Transport in Animals
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
42 Terms
What is the need for transport systems in multicellular animals
Larger organisms have longer transport distances to exchange sites so simple diffusion alone is too slow
Low SA:V ratio less surface area for absorption of nutrients and loss of waste - longer diffusion distance
Higher level of metabolic activity
Open Circulatory System
Transport medium can diffuse out blood vessels
Closed Circulatory System
Blood is confined to blood vessels
Single Circulatory System
Blood only passes through the heart once per circuit
Double Circulatory System
Blood passes through the heart twice per circuit
Pulmonary Circuit carries blood heart —> lungs (pick up oxygen remove carbon dioxide)
Systemic Circuit carries blood heart —> body (deliver oxygen)
Arteries Structure and Function
Thick smooth muscle layer Withstand high pressure
Elastic fibers – Allow stretching and recoiling for smooth flow.
Narrow lumen – Maintains high pressure
Collagen for support
Dilate and Constrict to control blood volume
Arterioles Structure and Function
Thicker muscle layer than arteries to restrict blood flow in capillaries
Branch of arteries into narrow blood vessels - transport blood to capillaries
Smaller than arteries to make pressure change more gradual
Thin Collagen and elastic layer
Capillaries Structure and Function
One cell thick squamous epitehlial cells short diffusion distance
Highly branches for large surface area - maximise gas exchange
Slows blood flow – Allows more time for diffusion
Narrow - sqaush red blood cells - maximise diffuion
Venules Structure and Function
Branch off of veins to transport blood to capillaries
Smaller than veins to make pressure change more gradual
Contains valves to prevent backflow
Veins Structure and Function
Thin muscle layer - Low risk of damage as blood is carried at low pressure (DO2 to heart)
Wide lumen - helps blood flow by less pressure
Contains valves to prevent backflow
No collagen or elastic layer
How is tissue fluid formed?
High hydrostatic pressure as arteriole end is wider diameter than capillary with same volume of blood
Forces out water and small moleules out of gaps in capillaries
Why is tissue fluid useful
All Substances e.g. water, glucose, amino acids, water, ions, oxygen can re - enter cells if needed
Waste products picked back up and removed
Hydrostatic pressure
(pressure exerted by liquid)
oncotic pressure
(tendency of water to move into blood via osmosis)
Why does more blood move out capillaries than in?
Hydrostatic pressure is greater than oncotic pressure so net movement of liquid is out of blood capillaries
Why is oncotic pressure high
Large molecules like plasma proteins are too large to fit through capillary gaps
Water moves via osmosis to capillaries
Once equilibrium is reached liquid left goes into lymphatic system
Why does cardiac muscle automatically contract and relax and never fatigue
It is myogenic
What do coronary arteries do
Supply the cardiac muscle with oxygenated blood for aerobic respiration
This provides ATP so cardiac muscle can continually contract and relax
Why is left ventricle wall thicker than right?
So it can contract with more force and pump blood at a high pressure
This is because it pumps blood out of aorta around whole body to recieve oxygenated blood
Why is right ventricle muscle thin
Doesn’t need to contract with as much force - lower pressure only pumps to lungs
Blood needs to flow through lungs and low pressure so doesn’t damage capillaries in lungs
Blood flows slowly at low pressure allowing more time for gas exchange
Why are atria walls so thin
Only pumps blood to ventricles which are very close needing minimal force
Also assisted by gravity
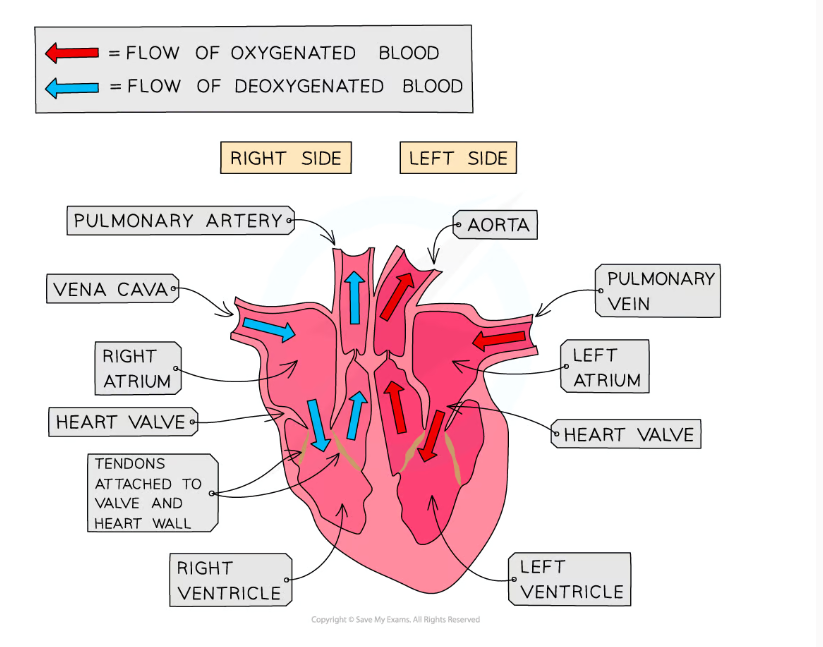
Structure of Mammalian Heart and blood flow
Deoxygenated Blood —> Vena Cava —> Right atrium —> Right Ventricle —> Pulmonary Artery
Oxygenated Blood —> Pulmonary Vein —> Right Atrium —> Right Ventricle —> Aorta
Cardiac Cycle
Atrial Systole - Walls of atria contract decreasing volume increasing pressure above ventricles opening AV valve
Blood is forced into ventricles and ventricles are relaxed in diastole
Ventriuclar Systole When blood fills ventricle walls contract volume decreases/ pressure increases above atria closing AV valves close to stop bacflow
Ventricular pressure rises above aorta and pulmonary arterey opening SL valve forcing blood out heart
Diastole Atria relaxes starts to be filled with blood and then ventricles relax
Pressure in ventricles drop closing SL valve
Blood flows into atria via pulmnoary vein and vena cava till pressure rises above ventricles opening AV valves
Blood trickles passively into ventricles
How do you calculate Cardiac Output?
Heart Rate x Stroke Volume
What is cardiac output?
The volume of blood that leaves the ventricle in one minute
Heart rate
Heart beats per minute
Stroke volume
Volume of blood that leaves the heart each beat
Control of cardiac cycle
Sinoatrial node releases a wave of The sinoatrial node (SAN) generates a wave of depolarization, causing the atria to contract (atrial systole).
The depolarization reaches the atrioventricular node (AVN), where there is a slight delay to ensure the ventricles contract after the atria.
The AVN sends the signal through the Bundle of His down the septum and into the Purkyne fibers.
The ventricles contract from the apex upward, ensuring efficient blood ejection
short delay as AVN transmits second wave - to allow atria to fill ventricles
Heart repolarizes
Electrocardiogram
A machine which measures the waves of depolarisation for irregularities
Tachycardia
When the heart is beating at over 100bpm - abonrmally fast
Bradycardia
When the heart is beating at less than 60bpm. May be too low, however fitter may contract harder
Fibrilation
Irregular heart beat or chaotic rhytm if heart
Ectopic Heartbeat
Additional heartbeats which are not in rhythm
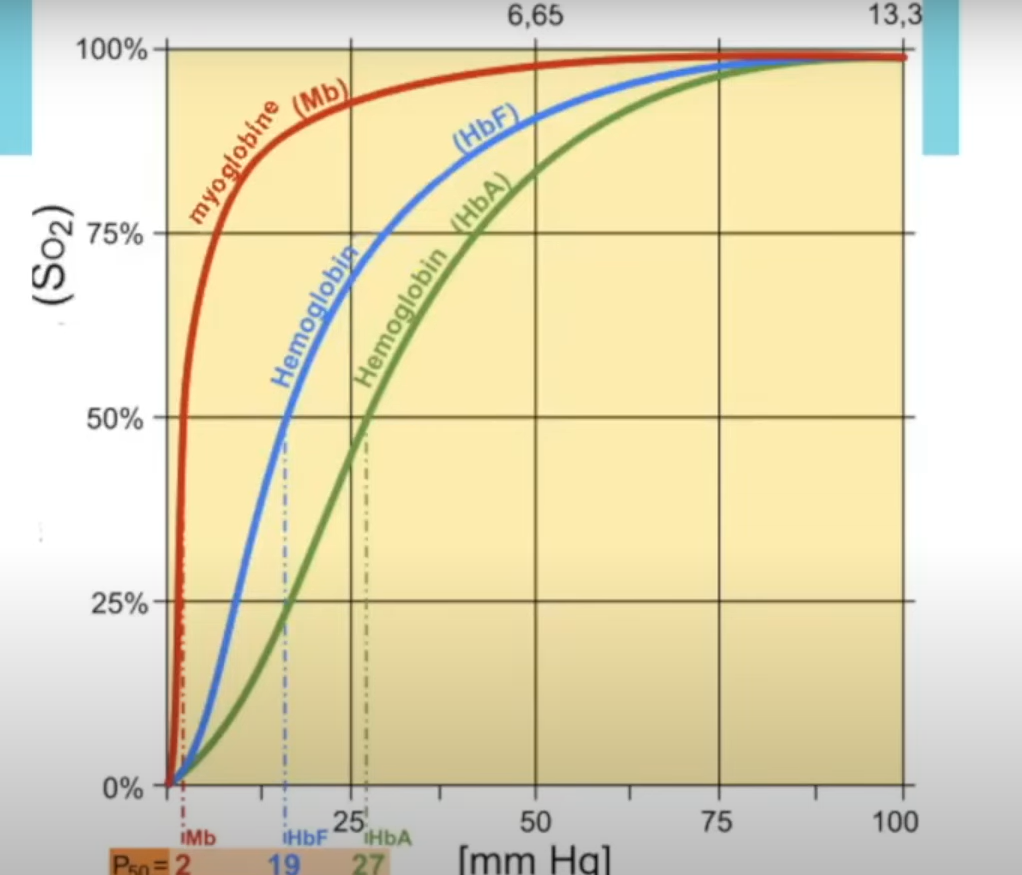
How do saturation of O2 pressure interact in Oxygen Dissosiactive Curve?
Percentage Saturation of O2 is lower at low O2 Partial Pressure (affinity is low at respiring tissues dissociates)
Percentage Saturation of O2 is high at high O2 Partial Pressure (high affinity at alveoli)
Why does the curve get steeper
Due to cooperative binding O2 binding causes conformational change in haemoglobin shape making it easier for further O2 to bind.
Bohr effect
High CO2 conc reduces the affinity of haemoiglobin for O2 as ph decreases
Why is Bohr effect useful
Same partial pressure of O2 at lower pH - high CO2 SHIFTS TO RIGHT
Far less oxygen is bound and is dissosciating at (site of repsiration)
Structure of haemoglobin
4 haem group with 2 alpha chains, 2 beta chains
shape is the oxygen dissociation curve
Sigmoid/S
Describe oxygen dissociation curve for fetal and adult human haemoglobin.
Fetal haemoglobin curve shifts to LEFT
Same partial pressure of O2 fetal Hba is more saturated with O2
This is because has to get O2 from mothers haemoglobin - must dissosciate O2 from adult to bind to fetal hba
What are the three ways CO2 is transported?
Dissolved in blood plasma
As carbaminohaemoglobin
85% In rbcs as hydrogen carbonate ions
Cholride Shift
Carbonic anhydrase in rbcs catalyses H2O and CO2 to form Carbonic acid
Carbonic acid dissociates to form hydrogen ions and hydrogen carbinate ions
Haemoglobin binds to H ions and dissociates from O2 forming haemoglobonic acid
Hydrogen carbonate ions diffuse out and chloride diffuses in - both negative