Palmer- Phys II- Exam II- TQs
1/202
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
203 Terms
What are the smooth muscle visceral motor effectors discussed in lecture (TQ) 5
- Within vasculature
-Within walls of the GI tract
- Sphincters
-Within walls of the bladder
-Withing Eye (iris- dilate/constrict pupil) (ciliary- near/far)
What are the visceral motor effectors of the heart that were discussed in lecture (TQ) 2
-cardiac muscle in walls of ventricles and atria
-AV and SA nodes
What are the glandular visceral motor effectors discussed in lecture (TQ) 4
-Sweat glands
-Salivary Glands
-Pancreas
-Stomach
What are the "miscellaneous" visceral motor effectors discussed in lecture? (TQ) 3
- adipose tissue
- liver
- kidney
The atunomic nervous system pathway is how many neurons?
Where does the first neron synapse?
2 neurons (pre and postganglionic)
synapses on autonomic ganglia
Where is the cell body of the pre-ganglionic neuron in the autonomic nervous system pathway?
what about the post-ganglionic cell body location?
- In CNS
- in PNS (ganglion)
What are the two main ways that sympathetics control local blood flow? 100% TQ
-Flow to capillary beds (via precapillary sphincters)
- Diameter of arterioles (via vasoconstriction/dilation)
The Diameter of arterioles is controlled by the ____________ muscle within _________.
_______________ leads to decreased blood flow. ____________________ leads to increase blood flow
100% TQ
smooth; arterioles
Vasoconstriction; vasodilation
The flow to capillary beds is controlled by ________________ ______________ (smooth muscle).
_________ leads to decreased blood flow and ______________ leads to increased blood flow.
100% TQ
precapillary sphincters
constriction; dilation
What allows sympathetic to control the amount of blood within local capillary circulation (mesenteric circulation)?
Flow to capillary beds via precapillary sphincters
What NT do we see released at sympathetic post-ganglionic neurons? 100% TQ
NE
What NT do we see released at preganglionic sympathetic, preganglionic parasympathetic and post-ganglionic para-sympathetic neurons? 100% TQ
Ach
Preganglionic sympathetic neurons release _______________.
Ach
Which division of the autonomic nervous system supplies more diverse functions across the body? 100% TQ
Sympathetic nervous system
What division of the autonomic nervous system uses adrenergic receptors?
What are the adrenergic receptor types? 100% TQ
Sympathetic NS
Alpha-1
Alpha-2
Beta-1
Beta-2
What division of the autonomic nervous system uses cholinergic receptors?
What are the cholinergic receptors types called?
Parasympathetic NS
muscarinic receptors
____________________ fibers going to sweat glands use the neurotransmitter __________________ and a __________________ receptor.
100% TQ
Sympathetic; Ach; muscarinic
What tissues uses sympathetic cholinergic innervation and what receptor type do they have.
Sweat glands, use Ach and muscarinic receptors
What types of sympathetic adrenergic receptor increases smooth muscle activity? TQ
(cause contraction of smooth muscle)
alpha-1
alpha-1 receptors, when active, promote increase smooth muscle activity in what effector organs?
-vascular smooth muscle
-GI muscles
-Urethral sphincter
-pilomotor (hair stand up)
-radial muscles of iris
What sympathetic adrenergic receptor is present on autonomic nerve terminal and in the GI tract, inhibiting activity of both sympathetic and parasympathetic pathways?
alpha-2
What are the two types of alpha-2 receptors that decrease release of neurotransmitters?
-autoreceptors
-heteroreceptors
____________________ are a subtype of alpha-2 receptors located on sympathetic post-ganglionic neurons that INHIBIT release of NE
autoreceptors
___________________ are a subtype of alpha-2 receptors that are present on parasympathetic post ganglionic neurons and INHIBIT the release of Ach
heteroreceptors
What are the functions of the Beta-1 receptors? (2) TQ
- increase activity of the heart
-increase activity of metabolism (lipolysis and renin secretion_
Which sympathetic adrenergic receptor decreases smooth muscle activity? TQ
Beta-2
In a dangerous situation, where would we want to see smooth muscle relax?
Which adrenergic receptor would we utilize to achieve this?
Airway (bronchioles) to actually increase respiration
Beta-2
Where does the sympathetic nervous system originate? 100% TQ
what is another name for the SNS
lateral gray horn from T1-L2
thoracodorsal NS
Pre-ganglionic fibers in the sympathetic NS are ______________ and post-ganglionic fibers are _________.
short; long
sympathetic ganglia are located where?
near the spinal cord
Which sympathetic ganglia supply vast area from the head to the feet? TQ
paravertebral ( aka sympathetic chain)
Which sympathetic ganglia supply the visceral organs (TQ)
Prevertebral (aka celiac, superior mesenteric, inferior mesenteric)
What unique sympathetic ganglia activates and releases epinephrine (80%) and norepinephrine (20%) into the blood?
adrenal medulla
What is the role of epinephrine in the blood (released by the adrenal medulla)
Activates Beta-2--> mast cells decrease activation of histamine released
T/F: Sympathetic synapse on effector organs is very specific
FALSE; very diffuse (branching varicosity)
What is the sympathetic NS impact on blood pressure?
How does this happen?
100% TQ
-increased BP
-NE released on Alpha-1 receptors causes contraction of smooth muscle walls in vasculature, raising pressure.
How is blood pressure raised using Beta-1 receptors
which sympathetic fibers cause the release of NE on these receptors?
- Beta-1 adrenergic receptors are stimulated, increasing cardiac muscle contractile force and SA, AV nodes increasing rate of depolarization.
Increased blood pumping =increased pressure
In regards to skeletal muscle blood flow being increased, which adrenergic receptor activity is increased and which is decreased?
increased activity= Beta-2
decreased activity= Alpha-1
What is an example discussed in lecture that leads to blood flow modulation of the skin?
which adrenergic receptor would be used to achieve this change in body temperature?
-warm environment (needing to cool body down by decreasing blood flow)
--alpha-2 to constrict vasculature and decrease blood to skin, allowing the skin to cool down
what allows heat to radiate from the body?
increasing blood flow to the skin
Which receptors are stimulated to increase blood glucose (liver) TQ
Beta-2 receptors
How is respiration/air flow improved using adrenergic receptors?
Beta-2 receptors decrease smooth muscle contraction in bronchioles, increasing O2/CO2 exchange
What two adrenergic receptors are used to decrease GI activity?
What effector tissues do they communicate with?
100% TQ
Beta-2 relaxes smooth muscle of GI
Alpha-1 contracts GI sphincters
That receptor causes urine formation to be decreased? What is the effector organ?
TQ
beta-1 receptor of the kidney.
(causes increase of NA resorption, decrease urine formation, and decrease blood flow to kidney)
Sympathetic stimulation of what muscle of the eye improves far vision?
what receptor is used?
100% TQ
Beta-2 receptor RELAXES ciliary muscle, causing flatter lens for far vision.
Decreased refractive power of the eye improves what vision?
distance vision
What is mydriases?
what is miosis?
-pupillary dilation
- pupillary constriction
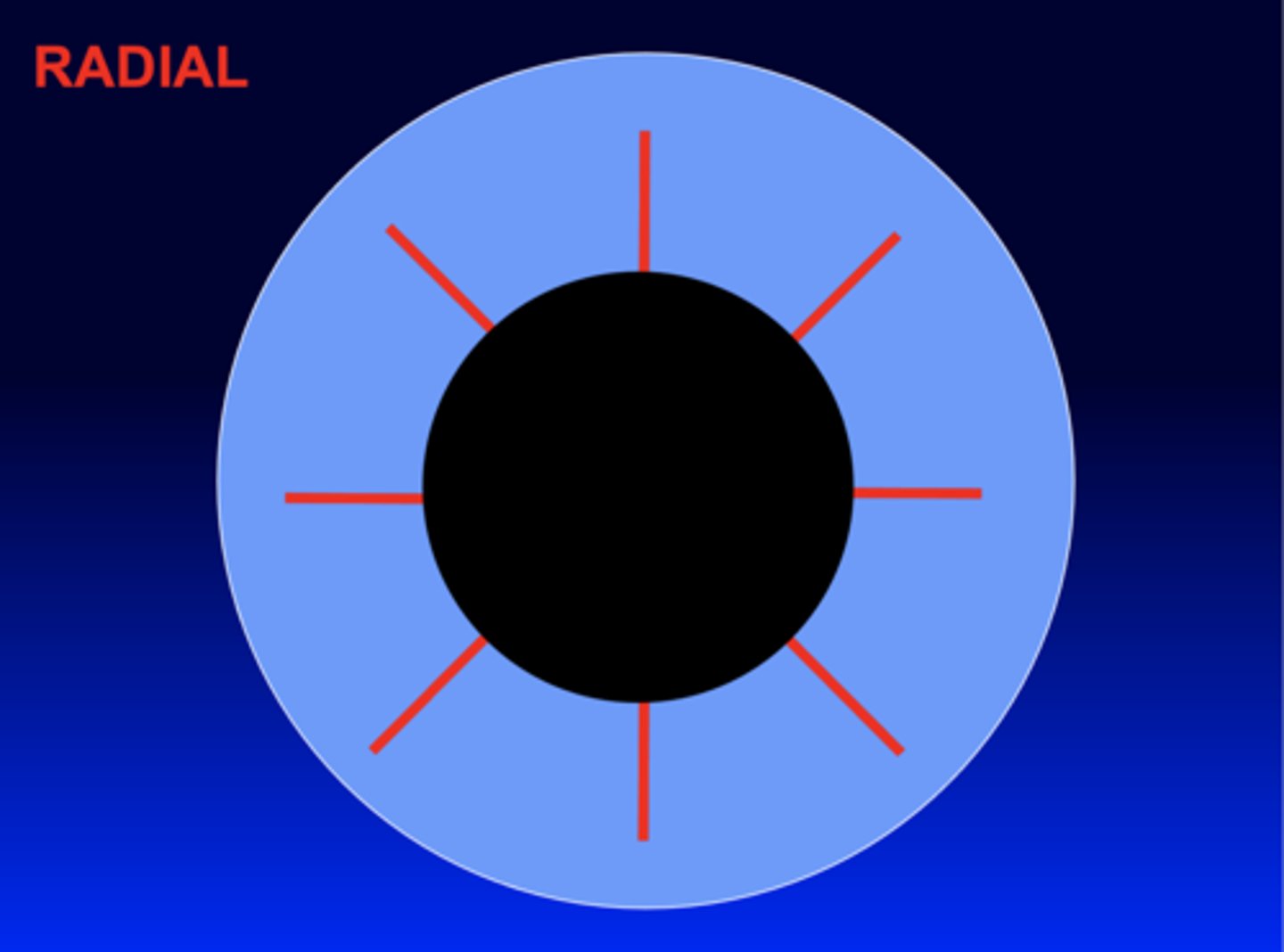
How is pupillary diameter increased with adrenergic receptors of the sympathetic NS? TQ
what muscle does the receptor act on? TQ
DO NOT MIX UP WITH B2
alpha-1 receptors cause constriction of the RADIAL (dilator) muscle of the iris, causing pupillary dilation.
Where does the parasympathetic NS originate from? TQ
what is another name for the Parasympathetic NS?
CN 3, 7, 9, 10 and S2-4
craniosacral NS
preganglionic fibers of the parasympathetic ns are ____________ and post-ganglionic fibers are _________________.
long; short
where do the long post-ganglionic fibers of the parasympathetic NS synapse?
parasympathetic ganglion near or inside effector organ
the parasympathetic NS improves what type of vision?
near vision (accomodation)
How is heart rate managed with the parasympathetic NS? (2 ways)
Ach stimulates muscarinic receptors of the heart, causing decreased AV and SA node rate of depolarization
AND
decreased cardiac muscle contractile force.
How is respiration managed in the parasympathetic NS? TQ
Ach released to muscarinic receptors constricts smooth muscle of bronchioles to deceased respiration.
What does Ach release onto muscarinic receptors of the GI tract cause?
smooth muscle of the GI increase activity and peristalsis
What are the muscles of peristalsis?
circular and longitudinal layers of smooth muscle in the GI
What is delayed or slowed gastric emptying?
what patients commonly are associated with this?
Gastroparesis
diabetes patients (due to potential nerve damage of GI)
What are the dietary recommendation for those suffering from gastroparesis (slowed gastric emptying?
small meals, smoothies, blended food. (fiber may worsen condition)
Muscarinic receptors of GI sphincters are ______________ when Ach is released to them, allowing an ____________________ in digestion.
relaxed; increase
What happens to the salivary glands, pancreas and stomach with Ach release onto muscarinic receptors (parasympathetic stimulation)?
increased rate of digestive enzymes secreted from these organs
What is another term for urination?
micturation
Parasympathetic activation of what muscle and sphincter allow an increase in urination? Are these contracted or relaxed?
- Contraction of Detruser muscle of bladder
-relaxation of internal urethral sphincter
Ultimately, when the parasympathetic activation of the detrusor muscle (causing contraction) and internal urethral sphincter (causing relaxation) occurs, urination is now controlled by what voluntary structure?
external urethral sphincter
Transitioning from visual focus far away to something near you is called?
accomodation
Ach released onto Muscarinic receptors of what muscle cause contraction increased roundness of the lens?
what type of vision does this improve?
ciliary muscle of the eye
near vision
How is pupillary diameter decreased (miosis) ? 100% TQ
parasympathetic (Ach;muscarinic) stimulation of the CIRCULAR muscle of the iris causes contraction, leading to constriction of pupil
What are the two autonomic control centers?
hypothalamus and brain stem
A muscarinic receptor antagonist inhibits the _________ and impairs various ______________________________ functions.
It can either ______________ parasympathetic function or _______________ sympathetic function.
receptor; parasympathetic
decrease; increase
What would you expect the symptoms to be is a patient took a muscarinic receptor antagonist that treats motion sickness?
-dry mouth
-dilation of pupils
-increased HR
-difficulty voiding urine
-decreased sweating
(sympathetic activity increased)
What condition is the progressive degeneration of the central autonomic neurons and ganglia?
what symptoms would you expect to see?
TQ
Shy-drager syndrome
- impotence
-difficulty urinating
-dizziness
-double vision
-indigestion/diarrhea
-heat intolerance
What condition causes a loss of sympathetic tone to 1/2 the face?
What symptoms would you see with this?
TQ
Horner syndome
- drooping eyelid on 1/2 face
- lack of sweating to 1/2 face
-constriction of pupil to 1/2 face
- 1 dry eye
(parasympathetic function increased)
What do you call a tumor of the adrenal gland?
What division of the autonomic NS would be increased in the symptoms?
What would the symptoms be? TQ
-Pheochromocytoma
-increased sympathetic NS
-panic attacks, racing HR, increased BP, throbbing headaches, cold hand/feet, feeling hot, nausea and vomiting.
What are the steps of a reflex signal
1. Receptor
2. Sensory Nerve
3. CNS center
4. Efferent nerve
5. Effector
What reflex contains receptors that are somatic sensory nerve endings found in skin, CT and or joints?
(Protective in nature)
Somatic Reflexes
What reflex contains receptors that are in visceral organs and mediated by autonomic nerves
(homeostatic in nature)
visceral reflexes
What is the autonomic (visceral) reflex receptor for blood pressure?
baroreceptor (mechanoreceptors)
Explain the sensory component of the baroreceptor reflex.
What are the two main baroreceptors and which is most influential?
-Frequency of receptor firing strength is detected. Increase in pressure= increase firing to signal for High BP, to signal to lower BP and vice versa
-Carotid Sinus (Most influential) and Aortic Arch
What is the carotid sinus innervated by?
glossopharyngela nerve
When looking at the baroreceptors of the Carotid sinus, what would you expect their response to be when low blood pressure is recognized?
they would decrease stimulation of firing to signal that blood pressure is low to the nucleus of solitary tract (medulla), thus stimulating for higher pressure.
what is the MOTOR component when there is a drop in blood pressure (as signaled already by the baroreceptors, signal is already at the nucleus of solitary tract in medulla)
long card, BIG TQ
-Efferent signals leave vasomotor center of medulla
-signal travels down spinal cord to synapse of sympathetic pre-ganglionic neurons
-sympathetic fibers travel to blood vessels and synapse on alpha -1 receptors to constrict smooth muscle
-vasoconstriction leads to increased blood pressure
Where is the origin of the signal whe there is a drop in blood pressure?
where is the origin of preganglionic fiber?
Where is the destination of post ganglionic fibers? and what does this cause?
Weird card, MUST KNOW. BIG TQs
- vasomotor (vasoconstrictor) center in medulla
- intermediolateral gray column from T1-L2
-smooth muscle of arterioles, alpha 1 adrenergic receptors cause constriction. increasing BP
What is a condition that has difficulty stabilizing blood pressure with sudden movements (such as sitting down to standing up quickly)?
Orthostatic Hypotension
Referring to the baroreceptor reflex, what are the steps to decrease BP when high blood pressure is detected?
Long car, MUST KNOW, TQs
- Sympathetic efferents will reduce rate of firing
- signal from vasomotor (vasoconstrictor) center in medulla decreases, thus reducing rate of firing.
-results is LESS vasoconstriction
When the vasomotor center increases activity, what is the outcome?
what about decrease in activity?
TQ
- more vasoconstriction (increased BP)
-less vasoconstriction (decreased BP)
What is the vagovagal reflex of the GI?
recommend reading the notes on this concept, little tricky
Receptive relaxation - mechanoreceptors detect distention of stomach --> info relayed to CNS --> CNS sends efferent info by way of vagal nerve to tell smooth muscle of stomach to relax
In regards to the pupillary light reflex, too much light causes ________________ of pupil, stimulating the __________________ pathway
. too little light results in _______________ of pupil, stimulating the ______________ pathway.
TQ
constriction; parasympathetic
dilation; sympathetic
In the sensory component of the pupillary light reflex, where do retinal ganglia cells (optic nerve) return light signals to?
pretectal region of the midbrain
A bright light is hitting your patients eyes. We know that the __________ fiber from the _______________ region of the midbrain is communicating with the ______________-_____________ nucleus, which is the origin of the parasympathetic fibers of the oculomotor nerve. This allows pupillary constriction via the muscarinic receptors.
long card...i know. TQ tho
efferent; pretectal; edinger-westphal (CN3)
Low light is detected in your patient's eyes. We know that the ________________ fiber from the ______________ region of the midbrain communicates with the ___________________ preganglionic fibers in the ______________ thoracics. This fibers synapse on the cervical ganglion and cause post-ganglionic fibers to cause pupillary _____________ due to _______-___ receptors on the radial (dilator) muscle.
I know, long card. TQ
efferent; pretectal; sympathetic; upper; dilation; alpha - 1
What has conscious (voluntary) control of fine, detailed movement (especially in the hands/fingers and facial muscles)
primary motor cortex
learned patterns of movements are controlled by _______________ _____________
basal nuclei
involuntary maintenance of posture and muscle tone is controlled by _________________ tracts and ___________ ____________.
extrapyramidal; muscle spindles
involuntary reflexes are coordinated by the __________ _______.
spinal cord (they don't need to reach the higher brain centers)
Coordinated actions that are reliant in sensory/motor integration are controlled by the ___________________
cerebellum
What is the origin of the corticospinal (pyramidal) tracts?
primary motor cortex
What neurons run from the primary motor cortex to the anterior gray area of the spinal cord to synapse on the lower motor neurons?
upper motor neurons (aka coticospinal-pyramidal tracts)
What is the clinical name for the corticospinal (pryamidal) tracts? 100% TQ
Upper-motor neurons
What is the origin of the extrapyramidal tracts?
Brain stem nuclei
(red nucleus, pontin-reticular nuclei, vestibular nuclei, medullary reticular nuclei)
T/F: extrapyramidal tracts consist of lower motor neurons in charge of involuntary movement.
FALSE: they are still UPPER motor neurons, but they do in-fact carry involuntary movement (posture, reflexes)
The precentral gyrus of the frontal lobe contains ... TQ
(BA- 4)
Primary motor cortex