psych unit 4 aos 1 - sleep
1/70
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
71 Terms
sleep def
naturally and regularly occurring state of consciousness that cyclical
sleep notes
follows internally regulated cycle
inds in behavioural state of perceptual disengagement (less awareness sounds, smells etc) + unresponsive to envo
psychological construct
psychological construct def
cannot be objectively measured thru data collection but widely understood to exist
consciousness
continuum of total to no awareness
sleep near no awareness end
diff between normal waking consciousness (NWC) and altered states of consciousness (ASC) on the continuum
brain wave patterns: NWC = high freq + low amp, ASC = lower freq + higher amp
awareness levels: NWC = high, ASC = sig reduced
perceptual abilities: NWC = all senses used to gather info and respond to stimuli, ASC = limited/absenttime orientation: NWC = continuous and linear, ASC = distorted
brain waves amplitude
indicates intensity of brain waves → how many neurons firing tgt same time
higher peaks + lower troughs = more synchronised brain activity e.g. during sleep
lower peaks + higher troughs = neurons less synchronised doing diff tasks e.g. while driving
techniques to measure physiological responses during sleep
EEG, EMG, EOG (objective)
video monitoring (subjective)
sleep diaries (subjective)
objective measurements of physiological responses during sleep
most reliable measure for bod changes during various consciousness states
EEG, EMG, EOG
DARE = detects, amplifies, records electrical…
electroencephalograph (EEG)
DARE activity of brain displayed as brain wave patterns
brain wave patterns vary in freq and amp
frequency and amplitude
frequency = no. brain waves per sec (speed)
amplitude = brain waves intensity as size of peaks + troughs (height)
brain wave types
beta waves = NWC, when alert, intense mental activity, high freq low amp
alpha waves = we relaxed, mid-high freq (slower than beta) mid-low amp
theta waves = light sleep/deep meditation, mid freq mid amp
delta waves = deep sleep/unconscious, low frew high amp
— as move into deeper NREM sleep → brain waves decrease in freq and increase in amp → when move into REM → brain waves increase freq and decrease amp
electromyograph (EMG)
DARE activity of muscles
electrodes attach to muscles → show movement, activity, tone, tension
light sleep = muscles spasm → EMG high activity
deep sleep = muscles relax → EMG low activity
electro-ocular graph (EOG)
DARE activity of muscles that control eye movement
doesn’t measure eye movement !! measures movement muscles around eye
useful for distinguishing REM and non-REM sleep
REM sleep = EOG rec high activity
NREM sleep = EOG rec low activity
objective measurements of physiological responses during sleep — advantages and limitations
+VES
non-invasive
inexpensive and safe
objective data
-VES
time consuming
cannot establish activity in specific brain area
subjective data of sleep — sleep diaries
self-reported log of ind daily sleep routine over time (usually weeks)
can record:
— qualitative data (e.g. describe dreams)
— quantitative data (e.g. 1-10 scale how refreshed after waking)
→ diary analysed by researcher → can be used alongside physiological methods → provide insight into person sleep issues
subjective data of sleep — sleep diaries advantages and disadvantages
+VES
ind’s thoughts and feelings considered
time-effective (?)
-VES
results v subjective → hard to compare diff ppl
results depend on ind reliability → needs conscious awareness and ability to describe using words
subjective data of sleep — video monitoring
used in sleep labs to study sleep (esp sleep disturbances + disorders)
vid cams record externally observable physiological responses e.g.
— body position
— breathing
— movements like tossing, sleep walking
subjective data of sleep — video monitoring +ves and -ves
+VES =
results can be used tgt with objective physiological measurements (can match real time in vids and observed physiological responses then to the electrical activity recorded by the machines? → more holistic understanding of ind sleep at specific time)
observe behaviour real time
-VES =
results can be subjective (diff ppl diff interpretations)
reviewing vids time consuming
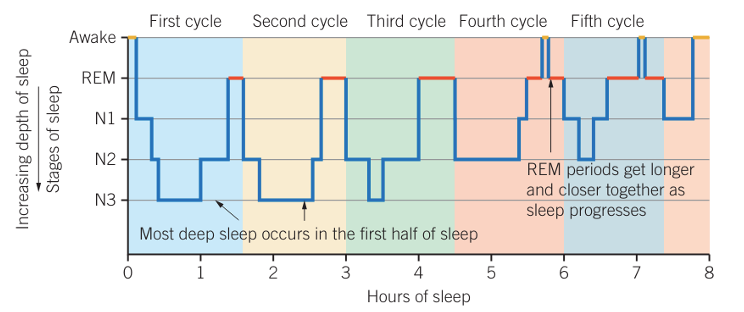
hypnograms
data of person’s sleep pattern
from left to right → stages of sleep being experienced over time
y axis = sleep stages (with decreasing depth as goes higher)
consider sleep cycles, amount hours in stages, ttl hours sleep, time person falls asleep/wakes, how many times awake
each sleep cycle = U-shape
person sleeps → N1 → N2 → N3 → back up stages → REM → repeats for 2nd cycle → third cycle onwards little time spent in N3 and more in REM → short awakenings may occur between cycles
typical adult = 4-5 sleep cycles
2 sleep types during rest
REM = rapid eye movement sleep
non-REM = non-rapid eye movement sleep
1 cycle of sleep…
period of NREM sleep followed by REM sleep (usually 90 mins)
after 1 cycle usually briefly wake
REM vs NREM sleep
duration: REM = 25% ttl sleep, NREM = 75% ttl sleep
brain activity: REM = very active, NREM = less active
muscle activity: REM = muscles paralysed, NREM = muscles active
eye movement: REM = present, NREM = not present
NREM sleep notes
around 75% ttl sleep
more in first half of night
when body recuperates
3 stages
NREM stage 1
light sleep = lose awareness envo
hypnic jerk (as muscles relax we may exp spasms)
easily woken, feel as though never slept
NREM stage 2
regular breathing, less movement
still light sleep but more diff to wake up than stage 1
NREM stage 3
deep sleep
slow + steady breathing
muscles fully relaxed + minimal movement
less responsive envo
if woken = ind groggy + disoriented
REM sleep
rapid eyeball movement behind eyelids
allskeletal muscles(except for breathing)paralysedparadoxical sleep = brain v active while body paralysed
imp for brain recovery and memory consolidation
most dreaming here
body paralysed so we don’t act from dreams, if woken can recall dream
how sleep cycle changes during night
early in night → more time in NREM stage 3 → as night progresses → more time in REM instead
circadian rhythm
bod changes occur as part of cycle within duration 24 hrs (to make us feel sleepy/awake certain times)
sleep-wake cycle
envo cues
ultradian rhythm
bod changes that occur as part of cycle within duration less than 24 hrs
heartbeat
respiration
hunger
sleep (90 min sleep cycle = one ultradian cycle)
suprachiasmatic nucleus in hypothalamus
coordinates circadian phase (rhythm?) by regulating melatonin release in response to light
retina detect light → transfer to SCN in hypothalamus → SCN send inhibitory (if high light) or excitatory (low light) messages to pineal gland → signal to stop (high light) or release (low light) melatonin dependent on amount light on retina
low light = melatonin released
melatonin def
neurohormone prod in pineal gland that initiates sleepiness when its levels increase every evening
melatonin levels
high melatonin levels = feel drowsy/tired
low melatonin levels = feel awake/alert
— in bloodstream
— note: melatonin levels in blood monitored by SCN via negative feedback loop
what is main envo cue to influence sleep-wake cycle
light
other influences on SCN activity
temperature: internal cue signals when to wake up and sleep (morning = SCN signals bod to wake = body temp rise = inds become alert, evening = SCN signals body sleep = body temp lowers = inds become sleepy, relaxed)
eating and drinking patterns: SCN regulates hormone release for appetite and metabolism → when we feel hungry and when digestive sys most active (morning = SCN promotes wakefulness = ppl have regular meal times and peak metabolism, evening = SCN signals body sleep = appetite and digestion decrease)
sleep change over lifespan
as we age → amount sleep time decreases → amount REM decrease rapidly from infancy to childhood then remains stable through adulthood
LIFESPAN SLEEP CHANGES — NEWBORNS
rec sleep hrs = 14-17
REM:NREM = 50:50
— sleep onset anytime
— circadian rhythm not yet developed (no regular sleep-wake pattern)
— irregular sleep duration
— 50% sleep time in REM for active sleep for rapid brain development
LIFESPAN SLEEP CHANGES — CHILDREN
rec sleep hrs = 9-11
REM:NREM = 20:80/25:75?
— amount REM has decreased from infancy
— NREM increases esp NREM 3 as bodies growing → growth hormone release in NREM sleep
— sleepwalking, bed wetting prone
— social factors like school reduce ability to nap during day
— early bedtime, wake up early
LIFESPAN SLEEP CHANGES — ADOLESCENTS
rec sleep hrs = 8-10
REM:NREM = 20:80/25:75
— sleep onset delayed in evening (bc biological shift from puberty → delay melatonin release)
— prone to partial sleep deprivation (staying up late, cannot sleep in as must wake up for school)
LIFESPAN SLEEP CHANGES — ADULTS
rec sleep hrs = 7-9
REM:NREM = 20:80/25:75
— sleep amount decreases further from adolescence → can be according to ind
— feel tired earlier in evening and awaken earlier than adolescents
— REM:NREM proportion and sleep duration remain relatively stable during this stage
LIFESPAN SLEEP CHANGES — ELDERLY
rec sleep hrs = 7-8
REM:NREM = 20:80/25:75
— sig decrease NREM 3 → eventually disappears fully as body needs less recovery
— sleep becomes more fragmented → awake more during night + napping during day
explanations for sleep diffs across lifespan
BIOLOGICAL FACTORS: changes in brain development + maturation of sleep regulatory systems → can influence sleep patterns
HORMONAL CHANGES: shifting hormone levels like melatonin → can influence sleep patterns
ENVO AND LIFESTYLE FACTORS: social demands, work schedules, stressors, lifestyle choices → can influence sleep patterns
changes for sleep across lifespan: exam advice → age and sleep duration
listed sleep hrs for each age group varies among diff sources → not one correct answer to hrs each group sleeps oc of variation within age grps → hence understand trends of how sleep duration changes between age grps rather than exact number of sleep hrs
sleep deprivation def
altered state of consciousness caused by inadequate quantity/quality of sleep
sleep quantity and quality
quantity = sleep amount
quality = how well we feel we’ve slept
— high quality sleep = makes us feel refreshed and energised
— low quality sleep = makes us feel lethargic and drowsy
partial sleep deprivation def
having some sleep in 24 hr period but less than what normally needed (quantity or quality)
partial vs total sleep deprivation
partial = some sleep but less than what needed
total = no sleep at all over 24 hr period or longer
partial sleep deprivation effects on…
ABC
affective functioning
behavioural functioning
cognitive functioning
partial sleep deprivation effects — affective functioning
involved with emotions
amplified emotional responses (intense or exaggerated compared to how we’d normally react)
easily irritated, short-tempered, moody, easily upset
can be hard to control emotions
partial sleep deprivation effects — behavioural functioning
involved with actions — generally observable
slower physical reaction times
unintended lapses into microsleep (v brief sleep period, 1-10 secs)
reduced motor control
more likely risky behaviours
partial sleep deprivation effects — cognitive functioning
involved with mental processes
difficulty concentrating (directing + maintaining attention)
more difficulty problem solving
memory impairment
irrational thoughts
difficulty doing simple repetitive tasks
dawson and reid’s research shows that…
sig relationship between fatigue from mild level sleep deprivation and legal levels of alcohol consumption on impaired performance
sleep deprivation vs BAC
17 hrs sleep deprivation = BAC 0.05
24 hrs sleep deprivation = BAC 0.10 — double the legal limit
comparative analysis sleep deprivation vs BAC
both -vely affect functioning
— e.g. affective functioning: both can impair emotional control, more easily irritated
— e.g. cognitive functioning: both can impair attention, decision making, concentration
what can cause diffs between inds for sleep deprivation on functioning
ind tolerance variations
severity sleep deprivation
severity alcohol consumption
— can all influence intensity of effects
circadian rhythm disorder
type sleep disorder where persistent pattern sleep disruption bc sig, consistent misalignment between circadian rhythm and sleep-wake schedule needed by ind
misalignment occurs → ind body cannot adjust → cause dysfunction → circadian rhythm disorder
misalignment causes: excessive sleepiness, insomnia, impairment person functioning
can cause ind unable sleep and wake appropriate times
— advanced, delayed, shift work
circadian rhythm disorder — delayed sleep phase syndrome (DSPS)
misalignment in timing sleep onset (delay) and awakening (compared to desired timing)
delay usually 2 or more hours
person fall asleep later than needed → wake up later
who’s at risk = adolescents (puberty → body biological clock naturally delays → teens higher risk DSPS), genetic factors, light sensitivity
circadian rhythm disorder — advanced sleep phase disorder (ASPD)
advance in timing sleep onset and awakening (compared to desired timing)
usually 2 or more hours earlier
fall asleep earlier than needed → wake up earlier
who’s at risk = older adults, ppl with autism spectrum disorder, genetic factors
circadian rhythm disorder — shift work
when ppl work shifts outside 9-5 business hours → can disrupt natural circadian rhythm (esp rotational night shifts → ind body continually adapting to diff sleeping times)
circadian rhythm cued by light → hence if need to work at night and sleep during day → then need to sleep when bright outside (lots light) and need to stay awake when dark at night → cause mismatch when they need to sleep/stay awake and tiredness levels
can experience poor sleep quality and quantity (e.g. bc light or noise during day when they try to sleep) → hence feel tired when awake → can negatively impact ability to work
treatment of circadian phase disorders
if ind adjust life commitments around their circadian rhythm → can exp less -ve impacts
bright light therapy
circadian phase disorders treatment — bright light therapy
timed exposure of eyes to bright amounts light
person exposed to special high-intensity light for set time → bright light reduce body production melatonin → make person more awake than normally would
BLT used at time when ind needs to feel more awake/alert
bright light therapy exposure timings for diff circadian rhythm disorders
DSPD = early morning when getting up
ASPS = early evening
shift work = evening before night shift
circadian rhythm sleep disorders and SCN
DSPD = SCN out of sync with external day-night cycle
ASPD =SCN out of sync with external light-dark cycle
shift work = SCN trouble adjusting to irregular sleep-wake patterns from ind’s schedule
circadian rhythm sleep disorders and eating/drinking patterns + body temp rhythm
irregular meal timing = bc SCN influences when ppl feel hungry and when dig system most active → hence when misalignment between external cues and internal clock → irregular meal times
temp rhythm misalignments = SCN may not signal appropriate temp changes for the sleep-wake cycle → hence hard to sleep when body temp not in optimal phase for sleep
sleep hygiene
sleep-related behaviours and envo conds that beneficial for sleep→ bedtime routine changes can improve sleep quality
zeitgebers def
envo cues that can synchronise and regulate bod circadian rhythm
— e.g. light, temp, eating patterns
— can shift ind 24 hr sleep-wake cycle → hence ind can use to improve their sleep-wake cycle → improve their mental wellbeing
zeitgeber — light
daylight is primary zeitgeber for human circadian rhythm — includes all direct and indirect sunlight during daytime
has greatest influence on on sleep-wake cycle bc detected by SCN → directly influence melatonin release by pg
all light wavelengths can shift sleep-wake cycle
blue light (prod from man-made artificial sources of light) powerful inhibition melatonin release
zeitgeber — temp
the degree of external heat in envo that can influence quality + quantity sleep
cool room temp → linked with improved quality + quantity sleep (bc body temp drops during sleep hence cooler room = body temp cool?)
18 degrees ideal
zeitgeber — eating and drinking habits
types + quantity food and drink ind consumes can influence quality + quantity sleep
circadian rhythm preps bod to be more efficient metabolising food during day when we active
long-term severe food deprivation, calorie restriction, perceived starvation → all affects SCN
alcohol, caffeine, high-sugar foods can -vely impact sleep
eating and drinking — de-synchronisation of circadian rhythm
when regularly eat and drink throughout night → can de-synchronise circadian rhythm
risk factor for night shift workers that eat and drink at night → increase risk circadian rhythm disruption → -vely impact sleep and wellbeing
neuromodulators and the sleep-wake cycle
dopamine and serotonin maintain alertness and motivation during waking hours → they become less active during sleep
decrease in dopamine and serotonin activity → contributes to transition from being awake to sleep
NEUROMODULATORS AND CIRCADIAN RHYTHM SLEEP DISORDERS
DSPS = serotonin disruptions → delayed release melatonin
ASPD = abnormal dopamine regulation → increased alertness evening + difficulty staying awake during day
shift work = exposure to light and work at night → affect release and sensitivity dopamine + serotonin → disrupted d + s signalling → difficulties falling asleep during day + staying awake at night
— s disruptions and abnornal d regulation → bc changes in their receptor sensitivities?