Oxygen
1/55
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
56 Terms
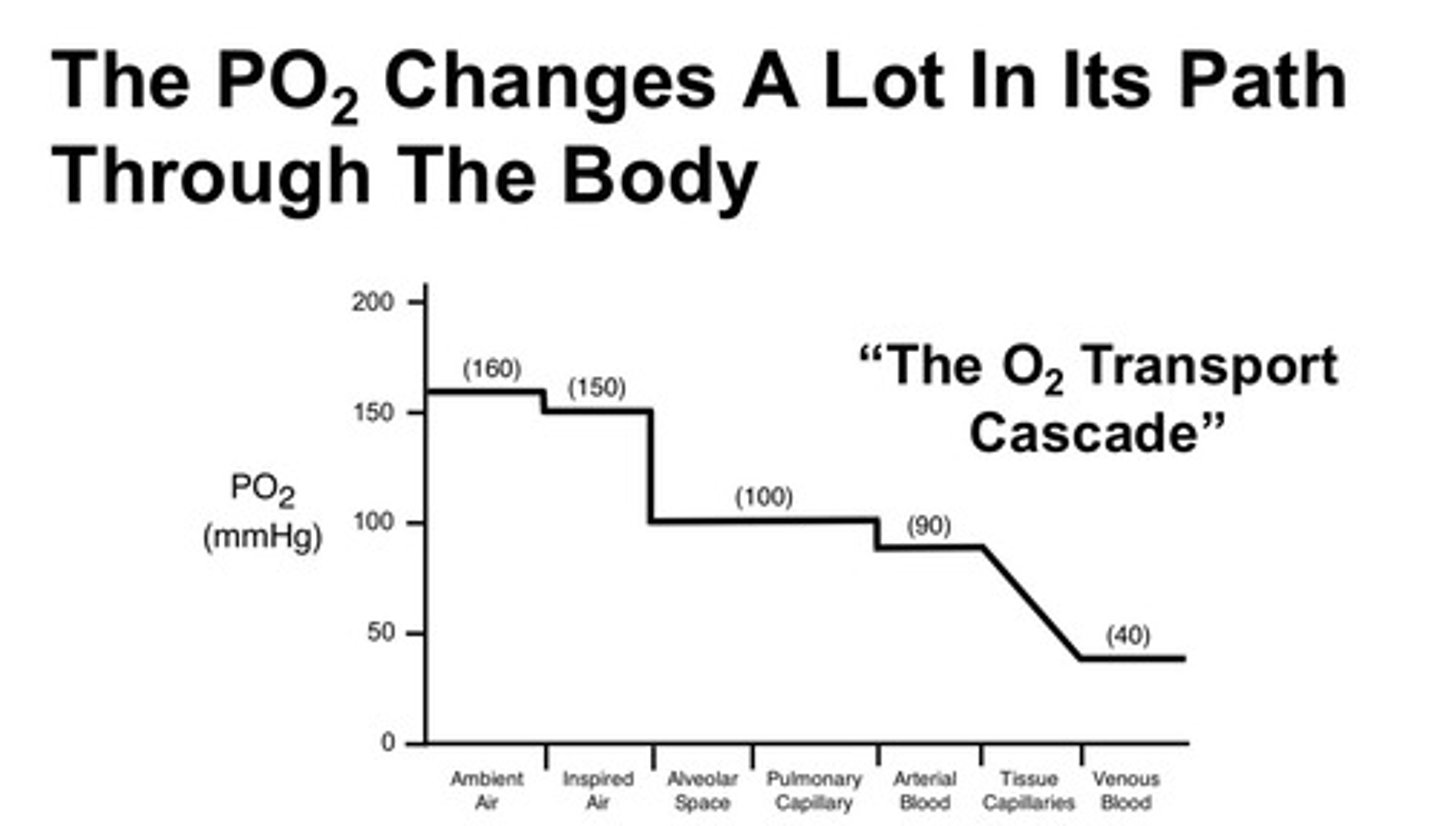
how do we measure the "amount of oxygen" in the different spaces of the body and what are the units?
we measure the partial pressure of O2 in the different spaces of the body; units are mmHg; and we consider the O2 transport cascade!
what is partial pressure
if you place a mixture of gases in a container, the partial pressure exerted by the kinetic energy of an individual gas is referred to as its partial pressure
FiO2 (inspired fraction of O2) does not change, unless?
unless patient is on a ventilator or on a different planet
although FiO2 does not change, ambient PO2 does change depending on where the patient is. why?
partial pressure at each point along the initial portion of the oxygen transport cascade are LOWER at HIGHER elevations than at sea level; as you go up in elevation, the barometric pressure declines which as a result causes a decline in ambient PO2 (thus you must use a different barometric pressure in the calculations than you would for a patient at sea level)
what is the FiO2 value?
always at 21%
what does PAO2 represent?
represents the oxygen tensions in alveolar air or partial pressure of oxygen in the alveolar space: represents the PO2 that is found in the alveoli of an ideal lung with normal ventilation-perfusion matching
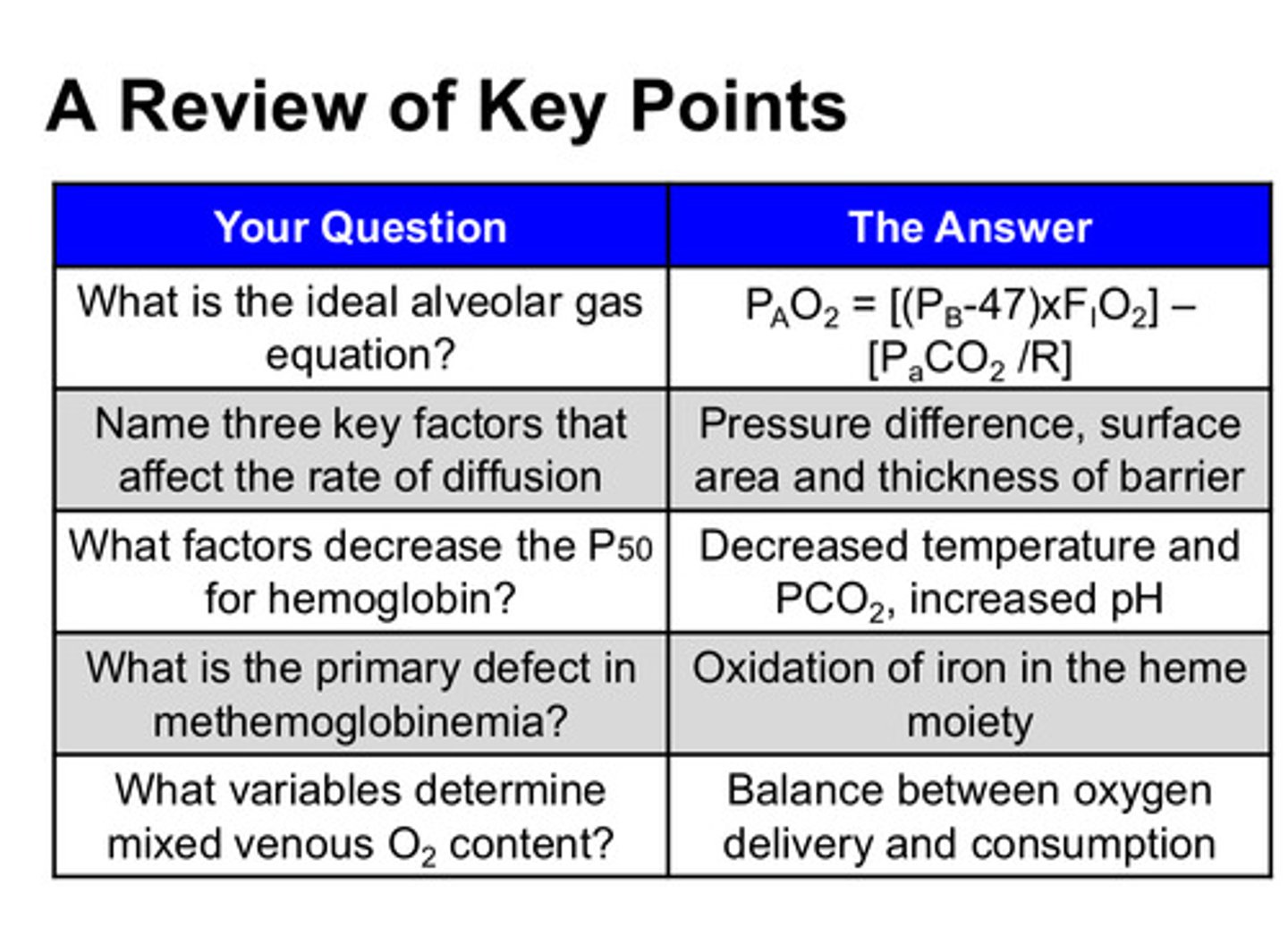
what is the ideal alveolar gas equation?
PAO2 = (PB−PH2O) x FiO2 − (PaCO2/R)
PH2O is the saturated vapor pressure of water at body temperature and is always = 47
PB is barometric pressure and at sea level = 760 (this changes with altitude)
FiO2 = .21 (this does not change)
in the alveolar gas equation, what does (PB-47) x FiO2 represent? what 2 things is it a function of?
represents how much oxygen is brought into the alveolus; this is a function of the PiO2 (inspired partial pressure of O2) and of alveolar ventilation
in the alveolar gas equation, what does (PaCO2)/R represent? what 2 things is it a function of?
represents how much oxygen is taken away from the alveolus; this is a function of cardiac output and of oxygen ventilation (or tissue consumption of O2)
why do we use the ideal alveolar gas equation?
we cannot directly measure PAO2 as we do not have probes that can sit in the alveoli
what does R represent in the ideal alveolar gas equation?
it is the respiratory exchange ratio measure at the mouth: VCO2/VO2 (this is the ratio of CO2 eliminated at the mouth/nose relative to the amount of oxygen taken up at the mouth each minute)
what is the average value of R
0.8 (this value varies based on the fuels being metabolized)
does the diffusion of oxygen from alveoli to the red blood cells happen quickly or slowly?
happens quickly! full equilibration between the alveolar and capillary PO2s occurs within only about 0.25 seconds (in other words, enough oxygen diffuses across the barrier to raise the capillary PO2 to the same value as the alveolar value in a very short period of time)
why do RBCs spend extra time passing by the alveoli despite how quickly oxygen diffusion occurs?
RBCs spend far more time in the pulmonary capillaries before exiting into the pulmonary veins (about 0.75 seconds) and this extra time is important because it gives individuals a large reserve capacity for diffusion and the ability to tolerate problems that interfere with diffusion without downstream effects on arterial oxygenation
what factors can slow the rate of diffusion of oxygen from alveoli to the red blood cells? (5)
1) partial pressure difference across the barrier (P1-P2 where P1 is partial pressure of gas in alveolus and P2 is partial pressure of gas in capillary)
2) surface area of the barrier
3) thickness of the barrier (THIS IS MOST IMPORTANT)
4) solubility of the diffusing substance
5) the molecular weight of the diffusing gas
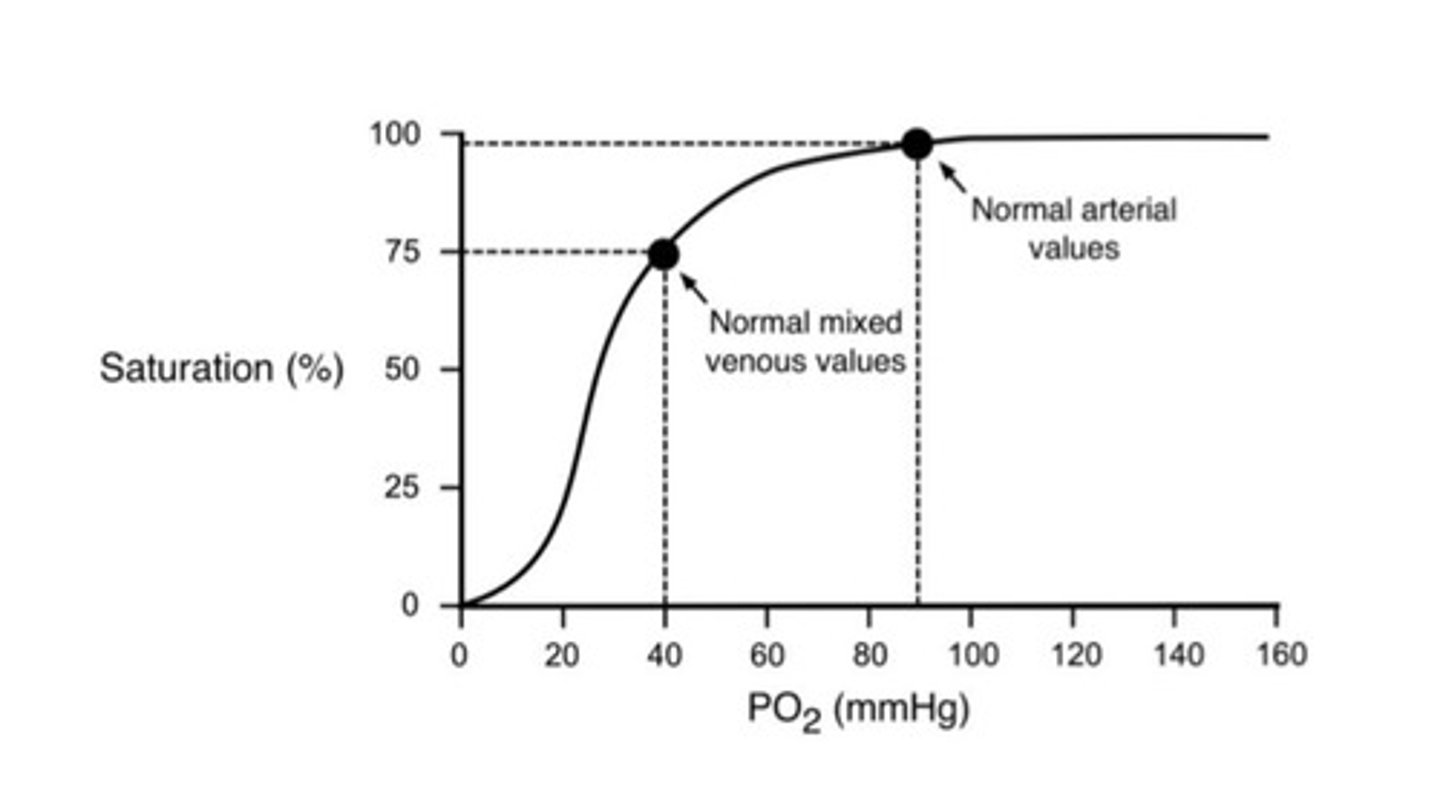
PaO2 represents what? how is this different from PAO2?
PaO2 is arterial PO2 and PAO2 is alveolar PO2; arterial PO2 is always less than the alveolar PO2 in healthy individuals and this normal alveolar-arterial oxygen difference is due to the blood from the bronchial and thebesian veins that drain directly back to the left side of the heart without going through a gas exchanging region of the lung
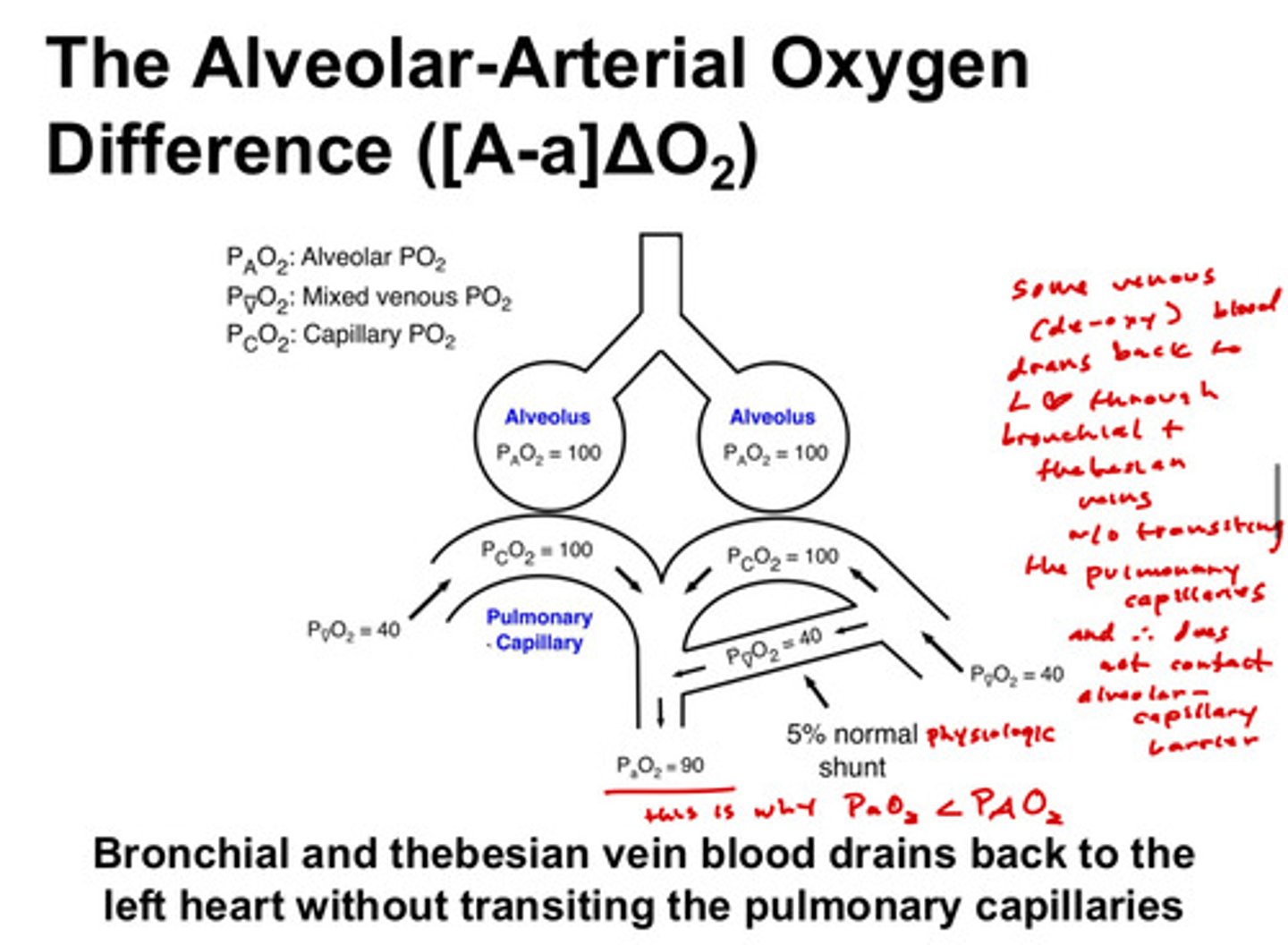
the blood coming into the left atrium is fully oxygenated blood in the pulmonary veins PLUS venous blood (deoxygenated) from the coronary arteries and some veins that drain the non-respiratory bronchi. so the blood in the left atrium does not have the exact same oxygen partial pressure as?
PAO2
what does hemoglobin do?
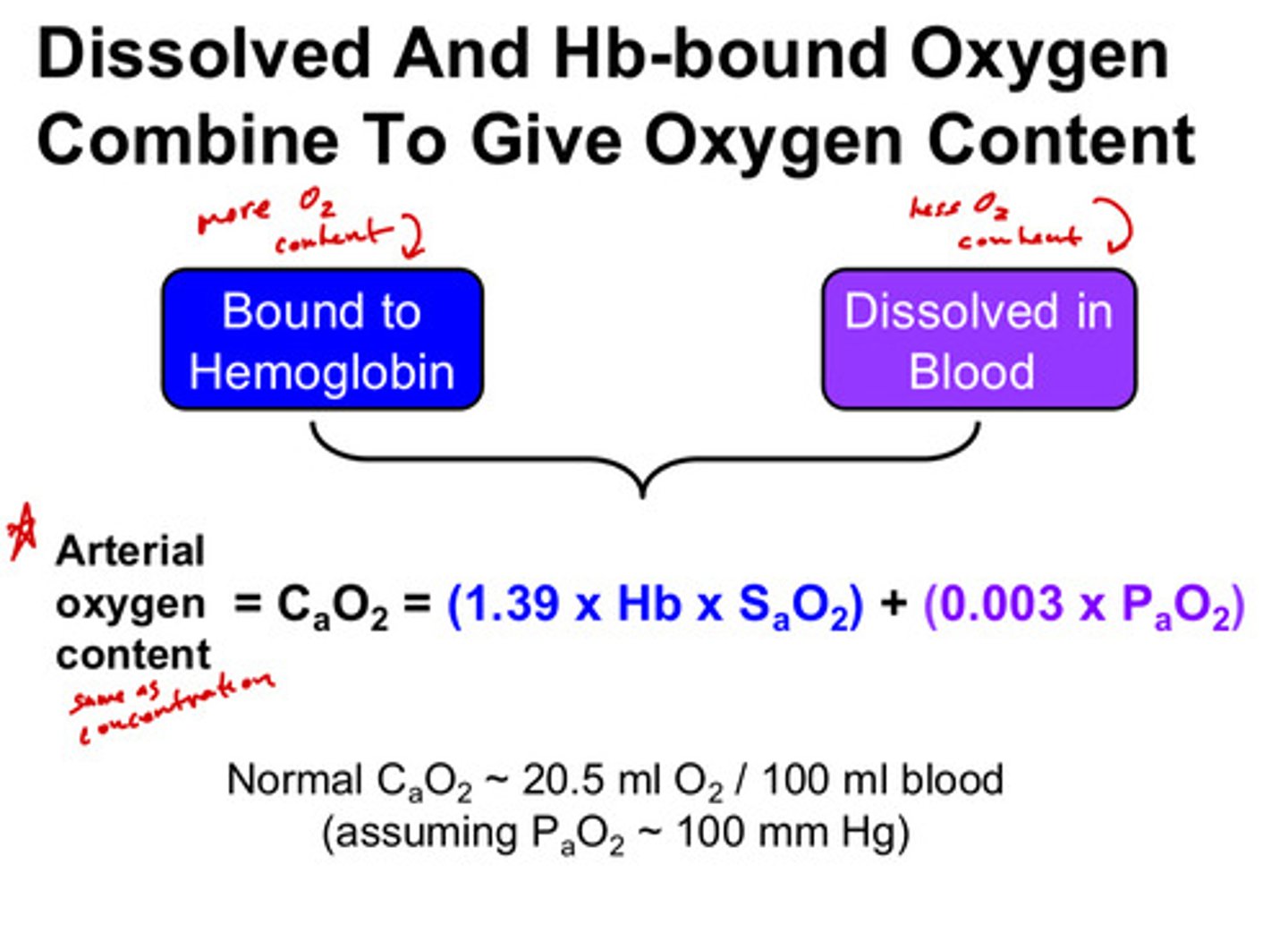
hemoglobin carries oxygen to all tissues in the body; it carries 20 mL O2/100 mL blood which is 70x more than carried in solution (solution only has about 0.3 mL O2/100 mL blood)
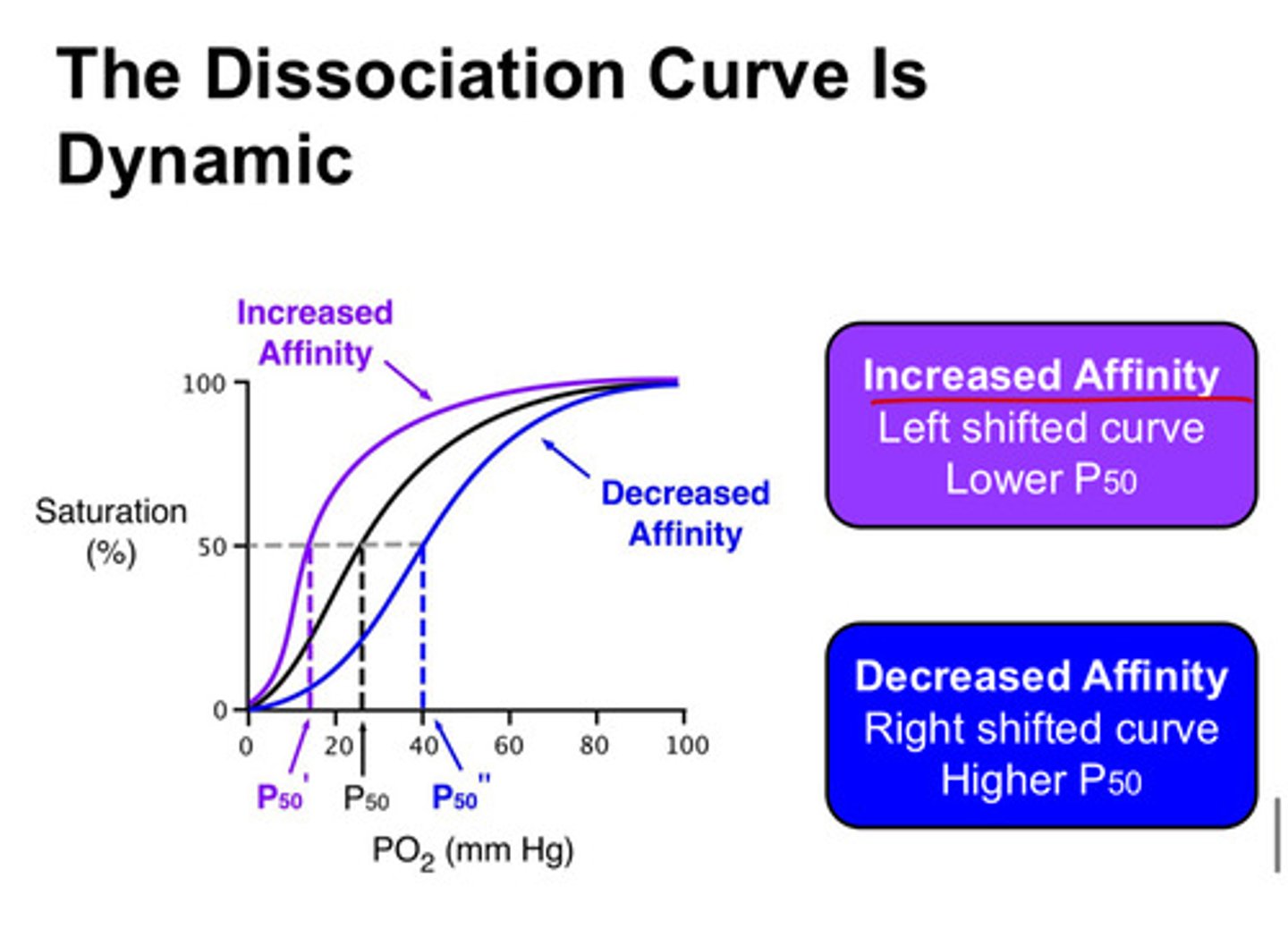
what is P50
P50 describes the hemoglobin's affinity for oxygen; represents the partial pressure at which 50% of the binding sites are occupied by oxygen
what does a lower P50 mean
means hemoglobin has increased affinity and we see a left shifted curve
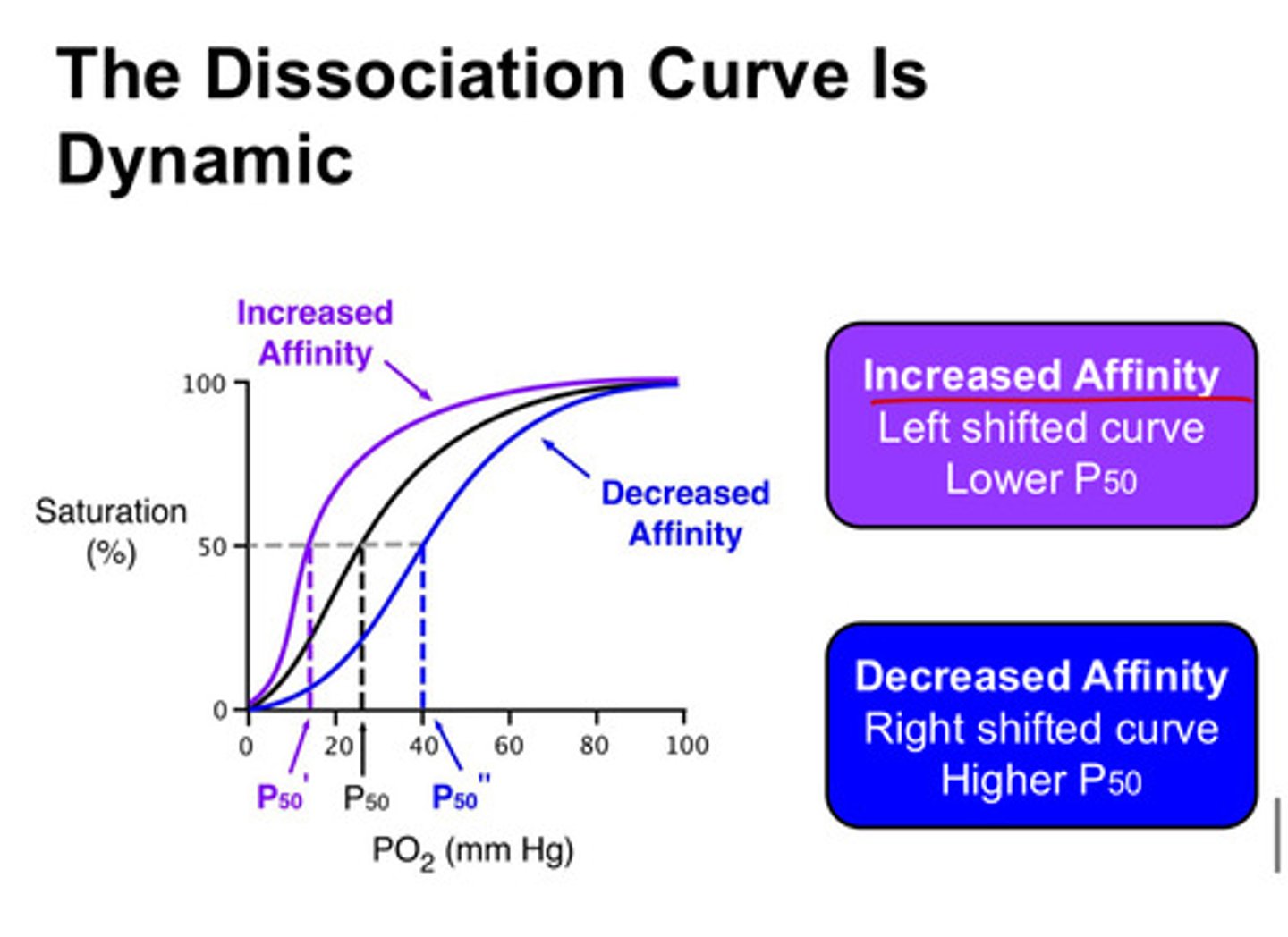
what does a higher P50 mean
means hemoglobin has decreased affinity and we see a right shifted curve
what 3 things can cause higher affinity of hemoglobin for oxygen
1) increased pH
2) decreased PCO2
3) lower temperature
what 4 things can cause lower affinity of hemoglobin for oxygen
1) decreased pH
2) increased PCO2
3) higher temperature
4) increased 2,3 DPG
is there more oxygen carried in hemoglobin or dissolved in the blood in the normal human?
there is more oxygen carried/bound in hemoglobin than dissolved in the blood in the normal human
the details around dapsone are not very important for you but do know that there are some medications that can cause hemoglobin to have an abnormal structure and not work correctly
dapsone causes oxidation of iron in the heme group which forms methemoglobin; this cannot bind oxygen!
summary points
define FiO2
inspired fraction of O2
Define PiO2
partial pressure of inspired O2
Define PAO2
alveolar partial pressure of O2
Define PaO2
arterial partial pressure of O2
Define SaO2
O2 saturation of arterial Hb
what does the fraction of a particular gas describe
within a gas mixture, what fraction is comprised of the gas in question!
what is the partial pressure of a particular gas
the pressure that gas exerts within a mixture of gases
what is the saturation of O2 on hemoglobin
it is a percentage and describes how completely the hemoglobin is carrying oxygen, but it does not give us information about how much hemoglobin is available to carry the oxygen
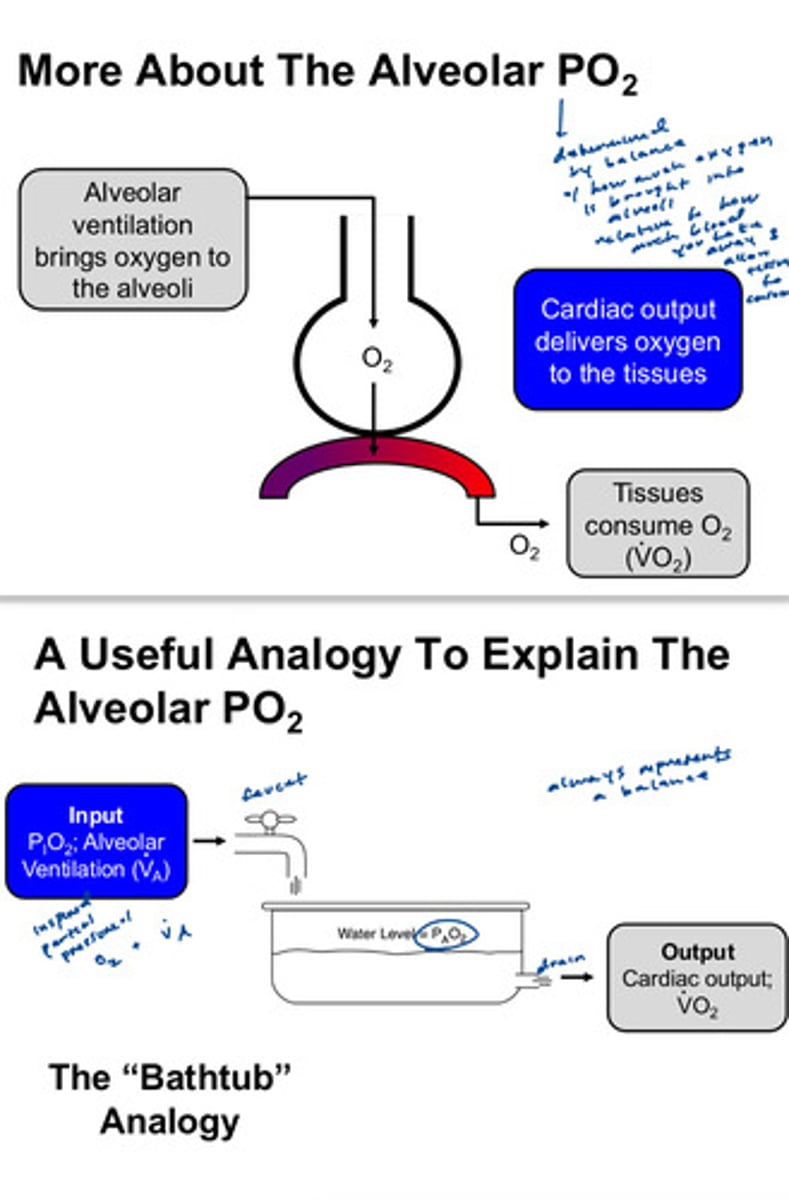
what is PAO2 determined by
how much O2 is being delivered to the alveoli relative to how much is taken away. it is the balance between the influx (from air) and efflux (into the blood) of oxygen in the alveolar space
influx of O2 into the alveoli is a function of what 2 things
the ventilation and the inspired partial pressure of oxygen (these are represented as VA and PiO2)
efflux of O2 out of the alveoli is a function of what 2 things
cardiac output and the oxygen consumption in the body
oxygen consumption in the body can be estimated by what
PCO2 divided by a metabolic quotient "R", which is usually 0.8 (we can more easily measure PCO2 than we can PAO2, so it is useful to be able to use this metabolic quotient number to calculate PAO2)
because CO2 diffuses so quickly from blood into the alveoli and vice-versa, we can assume what?
PACO2 = PaCO2; so we just call it PCO2 (this is NOT true for oxygen, only for CO2)
describe the alveolar gas equation in words
alveolar partial pressure of O2 = oxygen coming into the alveolus minus the oxygen going out of the alveolus into the blood
what is the alveolar gas equation
PAO2 = PIO2 - (PaCO2/R)
PAO2 = alveolar PO2 (mmHg)
PIO2 = FiO2(PATM-PH2O)
FiO2 = 0.21
PH2O = 47
PaCO2 = arterial PCO2 (mmHg)
R = respiratory quotient = CO2 produced per O2 consumed = 0.8
why is the alveolar gas equation important in terms of hypoxemia
the causes of hypoxemia can be narrowed down by knowing the PAO2 and comparing it to the PaO2
how can we figure out what the PAO2 is in real life
we can quickly measure the PaO2 and the PCO2 with a blood test called an arterial blood gas. we usually know the PiO2, so we can figure out what the PAO2 is!
case: prior to start of dental school, a 30 year old travels to alaska. their base camp is at an elevation of 7,500 ft and they then travel to a higher base camp to acclimate and will eventually try for the summit at 20,322 ft. when she is at base camp, what changes would you expect to see in the equation compared to when she was at sea level?
at sea level: PiO2 = (PATM - PH2O) x FiO2
= (760 - 47) x 0.21
= 149.72 = ~150
if we go to a higher altitude, the barometric pressure (PATM) will decrease! so
FiO2 will remain the same at 0.21
PiO2 will decrease due to decrease in barometric pressure
PAO2 will decrease due to decrease in PiO2
PaO2 will decrease as it will decrease whenever PAO2 decreases
case 2: when lying in her tent on the first day at higher altitude, she notices that her resting heart rate was elevated at 90 bpm. what is the mechanism for the increased heart rate and why does it increase?
her PaO2 decreases as a result of the gain in elevation. one of the main physiologic responses to acute decreases in PaO2 (referred to as acute hypoxemia) is an increase in heart rate to increase cardiac output. this response is primarily mediated by an increase in SNS activity; it is trying to improve oxygen delivery to the tissues in the situation of low oxygen in the blood
case 3: a 42 year old man is admitted to hospital for severe acute bleeding. vital signs are BP = 80/42, HR = 130, RR = 20 breaths/min, SaO2 = 98% breathing room air, hemoglobin concentration is low at 8g/dL. are these normal vital signs and why does his oxygen saturation appear normal in this situation?
BP is low
HR is high
RR is normal but at upper limit
SaO2 is normal
hemoglobin concentration is low
pulse-oximetry measures saturation of oxygen in the hemoglobin but does NOT tell you about content of oxygen. it only tells you how well the hemoglobin is carrying the oxygen, not how much hemoglobin there is. so a person can have low hemoglobin (anemia) but have normal SaO2
is a person has low saturation, what does this mean but what information do we not get?
they do not have access to enough oxygen either through low ventilation or low cardiac output, but this does not provide any information one way or the other about how much hemoglobin they have
what does the oxygen-hemoglobin dissociation curve show
it plots how saturated the hemoglobin is in the presence of a given partial pressure of oxygen. when hemoglobin is present in high oxygen, it is fully saturated (like in arteries), and when present in low oxygen, it is less saturation (like in veins)
when is pulse oximeter useful and when is it not?
useful when person has normal RBCs and hemoglobin content, not useful in situation of anemia or blood loss!
what can shift the hemoglobin-oxygen dissociation curve to the right?
right shift means decreased affinity and increased P50:
1) increased temp
2) increased PCO2
3) increased 2,3-DPG
4) decreased pH
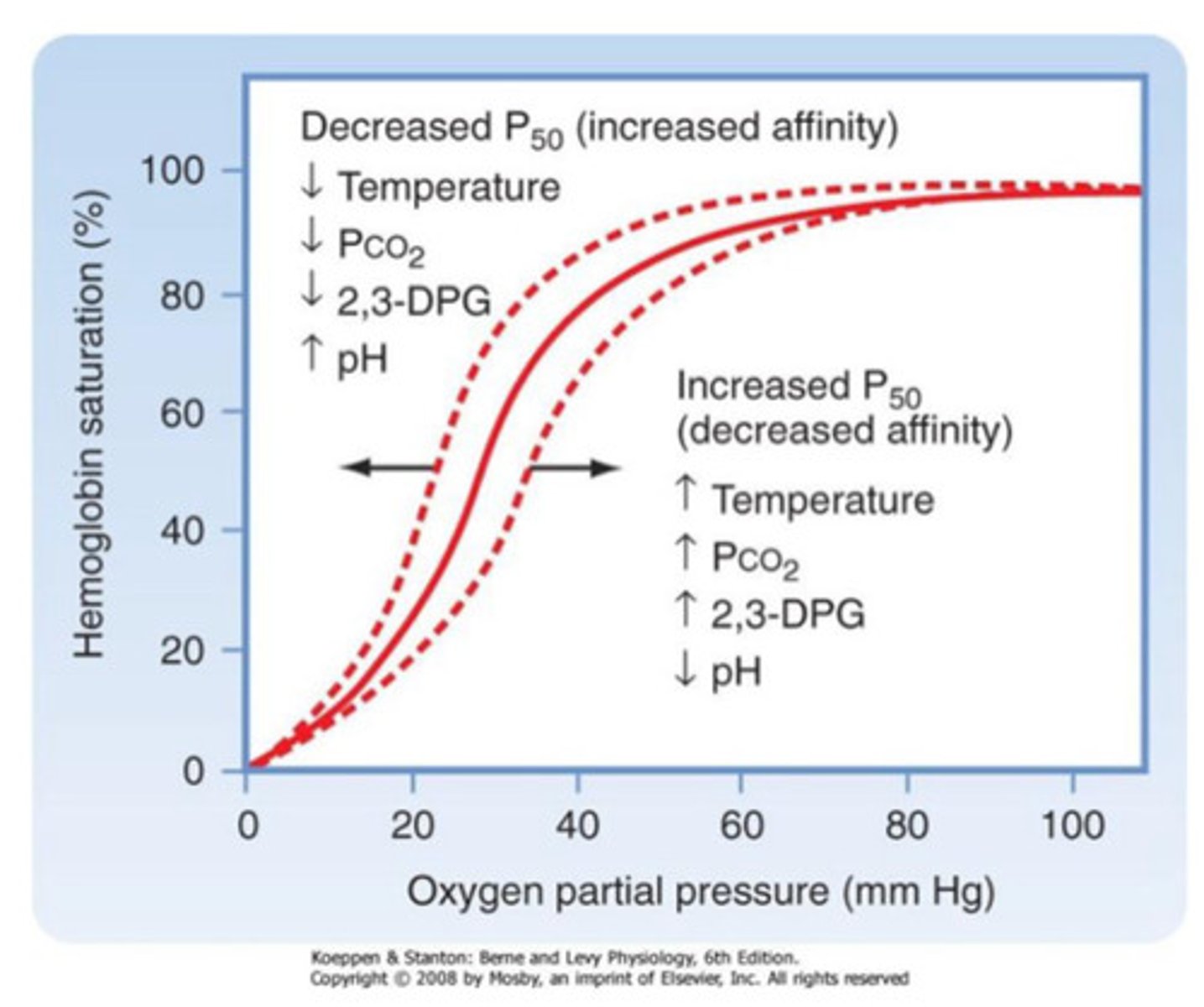
what can shift the hemoglobin-oxygen dissociation curve to the left?
left shift means increased affinity and decreased P50:
1) decreased temp
2) decreased PCO2
3) decreased 2,3-DPG
4) increased pH
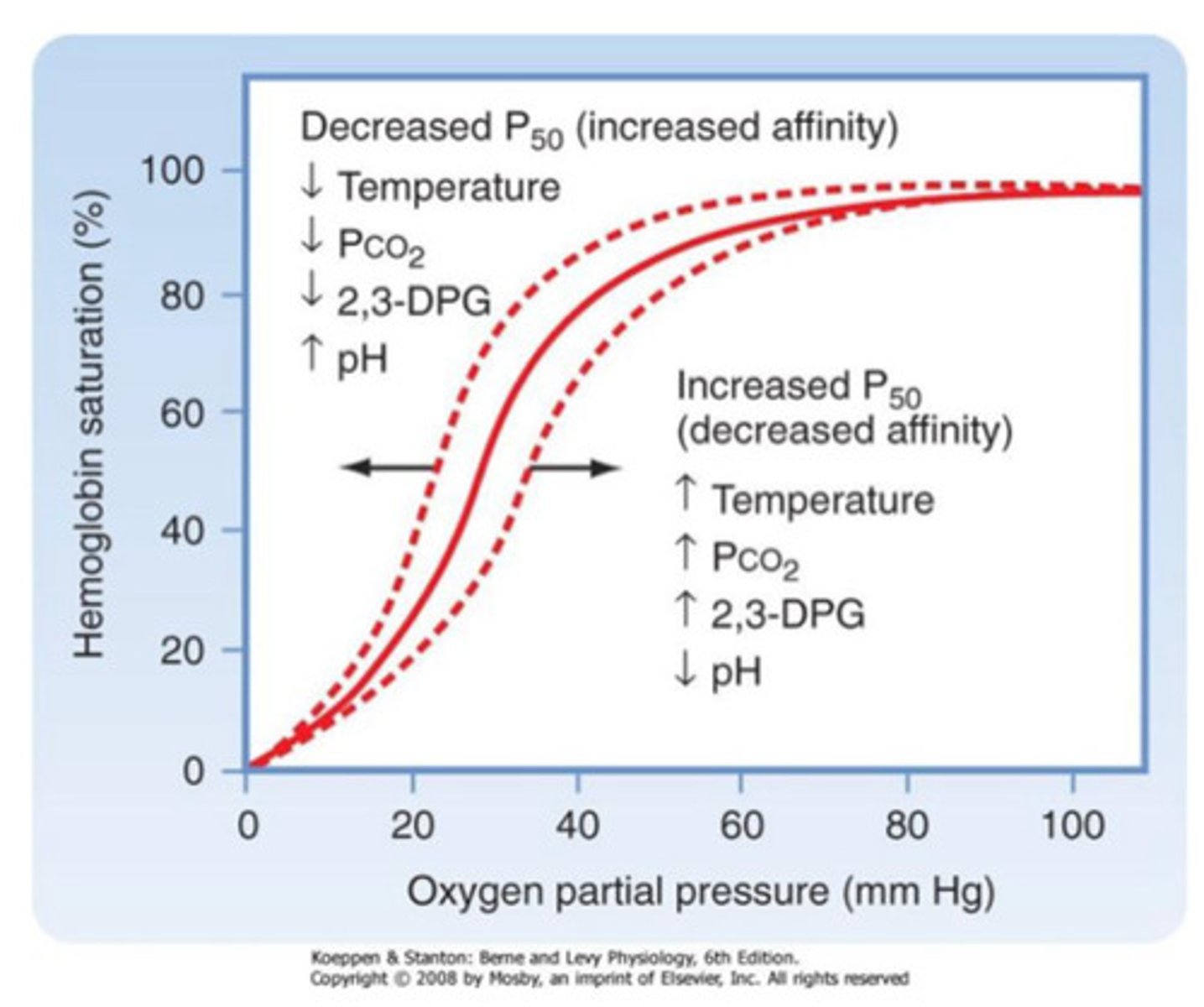
a right shift means what in the hemoglobin-oxygen dissociation curve?
hemoglobin is less likely to hold onto the oxygen compared with normal; tissues typically have higher oxygen demands in these situations
a left shift means what in the hemoglobin-oxygen dissociation curve?
hemoglobin is more likely to hold onto the oxygen compared with normal; typically have lower oxygen demands in these situations
explain why it would be important for hemoglobin to have lower affinity for oxygen at the quadricep muscle during a mile jog. what is happening at the muscle with regards to temperature and pH and pCO2
a muscle in use has higher temperature from increased perfusion, lower pH due to increased metabolic waste, and higher PCO2 produced from active metabolism. that muscle will need more oxygen supply for this increased metabolic activity. when the hemoglobin-oxygen dissociation curve is shifted right at the thigh, the oxygen will offload from the hemoglobin more easily, providing oxygen to these needy tissues
a little extra about 2,3-DPG!
it is produced within the red blood cells and helps offload oxygen in areas of need. it is naturally increased in the body in certain conditions, such as chronic anemia, living at altitude, chronic lung disease
the oxygen-hemoglobin dissociation curve can be applied to certain specific areas of the body or can be used to discuss the whole patient
for instance, fever shifts the oxygen-hemoglobin saturation curve to the right throughout the entire body