Infections of the vagina and vulva
1/48
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
49 Terms
3.5-4.5 (anaerobes predominate - lactobacillus produces the acid)
Normal pH of the reproductive women
4.5+ (lower prevalence of lactobacillus)
Normal pH of the Pre-pubertal and Post-menopausal women
Menstrual cycle, antibiotics, douching, unprotected sex, lubes, intravaginal medication
What are somethings that can affect the pH of the vagina and lead to infection?
Bacterial Vaginosis (increased anaerobic rods)
The most common cause of abnormal vaginal discharge in a reproductive female - NOT an STD; produces a fishy-like odor and grey/clear discharge
Multiple or new sexual partners, female partners, oral sex, douching, smoking, IUD
Risk factors for bacterial vaginosis
Gram stain 🏆, Amsel’s Diagnostic Criteria, Single swab with PCR and DNA probe tech (promising - BD affirm VPIII system)
What are the preferred diagnostics for Bacterial Vaginosis
Exam, Swab placed in 10% KOH (whiff test), Swab to mix NS (microscopy), pH over 4.5
What are the Amsel’s Diagnostic Criteria - gotta go 3/4?
Metro PO or intravaginally, Clindamycin cream intravaginally, Secnidazole PO, Tinidazole PO, Clinda PO
Treatment for bacterial vaginosis
Treat acute episodes (2x weekly suppressive metronidazole or intravaginal boric acid followed by metro OR metro and Fluconazole), change abx or change course, condom use for 3-6 months, no benefit from lactobacillus
For refractory cases of bacterial vaginosis (3 documented episodes in 1 year)?
Trichomoniasis (trichomonas Vaginalis)
What is the most prevalent non-viral STD worldwide that can infect the vagina, urethra, endocervix, and bladder?
foul, thin yellow or green discharge; dysuria, dyspareunia, vulvar pruritus, vaginal spotting, and lower abdominal pain
Symptoms for trich (50% are asymptomatic)
Strawberry spots on the cervix, elevated vaginal pH
Clinical findings for Trich
Trichomonas on microscopy, NAAT (most sensitive and specific)
Diagnostics for Trich
metro 🥇, Tinidazole, if allergic to nitroimidazoles → desensitize
Treatment for Trich
3 weeks if preg 🤰, 3 months if not
When should you retest for trich
Vulvar pruritus, burning, erythema, edema with excoriation, cheese-like dischage
Symptoms of yeast infection candidiasis
immunosuppression, DM, preg, recent broad spectrum abx
Risk factors for a yeast infection
Saline and 10% KOH (budding hyphae), Culture 🏆, PCR
Diagnostics for yeast infection
1 dose of fluconazole, topical antifungal (tercazole)
1st occurence of vaginal candiasis
2-3 doses of fluconazole over 3 days
Treatment of DM patients with vaginal candiasis
10-14 days of induction therapy (topical agent or oral fluconazole) then 150 mg fluconazole for 6 months, workup for DM and HIV
4+ candida infections in 1 year
Dorsal root ganglion (sensory nerve)
Where does HSV like to live (life-long latency)
vesicles → ulcer → crusting; burning, severe pain, dysuria low-grade fever, HA, myalgia
Symptoms of HSV - mean incubation is 1 week (primary outbreaks are worse and more widespread)
Cell culture, NAAT 🏆, IgG antibody assay (not super recommended - seroconversion takes 3 weeks)
Diagnosis of HSV
Antiviral (acyclovir, valacyclovir), antipyretic, pain med, suppressive therapy
Treatment for HSV
Chancre (isolated, nontender ulcer with raised rounded border)
Primary syphilis is characterized by
maculopapular rash that develops on the palms, soles, and mucous membranes, condyloma lata
Secondary syphilis (6 weeks to 6 months later) is characterized by
Cardiovascular, CNS, and MSK involvement
Tertiary syphilis (20 years later) is characterized by
Treponema pallidum (spirochete)
Etiology of syphillis
Direct detection of spirochete 🏆, Treponemal and nontreponemal (RPR) testing (seroconversion occurs 3-6 weeks)
Diagnosis of syphilis
Benzathine pen G IM 1x (doxy as an alt)
Treatment for primary, secondary, early latent Syphilis
Benzathine Pen G 3x IM weekly
Treatment for latent, tertiary, cardiovascular syphilis
Chancroid
An STI caused by H.Ducreyi that is characterized by an ulcer with soft irregular margins and friable bases, tender inguinal lymphadenopathy (if large buboes may form)
H. Ducreyi in cell culture, NAAT
Diagnosis for Chancroid
Azithromycin, Ceftriaxone
Treatment for Chancroid
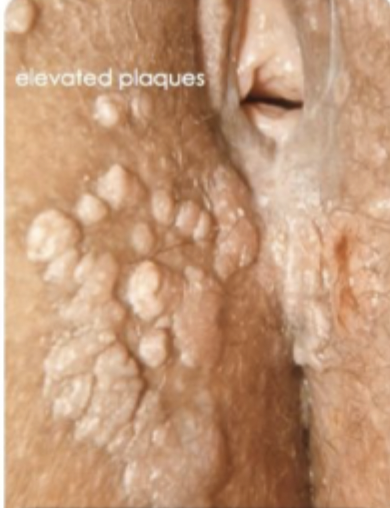
Granuloma Inguinale (Donovanosis)
An vulvar infection caused by Klebsiella Granulomatosis that is characterized by painless, inflammatory nodules that progress to highly vascular nontender ulcers that heal by fibrosis (keloids) - lymph nodes NOT affected
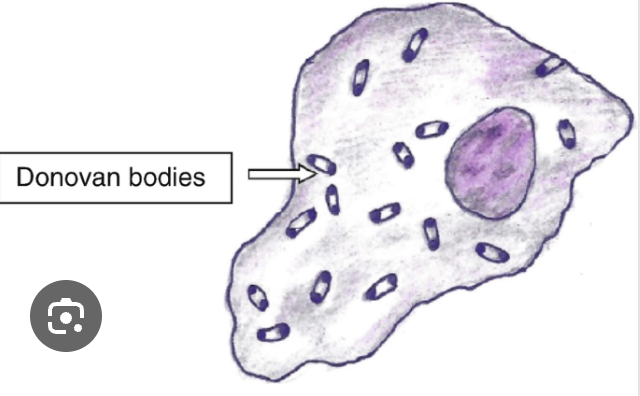
Donovan bodies (closed safety pin) on microscopic eval after wright-giemsa stain
Diagnosis for Granuloma Inguinale
Azithro 1g once weekly for at least 3 weeks
Treatment for Granuloma Inguinale
Chlamydia trachomatis serotypes L1, L2, L3
Etiology for lymphogranuloma venereum
Small painless papule → regional lymphadenopathy → anogenitorectal fibrosis
Stages of lymphogranuloma venereum
Culture/immunofluorescence, NAAT
Diagnosis of lymphogranuloma venereum
Doxy bid for 21 days
Treatment for lymphogranuloma venereum
HPV (86% from 6 and 11)
Etiology for genital warts
flat papulae or classic verrucous exophytic lesions
Findings for genital warts
Visualization on exam, biopsy if neoplasia is suspect, unclear diagnosis, immunosuppression
Diagnostics for genital warts
Sharp excision, electrosurgical needle tip excision, cryotherapy, laser ablation, topical agents (TCA, imiquimod, podofilox)
Treatment for genital warts - no treatment option boast 100% clearence
Multiple 2-5 mm flesh colored papules with central umbilication
Exam findings for Molluscum Contagiosum
Visual inspection if unclear biopsy
Diagnosis for Molluscum Contagiosum
Spontaneously resolve regress (6-12 months), treated by cryotherapy, electrosurgical needle coagulation, sharp needle tip curettage, topical trichloroacetic acid
Treatment for Molluscum Contagiosum