Organisms exchange substances
1/98
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
99 Terms
How does an organisms size relate to their SA:V ratio?
The larger the organism, the lower the SA:V ratio
How does an organism’s SA:V ratio relate to their metabolic rate?
The lower the SA:V ratio, the lower the metabolic rate
Why do smaller organisms not require specialised exchange or transport systems?
They have a large SA:V ratio which allows efficient exchange directly across the body surface
Why do smaller mammals have a high metabolic rate?
Due to their high SA:V ratio, they lose heat rapidly. Therefore, a high metabolic rate provides the energy needed to provide more heat and maintain a stable body temperature
Give some adaptations that large organisms have to increase SA:V ratio (7)
Large, folded body parts
Villi and microvilli
Alveoli and bronchioles
Spiracles and tracheoles
Gill filaments and lamellae
Thin wide leaves
Capillary networks
Why do multicellular organisms require specialised gas exchange surfaces?
Their small SA:V ratio means the distance that needs to be crossed to larger and substances cannot easily enter the cells
Name 3 features of an efficient gas exchange surface
Large SA:V ratio
Short diffusion distance
Maintained a concentration gradient
Explain the process of inspiration and the changes that occur during it
External intercostal muscles contract, pulling ribs upwards + outwards
Internal intercostal muscles relax
Diaphragm contracts and flattens
Lung volume increases
Air pressure in lungs initially drops
Air moves into the lungs due to gradient between atmosphere and lungs
Explain the process of expiration and the changes that occur during it
Internal intercostal muscles contract, pulling ribs downwards and inwards
External intercostal muscles relax
Diaphragm relaxes and domes upwards
Lung volume decreases
Air pressure in lungs initially greater than atmosphere
Air moves out of lungs from high pressure in lungs to lower pressure in atmosphere
Describe alveoli and their function in gas exchange
Tiny air sacs
300 mil in each lung so very large SA for gas exchange
Walls are one cell thick and covered with a network of capillaries so minimises diffusion distance
Network of capillaries also allows a constant blood supply which maintains a conc gradient to remove exchanged gases
What is the nasal cavity and what’s its structure?
The internal chamber of the nose that air passes through.
It is lined with ciliated epithelial cells and goblet cells
It also contains bones called turbinates that increase SA
What’s the function of the nasal cavity?
Moistens air entering the lungs which protects the delicate alveoli
Goblet cels secrete mucus which traps dust and bacteria
Describe the trachea and its function
Wide tube supported by C-shaped cartilage to keep the air passage open during pressure changes
Lined with ciliated epithelial cells which move mucus towards the throat to be swallowed, preventing lung infections
Carries air to the bronchi
Describe the bronchi and their function
Two tubes that branch off from trachea, one leading to each lung
Supported by smaller and less complete rings of cartilage to keep airways open
Lined with epithelial cells which move mucus up towards throat to be swallowed
Lined with goblet cells which secrete mucus
Elastic fibres found in the walls which allow them to stretch and recoil during ventilation
Smooth muscle found in the walls which can contract to narrow the airway and control airflow
Allow passage of air into the bronchioles
Describe the bronchioles and their function
Very small airways that branch from the bronchi
No cartilage
Smooth muscle present in walls so they can contract and relax to control airflow
Elastic fibres present in walls so they can recoil during exhalation
Epithelium cells become simpler and thinner to provide a short diffusion pathway
Allow passage of air into the alveoli
Describe the pathway taken by air as it enters the mammalian gaseous exchange system
Nasal cavity → trachea → bronchi → bronchioles → alveoli
What is tidal volume?
Volume of air that enters and leaves the lungs at normal resting breath (0.5dm³)
What is vital capacity?
Max volume of air we can inhale and exhale in one breath
What is residual volume?
The volume of air left in the lungs after the strongest exhalation
What is total lung capacity?
The total volume of air the lungs can hold after maximum inspiration
Vital capacity + residual capacity
Usually (5-6dm³)
Why can’t fish use their bodies as an exchange surface?
They have a waterproof, impermeable body surface, so gases can’t dissolve and diffuse across the membrane
They have a small SA:Volume ratio-their body surface is too small compared to their volume to supply enough oxygen to all cells
What’s the gas exchange organ in fish and their structure?
Gills
There are 4 layers of gills on both sides of the head
Supported by gill arches
Made up of stacks of gill filaments
Each gill filament is covered in lamallae which have a capillary network
Water rushes in and over the gills in the opposite direction to blood flow and then out through a hole in the sides of their head
How are gills efficient for gas exchange?
Large SA:V ratio created by many gill filaments covered by many gill lamellae
Short diffusion pathway due to a capillary network in every lamellae and very thin lamellae
Maintained conc gradient - countercurrent flow mechanism
What is the countercurrent exchange principle?
Water flows over the gills in the opposite direction to the flow of blood in capillaries
Ensures that equilibrium isn’t reached
Ensures that a conc gradient is maintained across the entire length of the lamellae
Why can’t insects use their bodies as an exchange surface?
They have a waterproof chitin exoskeleton + a lipid layer which prevent gases from diffusing through the surface
Small SA:V ratio
No lungs-use a tracheal system
What 3 adaptations do insects have to prevent water loss?
Small SA:V ratio where water can evaporate from
Waterproof exoskeleton
Spiracles open and close to reduce water loss
Name and describe the 3 main features of an insects gas transport system
Spiracles - round, valve-like openings running along length of abdomen. O2 and CO2 enter and leave via these. Trachea attach to these openings
Trachea - network of internal tubes extending through the body. Have rings within them to strengthen and keep them open
Tracheoles - smaller branches dividing off the trachea. Extend throughout all the tissues in the insect and deliver O2 to all respiring cells
Describe the 3 methods of moving gases in the tracheal system
By diffusion - when cells respire, they use up O2 and produce CO2, creating a conc gradient from tracheoles to the atmosphere
Mass transport - in which an insect contracts and relaxes their abdominal muscles, squeezing the trachea, to move gases on mass
When insects are in flight, muscle cells respire anaerobically to produce lactate-lowers water potential of cells so water moves from the tracheoles into cells by osmosis - decreases the volume in the tracheoles so more air from atmosphere is drawn in
How is the tracheal system efficient for gas exchange?
Large SA - large number of fine tracheoles
Short diffusion pathway - walls of tracheoles are thin and short distance between spiracles and tracheoles
Steep diffusion gradient - use of O2 and production of CO2
Where does gas exchange occur in plants?
At stomata
Describe 3 adaptations of a leaf that allow efficient gas exchange
Thin and flat to provide short diffusion pathway and large SA:V ratio
Many stomata in the underside of the leaf which allow gases to easily enter
Air spaces in the mesophyll allow gases to move around the leaf
How do plants limit their water loss while still allowing gases to be exchanges?
Stomata regulated by guard cells which allow them to open and close as needed
What are xerophytic plants?
Plants that are adapted to live in environments with limited water
What structural features do xerophytic plants have to enable efficient gas exchange whilst also limiting water loss? (5)
Curled leaves - trap moisture to increase humidity and reduce water potential gradient
Hairs - trap moisture to increase humidity
Sunken stomata - trap moisture
Thicker cuticle - reduces evaporation
Longer root network - reach more water at further distances at soil
Define digestion
The hydrolysis of large, insoluble molecules into smaller molecules that can be absorbed across cell membranes
Which enzymes are involved in carbohydrate digestion and where are they found?
Amylase - found in pancreas and salivary glands
Membrane-bound disaccharidases - sucrase, lactase and maltase found in small intestine
What are the substrates and products of the carbohydrate digestive enzymes?
Amylase - starch into maltose
Maltase - maltose into glucose
Sucrase - sucrose into glucose and fructose
Lactase - lactose into glucose and galactose
Name the 3 enzymes involved in protein digestion and explain their roles
Endopeptidases - hydrolyse peptide bonds between amino acids in the middle of a polypeptide chain
Exopeptidases - hydrolyse peptide bonds between amino acids at the end of a polypeptide chain
Membrane-bound dipeptidases - hydrolyse dipeptides into amino acids
How are certain molecules absorbed into the ileum despite a negative concentration gradient?
By co-transport
How does the ileum maximise absorption?
Ileum wall is covered in villi which have thin walls surrounded by a network of capillaries
Epithelial cells have even smaller microvilli
These features increases surface area, decrease diffusion distance and maintain a concentration gradient
Which molecules require co-transport to be digested into the ileum?
Amino acids and monosaccharides
Where does protein digestion occur?
Starts in the stomach, continues in the duodenum and are fully digested into the ileum
What are lipids digested by?
Lipase and the action of bile salts
Where are lipids digested?
The small intestine
Where is lipase produced?
In the pancreas
What needs to happen before lipids can be digested?
They must be emulsified by bile salts
This breaks them down into tiny droplets called micelles, which increases the surface area for lipase to act on
What are micelles?
Water soluble vesicles formed of fatty acids, glycerol, monoglycerides and bile salts
They deliver fatty acids, glycerol and monoglycerides to the epithelial cells of the ileum for absorption
Give 3 ways micelles help with lipid absorption
They make the fatty acids more soluble in water
They carry the fatty acids to the epithelial cells of the ileum
They help to maintain a higher concentration of fatty acids outside the epithelial cells by continuously delivering them to the cell surface
How are lipids digested?
Lipase hydrolyses the ester bonds between the monoglycerides and fatty acids
Why do fatty acids and monoglycerides not require co-transport?
They are non polar, so can easily diffuse across the phospholipid membrane of epithelial cells
What happens to fatty acids and monoglycerides once they enter the cell?
They are modified back into triglycerides inside of the endoplasmic reticulum and Golgi body
How do modified lipids leave the epithelial cell?
Vesicles containing the triglyceride are released and move towards the cell membrane
They leave the cell by exocytosis
Give 2 features of the cardiac muscle
It is myogenic - can contract and relax without nervous or hormonal stimulation
Never fatigues as long as it has a supply of oxygen
What are coronary arteries?
Supply the cardiac muscle with oxygenated blood
Branch off from the aorta
Relate the structure of the atria to their function
Thinner muscular walls - do not need to contract as hard as only pumping blood to ventricles
Elastic walls - stretch when blood enters
Relate the structure of the ventricles to their function
Thicker muscular walls to enable bigger contractions - creates a higher blood pressure to enable blood to flow longer distances
Left ventricle has thicker muscular wall to enable larger contractions to create higher blood pressure so blood reaches all the cells in the body
Label the heart
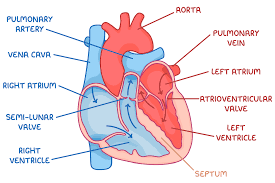
Which side of the heart carries oxygenated blood and which carries deoxygenated blood?
Right side - deoxygenated blood
Left side - oxygenated blood
Describe the pathway blood takes in the heart
Right side: deoxygenated blood from the body enters through the vena cava and leaves through the pulmonary artery to go to the lungs
Left side: oxygenated blood from the lungs enters through the pulmonary vein and leaves through the aorta to go to the rest of the body
What does the septum do?
Separates the deoxygenated and oxygenated blood
Maintains high conc of oxygen in oxygenated blood to maintain conc gradient to enable diffusion at respiring cells
What are the 2 types of valves in the heart?
Semi-lunar valves - between ventricles and arteries (pulmonary valve and aortic valve)
Atrioventricular valves - between atria and ventricles (bicuspid/mitral and tricuspid)
Whats the function of valves?
Prevent backflow of blood
What pressure changes cause valves to open/close?
They open when pressure is higher behind the valve
They close when pressure is higher in front of the valve
Why are two pumps needed in the heart instead of one?
To maintain blood pressure around the whole body - when blood passes through the narrow capillaries of the lungs, the pressure drops and therefore wouldn’t be flowing strongly enough to continue around the whole body. It is returned to the heart to increases the pressure.
What are the 3 stages of the cardiac cycle?
Diastole
Atrial systole
Ventricular systole
Describe what happens during diastole
The atria and ventricular muscles are relaxed
Blood enters the atria via vena cava and pulmonary vein
Volume and pressure in atria increase
Atrioventricular valves are open
Semilunar valves are closed
Volume of ventricles slowly increase as blood flows in passively
Describe what happens during atrial systole
Atria muscular walls contract
Pressure in atria increases
Volume in atria decreases
Atrioventricular vales are open
Semilunar valves are closed
Blood enters ventricles - volume increases and pressure stays low
Describe what happens during ventricular systole
After a short delay, ventricle muscular walls contract
Pressure in ventricles increases
Volume in ventricles decreases
Atrioventricular valves close
Semi lunar valves open
Blood flows into the arteries
What 3 main layers are the walls of arteries and veins made up of?
A thin inner lining of epithelial cells
A middle layer of elastic tissue and smooth muscle
An outer layer of collagen fibres
Relate the structure of arteries to their function
Muscle layer - thick so that constriction and dilation can occur to control volume of blood
Elastic layer - thick to help maintain high blood pressure by stretching and recoiling
Walls are thick to prevent the vessels bursting due to the high pressure
No valves
Relate the structure of veins to their function
Muscle layer - thin as blood is under low pressure so doesn’t need to be constricted
Elastic layer - thin as pressure is low so don’t need to stretch and recoil
Walls are thin as pressure is low so low risk of bursting and also means that vessels are easily flattened which helps blood flow
Have valves to ensure blood doesn’t flow backwards
Relate the structure of arterioles to their function
Muscle layer - thicker than arteries to help restrict blood flow into the capillaries so they’re not damaged
Elastic layer - thinner than arteries as pressure is lower
Walls are thinner than arteries as pressure is lower
No valves
Describe the structure of haemoglobin
A globular protein consisting of 4 polypeptide chains, each carrying a haem group which contains iron
Describe the role of haemoglobin
Present in red blood cells
Oxygen molecules bind to the haem groups and are carried around the body to where they are needed in respiring tissues
What is partial pressure (PO2)?
A measure of oxygen concentration in the surrounding area
How does partial pressure affect oxygen-haemoglobin binding?
When partial pressure of oxygen is high, haemoglobin has a high affinity for oxygen, so becomes saturated with oxygen (association)
When partial pressure of oxygen is low, haemoglobin has a low affinity for oxygen, so oxygen unloads (dissociation)
How does partial pressure of carbon dioxide affect oxygen-haemoglobin binding?
The Bohr effect - as partial pressure of CO2 increases, conditions becomes acidic causing haemoglobin to change shape. The affinity for oxygen therefore decreases so more of it unloads.
What do oxyhaemoglobin dissociation curves show? Describe their shape and what causes it
Oxyhaemoglobin saturation (%) against PO2.
They are S-shaped as when the first oxygen molecule combines with the first haem group, the shape of the haemoglobin become distorted (cooperative nature)-makes it easier for the next 2 oxygen molecules to bind. The final one has difficulty again as there is a low chance of finding a binding site.
How does carbon dioxide affect the position of an oxyhaemoglobin dissociation curve?
If there is a low partial pressure of CO2 (eg in alveoli) curve shifts to left due to increased affinity for O2
If there is a high partial pressure of CO2 (eg in respiring tissues) curve shifts to the right due to decrease affinity for O2
Explain why oxygen binds to haemoglobin in the lungs
Partial pressure of oxygen is high
Partial pressure of carbon dioxide is low
Affinity for oxygen is high
Oxygen associates with haemoglobin to form oxyhaemoglobin
Explain why oxygen is released from haemoglobin in respiring tissues
Partial pressure of oxygen is low
Partial pressure of oxygen is high
Affinity for oxygen is low
Oxygen dissociates from haemoglobin
What is tissue fluid?
Fluid containing water, glucose, amino acids, fatty acids, ions and oxygen which bathes the tissues. Supplies these materials to the cells while also removing any waste.
How is tissue fluid formed?
Capillaries have small gaps in the walls so that liquid and small molecules can be forced out
As blood enters the capillaries from arterioles, the smaller diameter results in a high hydrostatic pressure which forces tissue fluid out (ultrafiltration)
When tissue fluid is formed, what is forced out and what remains in the capillary?
What’s forced out:
-Water
-Dissolved minerals and salts
-Glucose
-Small proteins and amino acids
-Fatty acids
-Oxygen
What remains:
-Red blood cells
-Platelets
-Large proteins
How is tissue fluid reabsorbed?
Towards the venue end of the capillary, the hydrostatic pressure is low due to the loss of liquid
Large molecules remain in capillaries which creates a lowered water potential
This creates an osmotic gradient so water moved back into the capillary by osmosis
What happens to the remaining tissue fluid that doesn’t get reabsorbed?
It is drained into the lymphatic system, becoming lymph
It eventually re-enters the bloodstream near the heart
What is transpiration?
The loss of water vapour from the stomata by evaporation
Name and explain 4 factors that affect transpiration
Light intensity - more light causes more stomata to open so larger surface area for evaporation
Temperature - more heat means more kinetic energy so faster moving molecules therefore more evaporation
Humidity - more water vapour in the air makes water potential outside the leaf higher so reduces water potential gradient therefore less evaporation
Wind - more wind blows away humid air which maintains the water potential gradient therefore increasing transpiration
How is water transported in plants?
Through xylem vessels
Explain the cohesion-tension theory
Cohesion - water molecules form hydrogen bonds causing them to stick together ad travel up the xylem as a continuous water column
Adhesion - water sticks to xylem walls (capillarity)
Tension - as water is pulled up the xylem, it creates tension which pulls the xylem in to become narrower
Root pressure - as water moves into roots it increases volume of liquid inside the root therefore pressure inside the root increase which forces water upwards
Explain how water moves up the xylem (5)
Water vapour evaporates out of stomata on leaves. This loss in water volume creates a lower pressure
When this water is lost by transpiration, more water is pulled up the xylem to replace it
Due to the hydrogen bonds between water molecules, they are cohesive. This creates a column of water within the xylem
Water molecules also adhere to the walls of the xylem. This helps to pull the water column upwards
As this column of water is pulled up the xylem, it creates tension which pulls the xylem in to become narrower
Name the process whereby organic materials are transported around the plant
Translocation
How are organic substances transported around a plant?
Via the phloem
List the 2 key cells inside of phloem vessels
Sieve tube elements
Companion cells
Explain the structure of sieve tube elements
Living cells
Contain no nucleus
Contain few organelles
Explain the function of companion cells
Provide ATP required for active transport of organic substances
Is translocation an active or passive process?
Active
According to the mass flow hypothesis, what is the source and what happens here?
The source is the leaf
Here, sucrose is made in photosynthesis
How does sucrose in the leaf move into the phloem?
Sucrose is transported by facilitated diffusion through plasmodesmata into companion cells
Hydrogen ions are pumped out (with proton pump) of companion cells by active transport into the cell wall space (apoplast), creating a concentration gradient
H+ then re-enter companion cells through co-transport proteins which carry sucrose as well against their conc gradient
This results in a high concentration of sucrose in the companion cells
Sucrose then diffuses from companion cells into sieve tube elements - via plasmodesmata or membrane transport