5mL
ibuprofen for infants has a caution for
nausea
simethicone for infants should be administered
after meals and at bed time
can be mixed w/ water, formula, liquids and shaken prior
How should parents be instructed to alternate tylenol and ibuprofen
keep at least 3 hours between any doses, and at least 6 hours between doses of same medication
ibuprofen can be given before bed to help with sleep (lasts longer)
constipation:
<6 mos
>/= 6 mos
age >/= 2
>/= 6 yrs
<6mos: glycerin supps
>/=6mos: miralax or glycerin (quick relief only)
>/=2yrs: above + mag hydroxide, docusate, senna, rectal enemas
>/= 6 yrs: above + bisacodyl supps and mineral oil
constipation:
when should rectal enemas (eg. sodium phosphate, fleet, pedia-lax) NOT be used in children? why?
<2 yrs old
severe dehydration, electrolyte abnormalities
A diagnosis of bacterial meninigitis is made based on
lumbar puncture
(nuchal rigidity may be present in some cases but cannot make the final dx)
Empiric treatment in neonates with a fever is:
ampicillin PLUS
either ceftazidime, cefepime, or gentamicin
T/F: Ceftriaxone is a good alternative to patients who cannot tolerate ampicillin in their empiric meningitis regimen
False: it's avoided in neonates since it displaces bilirubin from albumin, causing brain damage (kernicterus), and can precipitate w/ Ca-containing solutions
Antibiotic avoided in neonates due to kernicterus and forming precipitates with solutions containing _____
Ceftriaxone
precipitates with solutions containing Calcium
Once a patient is no longer a neonate, then bacterial menigitis regimen switches from ________ to _____
ampicillin + cefotaxime or aminoglycoside (gent)
to
vancomycin plus either ceftriaxone or cefotaxime
bacterial meningitis treatment by age group
<1 month (neonatal)
1-23 mos
2+ yrs
amp + cefotaxime or aminoglycoside
vanc + 3rd gen ceph (ceftriaxone or cefotaxime)
vanc + 3 gen ceph (ceftriaxone or cefotaxime)
RSV can be deadly in:
premature babies and neonates
RSV is a common cause of
bronchiolitis (swelling and mucus build up in bronchioles
treatment for RSV is
primarily supportive
if severe: inhaled ribavirin
rsv prophylaxis is recommended:
pregnant patients 32 to 36 weeks gestation to protect Infants < 6 mos
If mother was not vaccinated, RSV prophylaxis is recommended during RSV season
what is available For RSV prophylaxis?
Nirsevimab (beyfortus)
pavlizumab (synagis)
whe is nirsevimab (beyfortus indicated)?
pavlizumab( synagis)?
bey:
Virazole is used for
severe RSV (inhaled ribavirin)
Pavlizumab is used for:
1st year of life:
preterm infants, esp if chronic lung dx
2nd year: preterm with cld
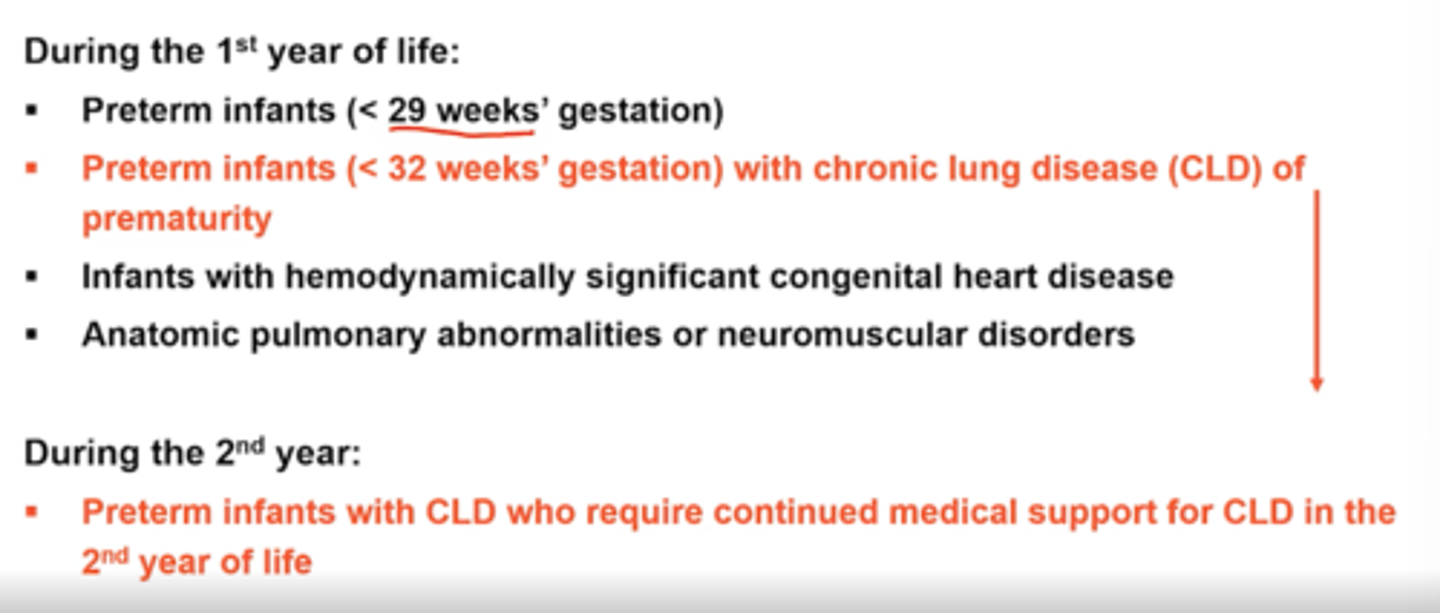
Synagis is dosed _____ and given ____ at the _____
monthly and given IM at the anterolateral thigh muscle
Patients should not receive more than ______ doses of palivizumab during the RSV season
5 monthly doses
T/F: If the baby becomes infected with RSV, give double doses of palivizumab
False: If a baby becomes infected, do not give ANY MORE doses of palivizumab
nirsevimab (beyfortus) is used for RSv prophylaxis. how is it given?
SINGLE im dose given in anterolateral thigh muscle
Croup is usually due to a________
viral infection
Croup affects the
upper airway (laryns, trachea, bronchi
Hallmark signs of croup
inspiratory stridor (high pitched breathing sound), barking cough, hoarseness
croup is most common in:
children <6
Mainstay of croup treatment
Systemic steroids (dexamethasone) +/- racemic epinephrine (if severe)
which isomer of epinephrine is the active isomer
L-isomer (levo)
What to use if racemic epinephrine is not available
L-epinephrine is used (use half the dose)
how are steroids (which one) dosed in croup?
SINGLE dose dexamethasone
0.6mg/kg PO/iv/im
nebulized Epinephrine is a (agonist/antagonist)
adrenergic agonist
Epinephrine MOA
relaxes bronchial smooth muscle, causes bronchodilation
racemic epinephrine dose and diluted in what
0.05-0.1 ml/kg max 0.5 ml (usually just give this) in NS
Term for "bed-wetting"
nocturnal enuresis
what age is bed wetting treated?
>5 years old
non-drug treatment for nocturnal enuresis
positive reinforcement
establishing daytime voiding patter/normal hydration pattern
alarm therapy
T/F: Bladder training exercises can improve nocturnal enuresis
false: These are not recommended. Embarassment should also be minimized
Next steps if behavioral methods are unsuccessful after 3 months
alarm therapy
alarm therapy with desmopressin
Only preferred medication for enuresis
desmopressin tablet
desmopressin drug class
synthetic analog of ADH (decreases nocturnal urine production)
T/F: Desmopressin nasal spray and injections can be used for enuresis
false: These are more commonly used for diabetes insipidus and hemophilia A
Contraindications to desmopressin
hyponatremia
boxed warning to desmopressin
severe, life-threatening hyponatremia can develop
side effects of desmopressin
headache
Codeine is metabolized to morphine by:
CYP2D6
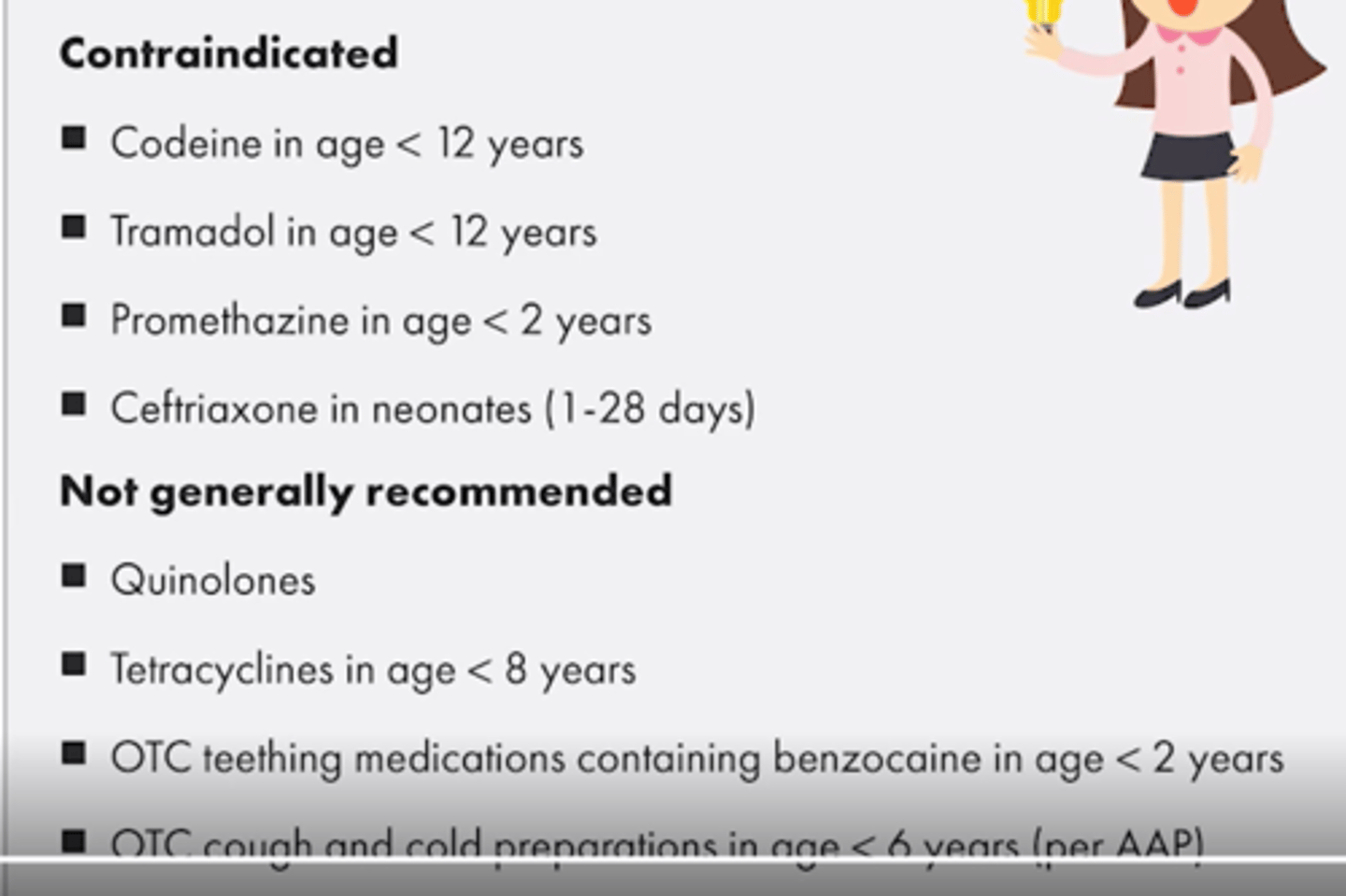
Codeine is contraindicated in:
all patients <12
patients <18 after tonsillectomy adenoidectomy
Prescription cough and cold meds with codeine or hydrocodone are no longer indicated in patients
<18
promethazine is contraindicated in
children <2
promethazine is limited in use to young children due to
potentially fatal respiratory depression
in addition to ceftriaxone, these antibiotics are not recommended in pediatric patients, but due to adverse effects on cartilage, bone, and muscle
quinolones
tetracyclines are not recommended in
children <8
tetracyclines have limited use in children because they:
can stain teeth, and deposit into bone and cartilajge
exception to limiting tetracyclines for patients 8+
tick-borne rickettsial diseases- doxycycline is the most effective and benefits may outweight cons
FDA recommends against the use of ________ in patients <______ for help with teething
benzocaine <2 years old
Benzocaine-containing teething products carry a risk of
methemoglobinemia
tramadol is contraindicated
in age <12
ceftriaxone is contraindicated in
neonates (1-28 days)
A patient is 3 years old and has a cough. Are there any safe cough/cold medications they can be recommended?
yes. OTC cough and cold preparations in age <2 are recommended against though, but this patient is three. there are likely some recommendations safe for use.
Common culprits of accidental overdose in children
iron, acetaminophen
(sulfonylureas can also be very fatal)
CI in pediatrics + ages