Card 4203 pacemaker midterm M1
1/103
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
104 Terms
CRMD
life saving devices that are for patients with various cardaic conduction disturabnces and tachyarrythmias
What do CMRD devices do
regulate brady through artifical pacing, resynch ventricles in heart failure, antitachy pacing and defib therapy, monitor arrhythmias
what are some CMR devices
pacemakers, CRT devices, ICD's, ILR
2 components of a pacemaker system
pulse generator and the leads
what does the pulse generator do
deliever electrical impulses to the heart, located in the pectoral region either in the L or R side of the chest ( mainly L)
header of a pulse generator
sits on top of the pulse generator, contains 1 or more open channels to allow of the connection of leads
intergrated circut
contains the components that make the pacemaker function
telemetry
refers to the capability of non-invasive communication between a programmer and the implanted pulse generator
reed switch
activated by applying a magnet to the device, which elicits a specific magnet response
capacitor
acts as a voltage multiplier to deliver a pacing pulse at a voltage higher than the stored capacity of the battery of 2.8 V
Ex) pacing the vents at 3.5v @0.4msec
accelerometer
a small spring board that moves in relationship to the patients activities, it creates a signal that correlates to increases in pacing rate
battery
powers the components in the pulse generator
pacemaker leads
provides a connective pathway from the pulse generator to the heart. the energy is delivered to the heart via the leads and when the pacemaker senses a interistic depol signal, the energy is carried back to the pacemaker via the lead
4 components of the pacemaker lead
1. the connector pin
2. the lead body
3. the electrode( distal end)
4. fixation mechanism
the connector pin
the connector pin and header must match for the pulse generator to function. the standard leads and headers are the IS-1. adaptors may be necessary
lead body
1 or 2 conductor wires run the length from the connector pin to the electrodes. will be either coaxial or coradial
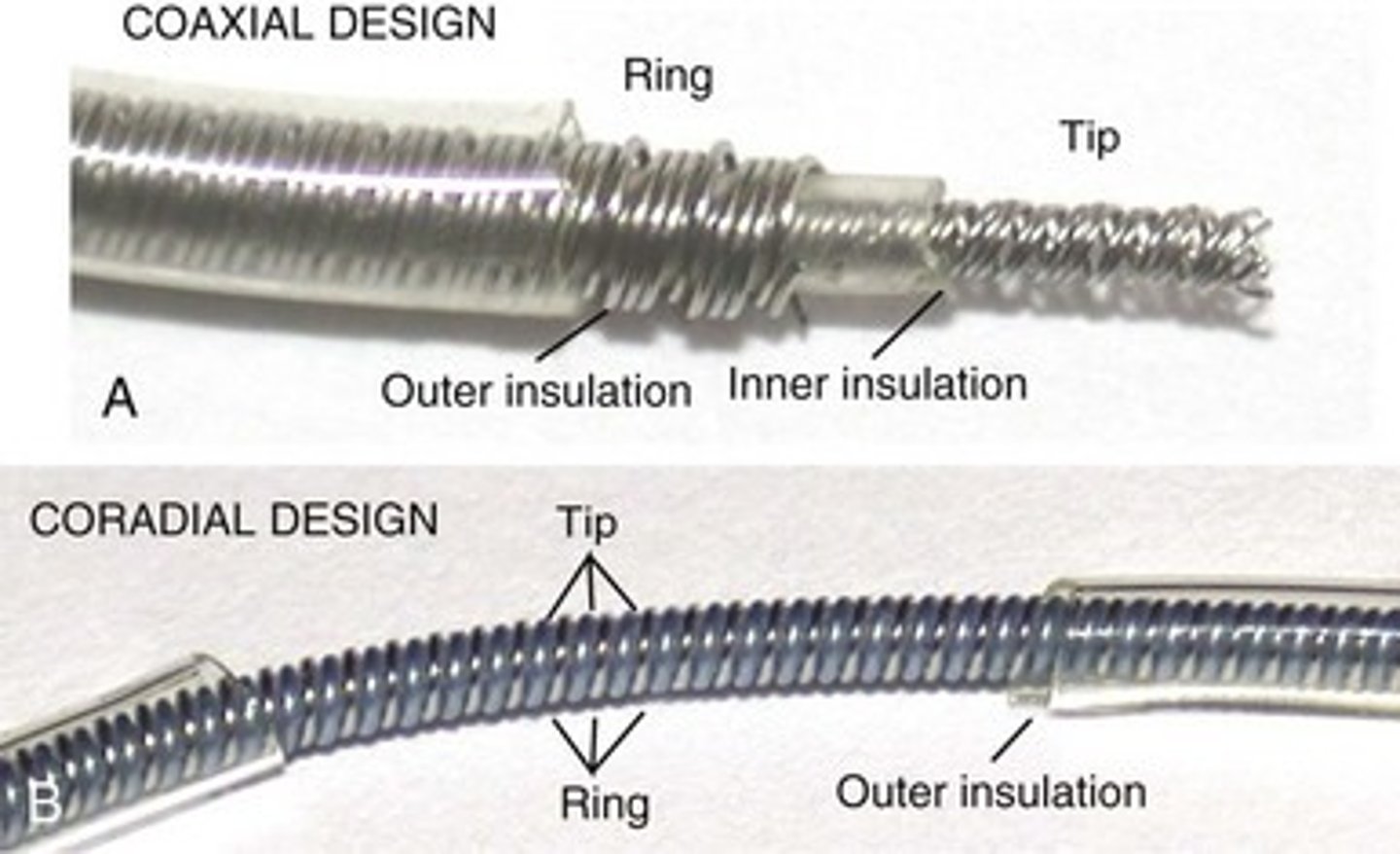
coaxial lead design
there is a inner conductor wire that is surrounded by a layer of insulation and a second wire that extends to the proximal anode electrode surrounding the insulated inner wire
coradial lead design
each wire is indy coated with insulation and the 2 coated wires are laid side-by-side to form a spring like apperance
electrodes
transmit electrical energy from the conductor wire to the surface of the heart. a small surface area electrode stimulation increases efficiency but larger surface area electrodes enhance sensing.
- we use a electrodes with a small radius and a complex surface structure
fixation mechanism
prevents the leads from dislodging after implanting
types of fixation devices
passive- fins/tines- in the trabeculations of the endocardial surface
active- extendable/retractable or a fixed screw on the tip, screwed into the myocardium
steriod eluting leads
leads that store a small amount of steriods ( dexamethasone) behind the distal electrode, the steriods help with inflamation that can cause an acute rise in capture threshold after lead implantation
unipolar leads
1 wire and 1 electrode. current travels from the pulse generator through the wire to the cathode tip and then back through to the anode tip, less complex than bipolar but more EMI problems
uncoated window
important to place this window away from the pectoral muscle due to the possiblity of stimulation when the electrical impulse is travelling back to the generator
oversensing
A lot of spikes for no reason, more likely to occur in unipolar leads because of the larger window for sensing
Bipolar leads
2 wire and 2 electrodes within the heart. current flows through one of the wires to the distal tip (cathode) and then back to the proximal electrode (anode) and then back up to complete the circuit
sensing configurations
unipolar-visualise pacemaker spikes
bipolar-minimize the posibiliy of oversensing
ohms law
V=I x R
voltage (V)
the electrical force that makes current move through a conductor
impedance (R)=omhs
the resistance to the flow of current by an electrical circut or device
current (I)= amps
the transfer of electrical charge through a cross-section of a conductor
we use milliamps as a unit
Convert volts to millivolts by 1000 or move the decimal three places to the right.
Convert amps to milliamps by 1000 or move the decimal three places to the right.
What will the current be if
Voltage = 5 V
impedance = 250 ohms (Ω)?
I = V/R:
5 V x 1000 = 5000 mV / 250 Ω = 20 mA
high lead impedance?
less current= pacemaker longevity will be extended
low lead impedance?
more current= short life span for the pacemaker
what does ohms law do
determines how much current is available for pacing output stimulus and how the lead issue may affect pacemaker longevity
how can leads become compromised
fracture, break, exessive flexing or overstressing, improper connection to the pulse generator
what resistance amount would be considered a fracture in the lead
a rise of > 200 ohms
what happens if fluid/insulation break gets into the pacemaker generator
it will lower the lead impedance. a drop of >200omhs would be seen
CRMD batteries
-They need to be safe as they will be implanted inside the body
-Have high-energy density to save on size and weight
-Have a predictable performance and are highly reliable
-Have a long service life to limit the number of surgical procedures that need to be performed
main power source for the pulse generator
lithium iodine- stable, long lasting, and has a predictable battery depletion curve. generates around 2.8 V and drops to 2.65 V when 90% battery life has been reached
what is the anode made of
lithium
what is the cathode made of
iodine
The ionic movement from the anode to the cathode happens through?
lithium iodine electrolyte
beginning of life ohms
0-1k ohms
needs replacement ohms
10-12k ohms
end of life ohms
>15k ohms
when does a battery need to replaced
2.65V
what if we need a voltage higher than 2.8V?
we would use a voltage doubler or tripler
the battery capacity is one of the major determinants of pulse generator longevity
based of the spesific chemistry and the size of the cell
what is the capacity in which a current can be drawn from the cell
0.5-2.0 AH
what other kind of battery can we use
carbon monfluride
when is lithium for a batter not good
when it is paired with an iodine cathode- internal resistance builds up and it can impact the batterys performance
what kind of battery does an ICD use
lithium/silver vanadium oxide or lithium/manganese dioxide
what is artifical pacing
delivery of electrical impulses of sufficient strength to cause depol
pacing capture
stimulus delivered outside of the myocardiaum refractory period causing a wave of depol
factors that affect the ability of the pacing stimulus to capture
1. Programmed voltage and pulse width of the pacing pulse
2. Integrity of the pacemaker system
component issue within pulse generator, loose set screw or lead fracture may result in loss of capture
3. Proximity of the distal pacing electrode to myocardium
dislodged lead post-implant maybe floating in the chamber
4. Viability of the myocardium
distal lead electrode placed in scar tissue from previous myocardial infarction
5. Stimulation of myocardial cells maybe be affected by the following:
drugs that can increase stimulation threshold - propaferone, flecainide, quinidine and procainamide
decreased sympathetic tone or enhanced vagal tone during periods of rest or sleep
severe metabolic disorders such as acidosis/alkalosis, hypoxemia, hyperkalemia, hyperglycemia
cardiac arrest, cardioversion, defibrillation
stimulation threshold
minimum amount of electrical stimulus needed to consistantly capture the myocardium outside of the hearts refractory period
Amplitude
measured in voltage, can be programmed up to 7.5 V
Pulse width
measured in milliseconds, length of time a stimulus is applied for, can be 2.0 ms
what is the most common programmed setting
2.5V @ 0.4msec
what is the safety margin
either double the voltage or triple the pulse width
When pulse widths are ≥ 0.3ms at a given voltage
tripling pulse width is not typically selected. It is less efficient (expend more energy), while not providing further safety. In this case, the voltage should be doubled to provide an adequate safety margin.
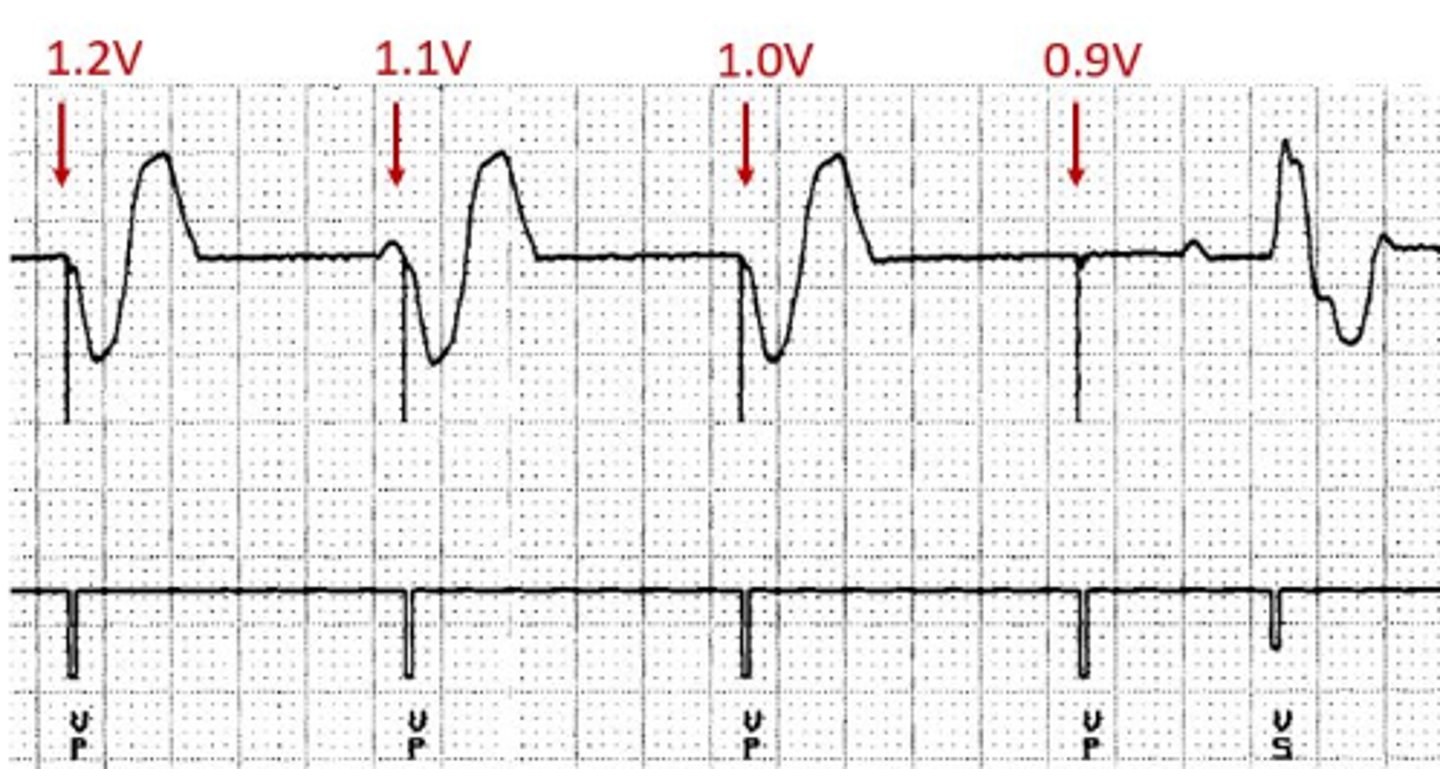
stimulation threshold test
involves decrementing the voltage or pulse width until loss of capture is seen on the ECG tracing. The stimulation threshold is the last pacing output to capture the heart.
example of stimulation threshold testing
In this example, the pulse width is held constant at 0.4ms while the voltage is decremented until loss of capture is seen. Loss of capture occurs at 0.9V so the ventricular stimulation threshold is 1.0V @ 0.4ms
strength duration curve
plots the combination of values (pulse amplitude/pulse width or voltage/milliseconds) at which capture occurs.
what does a strength duration curve demonstrate
It demonstrates graphically that at very high pulse amplitudes, only short pulse widths are needed to capture; as the pulse amplitude decreases, the pulse width must be increased to assure capture.
what the key leandmarks of the strength duration curve
the rheobase and the chronaxie
rheobase
The lowest point on this curve at infinitely long pulse duration. An increase in pulse width beyond this value does not provide more effective stimulation.
chronaxie
The pulse amplitude at twice the rheobase is called the chronaxie; the pulse width setting is desirable to minimize energy consumption while still maintaining an adequate safety margin.
the rheobase - The lowest point on this curve at infinitely long pulse duration
the chronaxie (chronaxie = 2 x rheobase).- The pulse amplitude at twice the rheobase
All points above the curve indicate sufficient stimulus to capture.
All points below the curve indicated sub-threshold stimulus.
sensing
the ability of the pacing system to detect and respond to intrinsic cardiac signals.
The amplitude of the signal that is detected will depend upon-
-the mass of the muscle under the electrode
-the contact of the electrode(s) with the myocardium
-the orientation of the electrodes relative to -the advancing wave of depolarization.
what do the filters in the pulse generator do
-sense only signals which have the same frequency components as P waves and R waves
-reject both low-frequency and high-frequency signals.
frequency range of P and R waves
10-50 Hz
frequency
rate of change of the signal over time
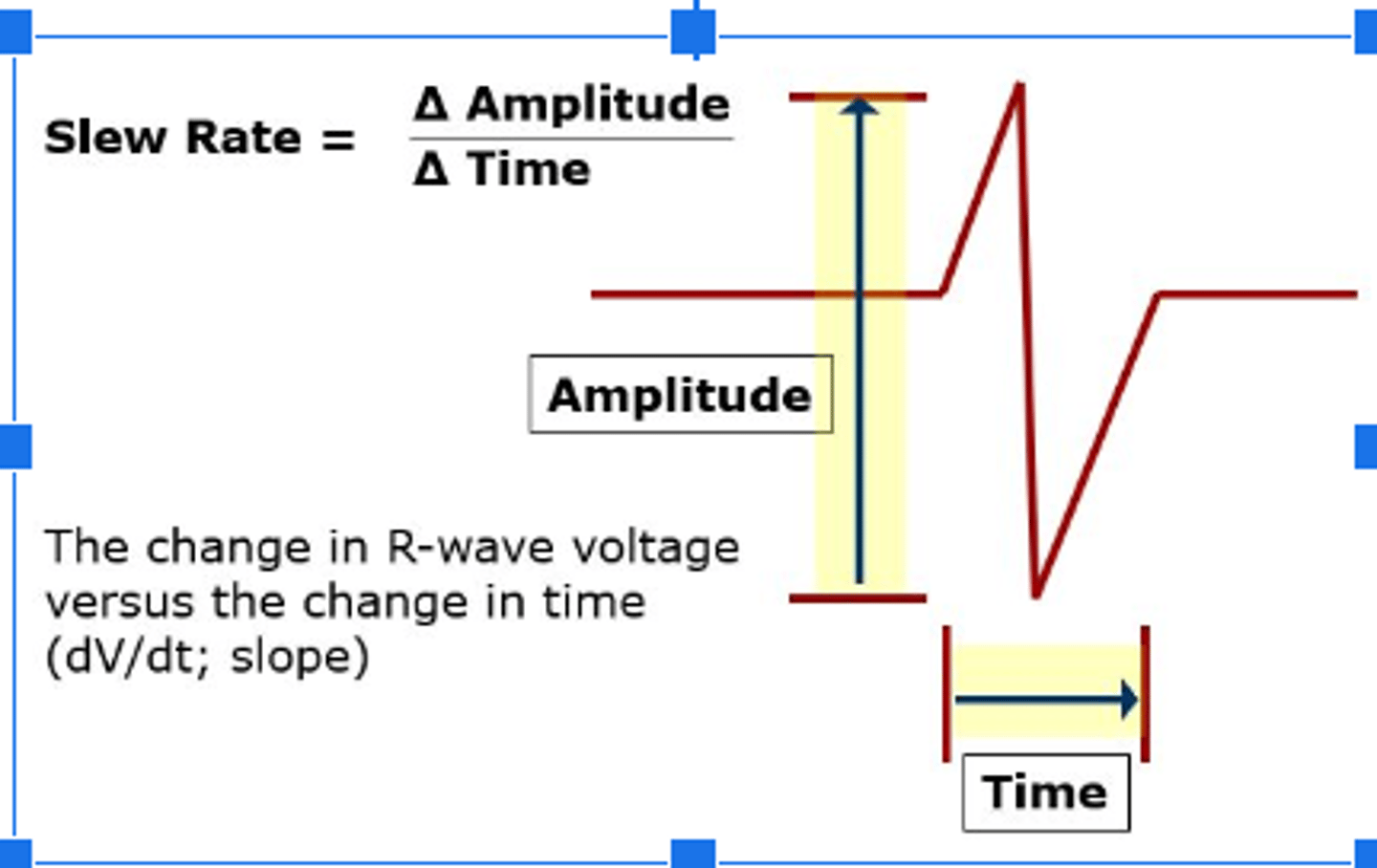
slew rate
represents the maximal rate of change of the electrical potential between the sensing electrodes and it is the first derivative of the electrogram (dV/dt).
slew rate measurements
at implant should exceed 0.5 V/sec for P waves;
0.75 V/sec for R wave measurements.
the higher the slew rate,
the higher the frequency content and the more likely the signal will be sensed.
-T wave, are much less likely to be sensed because of a low slew rate and lower frequency density.
pacemaker sensitivity
The greater the number, the less sensitive the device is to intracardiac signals.
The smaller the number, the more sensitive the device is to seeing intracardiac signals AND other signals we may not want it to see.
oversensing
pauses, when a signal gets past the filter and causes the pacemaker to misinterpret those signals as intrinsic P or R waves. When this occurs, the pacemaker inhibits sending a pacing stimulus to the atrium or ventricle
Need to make the pacemaker "less" sensitive
examples of oversensing
Skeletal myopotentials. T
Far-field events.
T waves.
Lead integrity issue.
loose set screw
EMI
undersensing
occurs when the pacemaker fails to see intrinsic atrial or ventricular activity and paces asynchronously. need to make it "more" sensitive
common reasons for undersensing
-improperly programmed sensitivity setting
-low myocardial voltage signal (post MI)
-lead integrity issue
-electrolyte abnormality.
magnet response
application to a CRMD is a simple way to acquire basic information about the device, temporarily disables tachycardia therapies,
reed switch
puts the pacemaker into a asynchronous pacing mode- which makes the pacemaker no longer sense but continuously paces
reasons to apply a magnet to a crmd
-Determine the battery status of the device.
-Let the clinician know what type of pacemaker is implanted.
-Troubleshoot potential issues with the device.
-Pace asynchronously when oversensing is present.
-Suspend ICD tachy therapies when issues present.
potential complications with magnet application
-Magnet application and asynchronous pacing have been known to initiate atrial or ventricular tachyarrhythmias in vulnerable patients with ischemic or recently infarcted hearts, with a history of VT/VF or with history of SVTs/Afib/Aflutter.
-there is a possibility of initiating an endless loop tachycardia when AV synchrony is lost during magnet application.
-Magnet application can possibly trigger the EOL indicator and change the pacing mode from dual chamber to single chamber.
class recommendations
Class I
Benefit >> Risk
Evidence and/or general agreement that a given treatment or procedure is beneficial, useful, effective
Class IIa
Benefit > Risk
Weight of evidence/opinion is in favour of usefulness/efficacy
Class IIb
Benefit = Risk
Usefulness/efficacy is less well established by evidence/opinion
Class III
Risk > Benefit
Evidence or general agreement that the given treatment or procedure is not useful/effective, and in some case may be harmful
diagnostic assesment
In order for a patient to be indicated for a CRMD, their cardiac condition should be documented by one or more diagnostic assessments.
sympotoms due to brady, tach or HF
Presyncope or syncope
General fatigue, poor or decreased exercise tolerance
Decreased mental acuity
Palpitations, skipped or irregular beating, or rapid heart rates
Signs and symptoms of heart failure: shortness of breath, jugular venous distension, enlarged liver on palpation, weight gain, ankle edema.
12 lead
A 12 lead ECG or rhythm strip during the symptomatic episode provides a definitive diagnosis. An ECG may also provide information about structural heart disease such as LBBB, Q waves, prolonged QT interval, etc.
ambulatory ecg monitor
Bradycardia or conduction disease secondary to structural heart disease is often intermittent in nature which makes it difficult to capture at the time of a 12 lead ECG. Prescribing a holter monitor or event recorder maybe effective in confirming symptoms with the rhythm disturbance
ETT
Exercise tolerance testing is performed to assess chronotropic response to exercise and to assess for presence of exercise induced arrhythmias and myocardial ischemia.
Carotid Sinus Massage
Carotid sinus massage (CSM) is performed to confirm if carotid sinus hypersensitivity and cardioinhibitory to carotid sinus pressure is the cause of presyncope or syncope. CSM is performed under continuous ECG monitoring.
tilt table test
Tilt table testing is performed to evaluate whether syncope is related to a cardioinhibitory response or vasodepressor response.
ILR
an implantable loop recorder (ILR) may be prescribed for the patient with persistent symptoms. The ILR is a leadless, subcutaneous cardiac monitor that can be implanted for up to 3 years. An ILR is the approximate size of a USB memory stick and can be effective for identifying abnormal rhythms.
EP studies
An EP study is effective in determining the need for a pacemaker but it is rarely chosen to solely assess for pacemaker insertion. An EP study may be used as an additional tool in the evaluation of patients with syncope in whom bradycardia is suspected but has not been documented with other non-invasive diagnostic assessments. EP studies may also be conducted to confirm if supraventricular or ventricular tachycardias are the cause of presyncope or syncope
ICD indication
people with a high risk of ventricular tachyarrhythmias
primary prevention
a patient that has cardiac disease but no significant vent tachy arrythmia