Advanced Nursing Exam 2: Key Terms & Definitions
1/89
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
90 Terms
regulation of the heart: sympathetic nervous system
increase HR, increases contraction force, increases BP
regulation of the heart: parasympathetic nervous system
activated with stimulation of vagus nerve; decreases HR
regulation of the heart: baroreceptors
o located in the aortic arch in the carotid
o ensures BP remains normalized
regulation of the heart: chemoreceptors
o in aortic arch in carotid bodies & medulla
o increases respiratory rate & BP in response to increase CO2
preload vs afterload
Preload is the force that stretches the cardiac muscles prior to contraction (filling, total body volume) - reduced via diuretics
Afterload is the load/force the heart pumps against - reduced via vasodilators & HTN meds
What is blood pressure's relationship with preload and afterload?
o Higher preloads and afterloads will lead to lowered cardiac output
o If BP is high, afterload is high
o If BP is low, preload is low
Where is the PMI? How does this change with ventricular hypertrophy?
o PMI = midclavicular 5th ICS
o may lower in patients with ventricular hypertrophy & become more lateral to the midclavicular line
What is troponin and how does it trend?
o biomarker of choice in the diagnosis of ACS
o detectable within 4 to 6 hours of MI, peak at 10 to 24 hours, and can be detected for up to 10 to 14 days
What is creatinine kinase and how does it trend?
o specific to cardiac muscle injury
o Rises within 3-6 hours, peaks at 12-24 hours, returns to baseline within 12-48 hours
What is CRP?
Inflammatory marker
What is homocysteine?
elevated levels indicate increased risk for CAD, PVD, and stroke
What is BNP?
marker of choice for distinguishing a cardiac or respiratory cause of dyspnea (high levels = heart)
Patient teaching for hypertension:
o symptoms/diagnosis do not usually onset until organs have been damaged
o Lifestyle changes should begin with prehypertension
o Simple 7: manage BP, control cholesterol, reduce BS, get active, eat better, lose weight, stop smoking
o Mediterranean diet (fish + chicken > red meat)
drugs for HTN: adrenergic inhibitors, ACE inhibitors, ARBs
o Adrenergic inhibiting agents — decrease SNS stimulus
o ACE Inhibitors — help with water & sodium retention
o A-II receptor blockers — act in the RAAS system
drugs for HTN: CCBs, direct vasodilators, diuretics
o Calcium channel blockers (CCB) — increase sodium excretion & help dilate the vessel
o Direct vasodilators — dilate vessel to decrease SVR
o Diuretics — decrease plasma volume
drugs for HTN crisis:
sodium nitroprusside (vasodilator), nitroglycerine, cardene (CCB)
If a patient is receiving a drug that reduces afterload, you should assess their:
blood pressure
Classification of HTN:
Normal: < 120/80
PreHTN: 120-129/> 80
Stage 1: 130-139/80-89
Stage 2: > 140/>90
Primary vs Secondary HTN:
o Primary: elevated BP of unknown cause
o Secondary: elevated BP with specific cause (only 5-10% of all cases)
What is cardiac output? How is it calculated?
o total blood flow through systemic or pulmonary circulation per minute (usually around 4-8L/min)
o CO = SV × HR
o SV= volume of blood pumped from L ventricle per beat
What is hypertensive crisis? (diagnostic level, risks, s/s, treatment)
o >180/>120
o Often seen in people with a history of HTN or with drug abuse
o s/s: HA, n/v, seizures, confusion, renal insufficiency, MI, HR, pulmonary edema, chest pain, dyspnea
o treated with hospitalization & IV drugs at a slow titration (goal MAP: 110-115)
What is a cardiac catheterization? Why is this test performed?
o Procedure: catheter inserted into arm, groin, upper thigh, or neck toward your heart
o Right-sided done to measure pressures, filling pressures, and lungs (Swan line purpose) - heart failure, hemodynamic issues
o Left-sided to done evaluate coronary arteries - STEMI & non-STEMI
After PCI and stent, thrombosis prevention includes...
o Dual therapy with aspirin + Plavix
o Effective if return of ST segment
o Monitor for s/s of bleeding
Modifiable & unmodifiable coronary artery disease risk factors:
Unmodifiable: age, gender (men), ethnicity (Caucasian), family history, genetics
Modifiable: Elevated serum lipid, HTN (>140/90), tobacco use & secondhand smoke – decreases estrogen in premenopausal women, physical inactivity, poor diet
How does high lipid levels effect CAD?
o Hyperlipidemia leads to increased platelet aggregation
o LDLs contain more cholesterol and attract more to arterial walls
Nursing interventions decrease the oxygen demand of the heart:
o Enhanced breathing techniques (pursed-lip breathing)
o Incentive spirometry
o Limit activity to decrease heart rate
o Beta-blockers
What does stable angina feel like?
o Occurs when 70%+ of arteries are blocked
o Lasts the same length of time each time it happens, occurs from the same causes, happens regularly
o Usually lasts < 10 minutes
o Relieved with rest, position changes, or nitrate use
EKG finding of acute MI:
For STEMIs, an ECG will show elevations of the ST segment
medications for angina: nitroglycerine, morphine, beta blockers
o IV nitroglycerin (NTG) - vasodilator; first choice med; causes hypotension
o Morphine - choice for chest pain that is not relieved by nitro, also relieves anxiety
o β-adrenergic blockers - lowers HR, BP, and contractility; reduces the risk of a second heart attack
medications for angina: ACE inhibitors, antidysrhythmics, stool softeners
o ACE inhibitors - stabilize BP & prevent ventricular remodeling; use ARB if cough or edema occurs
o Antidysrhythmic drugs - used for life-threatening dysrhythmias
o Lipid-lowering drugs
o Stool softeners - bowel regimen to prevent bearing down or constipation
Why is nitroglycerine given?
o Can be given to relieve chest pain and prevent chest pain
o Helps to vasodilate to relieve strain on the heart
o Effectiveness is measured based on decreased chest pain
What is acute coronary syndrome (ACS)?
o Ischemia that is prolonged and not immediately reversible
o includes both NSTEMIs and STEMIs
o Interventions: ECG, upright positioning, supplemental oxygen, IV access, nitroglycerin, statins, morphine, bedrest for 12-24 hours
complications of myocardial infarction: cardiogenic shock
o heart suddenly cannot meet body's oxygen demand
o associated with a high death rate
o treated with decrease in oxygen demand
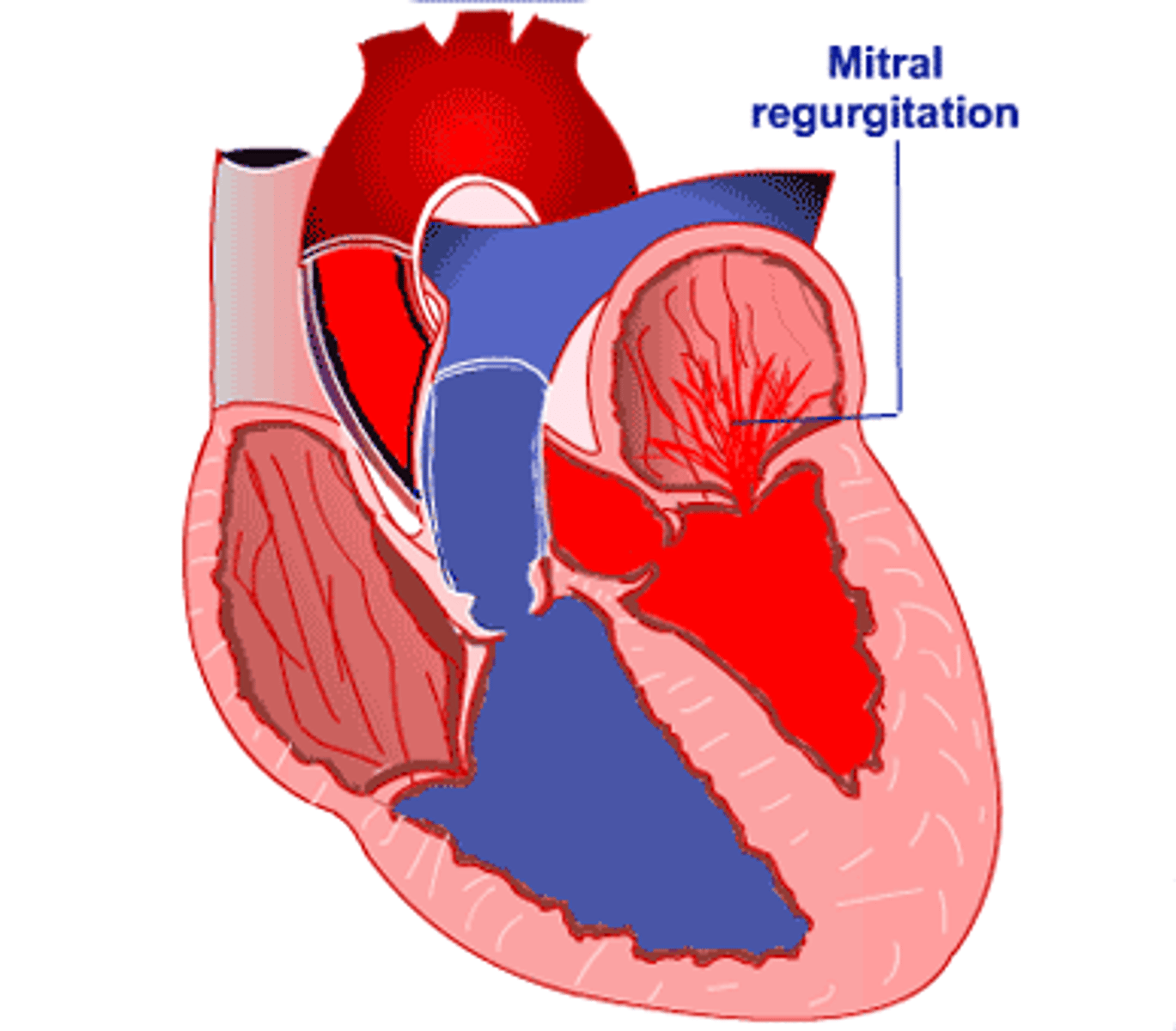
complications of myocardial infarction: papillary muscle dysfunction/rupture
o Causes mitral valve regurgitation
o Needs immediate heart surgery!
complications of myocardial infarction: left ventricular aneurysm
o Myocardial wall thins and bulges out during contraction
o Leads to heart failure, dysrhythmias, angina
complications of myocardial infarction: ventricular septal wall rupture
o s/s: loud systolic murmur, HF, cardiogenic shock
o requires emergency repair
o rare condition + high death rate
complications of myocardial infarction: acute pericarditis
o Inflammation of pericardium
o s/s: chest pain increases w/ inspiration or coughing + relieved by sitting forward
o diagnose with ECG
o treat with high-dose aspirin
complications of myocardial infarction: dressler syndrome
o Autoimmune reaction to necrotic heart muscle leads to pericarditis & fever 1-8 weeks after MI
o s/s: chest pain, MI, fever, malaise, pericardial friction rub, arthralgia
o treat with high-dose aspirin
o avoid NSAIDs & corticosteroids in the first four weeks after an MI
What is the most common complication of an MI?
arrhythmias
What is a STEMI? How is it immediately treated?
o occlusive thrombus creates ST elevation on ECG
o Treatment of choice: PCI
o Give IV thrombolytic within 30 minutes of arrival
What is an NSTEMI? How is it immediately treated?
o non-occlusive thrombus
o typically go to cath lab w/ PCI within 12-72 hrs; no thrombolytic therapy
o dual antiplatelet therapy & heparin
What is fibrinolytic therapy? Why is it used? What are complications/contraindications of the therapy?
o Used as a treatment for STEMI if they cannot go to cath lab
o Examples: tissue-type plasminogen activator
o Qualifications: no history of bleeding, chest pain must be occurring for < 12 hrs (preferably 3-4 hours after onset)
o Contraindications: bleeding, hypotension, kidney damage, LOC change
What is sudden cardiac death? (common causes, prodromal symptoms indication)
o Unexpected death from cardiac cause due to abrupt disruption in cardiac function resulting in loss of cardiac output and cerebral blood flow
o Commonly caused by ventricular dysrhythmias, structural heart disease, conduction disturbances
o If a patient has SCD but no prodromal symptoms, they did not have an MI (most likely due to an arrhythmia)
o If a patient has SCD and has prodromal symptoms, they probably had an MI
o Prodromal symptoms include chest pain, palpitations, dyspnea
o Death usually occurs within 1 hour of symptom onset
What is right HF? What are the symptoms?
o right ventricle pumps ineffectively; fluid backs up into the venous system
o s/s: jugular venous distention, hepatic congestion (hepatomegaly), lower extremity edema, renal failure
What is left HF? What are the symptoms?
o often occurs first; blood backs up into the lungs
o s/s: mild dyspnea, restlessness, agitation, slight tachycardia initially
What is biventricular failure?
Failure of both sides of heart, usually from when L sided has progressed to include R sided (symptoms of both sides will be present)
What are examples of general symptoms of heart failure?
edema, nocturia, cool skin, anxiety, chest pain, dysrhythmias
Systolic vs diastolic HF:
Systolic:
o HF + reduced left ventricle EF
o heart cannot pump blood forward; caused by impaired contractile function
Diastolic:
o HF with preserved EF
o impaired ability of the ventricles to relax and fill during diastole
What is acute decompensated heart failure (ADHF)? (early & late s/s)
o Sudden exacerbation of HF which requires urgent medical care
o Pulmonary & systemic congestion seen
o Early signs: increased RR, decreased PaO2
o Later signs: tachypnea, edema
o Further progression: respiratory acidosis, pulmonary edema
S/S of pulmonary edema:
Anxiety, dyspnea, frothy sputum, abnormal s3+s4
medications for CHF: diuretics, vasodilators, morphine, RAAS inhibitors
o Diuretics - decrease preload (loop diuretics - monitor potassium)
o Vasodilators - reduce circulating blood volume (nitroglycerine, sodium nitroprusside)
o Morphine - reduces preload & afterload, anxiety & dyspnea
o RAAS inhibitors - encourage fluid excretion
medications for CHF: positive inotropes
increase contractility
o β-agonists (dopamine, dobutamine, norepinephrine [Levophed])
o Phosphodiesterase inhibitor (milrinone)
o Digoxin - slows HR; do not give if HR < 60
What would be a primary assessment finding in a patient with CHF?
Sudden weight gain of >3 lb (1.4 kg) in 2 days may indicate ADHF, an exacerbation of chronic HF
Nursing interventions for CHF patient:
o High Fowler's position w/ feet in horizontal position in bed (promotes ventricular emptying)
o Low sodium diet (< 2g/day)
o DASH diet
o Daily weights
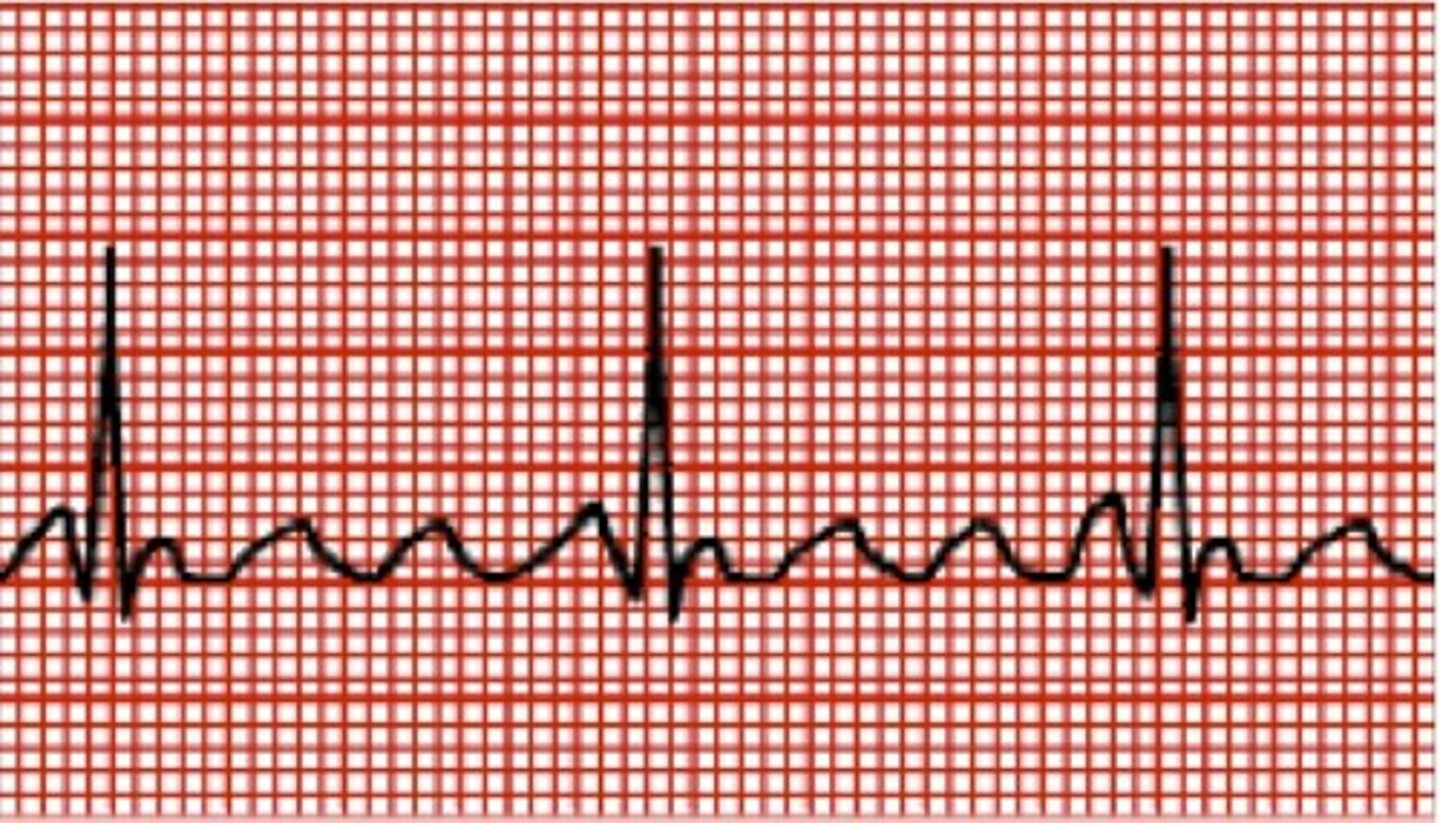
Meaning of the waves on an EKG strip:
o P- atrial depolarization (sinus vit)
o QRS - ventricular depolarization
o PR interval - the amount of time electrical impulse takes to travel from SA node to AV node
o T - ventricular repolarization
o U - repolarization of Purkinje fibers
o QT - start of ventricular depolarization to repolarization

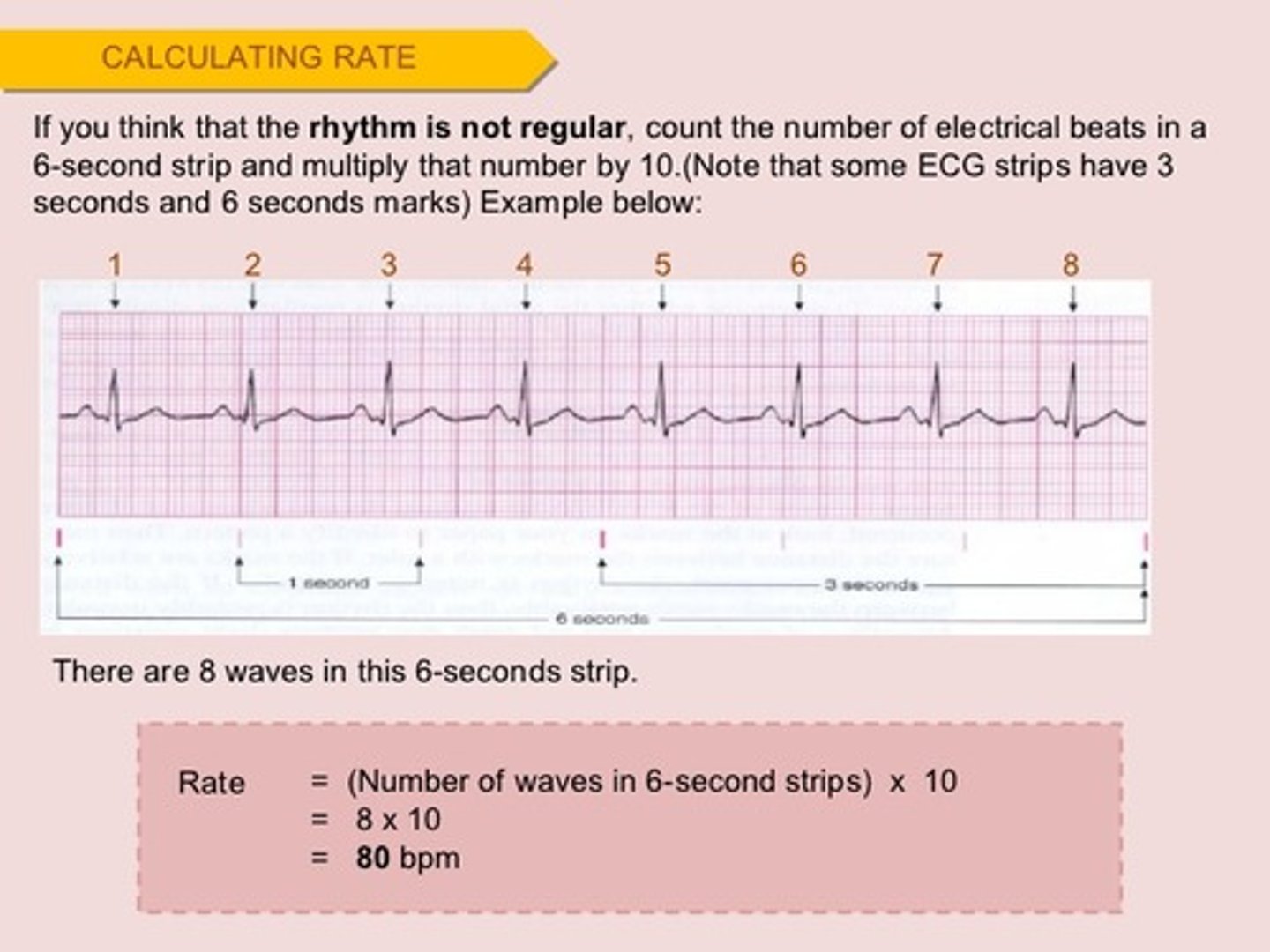
How can you determine heart rate by looking at an EKG strip?
Count number of R waves in a 6-second strip, multiply by 10 - this is the heart rate
What is sinus rhythm?
normal rhythm where each wave and complex have a normal shape and rhythm w/ HR between 60-100BPM

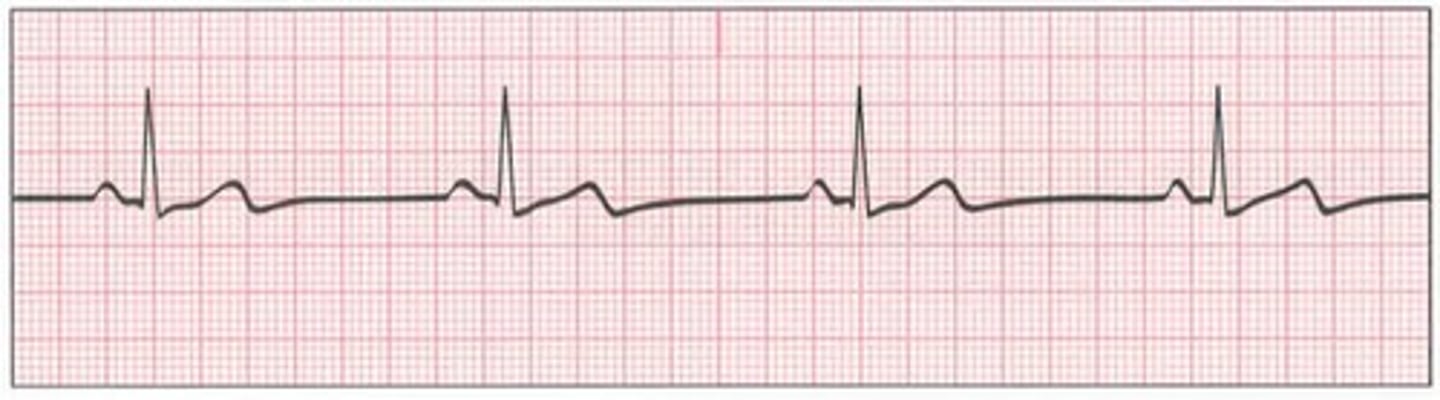
What is sinus bradycardia? (s/s & treatment)
- sinus rhythm where the SA node fires at < 60 BPM
- S/S: hypotension, pale skin, weakness, angina, syncope, confusion, SOB
- Treatment: atropine (increases HR), pacemaker, d/c offending medications
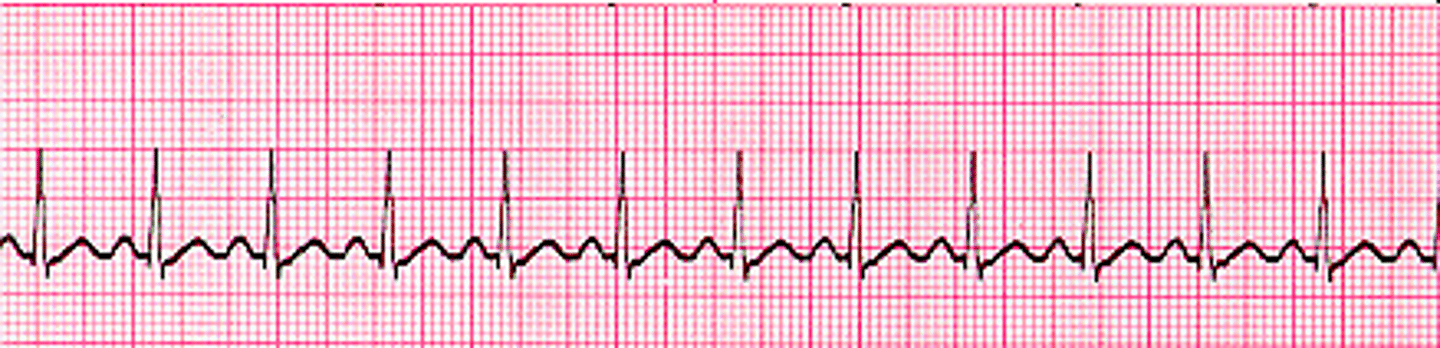
What is sinus tachycardia? (s/s & treatment)
- sinus rhythm where the SA node fires at 101-200BPM
- S/S: dizziness, dyspnea, hypotension (due to decreased CO), angina with CAD (due to lack of ventricular filling during diastole)
- Treatment: treat cause, vagal maneuver, beta blockers
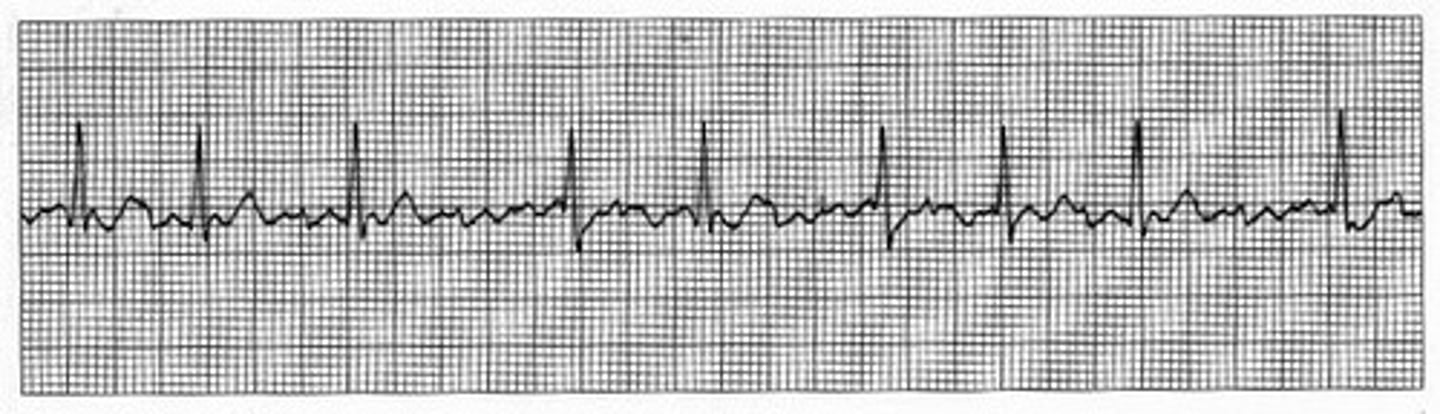
What is premature atrial contraction? (s/s & treatment)
- Irregular heart rhythm caused by an ectopic focus in atrium, distorting the P-wave
- Causes: stress, fatigue, caffeine, tobacco, alcohol, electrolyte issues
- S/S: heart “skips a beat”
- Treatment: withhold stimulants, administer beta blockers
- In patients with previous heart disease who are having PACs it could indicate electrical concerns in the ventricle that precipitates more serious issues!
What is paroxysmal supraventricular tachycardia? (s/s & treatment)
- ectopic focus above the bundle of his causes the ventricles to go too fast (rate of 120-220 BPM)
- Abrupt onset and termination of symptoms
- Associated with overexertion, stress, stimulants, and dig toxicity
- S/S: hypotension, dyspnea, angina
- Treatment: vagal nerve stimulation, adenosine, beta blockers, CCBs, amiodarone, cardioversion

administration of adenosine:
IV push should be administered undiluted and rapidly (over 1 to 2 sec). After administering , flush the line with 0.9% NaCl to prevent precipitation of particulate matter.
What is atrial flutter? (treatment)
- saw-tooth P-wave with a single ectopic focus in the atria and heart rate of 200-350 BPM
- "Flutters" shown indicate how many times the electrical current runs around the atrium before going to the ventricle
- Treatment: antidysrhythmic, cardioversion, radiofrequency ablation (high rates of energy focused at ectopic focus)
What is atrial fibrillation? (s/s & treatment)
- Most common dysrhythmia; usually seen with heart disease
- Atrial fibrillation "w/ RVR" means the ventricle rate is > 100
- Treatment: cardioversion, anticoagulation, radiofrequency ablation
If a patient has experienced Afib for longer than 48 hours, what changes about their care?
require 3-4 weeks of anticoagulation before cardioversion
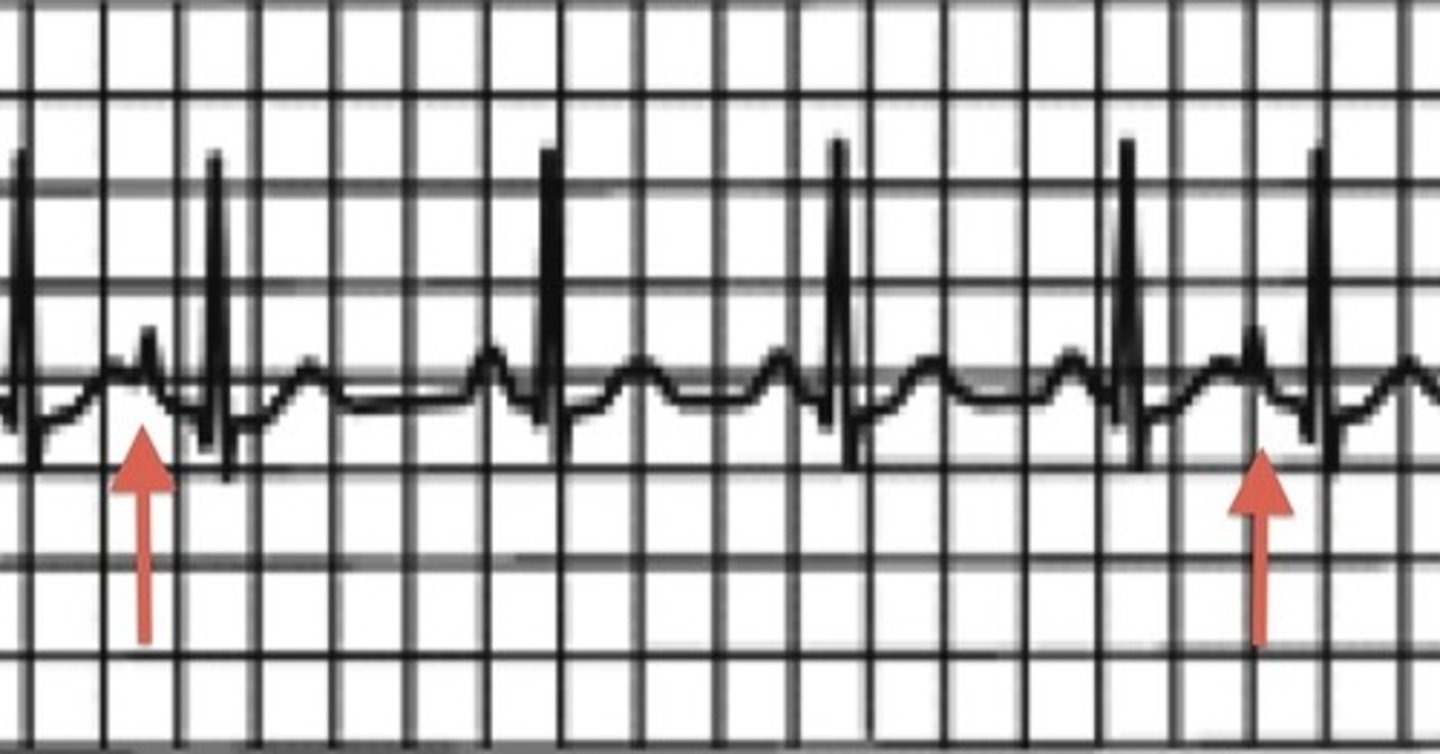
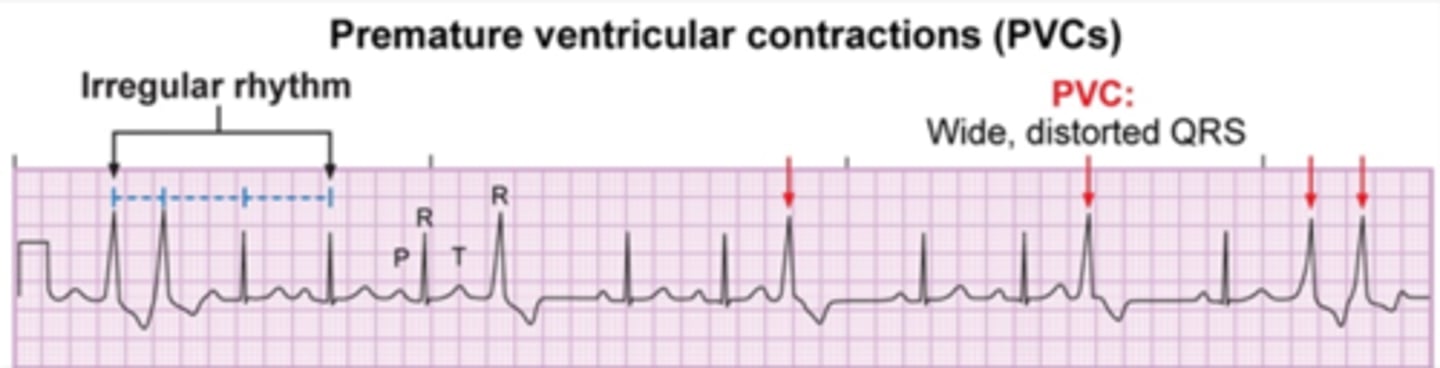
What are premature ventricular contractions? (types & risk)
- ectopic foci in the ventricles cause an early QRS complex, which appears as wide, distorted QRS
- 3+ PVCs = VTACH
- Caused by stimulants, electrolyte imbalances, hypoxia, heart disease
- Only harmful if the patient already has heart disease
- Note: monitor for pulse deficit
- Treatment: correct cause, antidysrhythmic
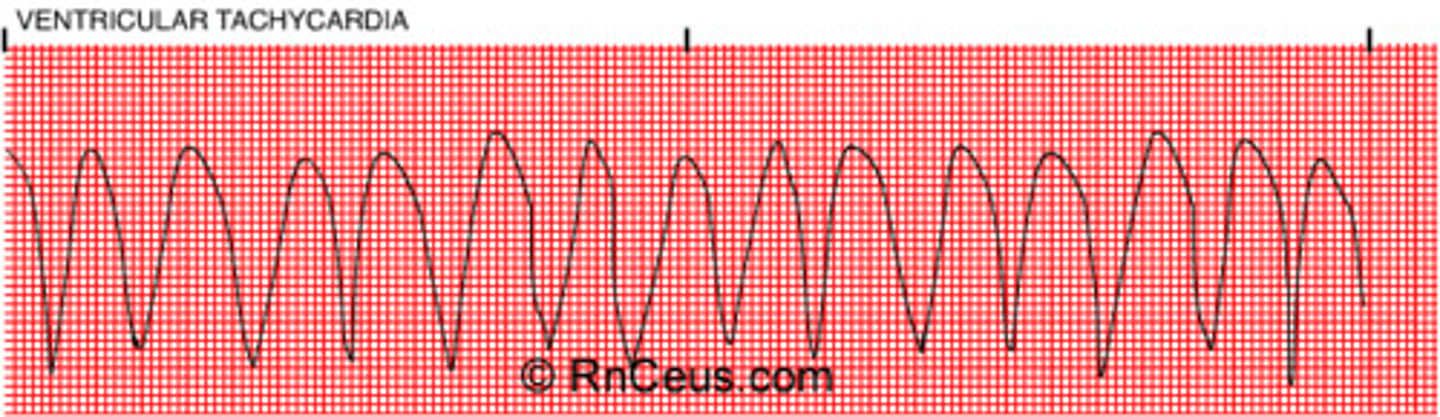
What is ventricular tachycardia? (s/s & treatment)
- ectopic foci take over as the pacemaker of the heart leading to wide, distorted QRS intervals (3+ PVCs in a row)
- Lethal dysrhythmia!
- Can be pulsing or pulseless (stable or unstable)
- S/S: hypotension, pulmonary edema, cardiac arrest
- Treatment: treat underlying cause, stable VT is treated with antidysrhythmic or cardioversion, pulseless VT is treated with CPR and defibrillation
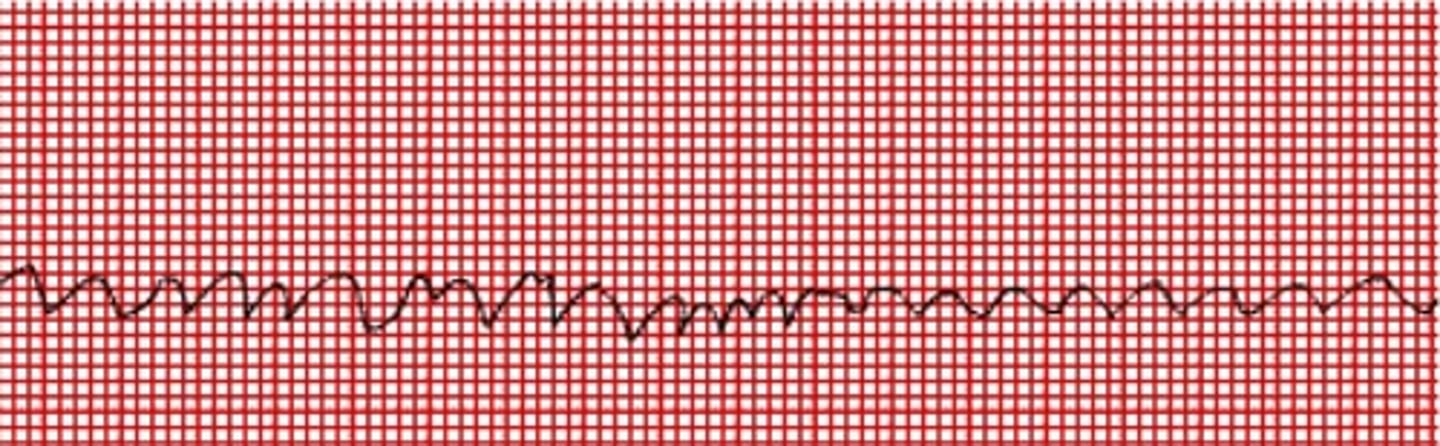
What is ventricular fibrillation? (causes & treatment)
- multiple ectopic foci in the ventricle leading to "quivering" with no effective contraction
- Lethal dysrhythmia!
- Heart rate is not measurable; patient is pulseless and apneic
- Caused by MI, ischemia, procedures
- Treatment: CPR, defibrillation, epinephrine, vasopressin
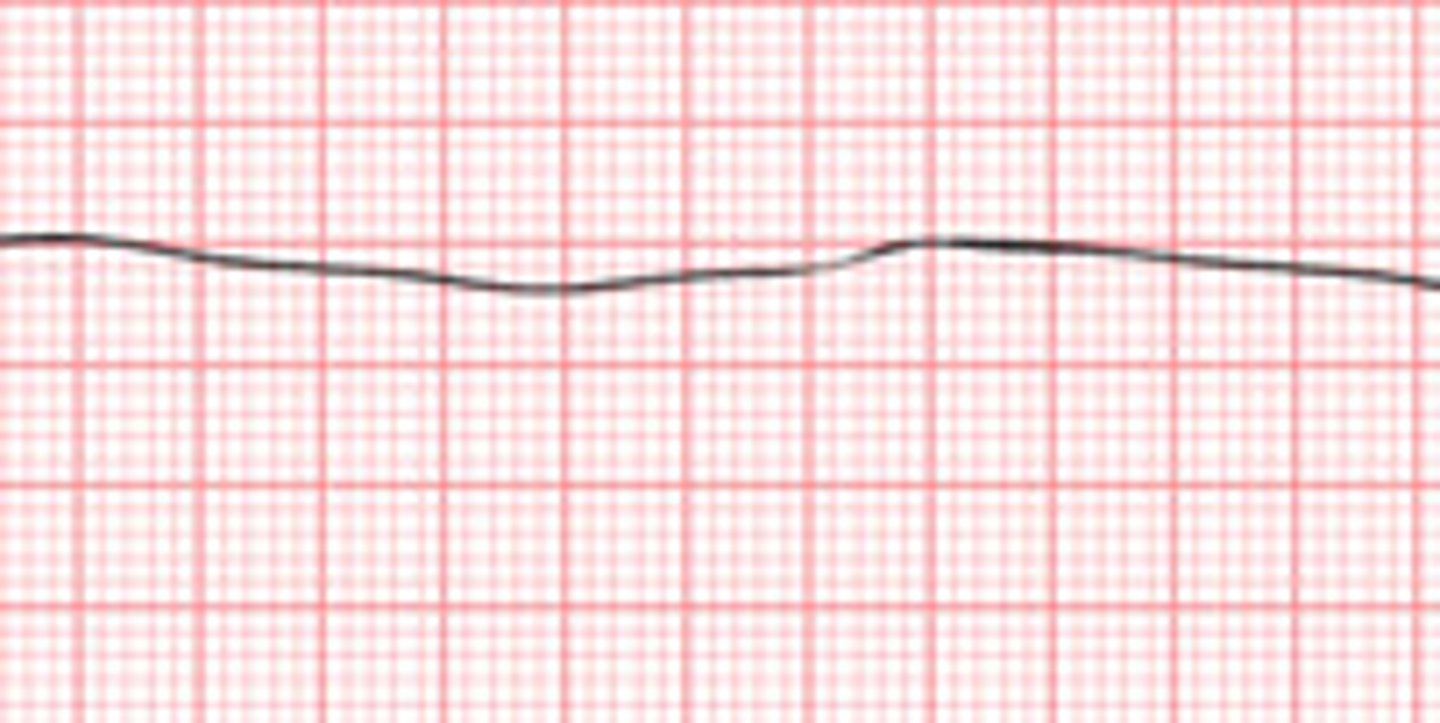
What is asystole and how is it treated?
- total absence of ventricular activity
- Not shockable!
- Must be assessed in more than one lead
- Treatment: CPR, epinephrine, vasopressin, intubation
What is Pulseless Electrical Activity and how is it treated?
- electrical activity observed on EKG but no mechanical cardiac activity is present
- Common causes - H's & T's
- Treatment: CPR, intubation, IV epinephrine
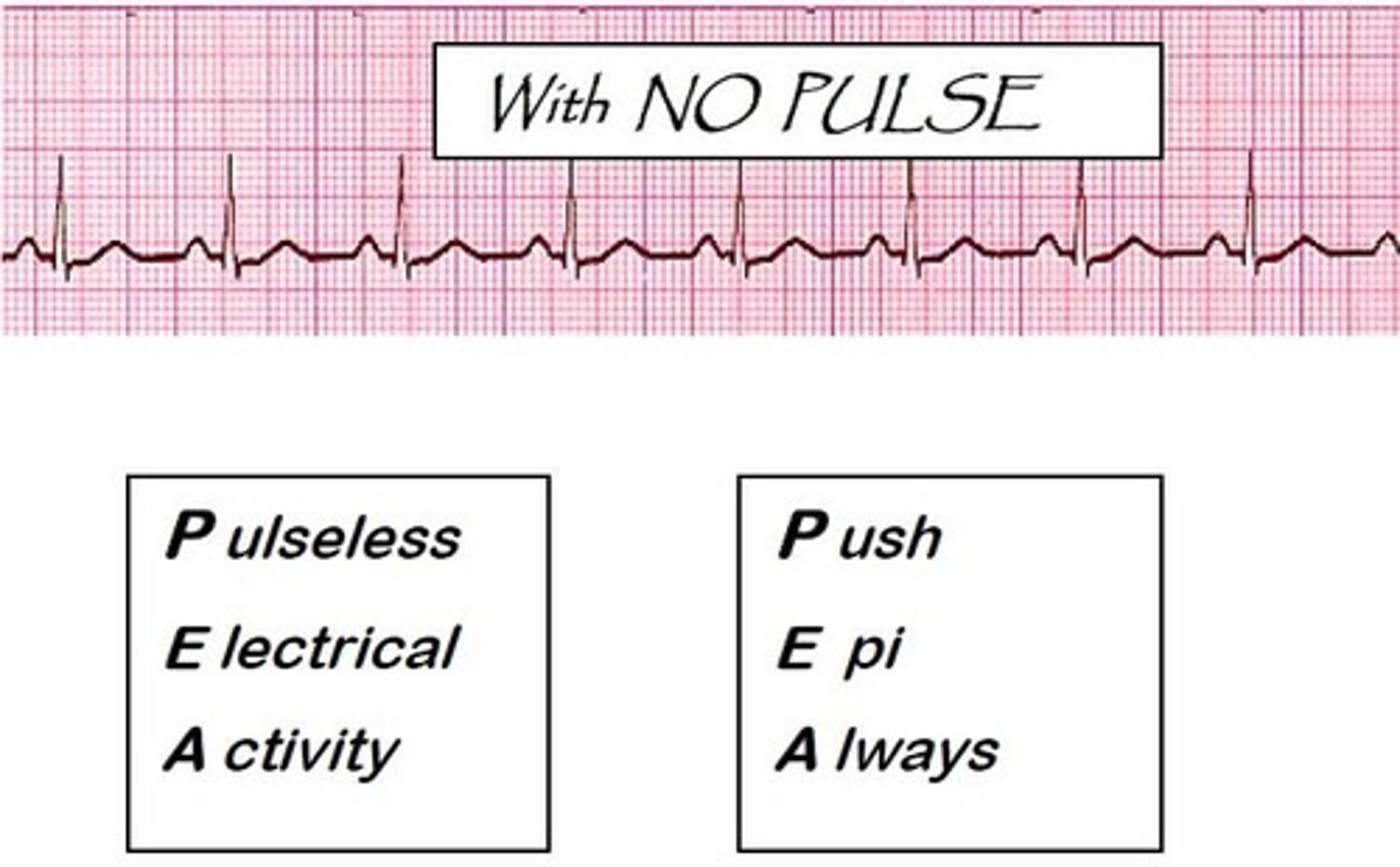
Common causes of PEA - H's & T's:
Hypovolemia, hypoxia, hydrogen ions (acidosis), hyper/hypokalemia, hypoglycemia, hypothermia
Toxins (drug OD), tamponade, thrombosis, tension pneumothorax, trauma
What instructions do you want to give a patient post-permanent pacemaker implantation?
Arm in sling on effected side, cannot raise arm for two weeks
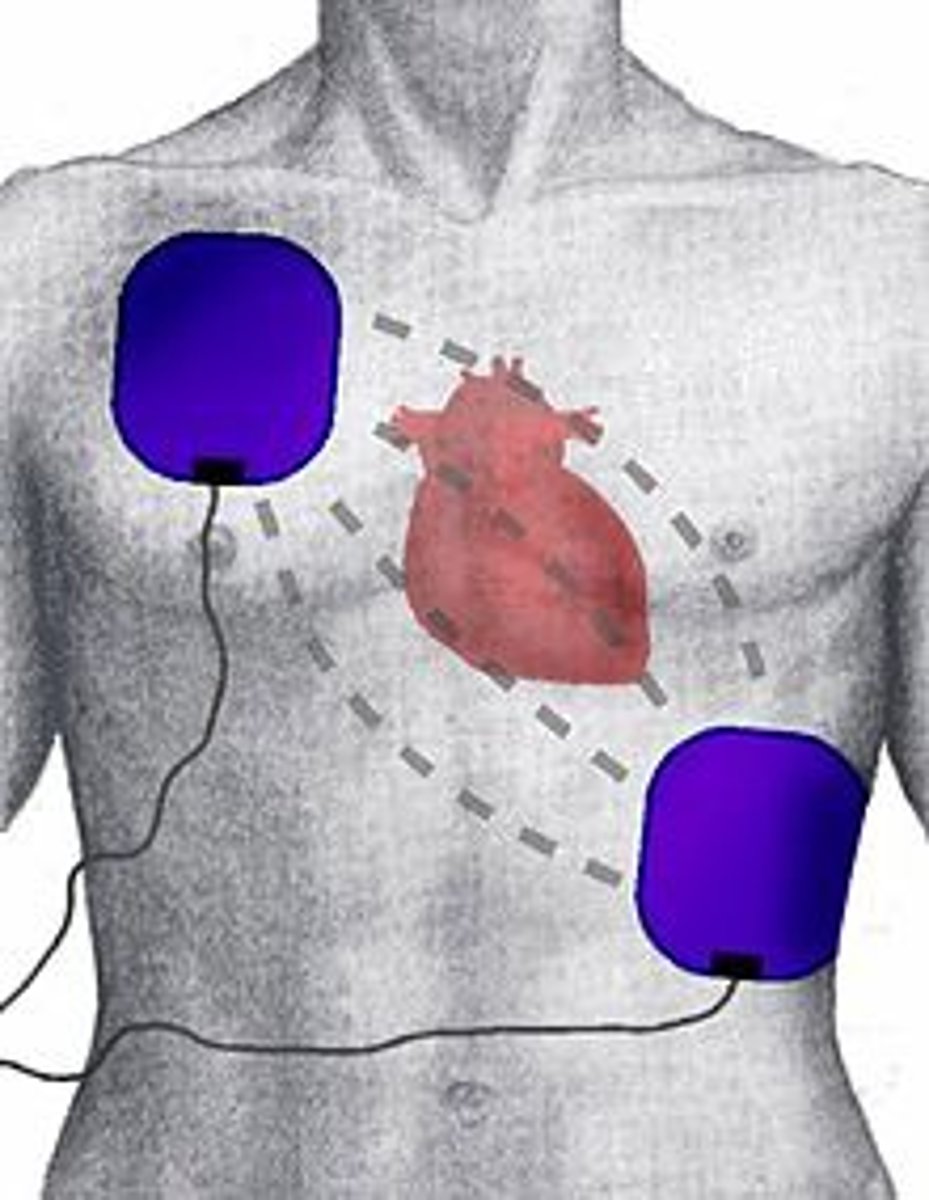
What is defibrillation?
- Allows SA node to resume pacemaker role
- Treatment of choice for ventricular fibrillation and pulseless ventricular tachycardia
- Needs to be performed within 2 minutes of dysrhythmia onset
- Can be monophasic (delivers energy in one direction) or biphasic (delivers energy in two directions) – paddle placement is same
- Recommended energy for initial shocks in defibrillation
· Biphasic: 120 to 200 joules
· Monophasic: 360 joules
- Immediate CPR after shock (within 10 seconds)
What is synchronized cardioversion?
- Synchronized circuit delivers a countershock on the R-wave of the QRS complex of the ECG – SYNC button must be ON!!!
- Treatment of choice for pulsing VT or supraventricular tachydysrhythmias
- Patient is sedated if stable prior to treatment
- Lower initial energies than defibrillation
- If patient were to become pulseless, turn SYNC off and defibrillate
What is infective endocarditis? (causes, risk factors, s/s)
o Caused by bacteria (Staphylococcus, Streptococcus) viruses and fungi
o Valves and endocardium are infected through the blood; parts of vegetation can break off and enter circulation
o Risk Factors: older adults, IV drug users; patients with prosthetic valves, intravascular devices, or on renal dialysis
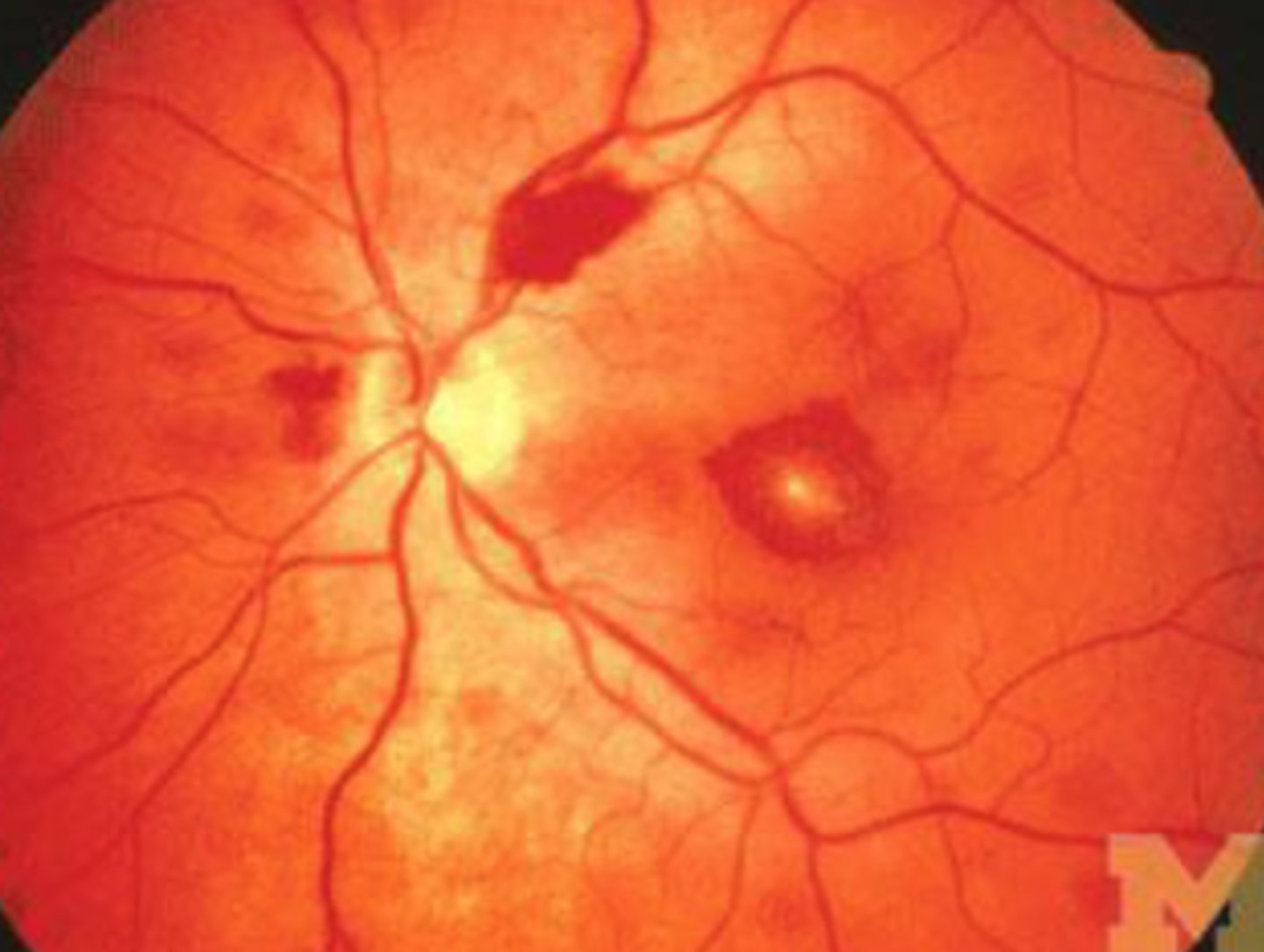
o S/S: fever, chills, weakness, muscle aches, fatigue, anorexia, new or worsening systolic murmur; if embolization into limbs – splinter hemorrhages in nail beds, petechiae, Osler’s nodes, Janeway’s lesions, Roth’s spots
Osler's nodes:
painful nodules on finger and toe pads

Janeway's lesions:
flat, painless, small, red spots that may be found on the palms and soles in patients with infective endocarditis

Roth's spots:
hemorrhagic retinal lesions
Symptoms to monitor for with IE that could indicate embolization to the spleen, kidneys, brain, or lungs:
- Spleen: pain in LUQ, tender rigid abdomen
- Kidneys: flank pain, hematuria, renal failure
- Brain: change in neuro status, visual changes, balance changes
- Lungs: dyspnea, chest pain, hemoptysis
What are the major criteria used to diagnose IE?
at least two of the following: two positive blood cultures 12 hours apart, nonvalvular regurgitation, or intracardiac mass or vegetation noted on echocardiography
Purpose of tests for IE (blood cultures, echo, chest x-ray, ECG, catheterization):
o Ask about recent dental or surgical procedures
o Two blood cultures drawn 1 hour apart from 2 different sites - will show infection & ESR + CRP levels elevated
o Echocardiogram done to detect vegetation
o Chest X-Ray will show cardiomegaly
o ECG will show AV block
o Catheterization used to assess valve function and coronary arteries before surgery
To prevent Infectious Endocarditis, prophylactic antibiotics given to select patients having:
- Certain dental procedures
- Respiratory tract incisions
- Tonsillectomy and adenoidectomy
- Surgical procedures involving infected skin, skin structures, or musculoskeletal tissue
- Patients with prosthetic material in the heart, history of IE, CHD, or heart transplants
Priority actions/parameters to monitor when caring for patients with endocarditis:
o Monitor neuro status for embolization
o IV long-term antibiotics - ensure IV drug users have access to PIV treatments; no central lines!
o Antipyretics, fluids, rest
List order of completion: ECG, blood cultures, IV antibiotic, Tylenol
ECG, blood cultures, IV antibiotic, Tylenol
How to prevent rheumatic fever:
Prevention & treatment of strep with antibiotics, proper IV-related technique
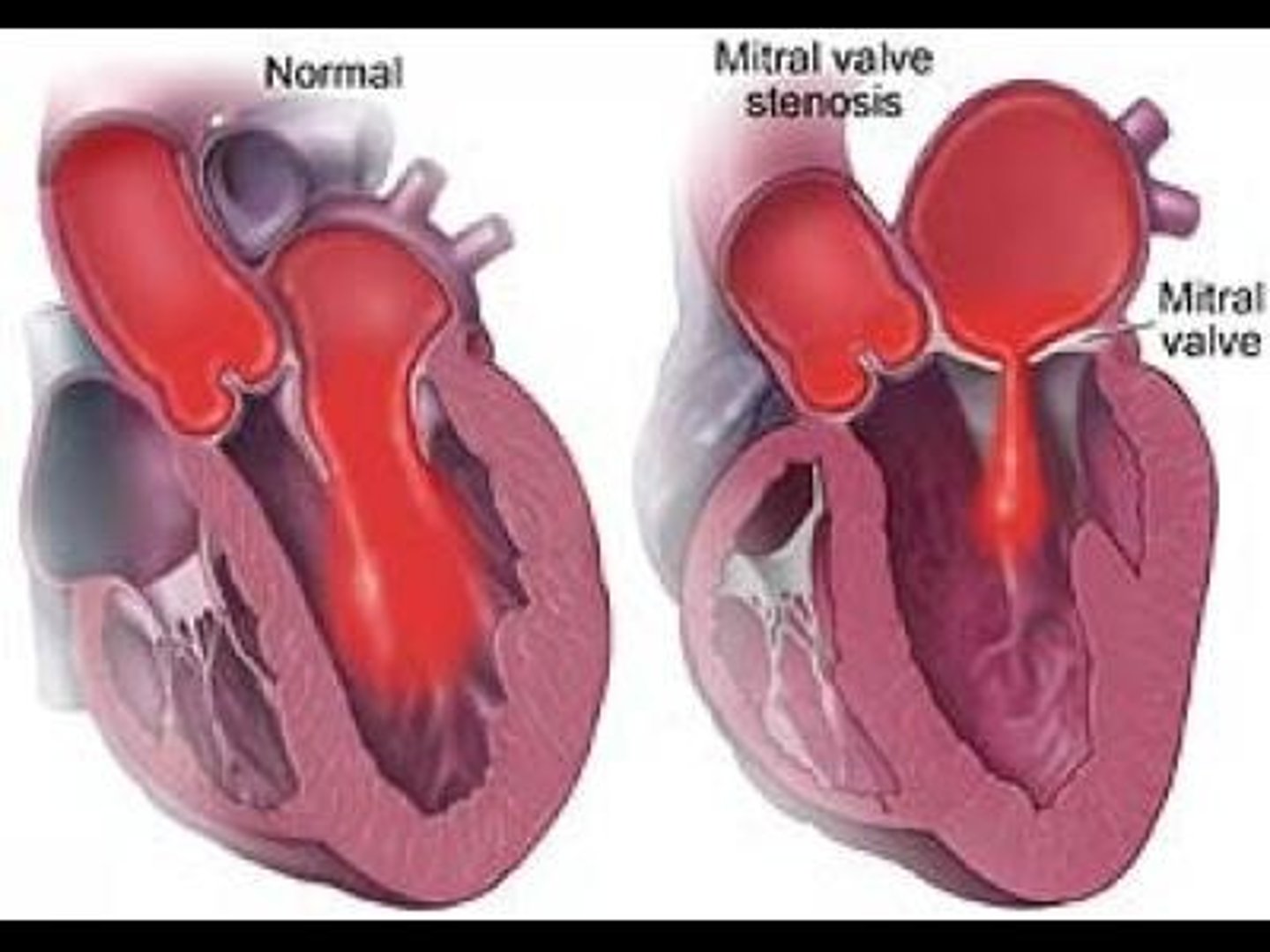
Mitral valve stenosis: (cause, s/s)
- Majority caused by rheumatic fever
- Results in decreased blood flow from left atrium to left ventricle
- Leads to increased left atrial pressure and increased pulmonary pressure; risk for atrial fibrillation
- S/S: exertional dyspnea, loud S1, fatigue, palpitations, hoarseness, hemoptysis, chest pain, stroke
Mitral valve regurgitation: (acute vs chronic)
Acute: causes pulmonary edema -> cardiogenic shock
· S/S: thready peripheral pulses, cool extremities
Chronic: causes hypertrophy -> decreased CO
· S/S: weakness, palpitations, progressive dyspnea, peripheral edema, S3
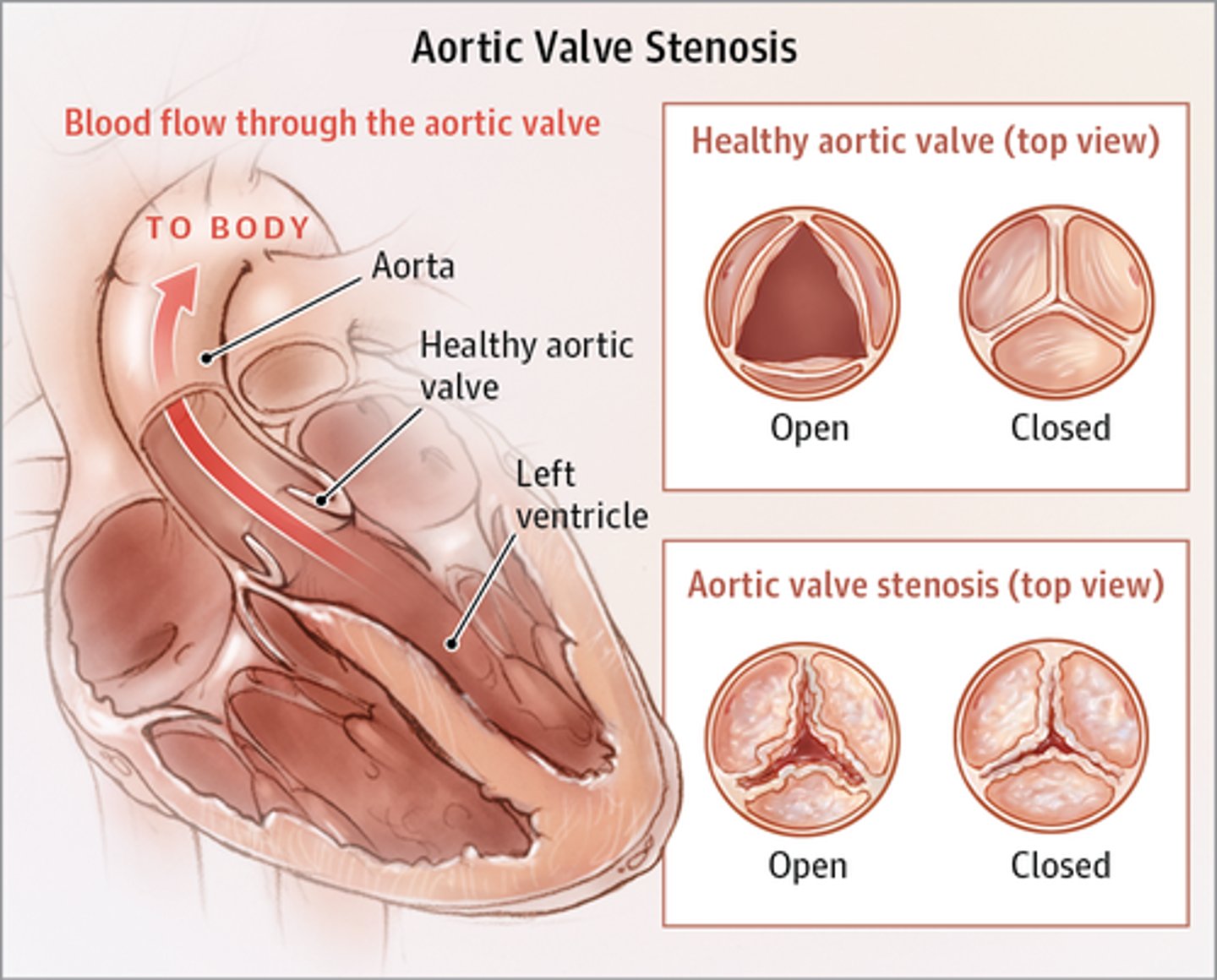
Aortic valve stenosis: (cause, s/s, treatment, caution)
- Often congenital
- Obstruction of blood flow from left ventricle to aorta leads to ventricular hypertrophy, decreased CO, pulmonary hypertension, and HF
- S/S: angina, syncope, dyspnea (symptoms do not present until valve is 1/3 original size), diminished S2, prominent S4
- Require valve replacement
- Use nitro cautiously because it can reduce preload & BP, can worsen chest pain
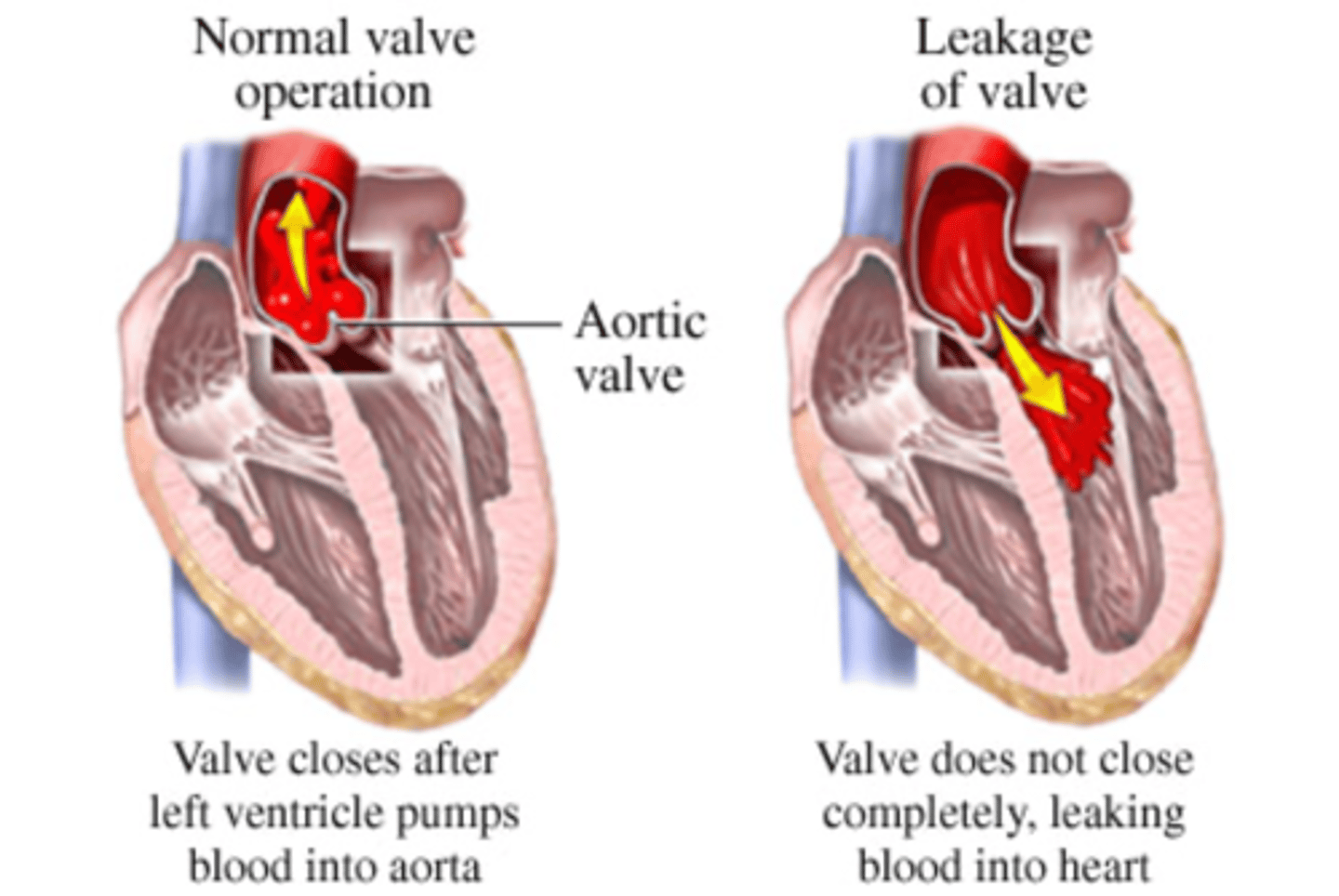
Aortic valve regurgitation: (acute vs chronic)
Acute: caused by infective endocarditis, trauma, or aortic dissection (life threatening!)
· S/S: dyspnea, chest pain, hypotension, cardiogenic shock
Chronic: caused by rheumatic heart disease, syphilis
· S/S: asymptomatic for years, exertional dyspnea, orthopnea, angina, S3, S4, "water-hammer" pulse
Regurgitation from aorta into left ventricle leads to dilation and hypertrophy, decreased contractility, and pulmonary HTN
What are predisposing factors for endocarditis in a patient with a prosthetic valve?
o Occurs due to the foreign nature of the prosthesis
o Patients with mechanical valve replacements require life-long anticoagulation