Respiratory Viral Diseases
1/90
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
91 Terms
what are the major viral respiratory pathogens?
influenza
respiratory syncytial virus (RSV)
common cold viruses (rhinoviruses, adenoviruses, coronaviruses)
emerging coronaviruses
influenza: symptoms
– fever, chills, headache, sore throat, general malaise
– Often, severe acute disease
influenza: encounter
– droplets, fomites (virus survives for hours on surfaces)
– More efficient transmission at low temperature and low humidity (winters)
influenza: entry
respiratory route
influenza: incubation period
1-3 days
influenza: contagious period
A person is contagious from 1 day before to 7 days after the onset of symptoms
influenza: complications
– Pneumonia, secondary bacterial infections
– Fatalities in the elderly, infants
annual influenza epidemics occur what time of year and due to what?
dec-mar
due to antigenic drift (small antigenic changes in virus)
occasional influenza pandemics occur how often and due to what?
irregular 10-50 year intervals
due to antigenic shift (large antigenic changes in virus)
which influenza strain caused the 1918 Spanish Influenza (20-40 million deaths)?
H1N1
which influenza strain caused the 1957 Asian Influenza (1-2 million deaths)?
H2N2
which influenza strain caused the 1968 Hong Kong Influenza (700,000 deaths)?
H3N2
which influenza strain caused the 2009 Swine Influenza (12,000 deaths)?
H1N1
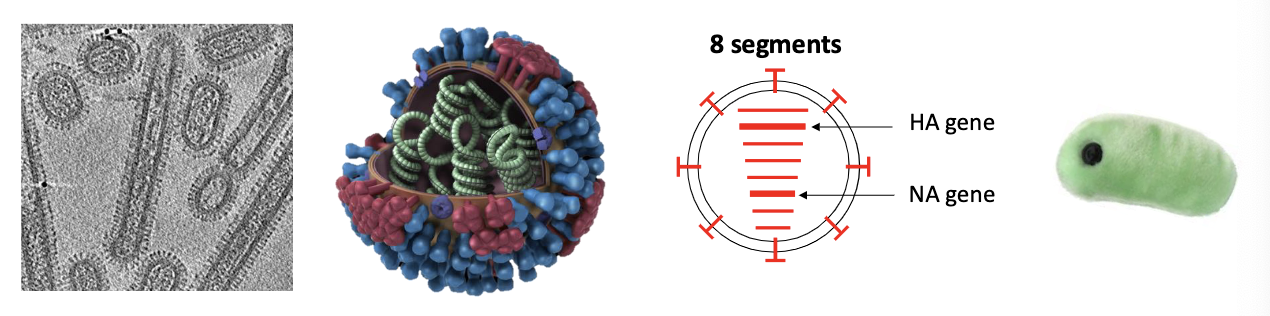
what kind of genome does influenza have?
negative-sense single-stranded segmented RNA genome (enveloped)
how many segments does influenza’s RNA genome have?
8 different segments (virus needs all 8)
most segments encode 1-2 proteins
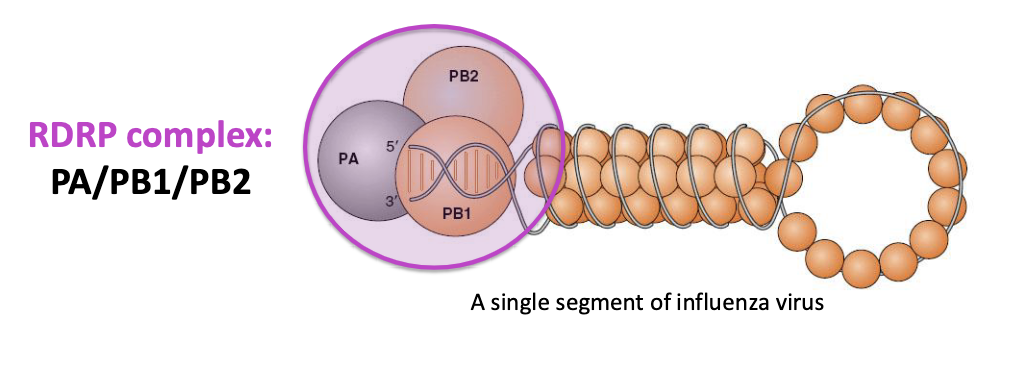
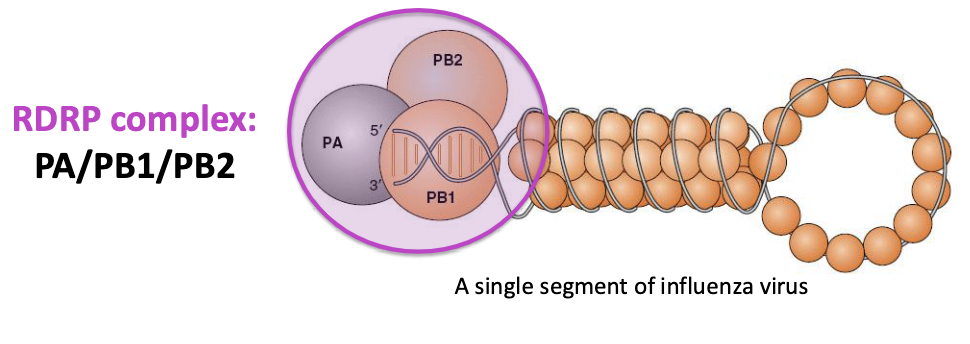
what replicates and transcribes the infleunza viral genome?
RNA-dependent RNA polymerase (RdRp)
this is targeted by current antivirals
what does it mean that RdRp has low fidelity?
makes frequent mistakes but does not correct them (leads to high genetic diversity aka complex classification)
what is the RDRP complex made up of?
PA/PB1/PB2
type A influenza infects what hosts?
humans, other mammals, birds (can cause epidemics and pandemics)
what are type A influenza reservoirs?
migratory aquatic birds
type B influenza infects what hosts?
mainly humans
type A infleunza causes epidemics/pandemics? type B?
type A → epidemics AND pandemics
type B → only epidemics
50% of annual influenza cases are which type?
type B
in wild birds, influenza is pathogenic/nonpathogenic.
nonpathogenic (replicates in gut and excreted into water)
how do new influenza A strains emerge?
constantly emerge from birds and spread to birds/mammals (including humans)
influenza A is divided into what subtypes?
H and N
18 subtypes of HA
11 subtypes of NA
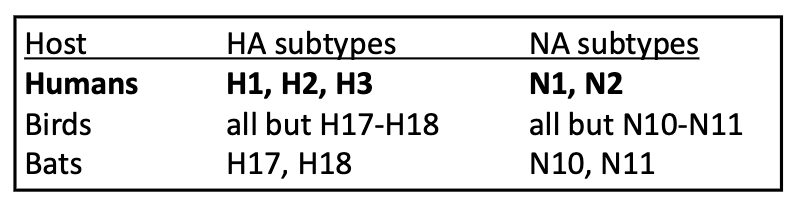
which influenza strains are capable of sustained transmission among humans?
only H1N1 and H3N2
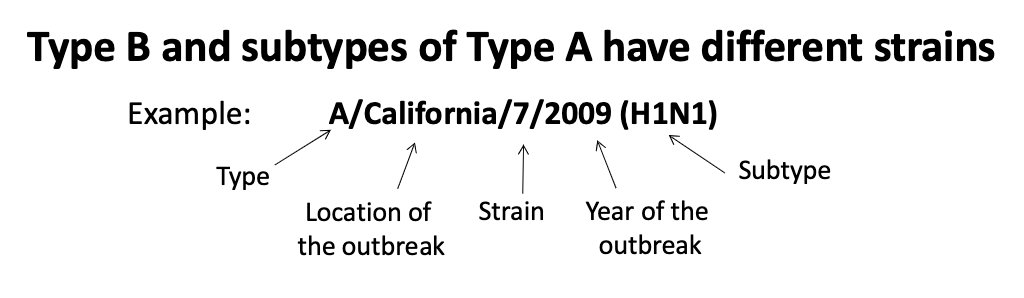
how are influenza strains named?
type, location of outbreak, strain, year of outbreak, subtype
influenza strains are species-specific. avian influenza binds to what cell receptors? human influenza?
Avian influenza
Binds alpha-2,3-sialic acid
Avian enteric tract
Human influenza
Binds alpha-2,6-sialic acid
Human respiratory tract
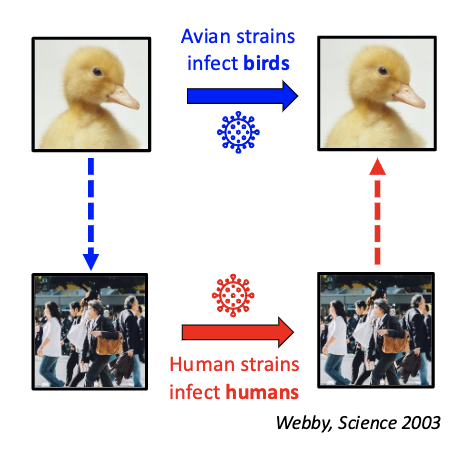
why does avian influenza RdRp not work well in human cells?
Avian hosts have a higher T than our airways
Protein interactions restrict viral polymerase activity
Avian Influenza strains must _______ to achieve efficient transmission
mutate
what are some important influenza proteins and what do they do?
hemagglutinin (HA)
viral entry into host cell
neuraminidase (NA)
release of progeny virions from cell
HA and NA are antigens and undergo …?
antigenic variation (drift vs shift)
• mutate such that pre-existing antibodies do not recognize them
what is antigenic drift?
random mutations (because RdRp is error-prone)
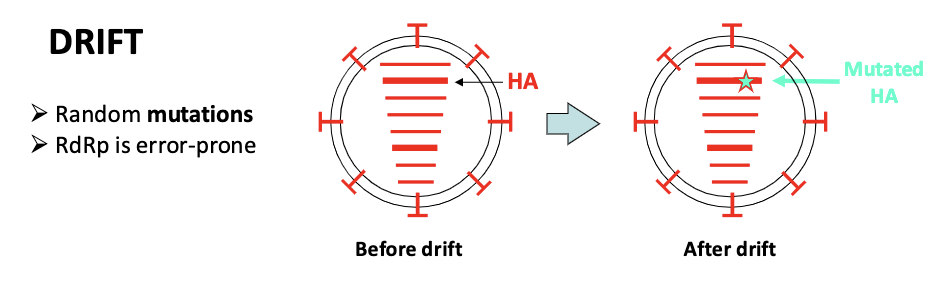
what are outcomes of antigenic drift?
epidemics
annual vaccinations
what are outcomes of antigenic shift?
existing immunity does not offer protection
pandemics
what is antigenic shift?
segment reassortment
can occur in mixed infections
very rare
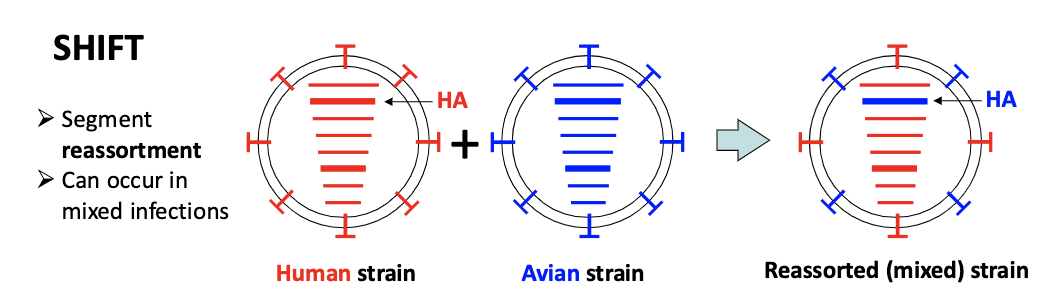
what animal is a “mixing vessel” for influenza reassortment? why?
pig
have both α(2,3)-and α(2,6)-linkage sialic acid
dense populations of SE Asia
if a new reassortment virus infects humans → no preexisting immunity → pandemic
H5N1 and H7N9 subtypes can sometimes infect humans. what does this result in?
avian influenza in humans
what is the main concern about avian influenza in humans?
bird and human influenza could undergo reassortment and yield a strain that is both highly contagious and virulent
Virus has not yet acquired the ability to infect humans easily or to be passed efficiently from person to person
avian influenza in humans is ______ contagious but _____ virulent.
mildly contagious (few human-human transmission)
highly virulent (H5N1 and H7N9 cause high mortality)
what are some influenza laboratory diagnoses?
rapid influenza diagnostic testing (RIDT)
fast but more false negatives
detect infleunza antigens
RT-PCR
(more accurate but takes longer)
detect influenza genomes
viral culture and isolation
influenza: prevention
hygiene
disinfection
vaccination
influenza vaccines are manufactured/administered every _____
year (based on strains from previous year’s flu season)
each hemisphere designs vaccines based on pervious season in the other hemisphere
when developing influenza vaccines, different combinations of strains can be used. what types?
Trivalent: a Type A H1N1 strain, a Type A H3N2 strain, and one Type B strain
Quadrivalent: a Type A H1N1 strain, a Type A H3N2 strain, and 2 Type B strains
what is an inactivated vaccine (IIV3)? and how is it administered?
Formaldehyde-treated virus
injection
what is a reconbinant vaccine (RIV3)? and how is it administered?
purified recombinant HA proteins
injection
what is a live attenuated vaccine (LAIV3)? and how is it administered?
cold-adapted, temperature-sensitive strain
nasal spray
effectiveness and safety of inactivated (IIV3) vaccine
60-90% (in healthy adults)
safe for anyone >6 mo
effectiveness and safety of recombinant (RIV3) vaccine
45-70% (in healthy adults)
effectiveness and safety of live attenuated (LAIV3) vaccine
90%
safety level of inactivated (IIV3) vaccine
anyone > 6mo
safety level of recombinant (RIV3) vaccine
anyone >18 yo
safety level of live attenuated (LAIV3) vaccine
healthy 2-49 yo (mucosal immunity)
how do antivirals work?
block NA
block RdRp
block M2 (but useless now due to resistance/drift)
antivirals should be used for what patients? but why should it be used sparingly?
people at risk of serious flu complications (children, elderly, pregnant)
resistance can develop quickly
antivirals must be adminstered within __days of symptoms
2
TRUE or FALSE?
A. Bats serve as reservoirs of Type A Influenza viruses
B. Influenza virus envelope bears two important viral antigens
C. Influenza virus is a double-stranded DNA virus
D. Only H1-H3/N1-N2 Influenza viruses are capable of sustained transmission among humans and causing pandemics
F: Bats serve as reservoirs of Type A Influenza viruses
T: Influenza virus envelope bears two important viral antigens
F: Influenza virus is a double-stranded DNA virus
T: Only H1-H3/N1-N2 Influenza viruses are capable of sustained transmission among humans and causing pandemics
All of the following statements about Influenza are correct EXCEPT one. Which is the EXCEPTION?
A. Health-care workers are at increased risk of acquiring influenza infection and, if infected, may transmit virus to their patients
B. Influenza pandemics occur at irregular and unpredictable intervals
C. Influenza virus is spread from person to person exclusively by respiratory droplets
D. Quadrivalent influenza vaccine typically consists of two Type A strains and two Type B strains
C. Influenza virus is spread from person to person exclusively by respiratory droplets
All of the following statements about antigenic changes in the Influenza virus are correct EXCEPT one. Which is the EXCEPTION?
A. Influenza A may undergo antigenic drift
B. Influenza B may undergo antigenic drift
C. Influenza A may undergo antigenic shift
D. Influenza B may undergo antigenic shift
D. Influenza B may undergo antigenic shift
Respiratory syncytial virus (RSV): transmission
– Droplets, aerosols, fomites
– Winter months
– Very common: by 2 yo nearly everyone is seropositive; frequent reinfections
Respiratory syncytial virus (RSV): disease manifestation
adults → URIs
children → laryngotracheobronchitis
older adults → severe heart/lung disease
Respiratory syncytial virus (RSV): damage is caused by…?
both RSV and host response
what is Bronchiolitis?
swelling and mucus buildup in the bronchioles (RSV infection in infants)
The bronchi carry air into your lungs
The bronchioles (at the end of the bronchi) carry air to small sacs called alveoli
The alveoli perform the gas exchange
what are symptoms of Bronchiolitis?
– Tachypnea (rapid breathing)
– Wheezing, lung hyperinflation
– Cyanosis
– Fever
what are some high-risk conditions for RSV infection in infants?
premature
pulmonary disease
congential heart disease
immunocompromised
RSV infections in infants: diagnosis
Rapid antigen test on nasopharyngeal aspirates
RSV infections in infants: treatment
oxygen tent, IV fluids
RSV infections in infants: prevention
passive immunization with an anti-RSV antibody (Palivizumab or Nirsevimab) in high-risk infants
vaccine during pregnancy (32-36 w)
what is key to dealing with RSV infections in infants?
rapid diagnosis and treatment
what account for 1/3 to 1/2 of all acute respiratory infections in humans?
common cold viruses
symptoms of common cold viruses? complications?
• Symptoms: rhinitis, sneezing, coughing, sore throat
• Complications: secondary bacterial infections
40-50% cases of common cold viruses are what kind of viruses? 10-30%? the rest?
• 40-50% cases – rhinoviruses
• 10-30% cases – coronaviruses (seasonal)
• rest - adenoviruses, RSV, and parainfluenza viruses
• symptoms indistinguishable
rhinoviruses: transmission
– Droplets, aerosols, fomites
– Winter months
rhinoviruses: complications
– sinusitis, otitis media, asthmatic bronchitis
there are >100 serotypes of rhinoviruses. what does this mean?
high antigenic variability
t/f: rhinovirus vaccine is likely.
false
how do adenoviruses work?
Can infect different organs
– Respiratory: common cold, pharyngitis, cough
– GI: diarrhea in children
– Eyes: conjunctivitis, i.e., “pink eye” (swimming pools)
– Lungs: acute pneumonia (military recruits)
– Disseminated infections in transplant patients
what’s an example of a adenovirus outbreak?
2018
– an outbreak at U. of Maryland (>40 cases, 1 death)
– an outbreak at New Jersey rehabilitation center (11 deaths)
what are the emerging human coronaviruses since 2003?
• SARS-CoV (2003)
• MERS-CoV (2012)
• SARS-CoV-2 (2019)
Highly pathogenic
Severe respiratory disease
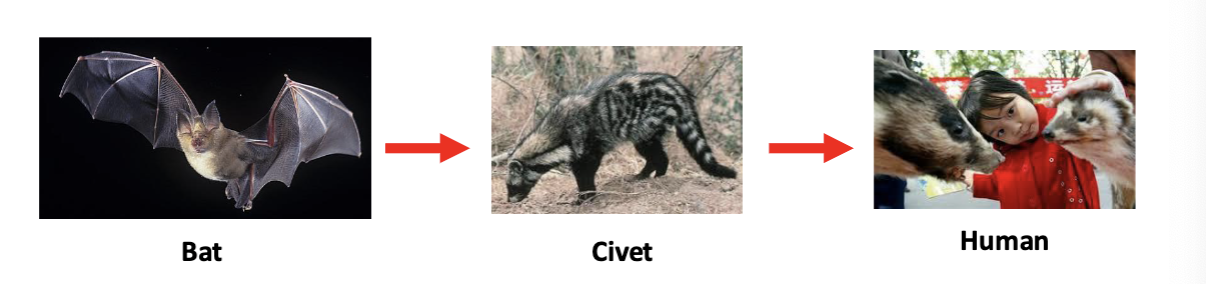
SARS-CoV:
place/year of origin
duration
mortality rate
human-to-human transmission
• Started in 2003 in Guanzhou, China
• Ended in eight months
• 8098 infections, 9.6% mortality
• 87% in China and Hong Kong
human-to-human transmission was common
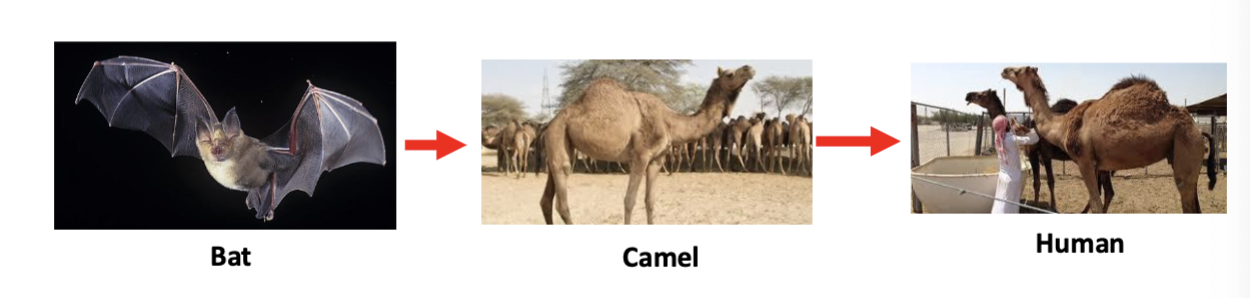
MERS-COV
place/year of origin
duration
mortality rate
human-to-human transmission
• Since 2012
• Mostly in Arabian peninsula
• Camels are a reservoir for MERS-CoV
• 2591 cases, ~35% mortality
human-to-human transmission was limited
SARS-CoV-2 (Covid-19):
place/year of origin
duration
mortality rate
human-to-human transmission
• 2019, Wuhan, China
• Global Covid-19 (WHO, as of 9/22/2024)
• Total cases: ~776 million
• Total deaths: ~7 million (~0.9% total cases)
• Total vaccine doses: ~13.6 billion
human-to-human transmission is common
SARS-CoV-2 (Covid-19): transmission
Respiratory transmission
– Droplets, aerosols, fomites
SARS-CoV-2 (Covid-19): disease
– Asymptomatic or mild, flu-like (~81%)
– Severe: pneumonia, shortness of breath (~14%)
– Critical: respiratory failure, septic shock, multiorgan failure (~5%)
– Risk of severe disease increases with age
SARS-CoV-2 (Covid-19): complications
– Long COVID
– Potentially: virus persists in the gut and causes a drop in serotonin levels
SARS-CoV-2 (Covid-19): vaccines and treatment
• Vaccines: recombinant (mRNA-based, protein-based)
• Treatments: Paxlovid
which of the common and emerging cold viruses cause mild illness versus severe disease?
• Rhinoviruses, adenoviruses, and seasonal coronaviruses mostly cause mild illnesses
• Emerging coronaviruses can cause severe disease
Are the following statements about Respiratory Syncytial Virus (RSV) TRUE or FALSE?
A. No vaccine against RSV is currently available
B. Passive immunization can be used to prevent infections
C. Rapid diagnosis of RSV infections is essential for successful treatment
D. RSV infections in newborns are typically mild and self-resolving
F: No vaccine against RSV is currently available
T: Passive immunization can be used to prevent infections
T: Rapid diagnosis of RSV infections is essential for successful treatment
F: RSV infections in newborns are typically mild and self-resolving
TRUE or FALSE?
A. Most cases of common colds are caused by circulating coronaviruses
B. Emerging human coronaviruses occasionally cause outbreaks of severe respiratory disease
C. Vaccines against rhinoviruses are administered annually
D. Adenoviruses can infect multiple organs
F: Most cases of common colds are caused by circulating coronaviruses
T: Emerging human coronaviruses occasionally cause outbreaks of severe respiratory disease
F: Vaccines against rhinoviruses are administered annually
T: Adenoviruses can infect multiple organs