intro to critical care- clin med
1/85
Earn XP
Description and Tags
clin med 1
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
86 Terms
ways to deliver oxygen to pts
nasal cannula
simple face mask
venturi mask
mid flow nasal cannula
non-rebreathing mask
HiFlow
CPAP
BiPAP
ventilators
nasal cannula
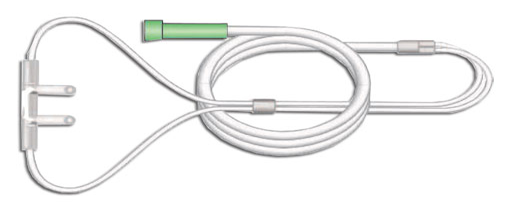
if the NC is set to < 4 lpm . . .
humidity is not required
a simple face mask delivers
35-50% O2 at flows of 6-10 lpm
a simple face mask is used for
short term use only
what can you not use a simple face mask at?
flows of less than 6 lpm
a simple face mask does not require
humidity
simple face mask

a simple face mask can be used for delivery of
inhaled medications
bronchodilators, steroids, narcan
venturi mask

venturi masks deliver
24-50% O2 depending on which connector is used
a venturi mask is an accurate way to
deliver O2
venturi masks are ideal for
CO2 retainers or hypoxic drive pts
when using a venturi mask be sure to
ensure connectors are not covered
never use bubbler humidifier
mid flow nasal cannula

a mid flow nasal cannula
provides higher fiO2 than traditional NC
mid flow NC
O2 flow 7-15 lpm
humidified
non-rebreathing mask

NRB delivers
80-100% O2 at flows of 12-15 lpm
with a NRB, the reservoir bag must
not collapse during inspiration, if it does you should increase the flow
with a NRB you should
never humidify
do not remove one-way valves
HiFlow

HiFlow delivers the
highest percentage of O2
how does HiFlow work?
oxygen is blended with compressed air up to 50 psi
gas is heated to 37 C and humidified to near 100%
cannula should occlude approx. 50% of nares
normal pH in an ABG
7.40 (7.35-7.45)
normal PCO2 in ABG
40 (35-45 mmHg)
normal HCO3- in ABG
24 (22-26 mmol/L or meq/L)
normal Na+
135-145 mEq/L
normal K+
3.5-5.0 mEq/L
normal Cl-
96-109 mEq/L
normal total CO2
24-30 mEq/L
if pH is less than 7.4
acidosis
if pH is greater than 7.4
alkalosis
if acidotic and CO2 is increased
respiratory
if acidotic and CO2 is decreased
metabolic
if alkalosis and CO2 decreased
respiratory
if alkalosis and CO2 increased
metabolic
if pCO2 and Bicarb move in the saME direction, it’s
primary MEtabolic
if pCO2 and Bicarb more in a diffeREnt direction, it’s
primary REspiratory
Aa Gradient
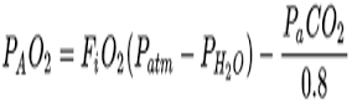
normal Aa gradient is
Normal= age/4 + 4
CPAP is a
fixed positive pressure throughout the respiratory cycle
CPAP appears to be more
effective in reducing the need for tracheal intubation and possibly mortality in pts presenting with ACPE
CPAP is the first line tx for
OSA
BiPAP
when the ventilator delivers different levels of pressure during inspiration (IPAP) and expiration (EPAP)
BiPAP ventilation appears to be more effective in
reducing mortality and the need for tracheal intubation in pts with an acute decompensation of COPD
CPAP/BiPAP indications
respiratory distress secondary to suspected CHF
acute cardiogenic pulmonary edema
pneumonia
COPD (asthma, bronchitis, emphysema)
OSA
CPAP/BiPAP contraindications
unconsciousness
suspected PTX
inadequate respiratory drive
shock/hypotension
chest wall trauma
persistent N/V
active upper GI bleed or hx of recent gastric surgery
CPAP/BiPAP problems related to pressure
sinus pan
gastric insufflation
PTX
CPAP/BiPAP problems related to airflow
dryness
nasal congestion
eye irritation
CPAP/BiPAP other complications
claustrophobia
air leaks from poor mask seal
pressure sores at nasal bridge or face
CPAP settings
pts suspected with ACPE set to 10 cm H2O
oxygen should be titrated based on PCO2, PaO2, and titrated to the pt SpO2 @ bedside with a target of 88-92%
BiPAP settings
For patients receiving BiPAP start with an IPAP of between 10-15cm H2O (generally not to exceed 25cmH2O), and EPAP of between 4-7cm H2O.
Default 10/5cmH2O
This pressure can be titrated up or down depending on the combination of clinical effect as well as patient comfort.
Failure to improve oxygenation should prompt an increase in fractional inspired oxygen and EPAP.
Oxygenation
Failure to improve the hypercarbia should lead to an increase in IPAP.
Ventilation
Improved ventilation with greater IPAP-EPAP
what is preferred for acute exacerbations of COPD?
BiPAP
interventions that decreased mortality
Noninvasive Ventilation
Mild hypothermia after cardiac arrest (32-34C)
Prone Positioning in ARDS
Low tidal volume ventilation in ARDS
TXA in patients with or at high risk of traumatic hemorrhagic shock
Daily interruption of sedatives in critically ill patients
Albumin in cirrhotic patients with SBP
Assist Control v. PRVC/VC + ventilators
minimize risk of barotrauma d/t high pressure peaks
guarantees delivery of desired tidal volume
decelerating flow pattern may provide better distribution of ventilation and oxygenation
can better meet pt’s inspiratory flow demands
when doing AC/PRVC ventilators what do you need to determine the settings for/what parameters?
RR
tidal volume (Vt)
PEEP
FiO2
inspiratory time and flow trigger
with a NC, the O2 concentration will vary with
pt breathing patterns
NC 1 lpm
24%
NC 2 lpm
27%
NC 3 lpm
30%
NC 4 lpm
33%
NC 5 lpm
35%
NC 6 lpm
38%
the max a NC can be set to is
6 lpm
AC/PRVC- RR
you should use pt hx as well as any lab data available to guide decision
normal RR in adults
12-24 bpm
for a higher pCO2 values on ABG→ AC/PRVC RR
choose a higher initial RR to aid ventilation and correct respiratory acidosis
average total lung capacity of an adult
about 6 L
the tidal volume (Vt) is
the volume of air that is inhaled or exhaled in a single breath
tidal volume
Vt
factors that affect lung volumes→ larger volumes
taller height
higher altitudes
non-obese
factors that affect lung volumes→ smaller volumes
shorter height
lower altitudes
obese
selecting appropriate Vt→ AC/PRVC
volumes > 10 ml/kg can cause severe and accelerated complications such as volutrama, barotrauma, biotrauma; leading to ARDS
standard Vt selection
6-8 mL/kg
Vt selection
calculate predicted body weight (PBW)
Vt selection→ males
males= 50 +2.3 (height (in) - 60)
Vt selection→ females
females= 45.5 +2.3 (height(in) -60)
ARDSnet
strategy using high RR and low Vt (ARDS)
goals of ARDSnet
Vt at 6 mL/kg PBW
PaO2 55-80mmHg or SpO2 88-95%
Plateau pressure </= 30 cm H2O
pH 7.15-7.45
PEEP→ AC/PRVC
a small amount of end-expiratory pressure, my convention 5cm H2O, is used to mitigate alveolar collapse
complications of PEEP
decreased venous return, barotrauma, increased ICP
higher levels of PEEP
can be used to improve hypoxemia or reduce ventilator associated lung injury as in ARDS
FiO2 in AC/PRVC is initially set at
100%
goal of FiO2
titrate down to a goal of <60% as tolerated to avoid complication of O2 toxicity
FiO2 is ideal at . . .
generally at <50% and ideally at 40% before initiating SBT