Psych 160D/Bio N165: Final Exam!
1/194
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
195 Terms
Major roles of the Limbic System
controls *mood, attitude, & storage of emotional memories*
- basic metabolism control; appetite & circadian rhythm
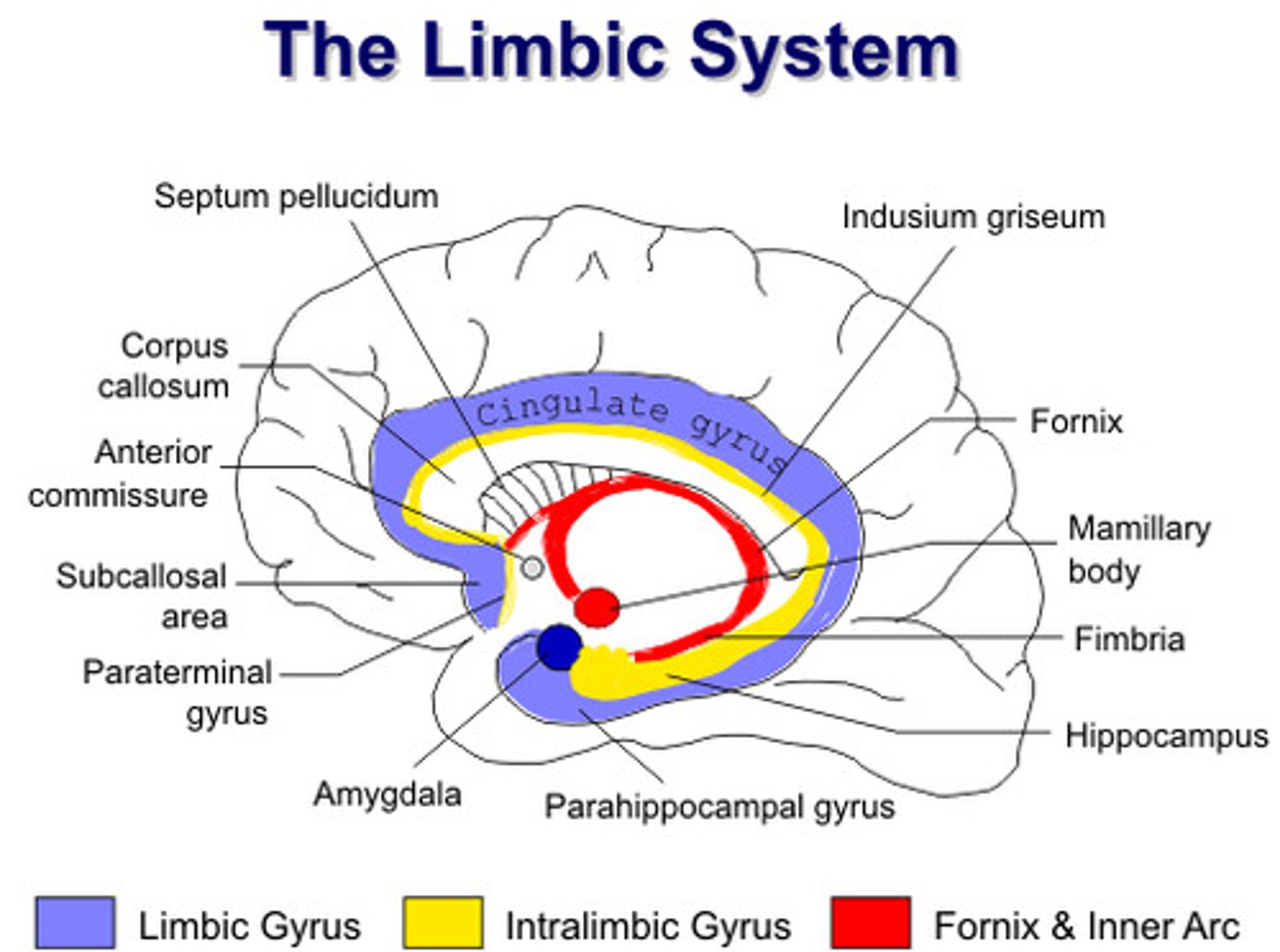
What happens if regions within the limbic system become hyperactive?
temporal lobe seizures
Hormones
released by different structures in the limbic system that can set up a cascade of cognitive and physiological response
Depression
neuropsychiatric disorder with symptoms such as
- low mood
- insomnia/hypersomnia
- weight loss/gain
- anhedonia: loss of pleasure
- suicidal ideation
- fatigue: feel as though it takes way too much energy to even get up to use the bathroom
- psychomotor retardation/agitation
- guilt/worthlessness
- brain fog
- delusions
!! underlying genetic predispositions + environmental triggers

When do delusions in depression occur?
only in very severe cases of depression
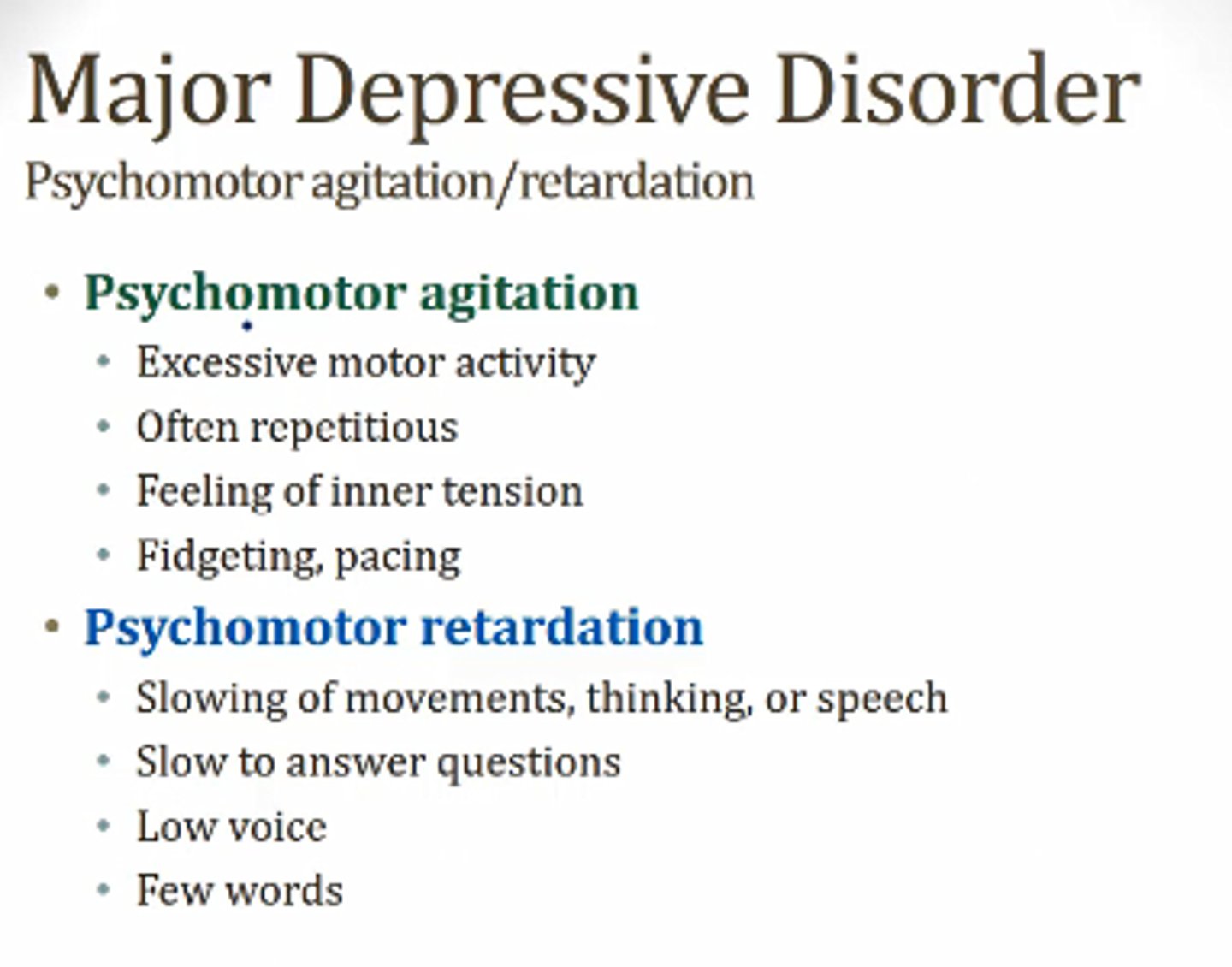
Psychomotor agitation vs. Psychomotor retardation
- agitation: jittery/hyperactive/anxiety thinking; pacing, uncontrolled tongue movements, pulling off & putting on clothes quickly, etc.
- retardation: thinking/movement are very slowed
What neuropsychiatric disorder can be a FATAL disease?
depression
- suicide is 10th leading cause of death
How to diagnose depression?
- heavily reliant on SELF REPORT; hard to just visually diagnose
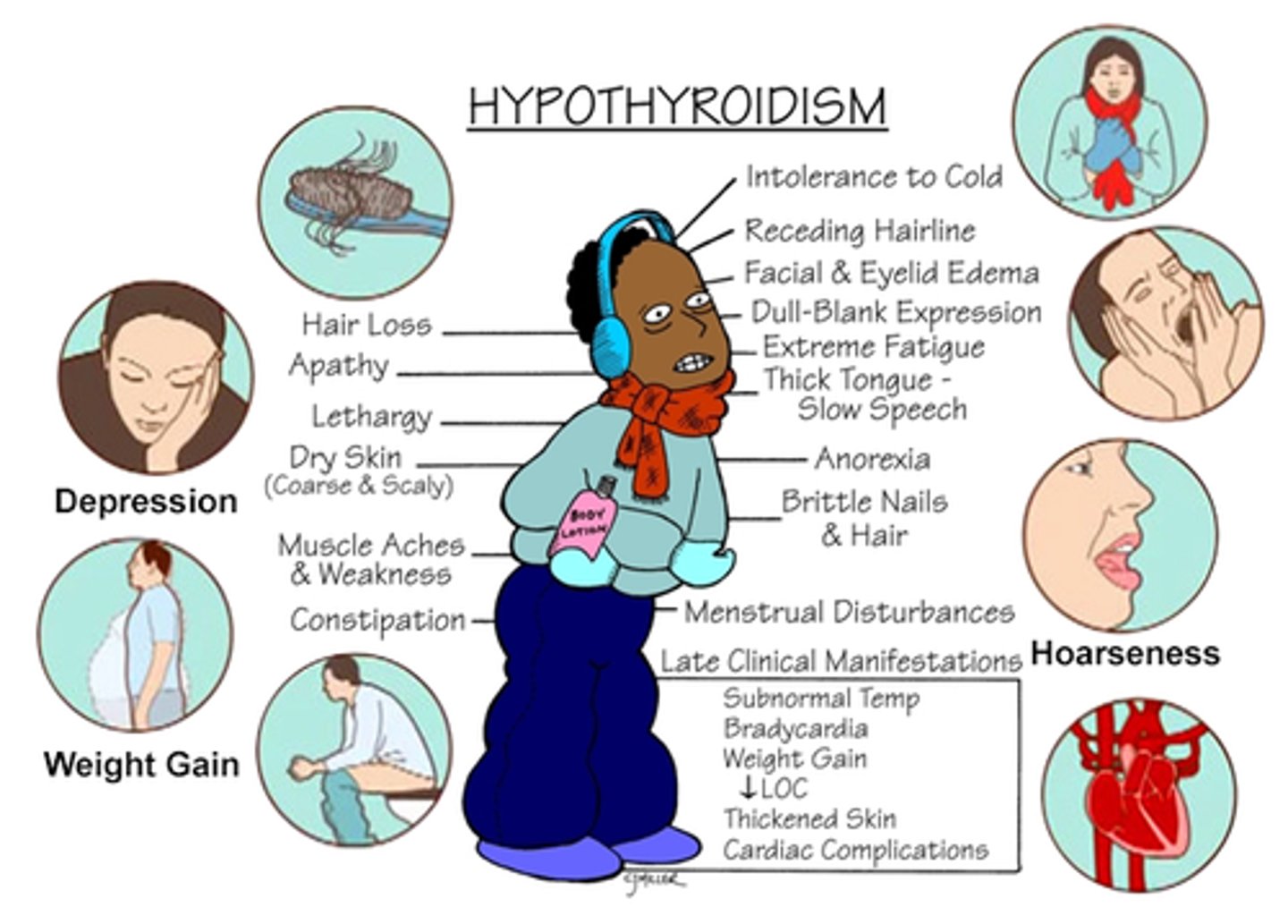
Why is it important to rule out other medical conditions/dementia when assessing a patient for depression?
medical conditions that affect hormones such as thyroid diseases/hashimotos & dementia is because they can often have depression as a secondary symptom; the depression can be cured if the initial problem is resolved instead of putting them on anti-depressants
Endogenous vs. Reactive meaning in terms of depression
Endogenous: depression due to an internal/chemical problem in the body
Reactive: depression due to external problems such as something bad that triggered the depression
idea is that maybe something reactive occurred that triggered a biological change in an individual, causing development of depressive disorder
Who is at higher risk for suicide, and why?
Who is more likely to have depression?
- men; may be because testosterone levels are higher making it possibly easier to act on suicidal ideations
- women; may be because we have more fluctuation of hormones, are women are more inclined to talk about their emotions and seek treatment

Melancholic depression
classic form of depression with low mood
- insomnia
- loss of appetite
- anhedonia

Atypical depression
- overwhelming reactions to environmental circumstances
- paradoxical anhedonia: APPEARS happy but doesn't FEEL happy
- comfort eating: major weight gain
- hypersomnia: sleeping too much
- leaden paralysis: limbs feel heavy = feel like they are paralyzed
- hypersensitivity to small/non-negative things

Potential cause of Atypical depression?
*changes in circadian rhythm* causing "hibernation" like symptoms
Dysthymia
low-grade depression
- lasts VERY LONG TME; > 2 years

Adjustment disorder with Depressed mood
depressed mood due to a significant event/stressor/trigger
- symptoms are significant but not enough to meet criteria for major depression
- kind of like a grey area between normal grief & major depression

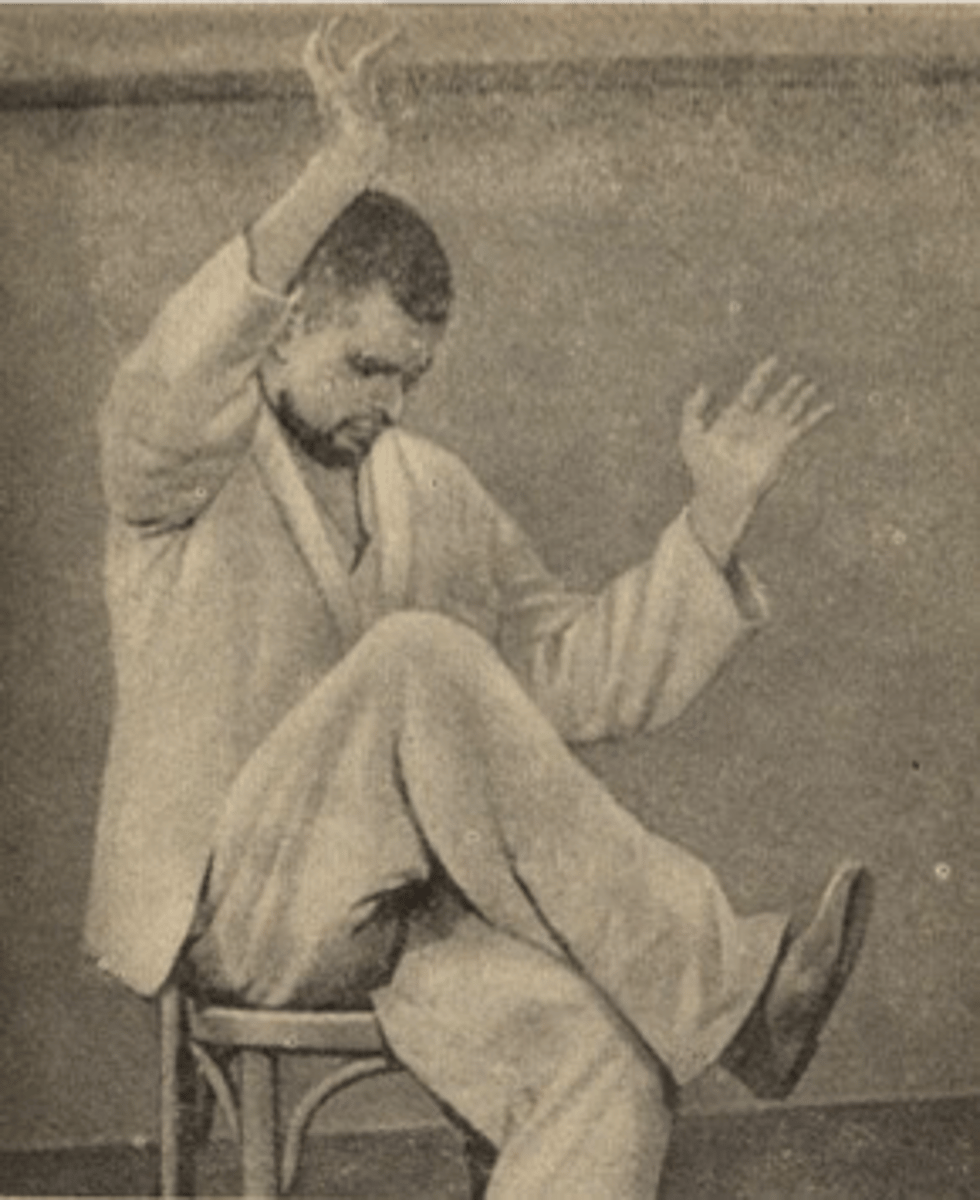
Catatonic depression
rare, severe depression with disturbances of motor behavior and speech
- severe psychomotor retardation; can put them into certain positions they will maintain over a long period of time
- they are "cut off from the world"
Depression due to hormonal influence: Postpartum depression
intense, sometimes disabling depression experienced after giving birth
- lasts longer than the typical 2 week 'baby blues'
- lasts ~ 3 months-years
- cause: massive change in brain/body chemistry due to delivery of placenta = major, abrupt change in hormone levels

Postpartum psychosis/mania
delusional/abnormal thinking and beliefs
- involved in those cases where mothers feel the need to kill their babies
- rare!
Depression due to hormonal influence: Premenstrual Dysphoric Disorder (PMDD)
severe, debilitating prementrual symptoms
- start ~ 1 week prior to period & ends abruptly when period ends
- treatment: lose dose anti-depressants during symptoms
Depression due to circadian rhythms: Seasonal Affective Disorder (SAD)
depressive episodes beginning fall/winter & resolving in spring
- at least 2 episodes have occurred in fall/winter months for at least 2 years
- intense hunger, weight gain, hypersomnia, depression
- treatment: light therapy
^ similar to hibernation symptoms

What does it mean that causes of depression are MULTIMODAL?
there are multiple causes that contribute to the development of depression
- biology: short alleles, reduced MAOs, smaller hippocampus, female hormones
- psychology: learned helplessness, rumination, trauma
- social: lack of support, early life neglect/trauma
- sociocultural: female gender roles, sexuality, racism,
Biological cause of depression
reduction of MAOs, changes in hormones, changes in circadian rhythms, stress responses
Monoamine hypothesis
changes in levels of crucial neurotransmitters such as MAOs can have psychological effects affecting mood
- ex: anti-psychotics that decrease dopamine can lead to other side effects such as depression
Specific monoamine hypothesis
pre-synaptic & post-synaptic changes in norepinephrine & serotonin can lead to depression
Psychosocial cause of depression
there is a positive correlation between stressful events/triggers & the onset of depression
- everyone has differences in what may trigger their depression based on genetic factors
- ex: a spike in cortisol due to a major life event may alter serotonin pathways from here on out = ongoing biological effect that maintains depressive symtpoms
Cognitive model of depressed patients by A.T. Beck for Psychosocial depression
depressed patients who whole negative views of themselves will cause recurrent patterns of depressive thinking towards themselves, the world, and others
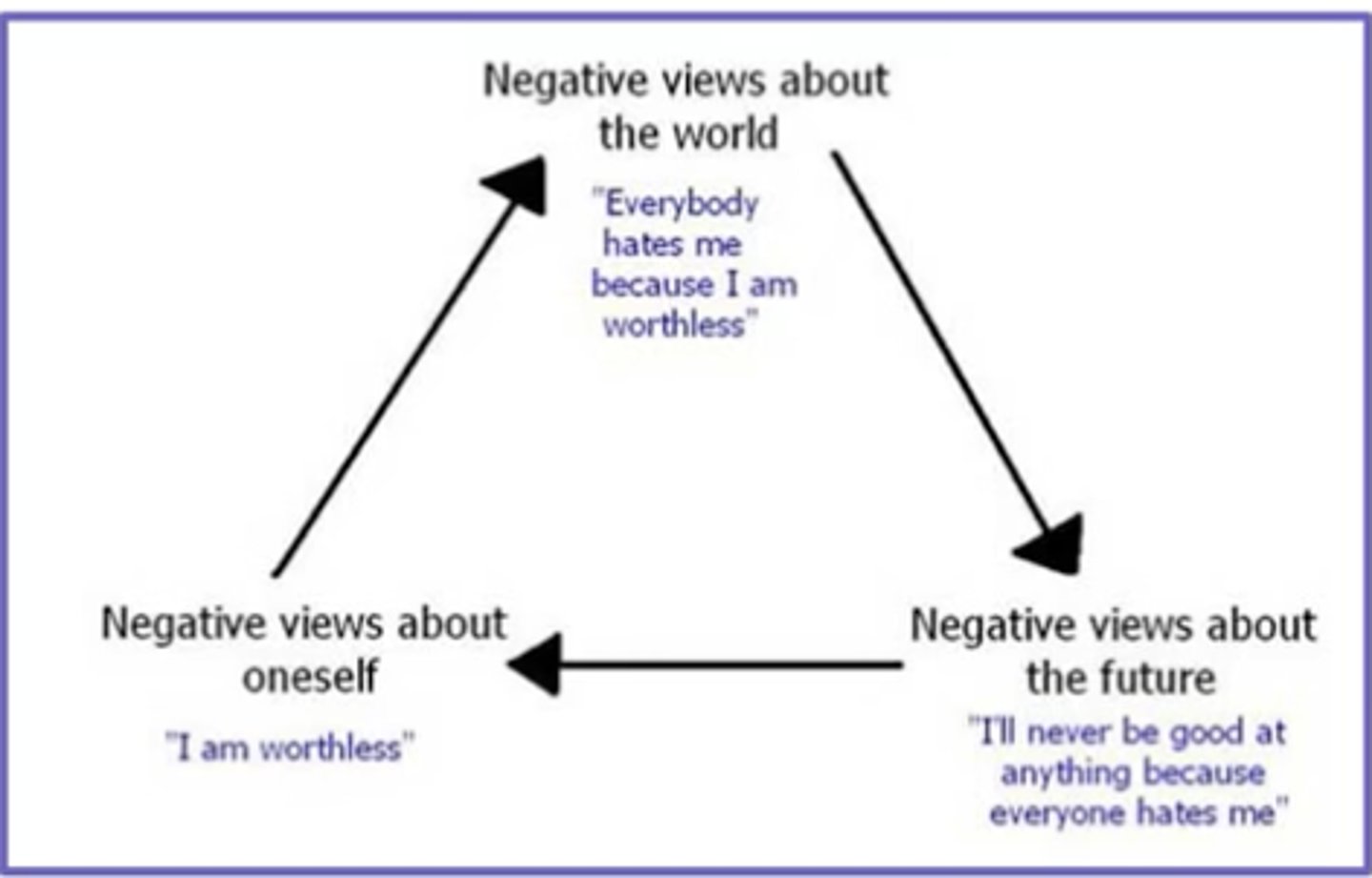
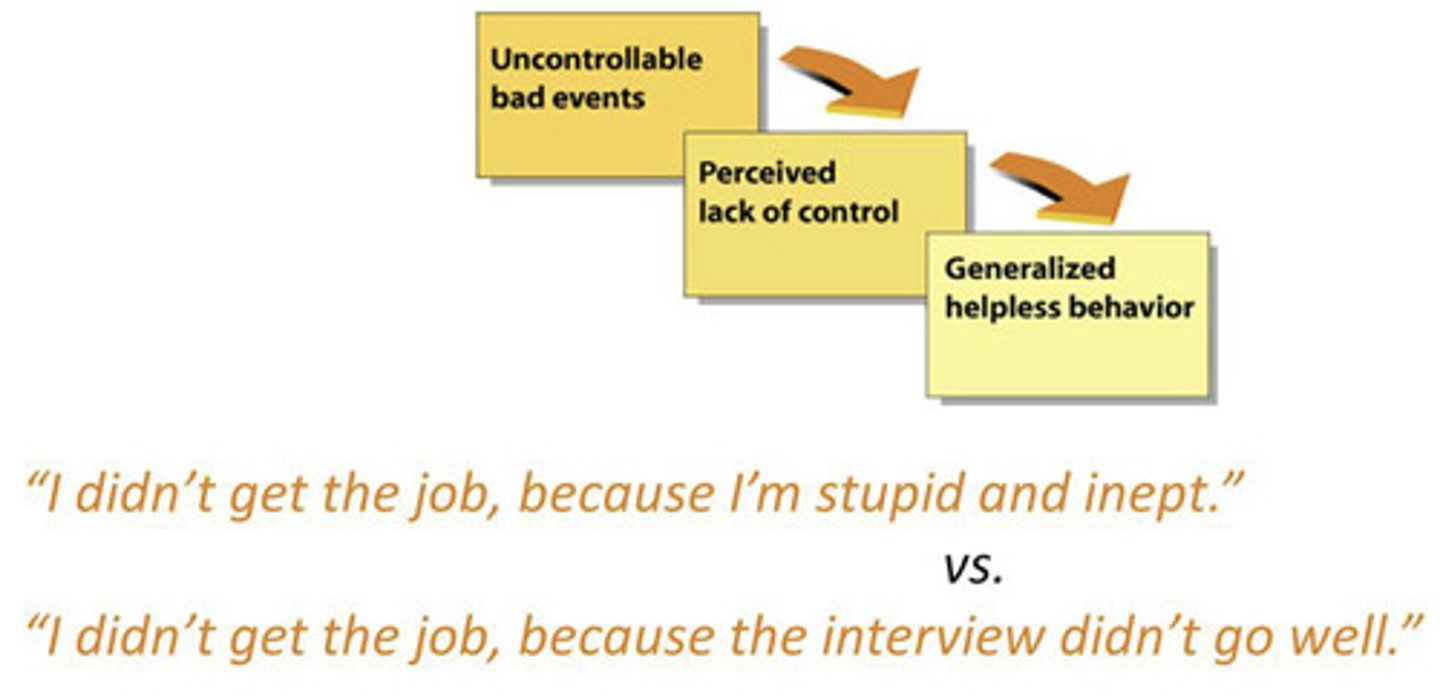
Learned hopelessness theory for Psychosocial depression
depressed patients lose hope that life will get better based on previous experiences, so they generalize past experiences to future situations
- focus on self-worthlessness
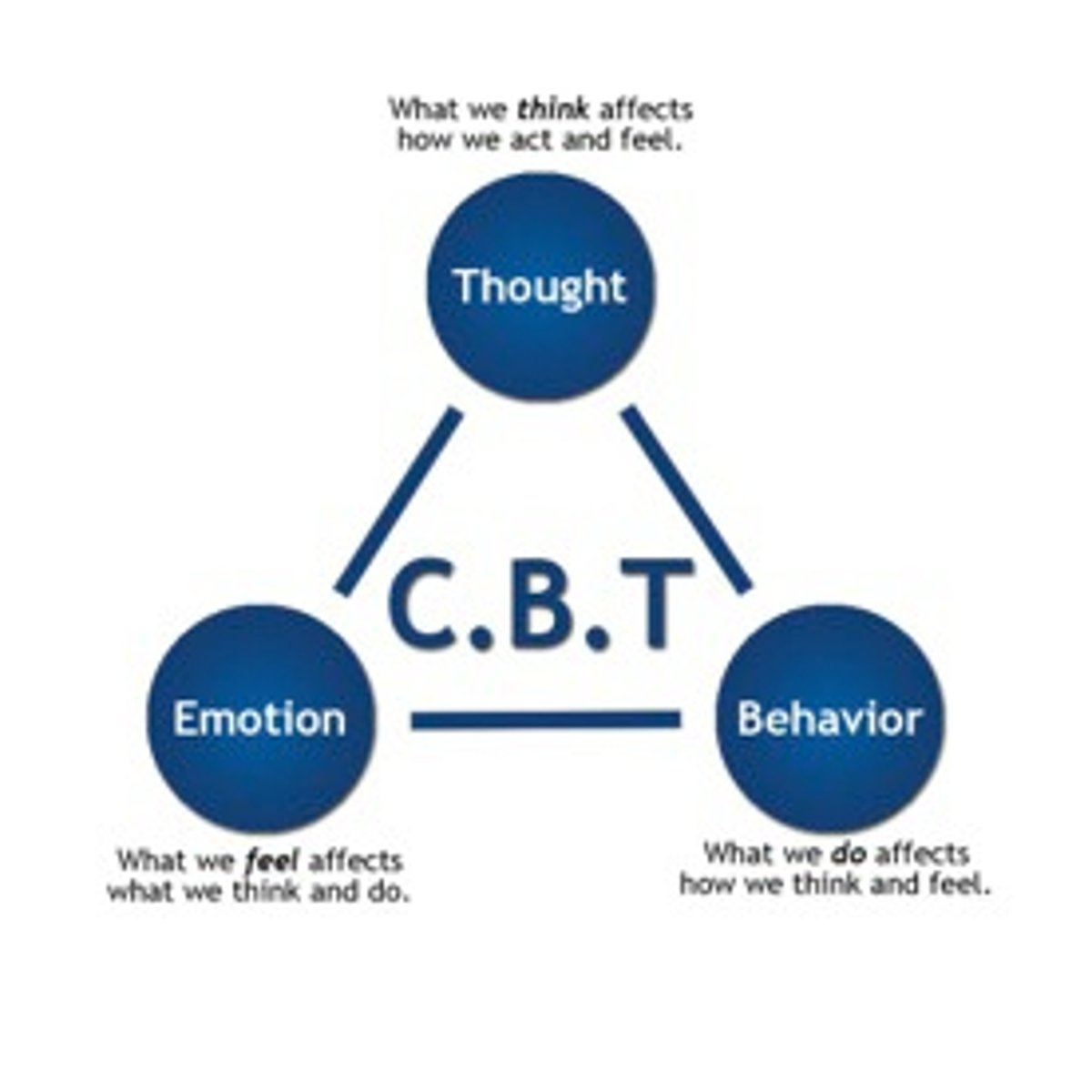
Psychotherapy treatment for depression
CBT: cognitive behavioral therapy
- attempts to break negative thinking/perseverance loop/learned helplessness
- hoping they can catch themselves in the future & change their way of thinking to prevent worsening of symptoms
Medication treatment for depression
- MAOIs: inhibit the enzyme that breaks down MAOs in the synapse to keep them around longer
- tricyclic antidepressants: 3-ring chemical structure that treats depression; *works on SEROTONIN & NOREPINEPHRINE*
^^ can take a long time to work; 6-8 weeks
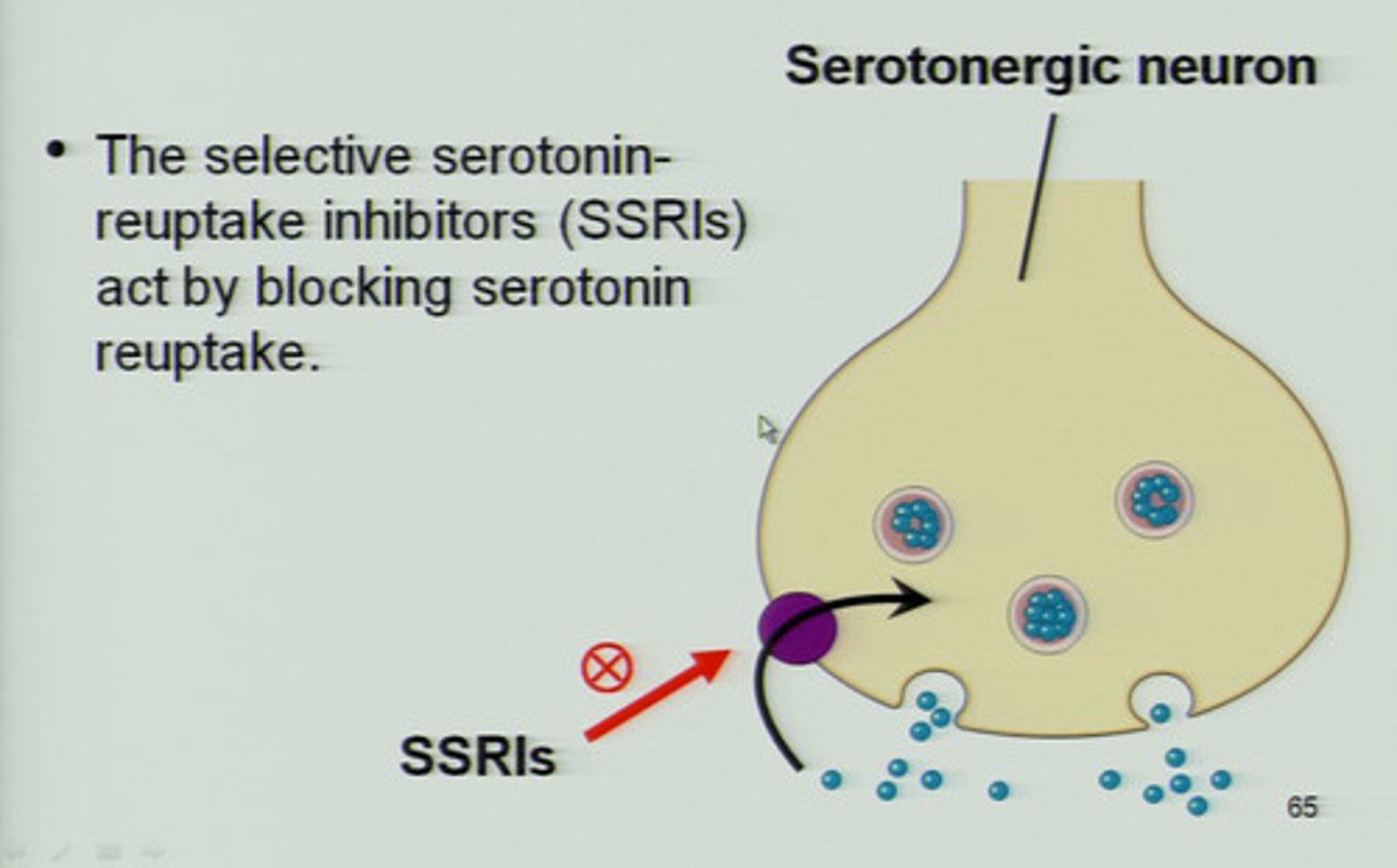
SSRIs/Selective serotonin reuptake inhibitors
blocks reuptake of serotonin so that there is more serotonin available to act on the receptors in the post-synaptic cleft
NSRIs/Noradrenergic serotonergic reuptake inhibitors
blocks reuptake of serotonin & norepinephrine
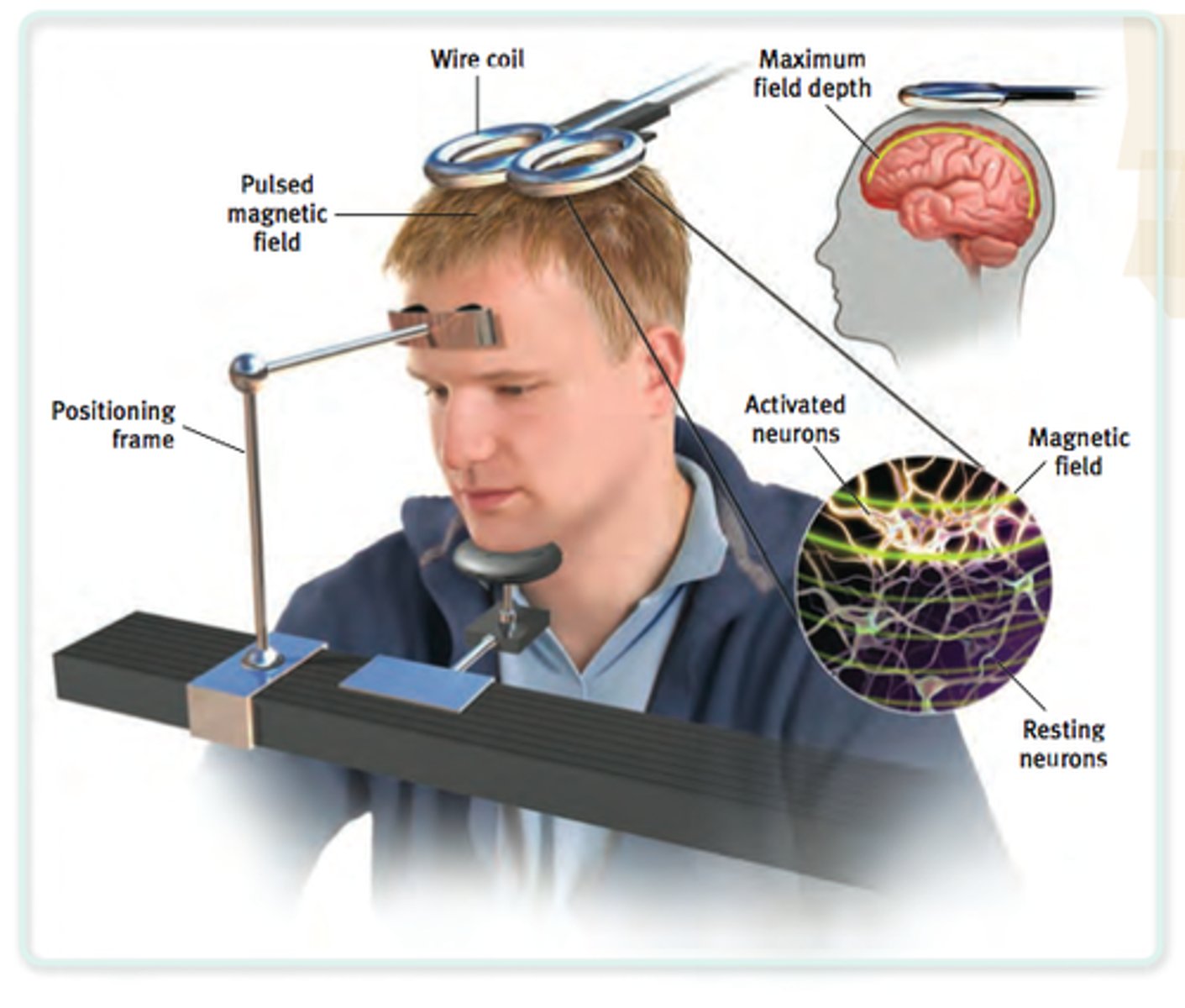
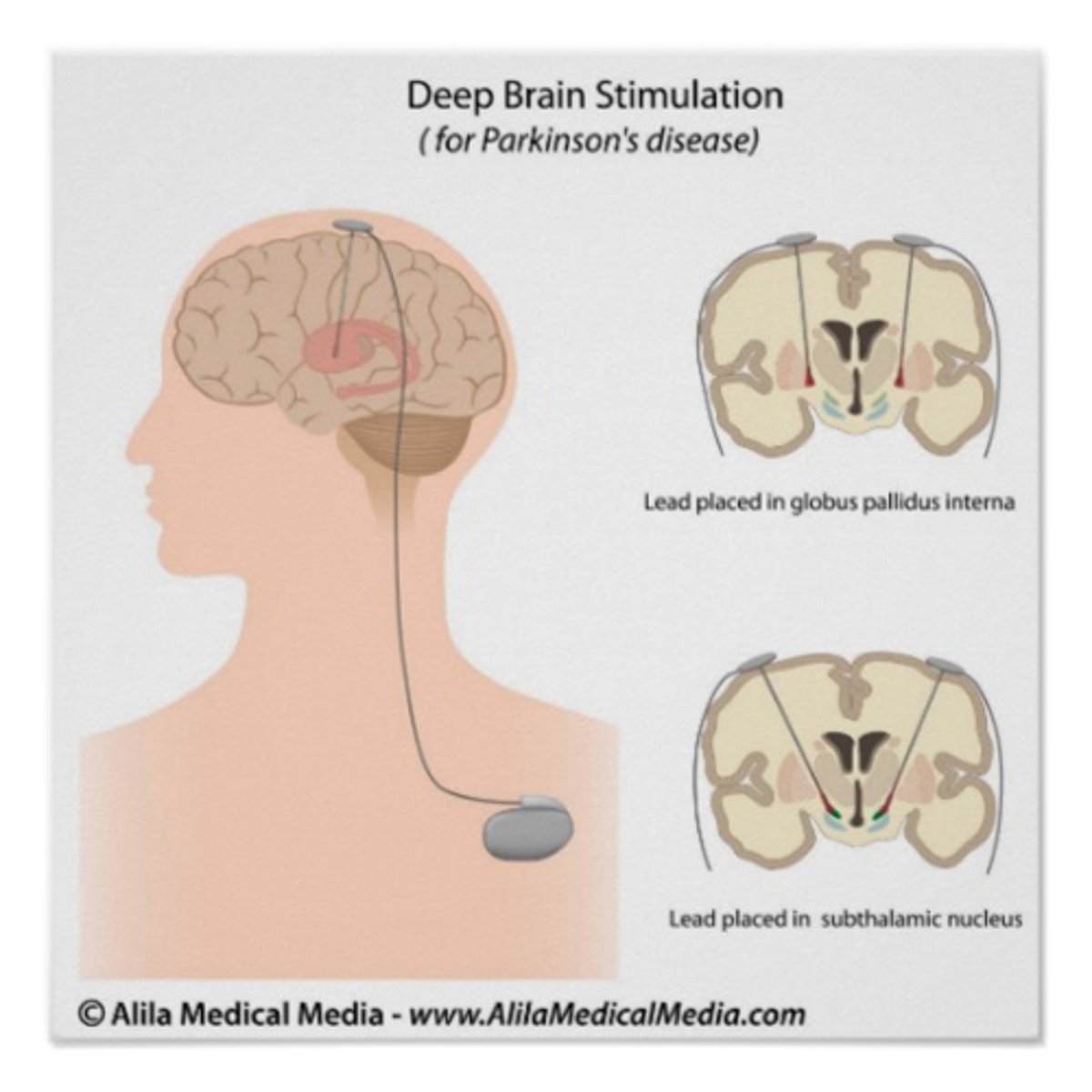
Stimulation treatment for depression
- electroconvulsive shock therapy
- transcranial magnetic stimulation
- deep brain stimulation
Electroconvulsive shock therapy
used to treat severe depression; given 3x/week for 1 month, then monthly maintenance
- basically a grand mal seizure to "reset" the brain
- may experience slight fatigue/memory loss

Transcranial magnetic stimulation
milder version of electroconvulsive shock therapy
- inducing electrical current in brain on the external surface
Deep brain stimulation
used to treat severe depression; electrodes placed inside brain in basal ganglia
- very invasive so risk for infection but best results, usually immediate
A patient presents to the ER with rapid speech, delusions of grandeur, and psychomotor agitation. What is the likely diagnosis?
a) drug ingestion
b) brain tumor
c) mania
d) A & C
e) all of the above
e) all of the above
What is mania?
state of extremely elevated mood & impulsivity, often times putting oneself at risk
- irritability, anger, rage
- delusions
- hypersensitivity, hypersexuality, hyperreligiosity
- racing thoughts --> pressured speech: thoughts are so fast & abrupt their speech is the same; cannot even get a word in when talking to them
- decreased need for sleep --> leads to psychosis/delusions

What is hypomania?
like a stepping stone on the way to full blown mania; overly excited, euphoric but* still coherent*
- highly productive & focused
- decreased need for sleep; enough to avoid psychosis but still prominent
- extroversion
- *NO DELUSIONS!*

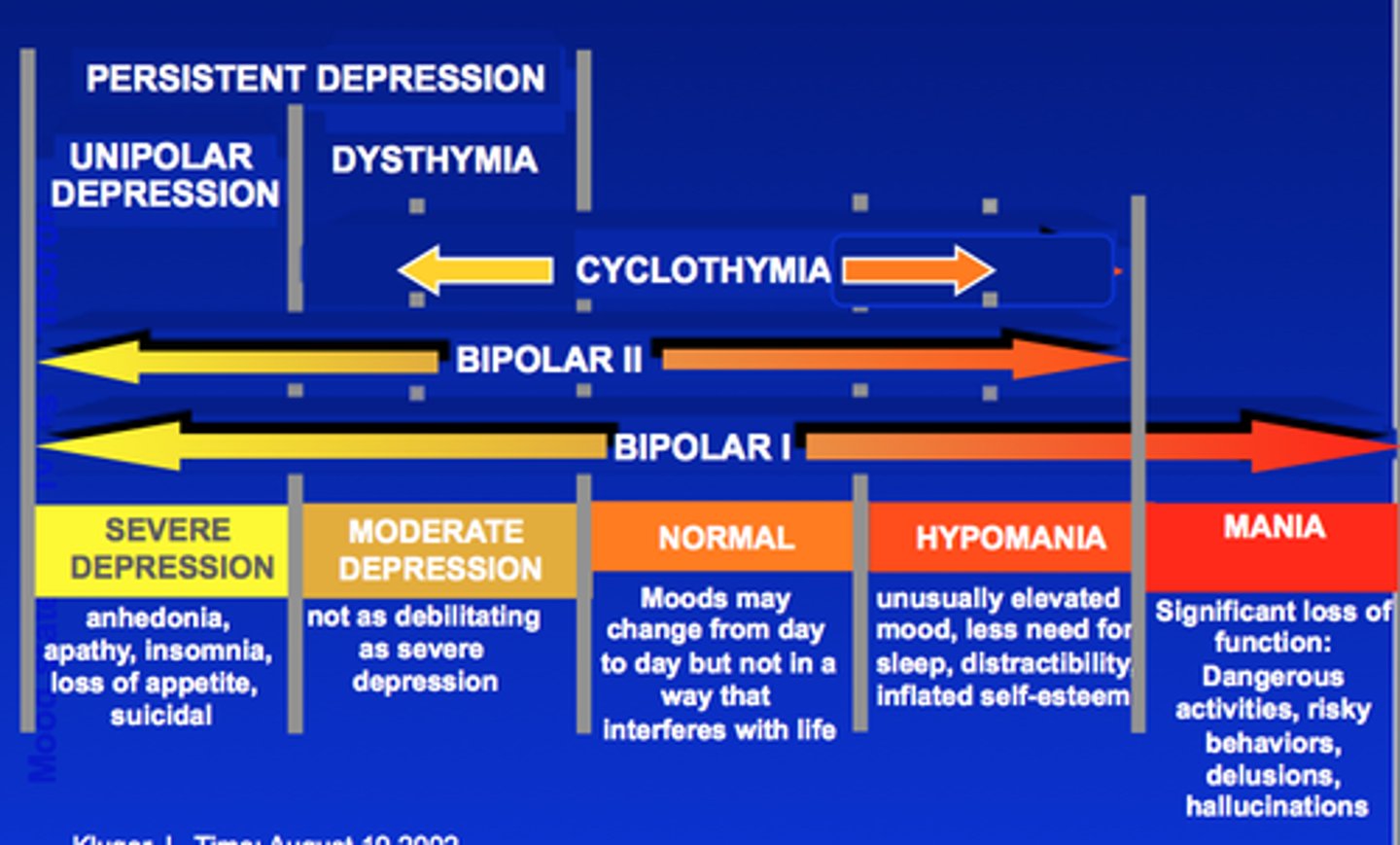
Bipolar 1
episodes of severe depression & full mania
- more common in males

Bipolar 2
episodes of severe depression & hypomania
- more common in females
Cyclothymia
episodes of dysthymia & hypomania; low-grade Bipolar
What is the prevalence for Bipolar between genders?
equal prevalence, not sex linked!
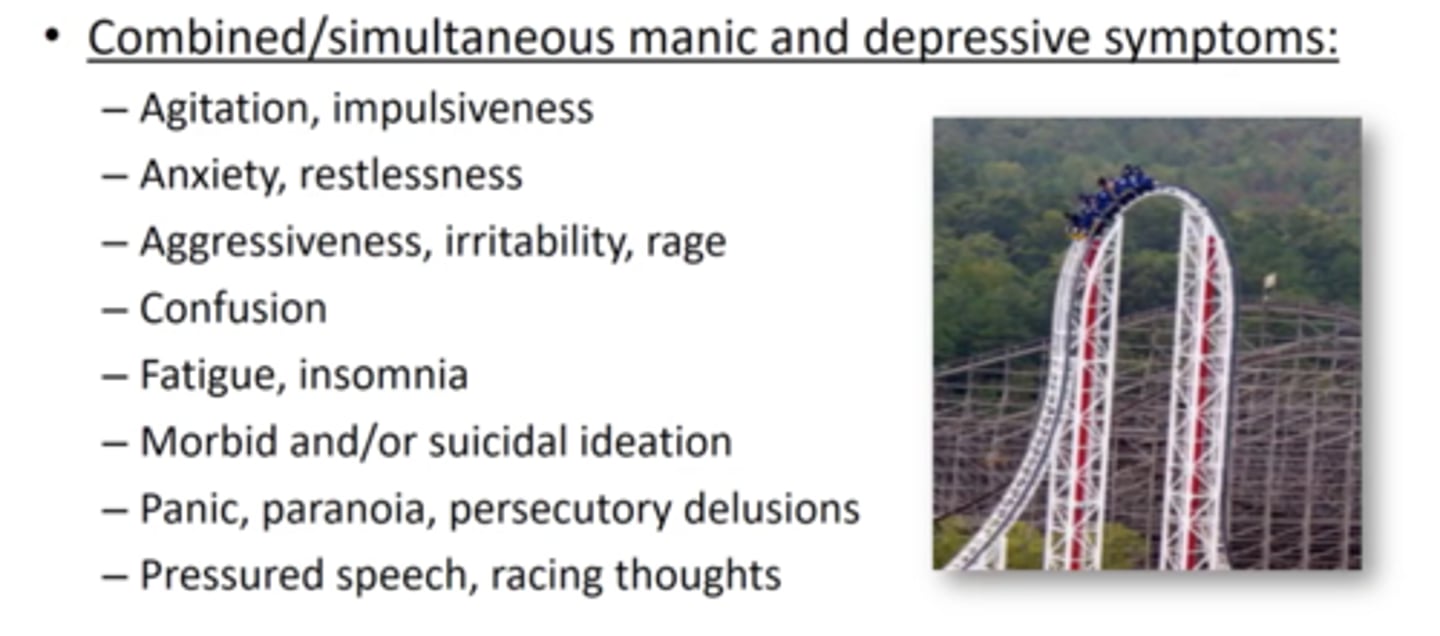
Mixed affective disorder
SIMULTANEOUS manic & depressive symptoms
- agitation/impulsivity
- anxiety
- aggression/rage
- fatigue/insomnia
- suicidal ideation
- paranoia
- pressured speech/racing thoughts
Cause of Bipolar disorder
- genetics & environmental triggers
- different size of hippocampus, PFC, amygdala
- abnormal hypothalamus-pituitary-adrenal-axis
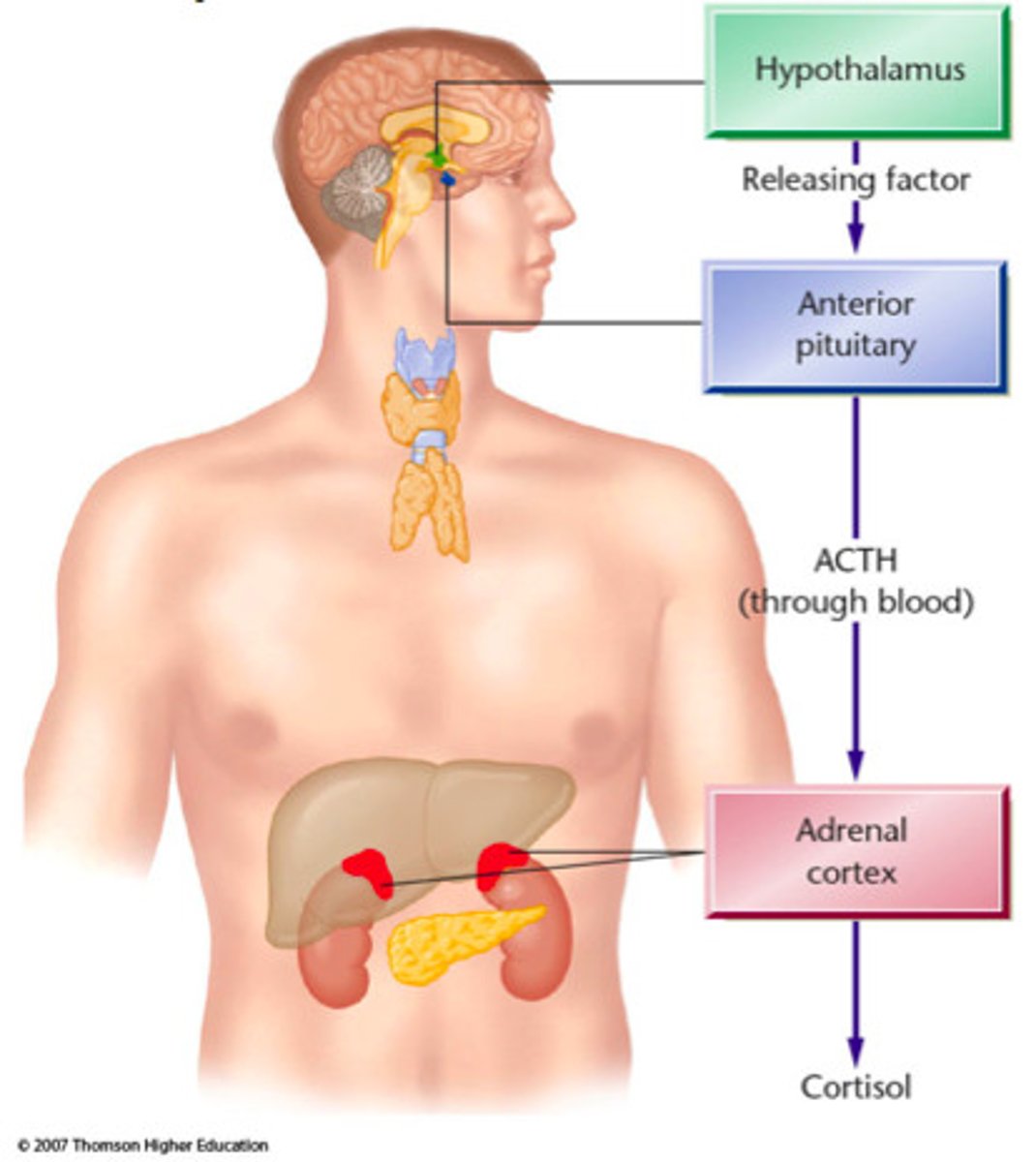
Hypothalamus-pituitary-adrenal-axis
major part of neuroendocrine system that CONTROLS REACTIONS to stress & regulates hormonal body responses such as mood & emotion
- abnormal in those with mood disorders like BD, depression, anxiety
Mood stabilizers for Bipolar disorder
are used to balance mood & PREVENT MANIA in those with Bipolar disorder
- ex: Lithium
- must be used with anti-depressant!
Anti-convulsants/anti-seizure for Bipolar disorder
lowers overall/brain-wide activity to produce calming effects
For Bipolar disorder, what 2 medications always have to go together?
mood stabilizers like Lithium always have to go with anti-depressants & vice versa, to avoid major depressive episodes or hyper-manic episodes
Anti-psychotics for Bipolar disorder
lowers dopamine & treats manic agitation
Anxiety
diffuse, feelings of fear & apprehension that are more exaggerated than it should be, or occur when there is no reason to be scared
- everyone feels anxious but its a disorder once it interferes with daily life

Phobias
intense, irrational fear & response of specific objects/situations
- may develop through classical conditioning = one exposure is now generalized to every future exposure

Anxiety disorder
set of disorders where normal anxiety response is inappropriately provoked by homeostatic imbalance
- there is an imbalance in one's baseline chemistry/stress response causing an inappropriate fear response to irrational things
Maladaptive behavior in Anxiety
continued stress response after a trigger/stimulus is gone, making it difficult to function normally & reduce anxiety
Possible physiological cause of Anxiety
low levels of GABA = less inhibition
What is helpful to treat low levels of GABA/the possible physiological cause of Anxiety?
- anxiolytics: increase GABA inhibition to quiet down excitation
- SSRIs: have effects on GABA circuits
Long-term medication treatment for Anxiety
anti-depressants
- SSRIs
- NSRIs
- MAOIs
Short-term medication treatment for Anxiety
anxiolytics; they are addictive which is why they are used for short-term treatment; affect GABA circuits
- Xanax
- Valium
- Ativan
Beta-blockers for Anxiety
alter natural physiology anxiety responses to calm someone down
- ex: slow heart rate
Generalized Anxiety Disorder (GAD)
chronic anxiety & TENSION > 6 months; not due to something happening such as finals, projects, etc.
- anticipating the worst, overly concerned about health/money/family/work
- headaches, stomachaches, muscle tension, trembling
- women 2x > men (this may also have to do with the fact that women are more likely to go in and get treated/tested)
Genetic cause of Anxiety
childhood trauma may lead to hypervigilence (always on eggshells/nervous), which can set someone up to be triggered later in the future by a major life event & develop GAD
Obsessive Compulsive Disorder (OCD)
anxiety disorder characterized by obsessive/distracting/intrusive thoughts that are relieved by completing certain compulsions
- common compulsions: checking & washing

Causes of OCD
hyperactive caudate nucleus
What does the caudate nucleus have to do with OCD?
the caudate nucleus is involved in motor habit forming; so when this is hyperactive it can cause repeated habits such as washing hands 5x, checking the door 10x, etc.
Treatment for OCD
- SSRIs: serotonin calms down activity in caudate nucleus
- DBS: can eradicate OCD symptoms
- CBT
Panic disorder
recurring panic attacks that feel like one is dying
- chronic fear that panic attack will happen again
- heart palpitations, sweating/shaking, chest pain, nausea, light-headed, feels like dying

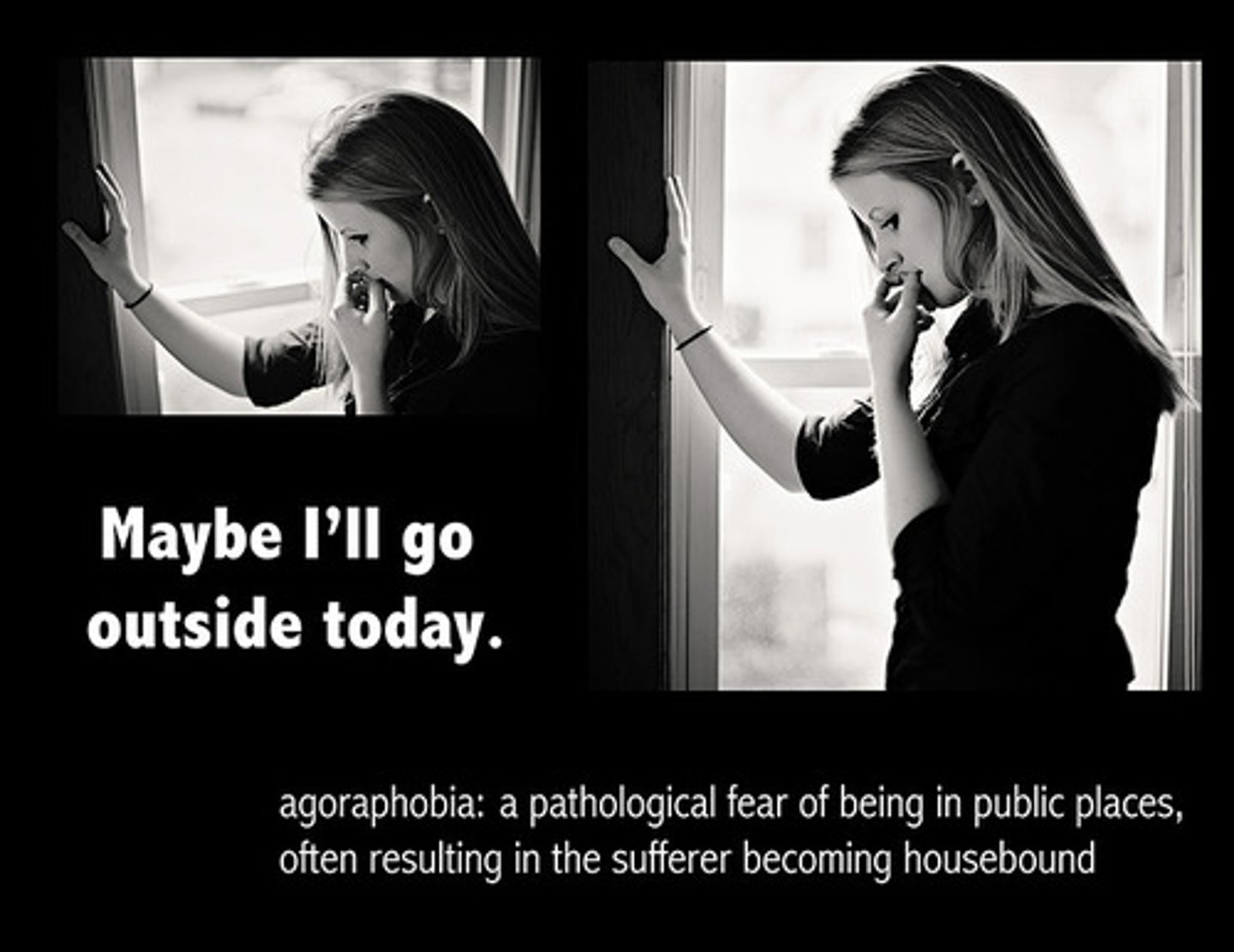
Agoraphobia
develops as a result of panic disorder; fear of having a panic-attack in situations where it would be hard to get to a safe space; fear of crowds/public settings
- Sheila from Shameless ):
How do panic disorder patients self soothe?
alcohol & nicotine
- these actually increase risk of panic attack!

Causes of Panic disorder
- genetics & environmental triggers
- huge stressful event that may eventually change/imbalance limbic system
- stimulant use
Posttraumatic Stress Disorder (PTSD)
anxiety disorder following major traumatic event lasting > 6 months
- nightmares/flashbacks
- hypervigilence
- easily startled
- lack of sleep
- depression
- avoidance
Biological basis of PTSD
- higher levels of cortisol
- differences in amygdala, hippocampus, PFC which are related to fear processing
- abnormal hypothalamus-pituitary-adrenal-axis
The frontal lobe is highly developed in?
social animals!
- humans
- chimps
- elephants

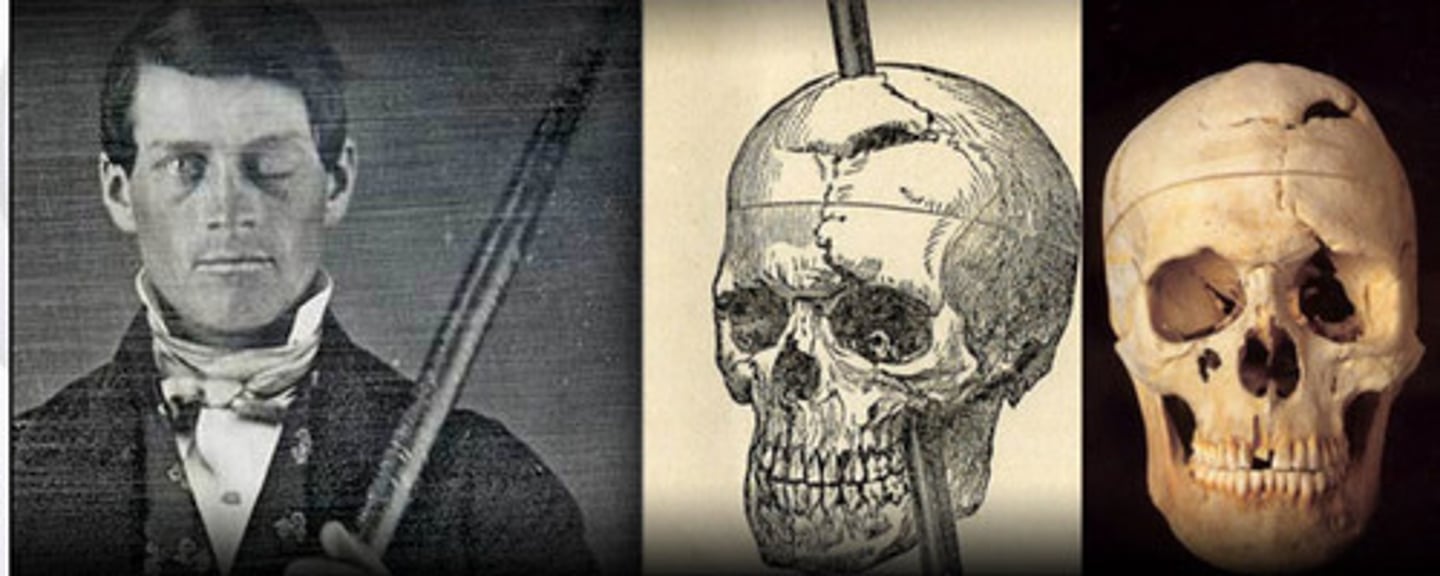
Who was Phineas Gage & why is he so important?
had a railrod shot through his PFC & eye which drastically changed his personality
- went from being very pleasant to loud, annoying, rude
- suggested that certain areas of the brain have to do with personality & behavior
After 10 months of chronic tension, a patient continually worries about imminent disasters that she is unable to concentrate on her work. She will most likely be diagnosed with??
a) Panic disorder
b) GAD
c) Bipolar disorder
d) Visual object agnosia
e) Cotard syndrome
b) GAD

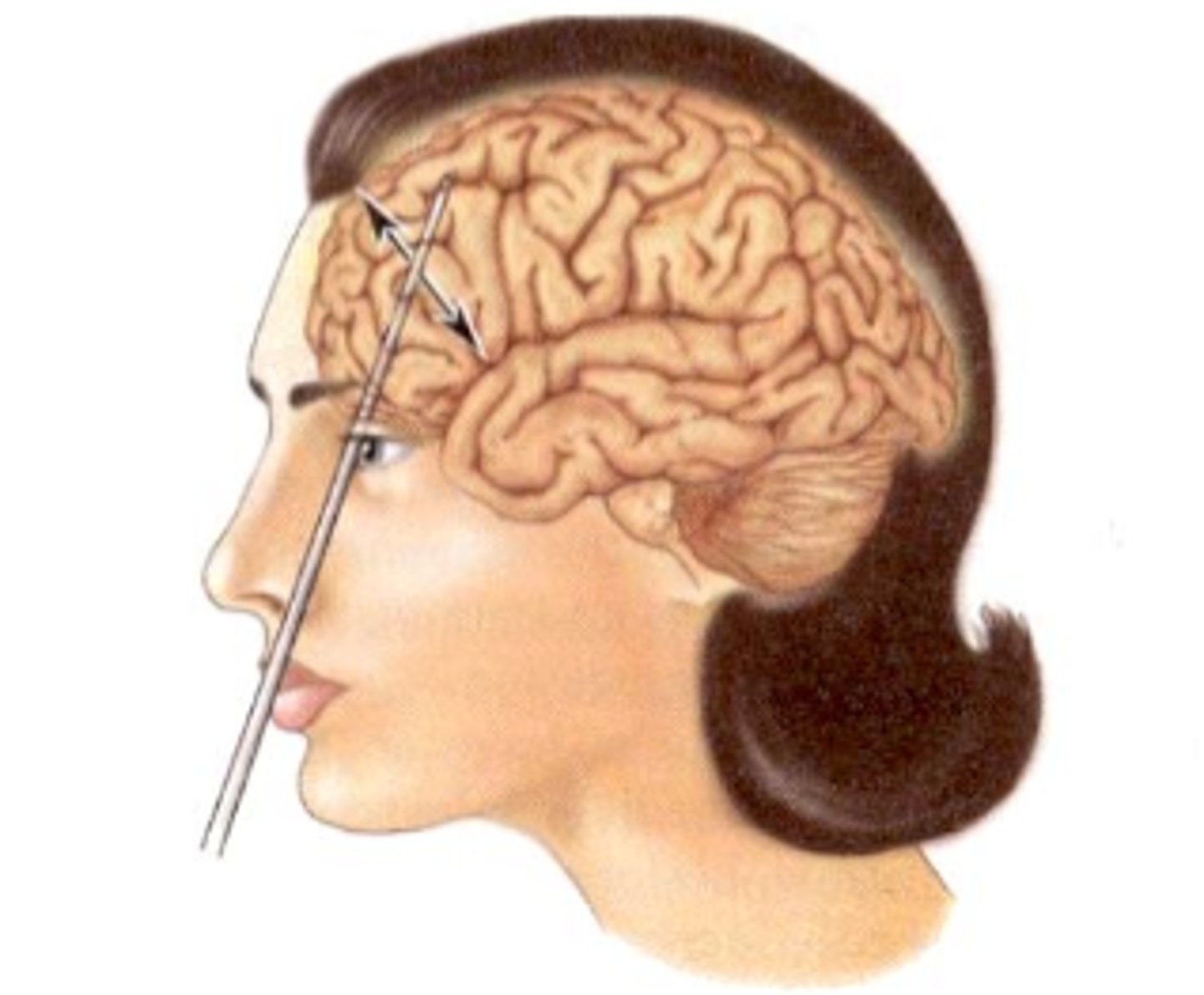
Lobotomies
popular surgery in the 30s-50s that consisted of uncontrolled destruction of the frontal cortex
- *separating prefrontal cortex from the rest of the brain*
- won a Nobel Prize
- went through the eye with an "ice pick" that didn't destroy vision
- used by *Dr. Freeman*
- last one performed in the 80s
Dorsolateral PFC
highest cortical area responsible for motor planning, executive function, regulation, & working memory
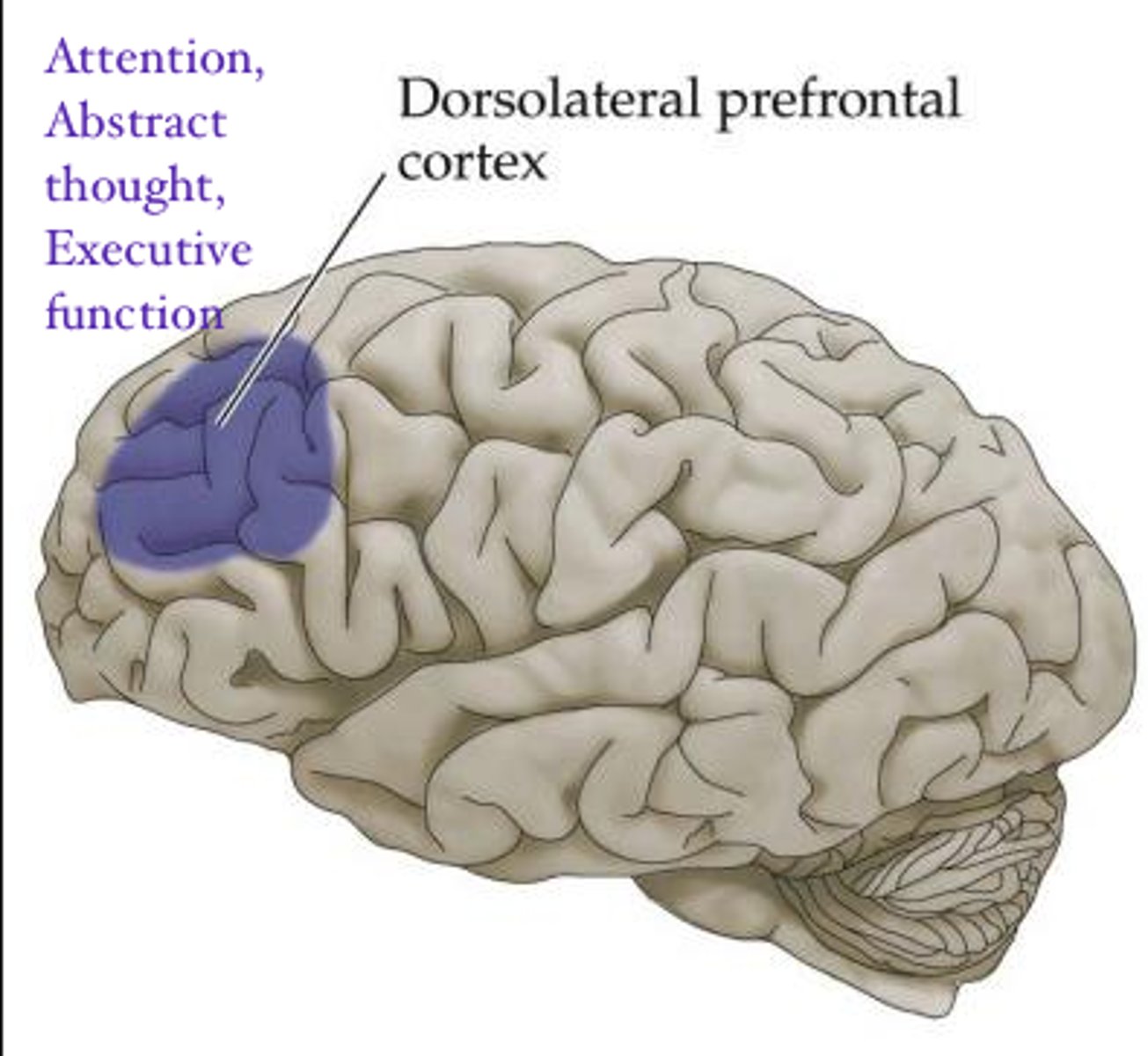
Damage to dlPFC causes?
frontal convexity syndrome; loss of higher order executive control!
- apathy, depressed
- impaired ability to plan
- lack of impulse control
- *PERSEVERATION*
- psychomotor retardation
- impaired working memory
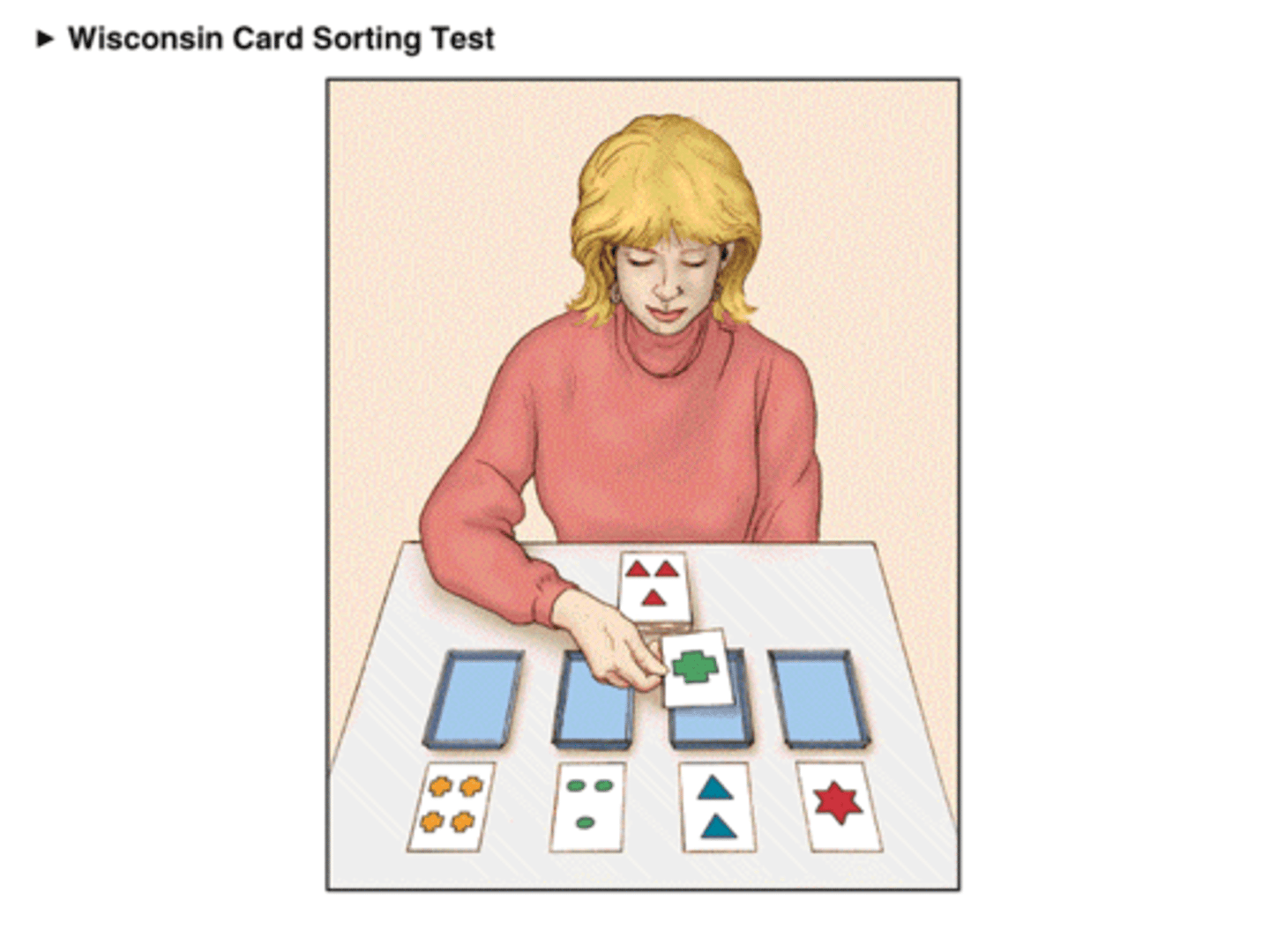
Wisconsin Card Sorting Task
used to study dlPFC & those with Frontal Convexity Syndrome
- unspoken set of rules that subject must identify after trial and error, rule changes without notification & subject must change their actions to figure out the new one
- those with dlPFC perseverate & have trouble changing the task even though they know they should
Anterior cingulate cortex (ACC)
in the medial wall responsible for emotional control & reward
- decision making (is this rewarding, should i do it?)
- empathy
- reward anticipation
- blood pressure/heart rate
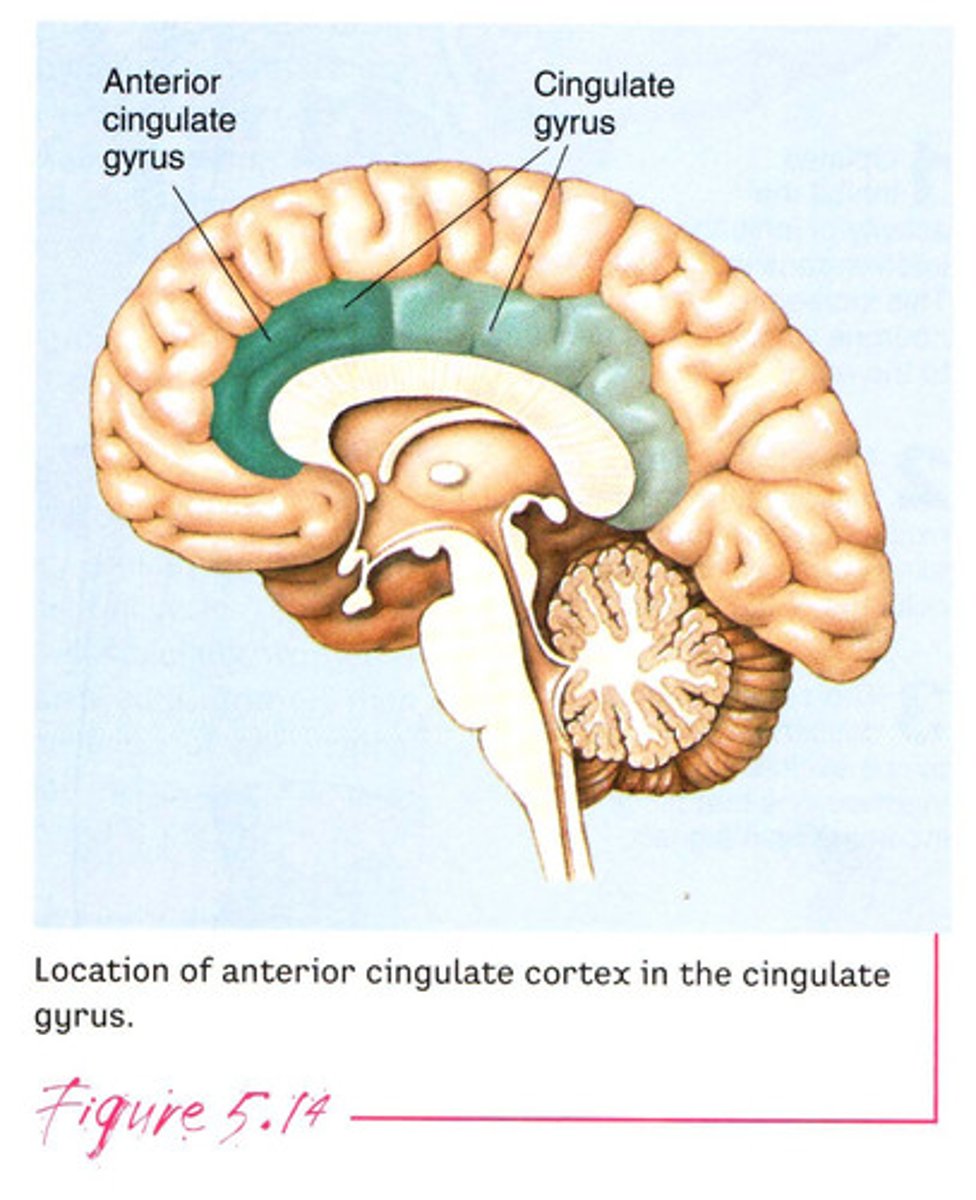
Damage to anterior cingulate cortex (ACC) causes?
medial frontal syndrome/akinetic mutism
- limiting movement & speech
- lower extremity weakness
- loss of bladder control
!! NOT PARALYZED, just lack the motivation/will to move or speak

Treatment for Medial frontal syndrome/akinetic mutism
- stimulants to increase motor/speech output
- L-dopa to increase dopamine which may increase movement
Orbitofrontal cortex
above the eyes involved in sensory integration
- associating taste to a flavor
- decision making based on reward/punishment
- regulates planning behavior
!! taking in sensory information, evaluating what we do with that, then deciding & planning what to do and how to do it
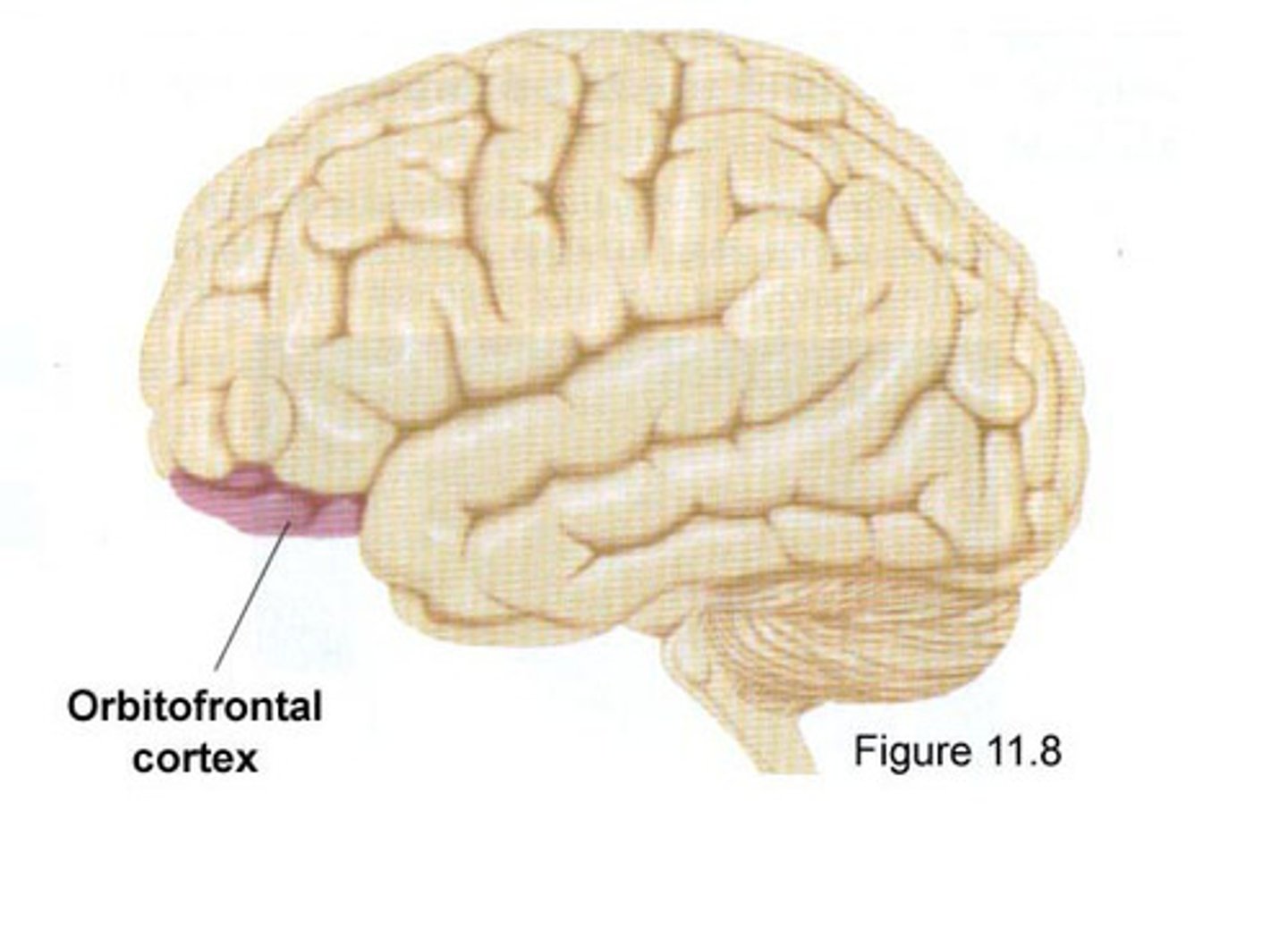
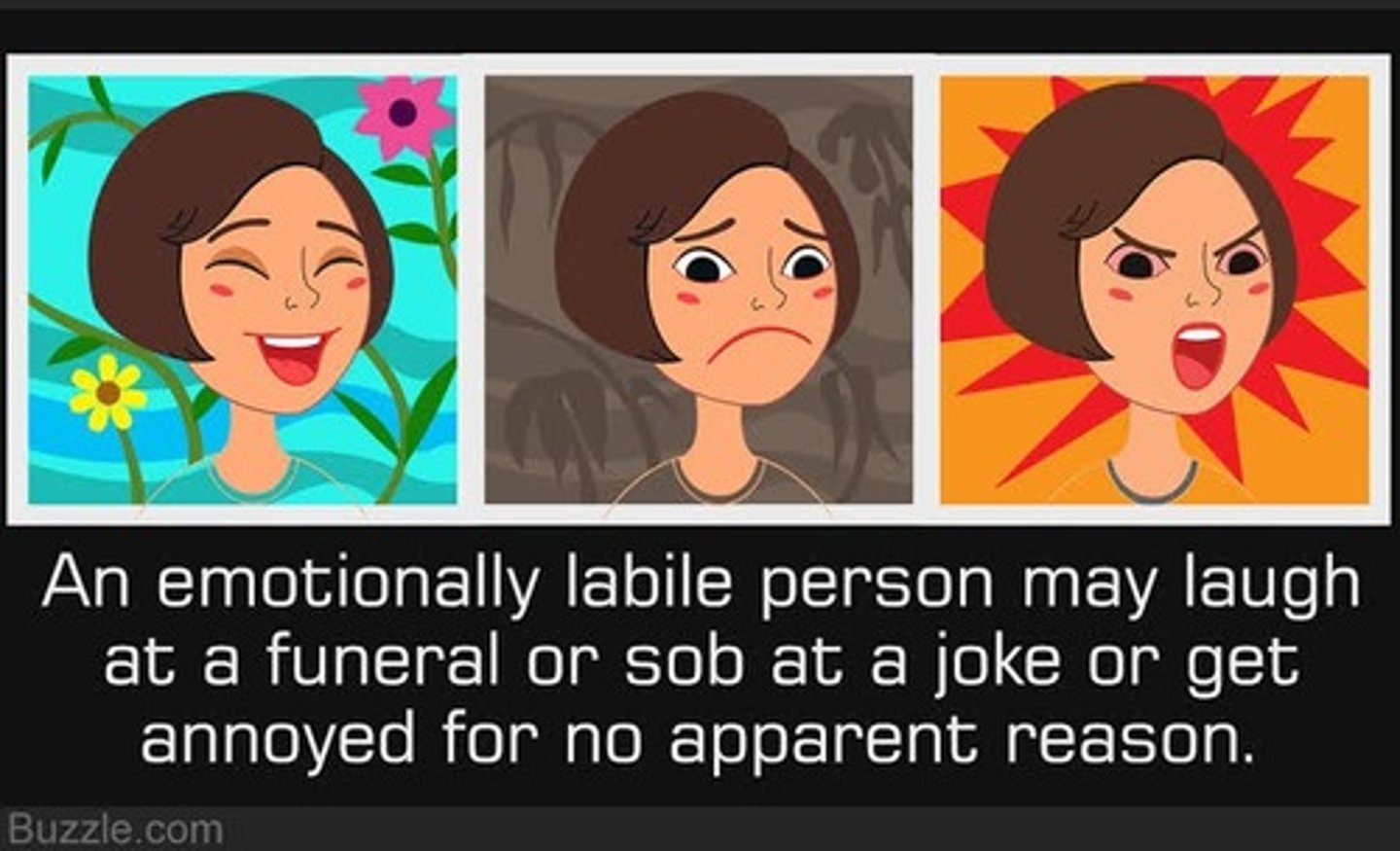
Damage to orbitofrontal cortex causes?
orbitofrontal syndrome
- pseudo-psychopathic: disinhibited/lack of impulse control!
- inappropriate social behavior
- poor judgement/danger awareness
- dangerous sexual behavior
- lack of empathy
- easily distracted
- associated with dementia?
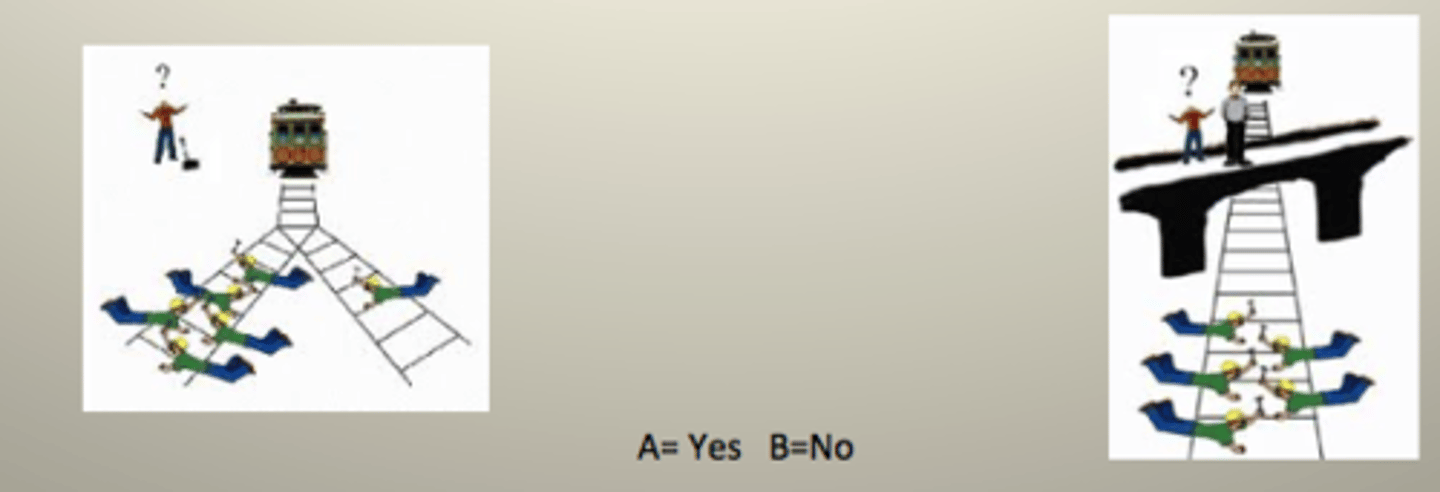
Trolley car dilemma
used to test one's empathy & understanding of right/wrong, especially in those with orbitofrontal syndrome (damage to orbitofrontal cortex)
Antisocial Personality Disorder
long term patterns of manipulation, exploiting, violating the rights of others with a lack of empathy
- reckless disregard
- aggressive
- superficial charm: pretending to care
- feeling above the law/failure to conform to social norms/expectations
- *common in felons/criminals
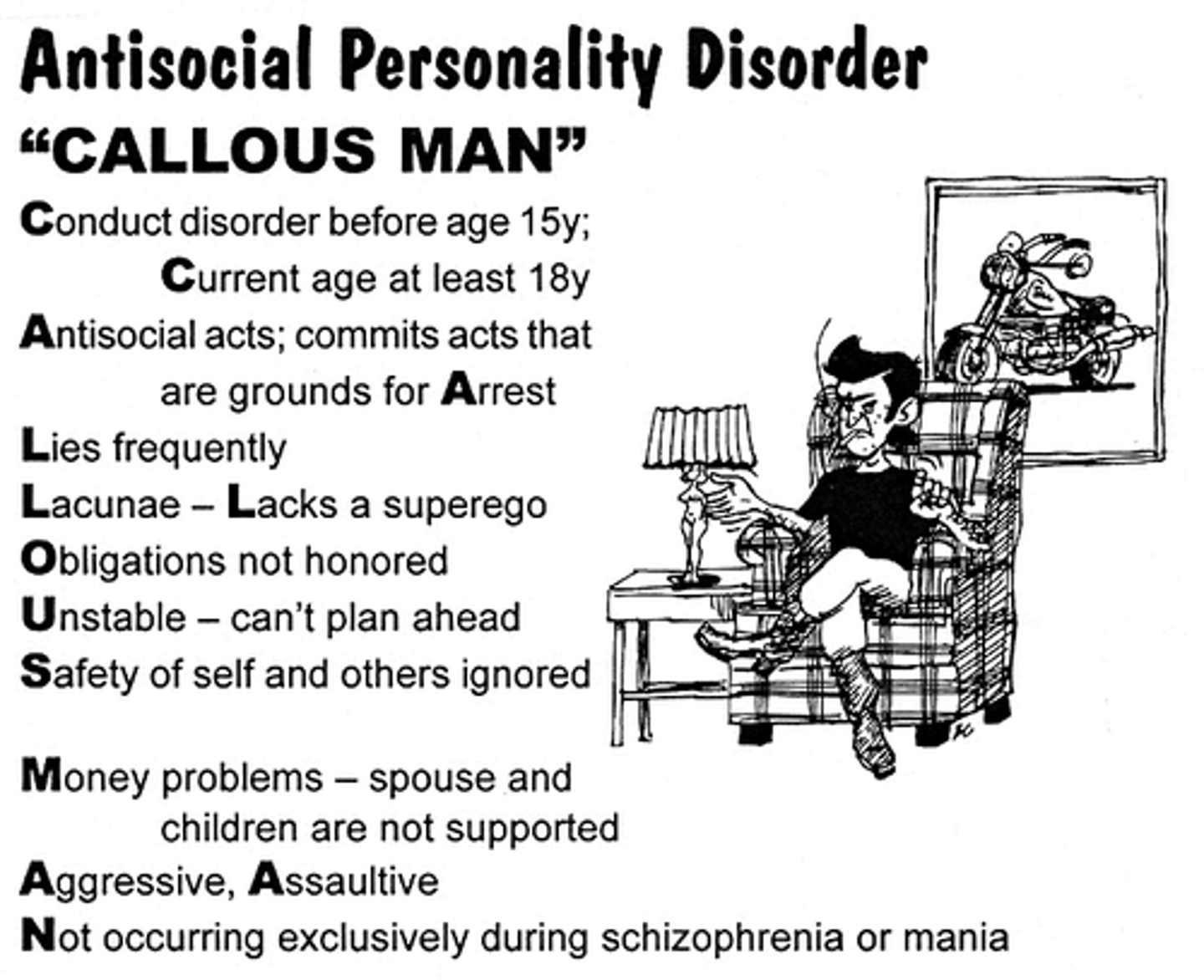
What happens if an individual shows signs of Antisocial personality disorder before the age of 18?
diagnosed with conduct disorder
Conduct disorder
juvenile antisocial personality disorder
- bedwetting (due to lack of control)
- animal abuse
- pyromania
- authority problems

Psychopathic personality disorder
arrogant, callous, manipulative, intentional, organized, etc.
- no empathy

Sociopathic personality disorder
impulsive, prone to boredom, irresponsible, reactive
- no empathy
- *dissocial personality disorder*
Tourette's syndrome
motor & verbal tics that can change overtime; typical onset is in childhood
- temporarily suppressible tics that feel like an unwanted urge; feel relief once they complete the tic
- only 10% have coprolalia (innapropriate vocal tics)
- common in association with OCD, ADHD, etc.
- boys 4x > girls

Cause of Tourette's syndrome
- frontal lobe & basal ganglia inhibition = lack of vocal/motor impulse control
- DECREASED size of caudate nucleus is correlated to WORSENED severity
- stress makes tics worse
Treatment for Tourette's syndrome
- CBT to change tic habit to something more manageable
- DBS
- antipsychotics, antidepressants, blood pressure meds
Kluver-Bucy syndrome
a higher order object identification problem & LOSS OF FEAR RESPONSE
- impairment in recognizing right/wrong & what is salient & what is not
- eating inappropriate objects
- identifying objects with mouth
- sex with innapropriate objects
- visual agnosia (explains identifying objects by mouth)
- hypermetamorphosis: finding everything salient
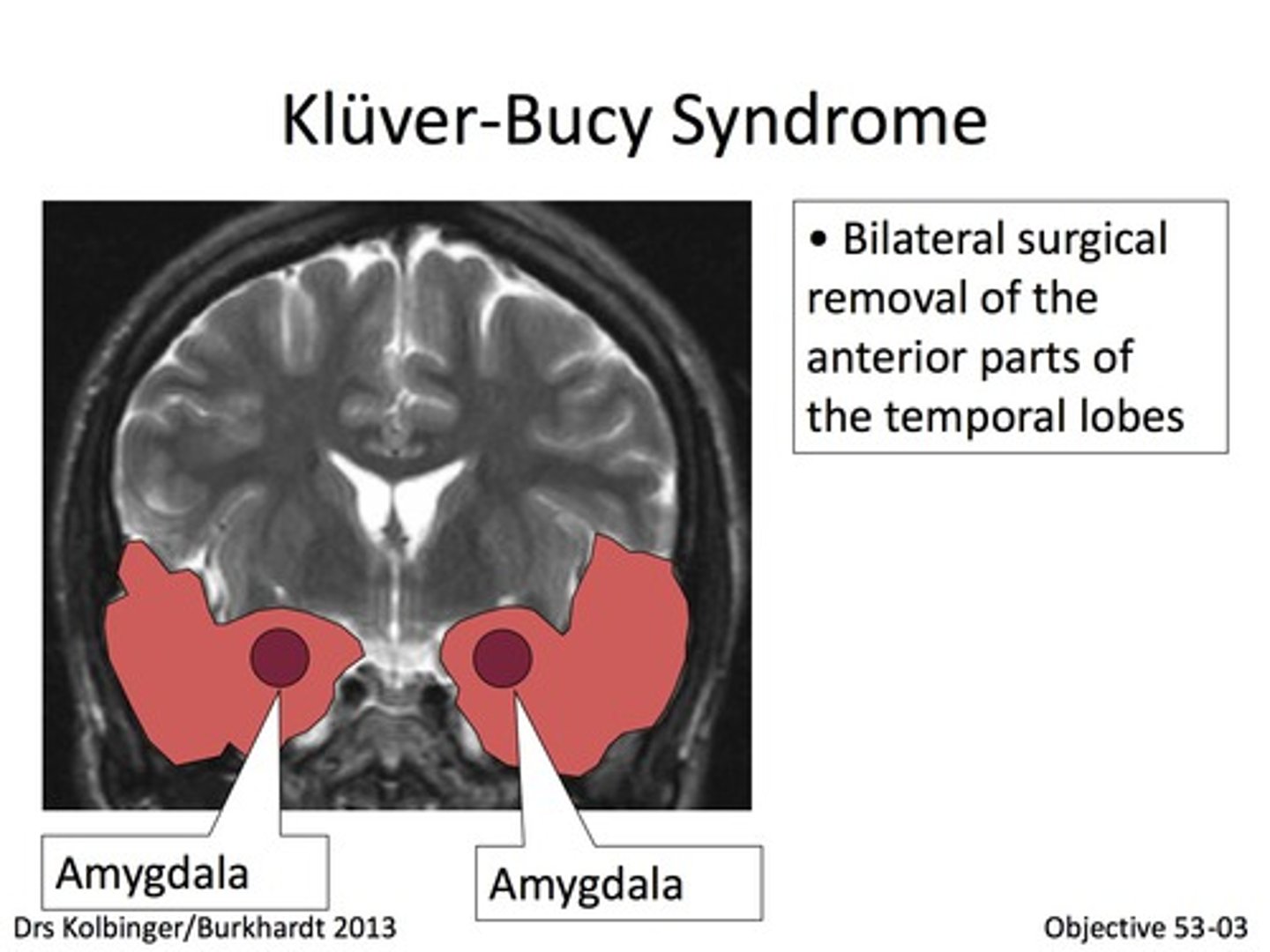
Cause of Kluver-Bucy syndrome
bilateral damage to amygdala & limbic-frontal connections
- affects our fear response
Hypermetamorphosis in Kluver-Bucy syndrome
hyperreactive to whats in the environment; everything is salient/important!
Following a head injury, a patient complains of problems with his sense of smell & is described as reckless and impulsive. What area of his brain is damaged?
a) dorsolateral PFC
b) orbitofrontal cortex
c) medial frontal cortex
d) none of the above
b) orbitofrontal cortex
- lack of impulse control
- innapropriate social behavior
- laughing at funerals
- orbitofrontal cortex is close to olfactory system
A patient with working memory problems and perseveration on tasks has damage to what brain region?
a) dorsolateral PFC
b) medial frontal cortex
c) orbitofrontal cortex
d) none of the above
a) dorsolateral PFC
- loss of executive function
- inability to change tasks
- impaired working memory
Schizophrenia
a psychological disorder characterized by positive, negative, & cognitive symptoms
- mind is split from reality

Positive Schizophrenia symptoms
additions to normal cognition/function
- hallucinations: experiencing sensory input that is not actually there; smell, sight, hearing
- delusions: irrational belief; thought disorder
- disorganized speech/thought: fueled by delusions; hard to maintain clear/consistent thought
Negative Schizophrenia symptoms
loss of normal cognition/function
- flat affect: low mood
- poverty of speech: limited production of speech
- lack of motivation: impacts speech, taking care of oneself, etc.
