Dental Anatomy 2 - Final Exam
1/27
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
28 Terms
TMJ
Bilateral ginglymodiarthroidal joint
Ginglymo (hinge rotation) - Open and close around horizontal axis; teeth separation and occlusion with no positional change
Diarthroidal (translation) - When rotation ends, inferior head of lateral pterygoid pulls condyle forward against articular eminence
Upper compartment (translation) - superior surface and temporal bone
Lower compartment (rotation) - inferior surface and condyle
Mandibular Movement Steps
Opening
Depressor muscles contract, elevators relax, hinge movement begins
Pure hinge movement stopped by temporomandibular ligament
Inferior head of lateral pterygoid contracts, pulling disk and condyle. Digastric and hyoid muscles contract
Condyle slides on crest of eminence as inferior head of lateral pterygoid relaxes
Closing
Temporalis contracts to move mandible back and up
Superior head of lateral pterygoid contracts to bring disc to anterior surface of condyle
Depressor muscles relax
Elevator muscles contract to pull condyle up until condyle hits superior position
Anatomical Planes and Axes of Rotation
Horizontal Plane
Rotation of the horizontal axis - Hinge motion. Horizontal axis is called terminal hinge axis when condyle is sitting in mandibular fossa.
Frontal Plane
Rotation of frontal (vertical) axis - One condyle moves anteriorly while other condyle remains in terminal hinge position. Considered unnatural because of articular eminence inclination.
Sagittal Plane
Rotation of sagittal axis - One condyle moves inferiorly while other condyle remains in terminal hinge position. Considered unnatural because of musculature and ligaments of TMJ.
Translational Movement
Teeth, condyles, and rami move in the same direction and to the same degree
Mandible moves slightly forward during opening.
Usually, both rotation and translation occur simultaneously (When mandible rotates around an axis, the axis is also translating)
Ligaments of TMJ
Temporomandibular Ligament
Outer oblique portion limits opening movement
Inner horizontal portion limits posterior movement
Stylomandibular and Sphenomandibular Ligaments - Limit opening and anterior movement
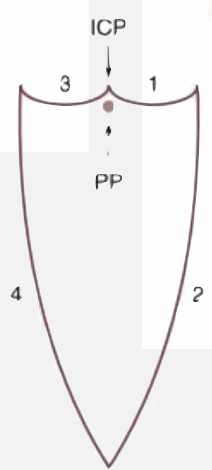
Sagittal Plane Movements
Represented in Posselt’s Triangle
Posterior Functional Border Movement
Anterior Functional Border Movement
Superior Contact Border Movement
Mastication
Posterior Functional Border Movement
Two stage hinge movement:
Stage 1 - Pure rotation while condyles are in CR (20-25 mm)
Stage 2 - Rotation while condyles move anteriorly and inferiorly (causes axis of rotation to translate)
Maximum opening stopped from capsular ligaments (40-60 mm)
Anterior Functional Border Movement
Condyles remain in anterior and inferior position
Pure hinge motion moves mandible from maximally opened to maximally protruded position
Ligaments pull condyles slightly posteriorly as mandible moves to protruded position
Superior Contact Border Movement
Determined by occluding teeth surfaces
Factors causing delineation include:
CR and MIP variations
Cusp inclination steepness
Overjet and overbite
Maxillary anterior teeth lingual surface anatomy
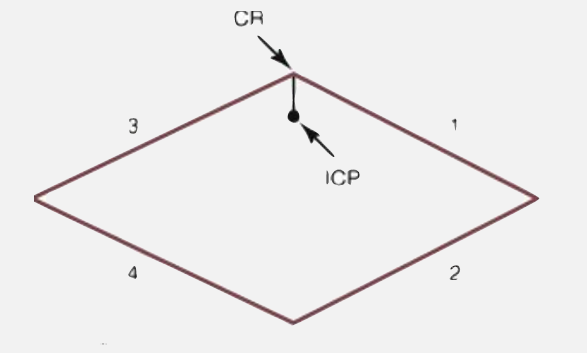
Horizontal Plane Movements
Recorded by Gothic Arch
Left Lateral Border
Continued Left Lateral Border
Right Lateral Border
Continued Right Lateral Border
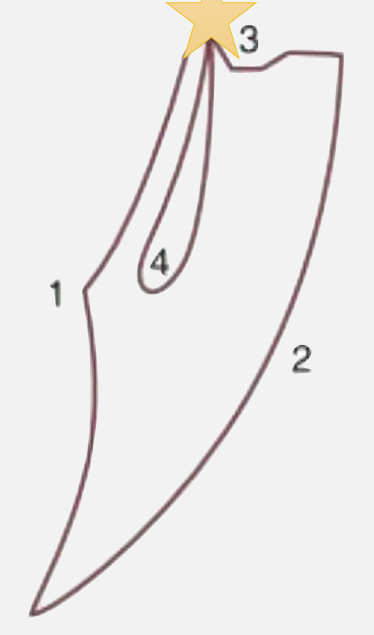
Frontal Plane Movements
Makes a shield pattern
Left Lateral Superior Border
Left Lateral Opening Border
Right Lateral Superior Border
Right Lateral Opening Border
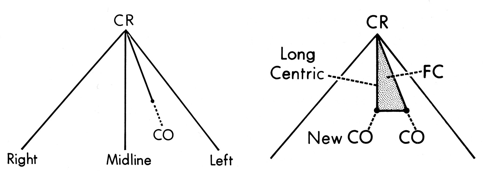
Gothic Arch Tracing
CR-CO should be down midline and be short
If adjusted, long centric or freedom in centric may occur which is undesirable and may need orthodontic treatment
Anterior Guidance
Anterior teeth protect the posterior teeth and TMJs during excursive movements through posterior disclusion
Effects of anterior guidance are most on premolars
Anterior teeth are protected by distance from TMJ because forces are closest near joint
Condylar Guidance
Functional relation of hard and soft tissue in TMJ
The steeper the articular guidance, the taller the cusps may be
Anterior guidance must be equal to or greater than condylar guidance for excursive movements
Mandibular Movement Rules
Memorize Picket Fence of Dentistry
Tooth types occlude with the same tooth type of opposite jaw (ex: first premolars only occlude first premolars)
Arrows on maxillary quadrant represent direction of mandibular movement; arrows on mandibular quadrant are opposite of mandibular movement
Side of lateral excursion is working side; side opposite of lateral excursion is non-working (balancing side)
Arrows pointed to supporting cusps are balancing movement; arrows pointed to non-supporting cusps are working movement
Specific rule: If arrow is on mandibular teeth image and it is pointed mesiobuccally or mesiolingually, the mandibular movement is considered non-functional
Occlusal Analysis
Systematic examination of occlusion that considers the interocclusal relations of mounted casts
Cast Analysis exercise is used in diagnosis, planning, and treating prosthodontic and TMD patients
CR vs MIP Scenarios and Articulator Settings
Centric Relation
Reorganize the occlusion, including vertical dimension
All teeth will be treated by indirect restorations
When doing occlusal analysis or establishing a new occlusal plane
Settings: Latched; Pin should not touch surface
Maximal Intercuspal Position
Stable occlusions restored in the present mandibular position
No changes to occlusal plane or vertical dimension of occlusion
Settings: Unlatched; Pin should touch surface
Diagnostic Mounting and Occlusal Analysis Form
Articulator Condylar Element Settings - How much inclination set on articulator
Wear - Identify all wear facets (wear line or plane caused by attrition) in teeth
Centric Occlusion - Verify that CO records is same as what is in the mouth. Check first occlusal contacts. If there is mismatch, restart everything :(
Maximum intercuspation - Are condyles fully seated in fossa
Mandibular Displacement - Measures displacement in mm between CR and MIP
Vertical displacement is measured by marking maxillary incisor edge in mandibular teeth
Horizontal displacement is measured by marking vertical line on reference point in posterior teeth (mandibular is fixed so additional markings are done on maxilla)
Frontal displacement is measured with vertical line between central incisors
Indicate laterotrusive and mediotrusive contacts - Healthy occlusion does not have contacts
Indicate protrusive interferences - Healthy occlusion has anterior teeth contact for anterior guidance
Overbite and overjet distance (measured in MIP)
Anterior teeth coupling - Is there anterior guidance?
Based on the above, decide whether treatment is needed
Diagnostic Cast Armamentarium
Diagnostic Mountings
Red, Blue, and lead Pencil
mm ruler
Shimstock - Identifies first point of contact
Accufilm II (red/black) - Marks contact
Never discussed tbh:
Boyle Gauge
Cleoid/Discoid
Fiberglass eraser and or scalpel
Occlusal Disease
Deformations or disturbances that prevent occlusion
Signs precede symptoms and damage progresses if not treated early
Destructive dental disorder causing tooth loss, discomfort, and decreases orthodontic longevity
Tooth Deformation Mechanisms
Stress - Produces compression, flexure, and tension resulting in fractures and abfraction
Friction - Occlusal surface wear in the form of attrition and abrasion
Corrosion - Chemical/electrochemical degradation (usually with pH < 5.5) appearing as cupped-out dentin area usually on posterior teeth. Caused by:
Bulimia - Enamel loss of lingual surface of anterior teeth
GERD - Enamel loss of lingual surface of molars where gastric acid could pool
Gingival crevicular fluid - Acidic pH affects non-carious cervical lesions
Attrition, Abrasion, and Abfraction
Attrition
Aka bruxism
Usually on lower anterior teeth
Matching wear facets
Anterior Guidance Attrition - Wear on lingual enamel on maxillary anterior teeth
Abrasion
Caused by continuous food chewing, excess toothbrushing or use of foreign objects
Abfraction
Stress-induced, non-carious cervical lesion
Another theoretical cause is toothpaste abrasion
Splayed Anterior Teeth
Forward deflection of mandible from posterior incline interference
Should be treated early by eliminating the deflective interferences
Early stages of teeth splaying may present with fremitus and sore teeth
Also caused by thick lingual restorations of the maxillary anterior teeth and over-contoured mandibular teeth restorations
Advanced Occlusal Disease
Combination of attritional wear and shifted teeth
Destroyed Dentition
Includes severe wear, teeth fracture and elongated alveolar processes
Sensitive Teeth
Occlusal overload produces sensitivity due to pulpal hyperemia or the presence of surface micro-cracks. Exaggerated effect causes soreness
These teeth are vital; occlusal adjustment provides immediate relief
Split Teeth and Fractured Cusps
Cusp incline hitting strong occlusal forces causes fracture lines
This sign precedes cusp fracture or split tooth
Painful Musculature
Deflective interferences can strain masticatory muscles to achieve MIP
Interfering posterior teeth aggravate this by causing excessive wear, hyper mobility, fractured cusps, and hypersensitivity