L27 Pain (Imported from Quizlet)
1/82
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
83 Terms
Diabetes mellitus and leprosy
Loss of pain sensation (due to nerve damage) is a feature of what?
They are unaware of minor injuries
What does an absence of pain mean for a person?
Because it is both a discriminative sensation and a graded motivation (or behavioural drive)
Pain differs from the classical senses (vision, hearing, touch, taste and smell) - why?
Allodynia, referral, temporal augmentation, after-sensations, emotional, hyperpathia
Pain is a leading clinical complain that can present mystifying symptoms, such as: __________ (sensitisation to normally innocuous stimuli), _______ from deep tissue to skin, radiation over wide regions, _________ ______________ ("windup"), persistent ______-___________, __________ variability and ____________ (hysterical responses)
Intensity
Pain can attain intolerable ____________ but it can disappear in the heat of battle
Psychic suffering of any sort
Pain is a universal human experience that is commonly generalised to ...?
Pain is a distinct sensation, detected and transmitted by specific receptors and pathways to distinct "pain areas" of the brain
What is the specificity theory?
Pain is an integrated, plastic state represented by a pattern of convergent somatosensory activity within a distributed network (a so-called 'neuromatrix')
What is the convergency theory?
Complex interactions between a number of brain areas
What is pain perception dependent on?
Activating stimulus, fibre-type and conducting velocity
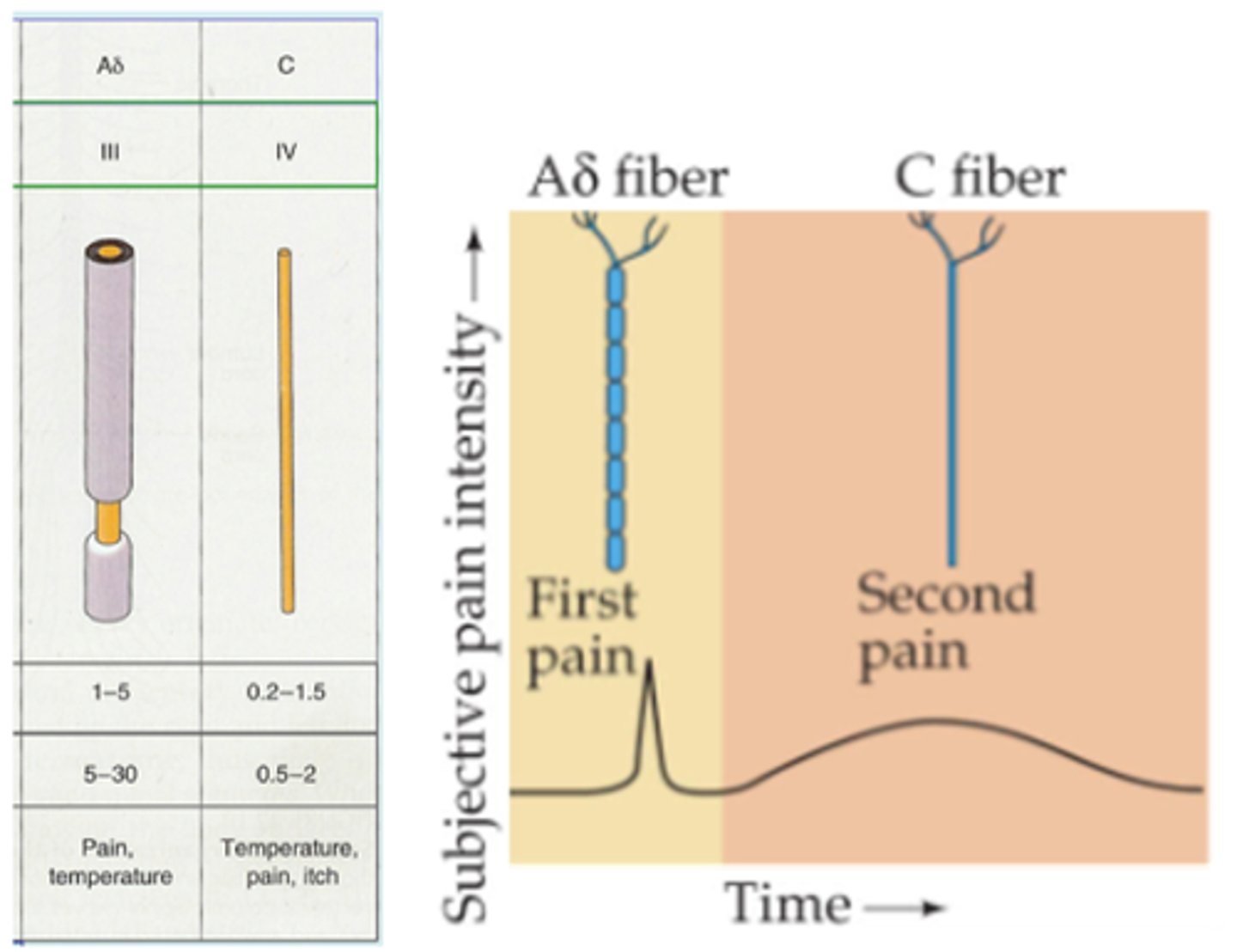
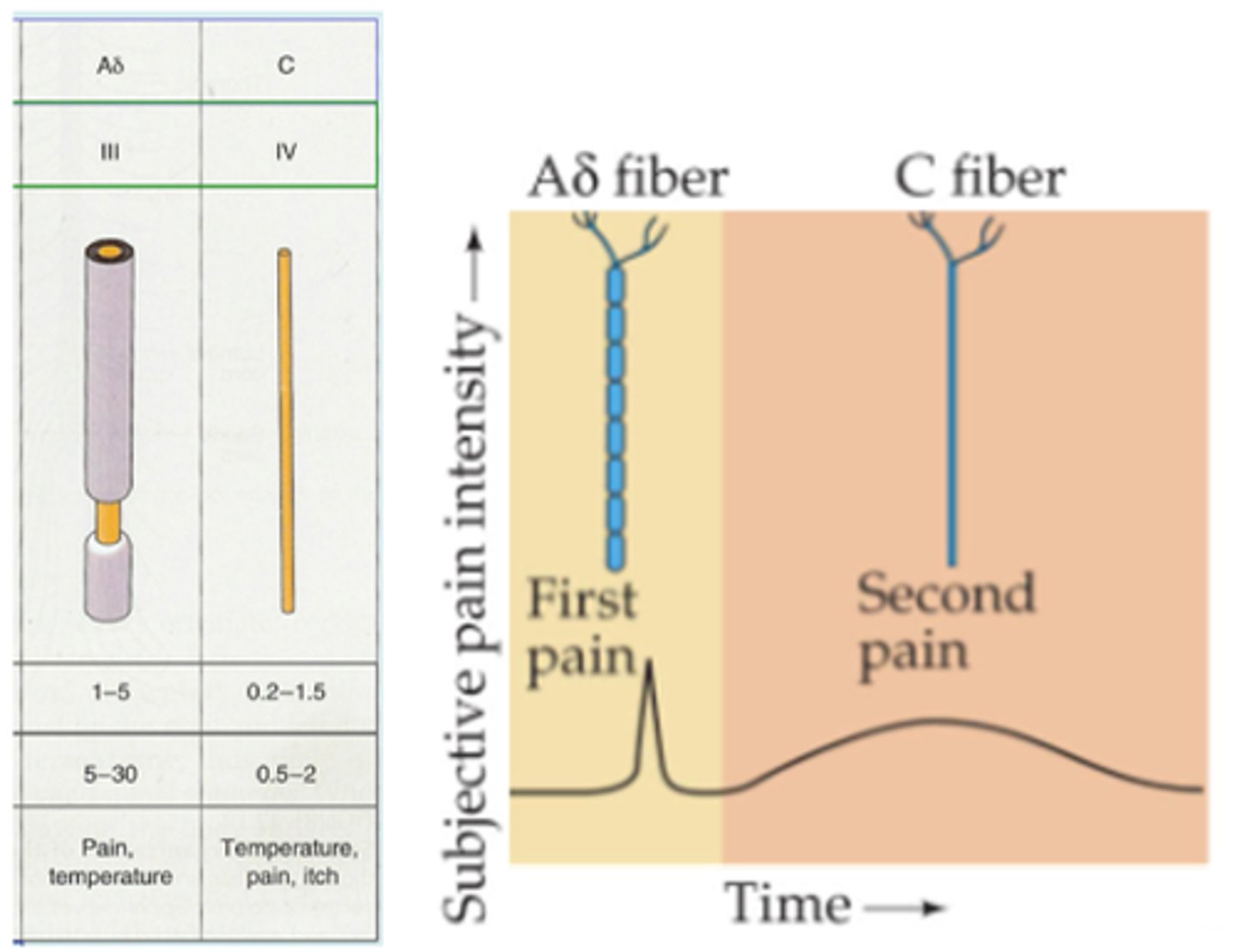
Afferents with free nerve endings are classified according to what 3 things?
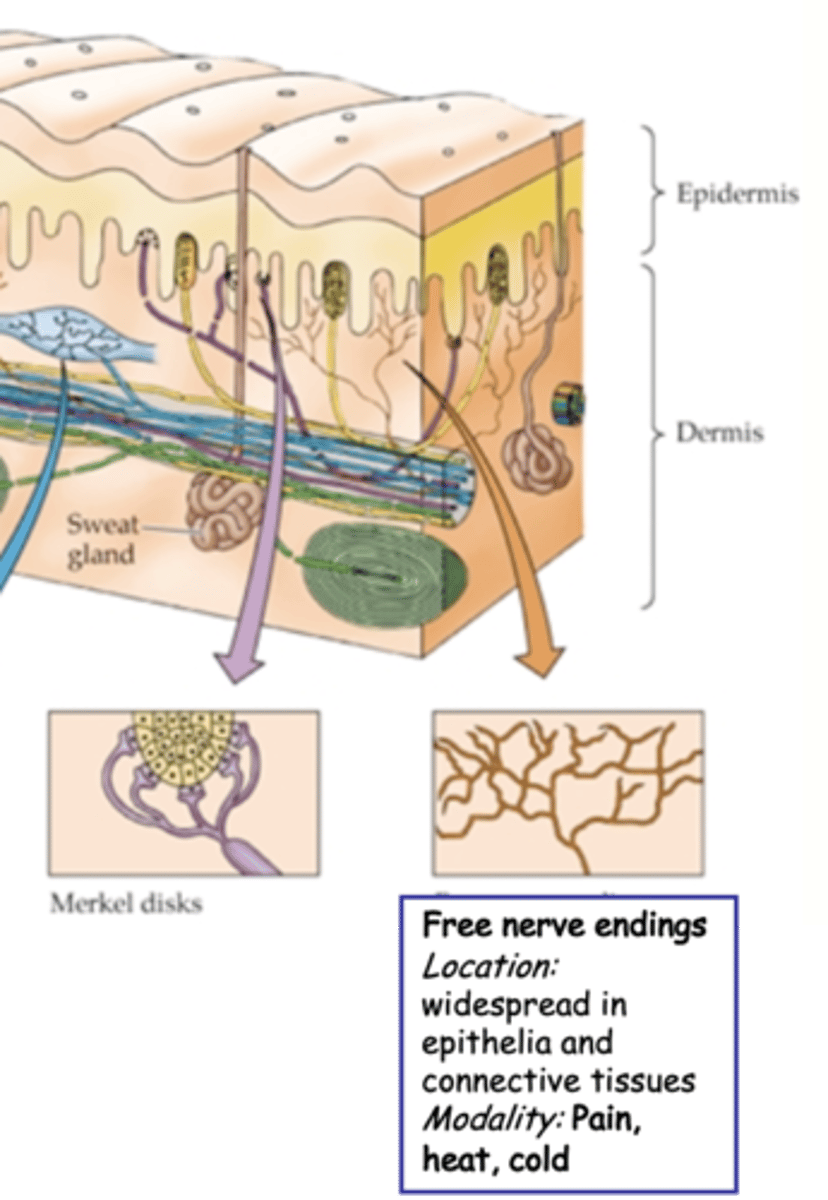
Aδ, 20, sensitive, thermal
(Afferents with free nerve endings) Lightly myelinated ___ fibres are fast ~__m/s (relatively fast but still much slower than proprioceptors)
-> Mechano-____________
-> Mechano_________-sensitive
C, 2, polymodal
(Afferents with free nerve endings) Unmyelinated _ fibres, slow ~_m/s
-> _____________: mechanical, thermal and chemical
Pain, afferents, free nerve endings
Nociceptors respond specifically to ______ and are a subset of ___________ with _____ _______ ___________
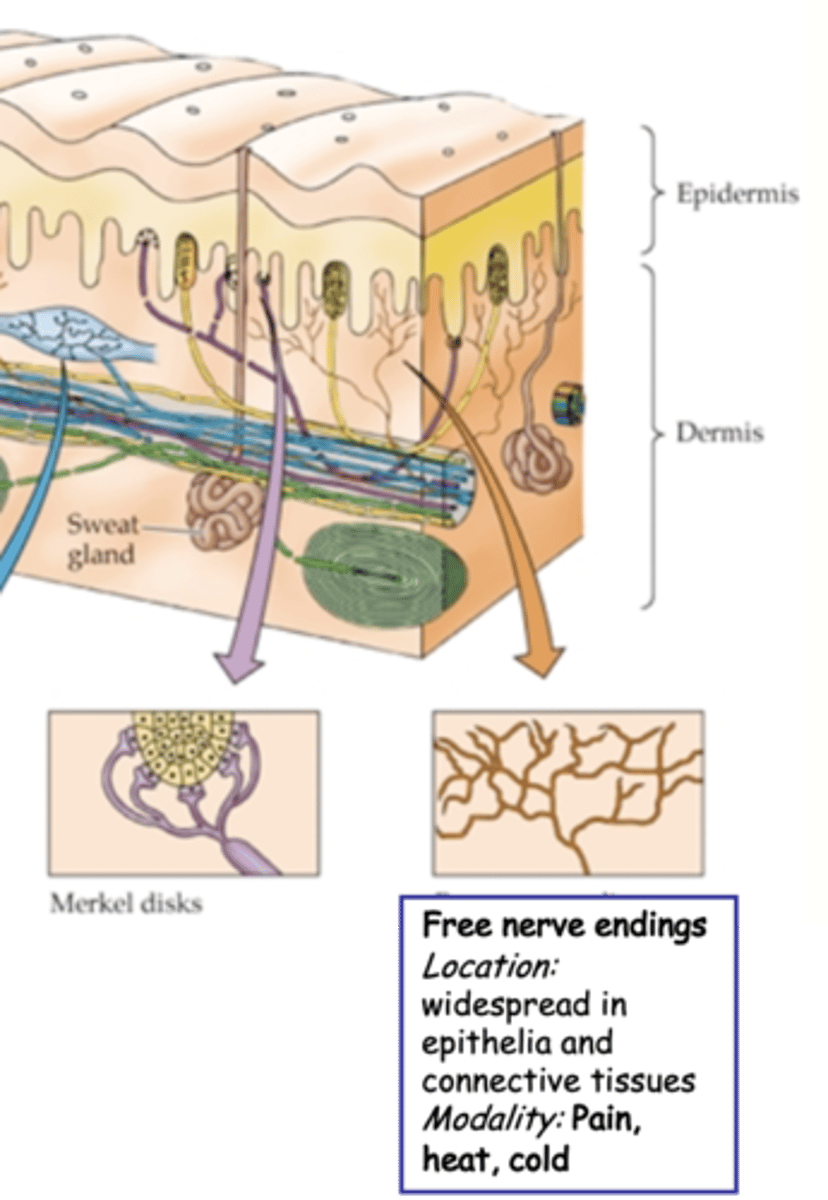
Heat, pain perception
Nociceptors are most easily demonstrated for ______ responses
I.e. can find afferents whose activity correlated with ______ _____________
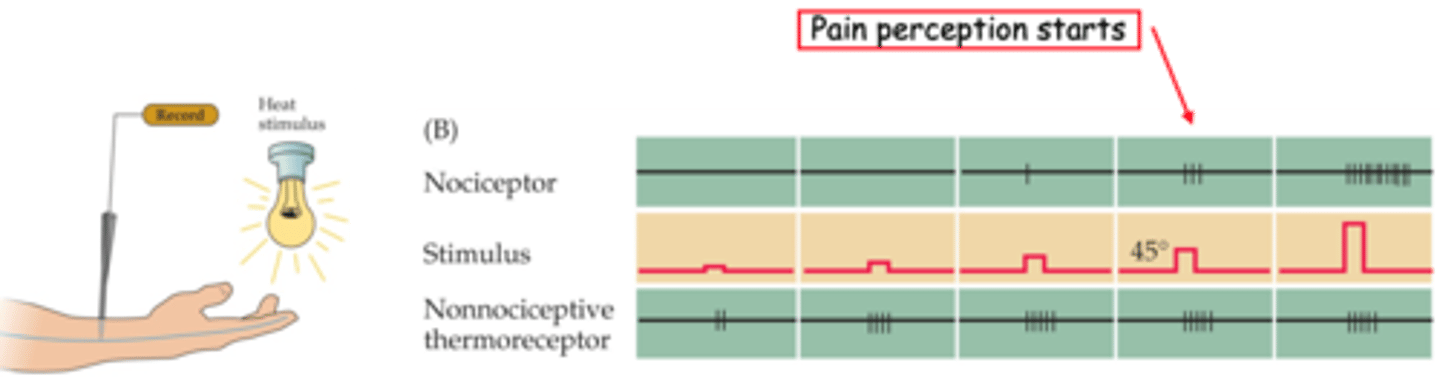
Saturated, ramping up
It is clear that thermoreceptor activation has already __________ before pain is perceived - i.e. pain is not due to _________ ___ of normal receptors
Fast and slow pain
What are the 2 categories of pain mediated by different fibre types?
Sharp and immediate; can be mimicked by direct stimulation of Aδ fibre nociceptors
Describe fast or 'first' pain
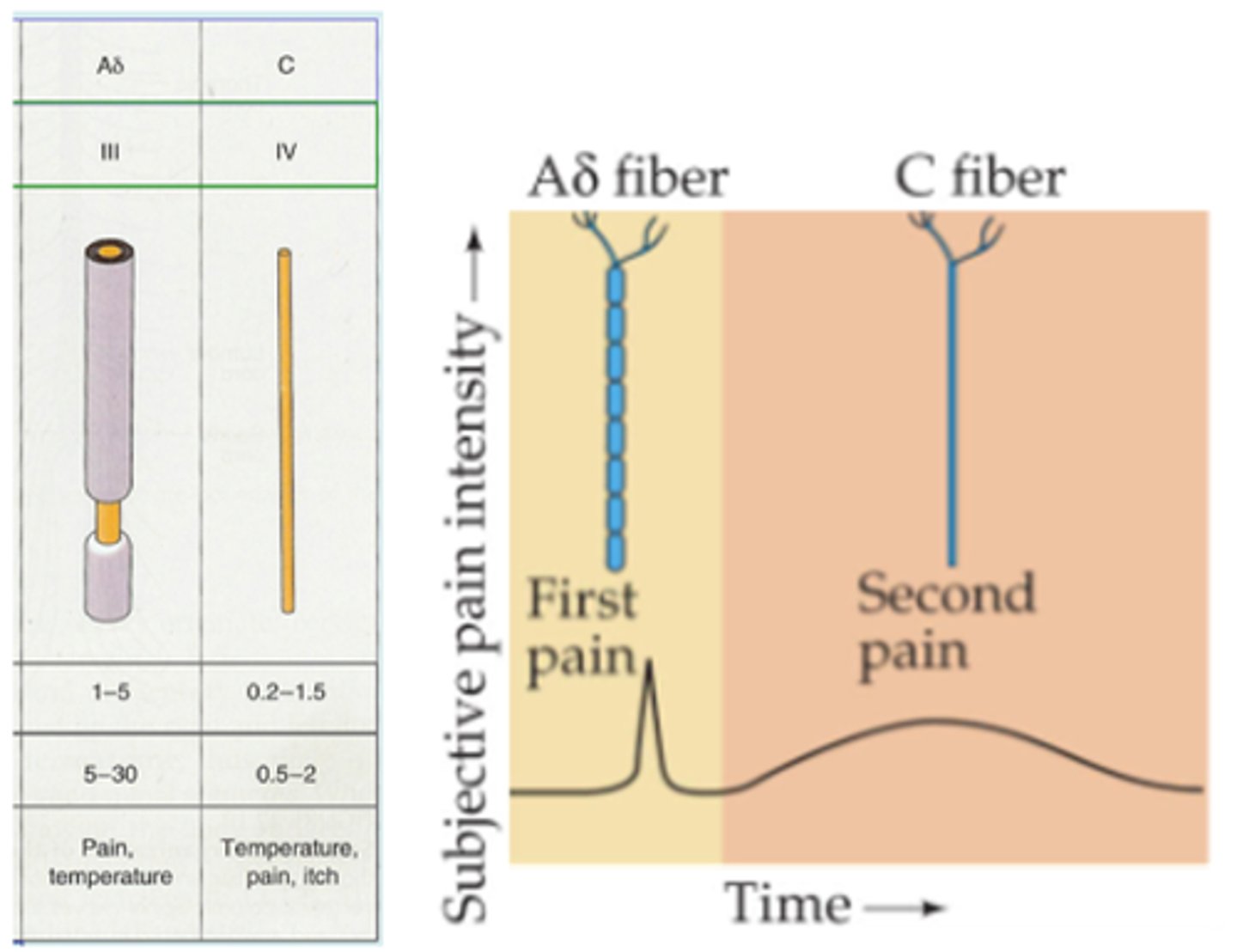
More delayed, diffuse and longer-lasting; mimicked by stimulation of C fibre nociceptors
Describe slow or 'second' pain
By selectively blocking the fibres in turn
How can specificity be demonstrated experimentally?
α, β, never
Stimulation of A_ and B_ (proprioceptive and mechnorecptive) fibres ______ elicits the pain sensation
Heat
Specific molecular receptors associated with nociceptive nerve endings are activated by what?
Capsaicin, Aδ, C, 45
The _________ receptor (TRPV1) is activated in nociceptive __ and _ fibres at __°C and by __________ (a vanilloid which is the active component in chilis)
Aδ, 52
Related receptors (other TRPs) are activated in __ fibres alone at even higher thresholds (__°C)
Heat-detection machines
These molecular receptors are known to respond directly to heat - they themselves are the ...?
Endogenous vanilloids released by stressed tissues
What is capsaicin thought to mimic?
Transient receptor potential protein family
What does TRPs stand for?
Release, chemicals
Nociceptors may also work by detecting __________ of __________ from stressed cells
Sensory discriminative and affective-motivational
Pathways carrying nociceptive information to the brain are complex, what are the 2 components?
Location, intensity and type of stimulus
What does sensory discriminative signal?
'Unpleasantness' and enables autonomic activation, classic fight or flight response
What does the affective-motivational signal?
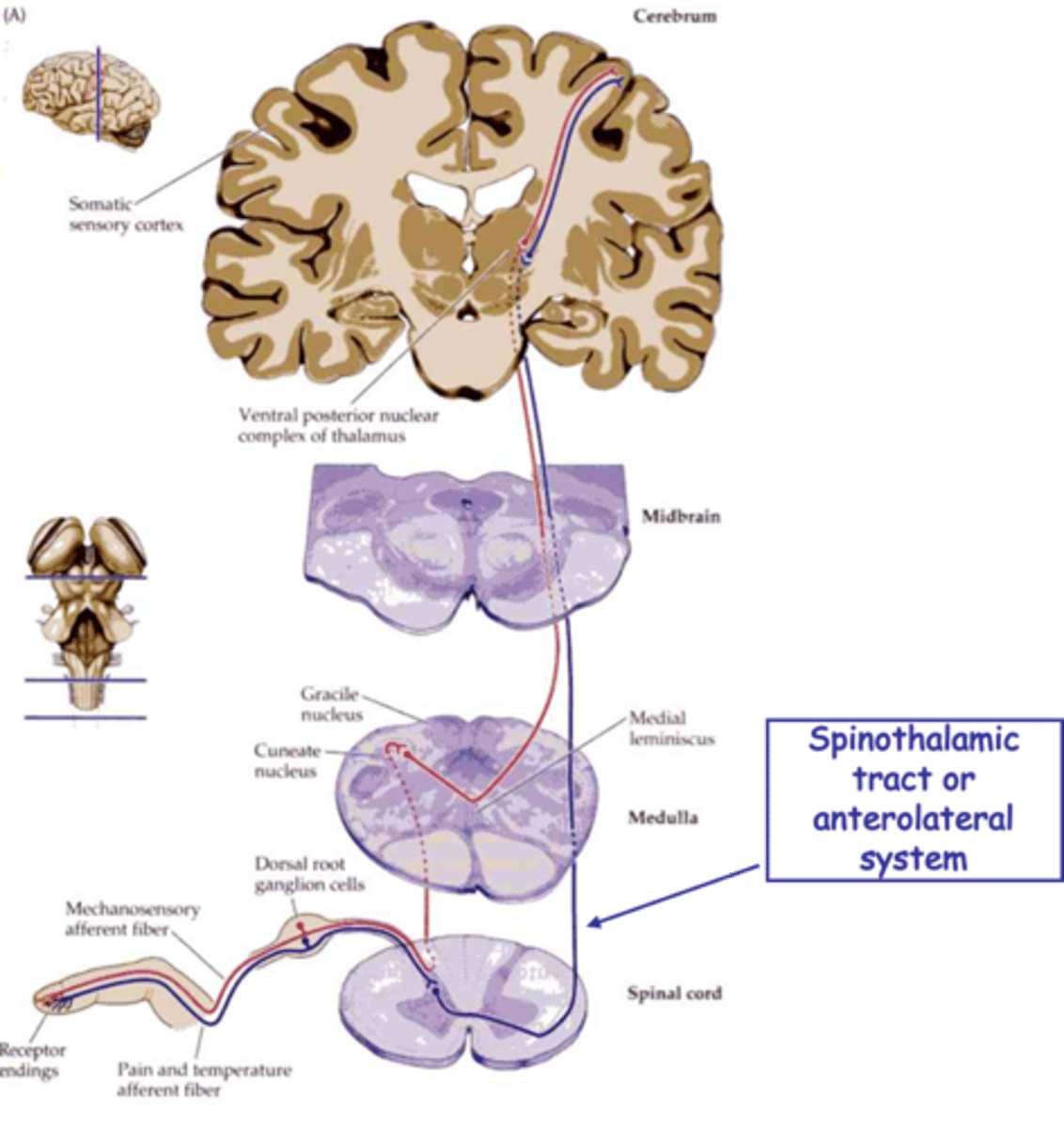
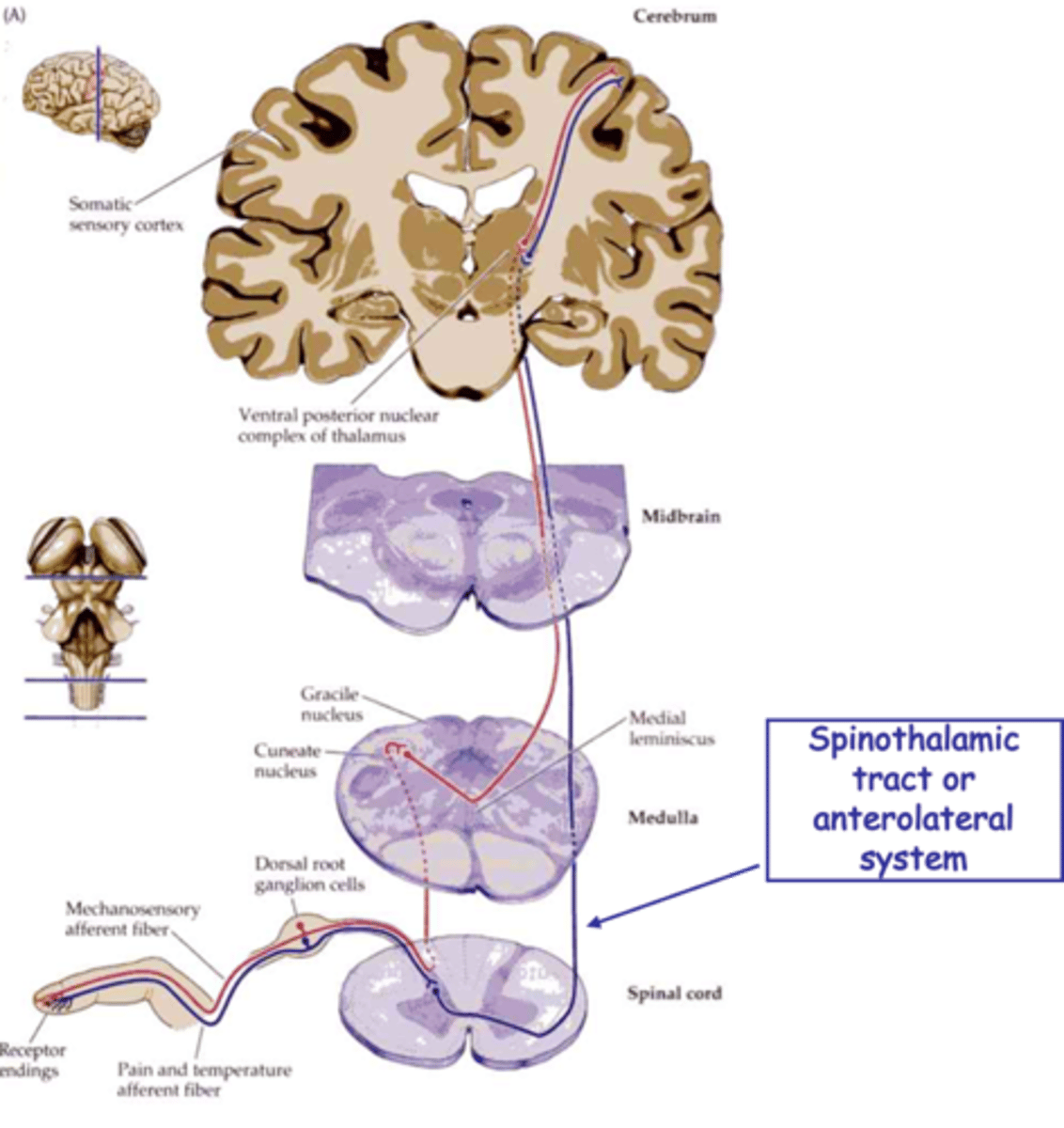
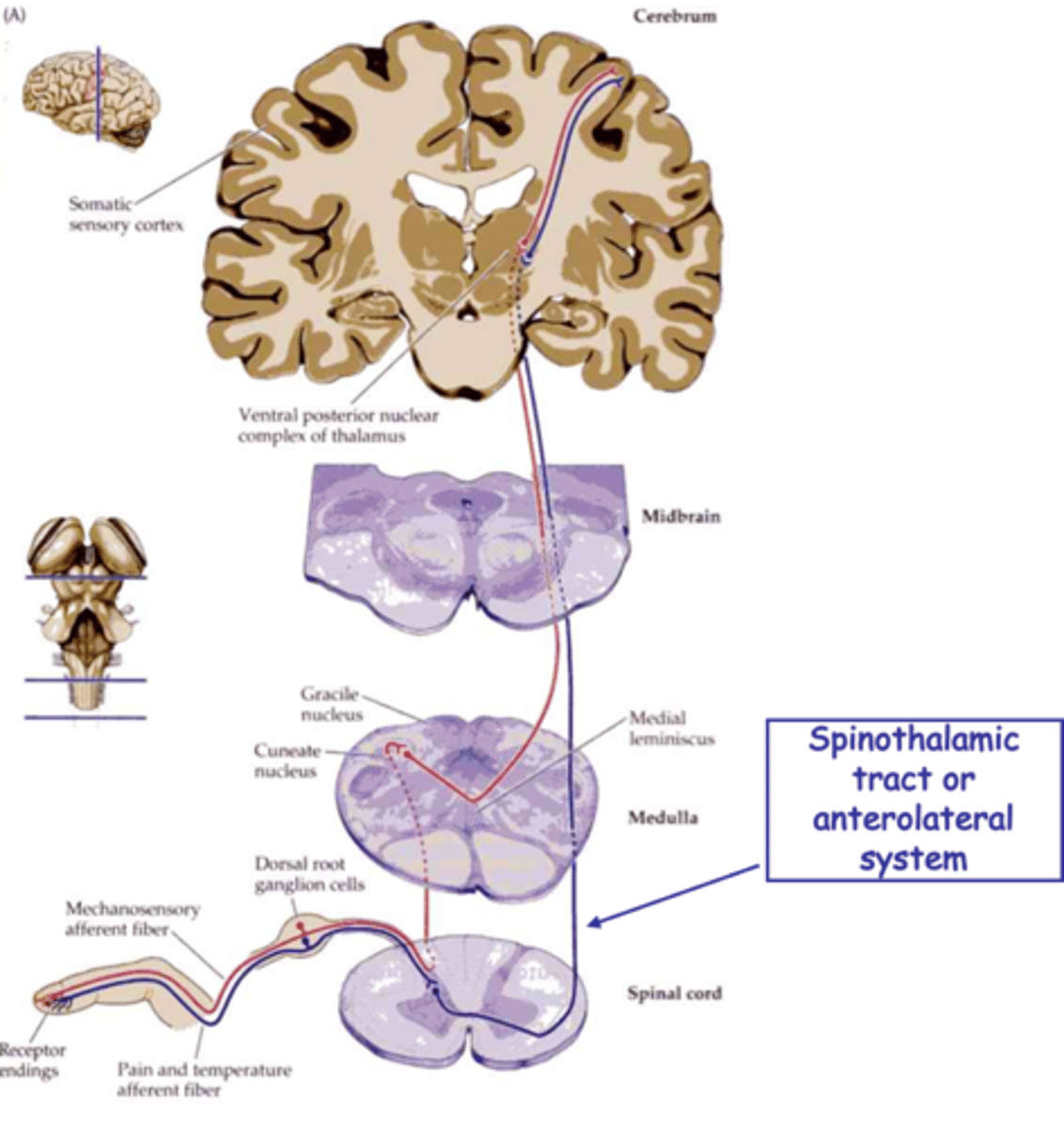
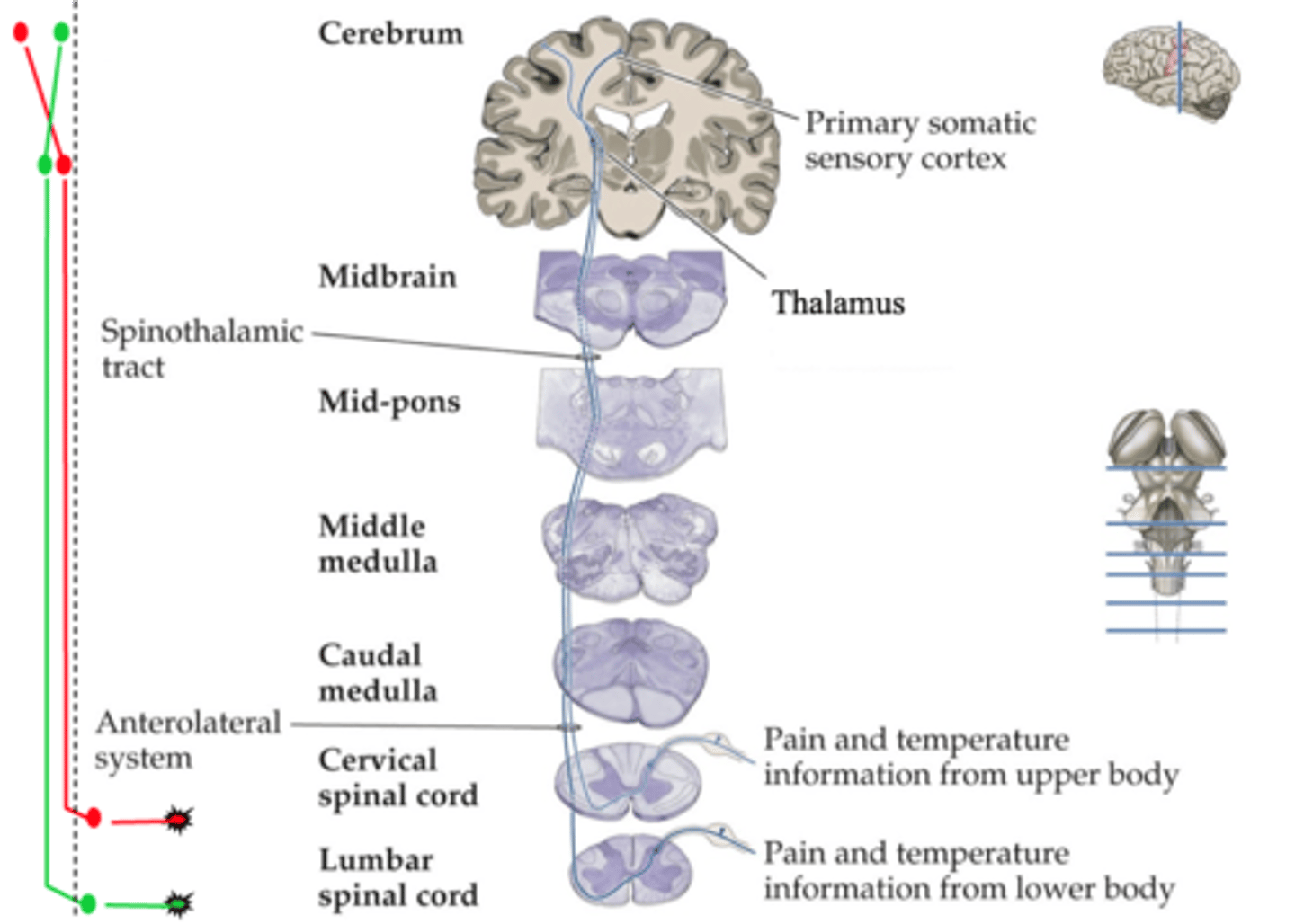
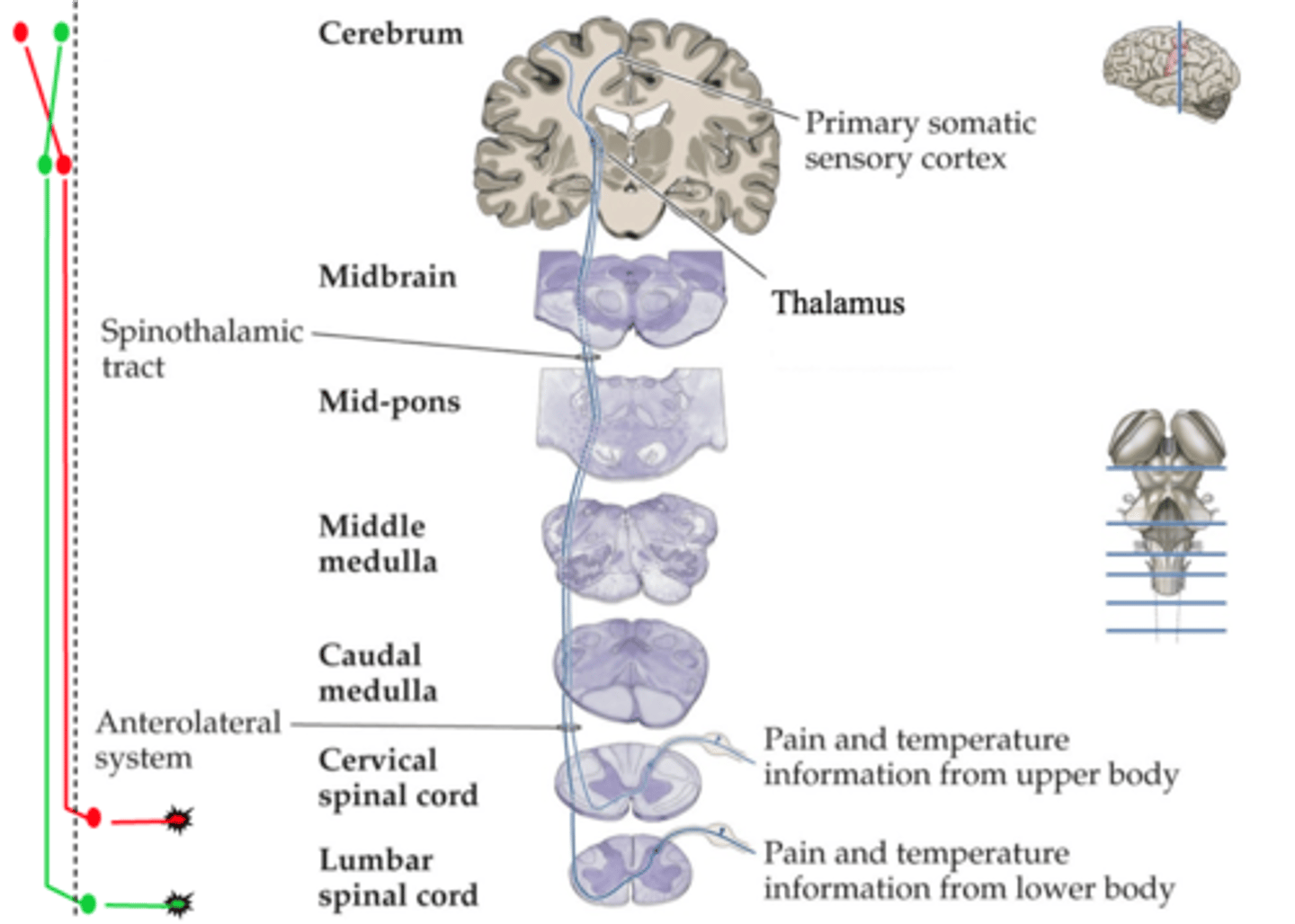
Spinothalamic tract
The discriminative pathway is easiest to define and involves the _________________ _______ which is also called the anterolateral system
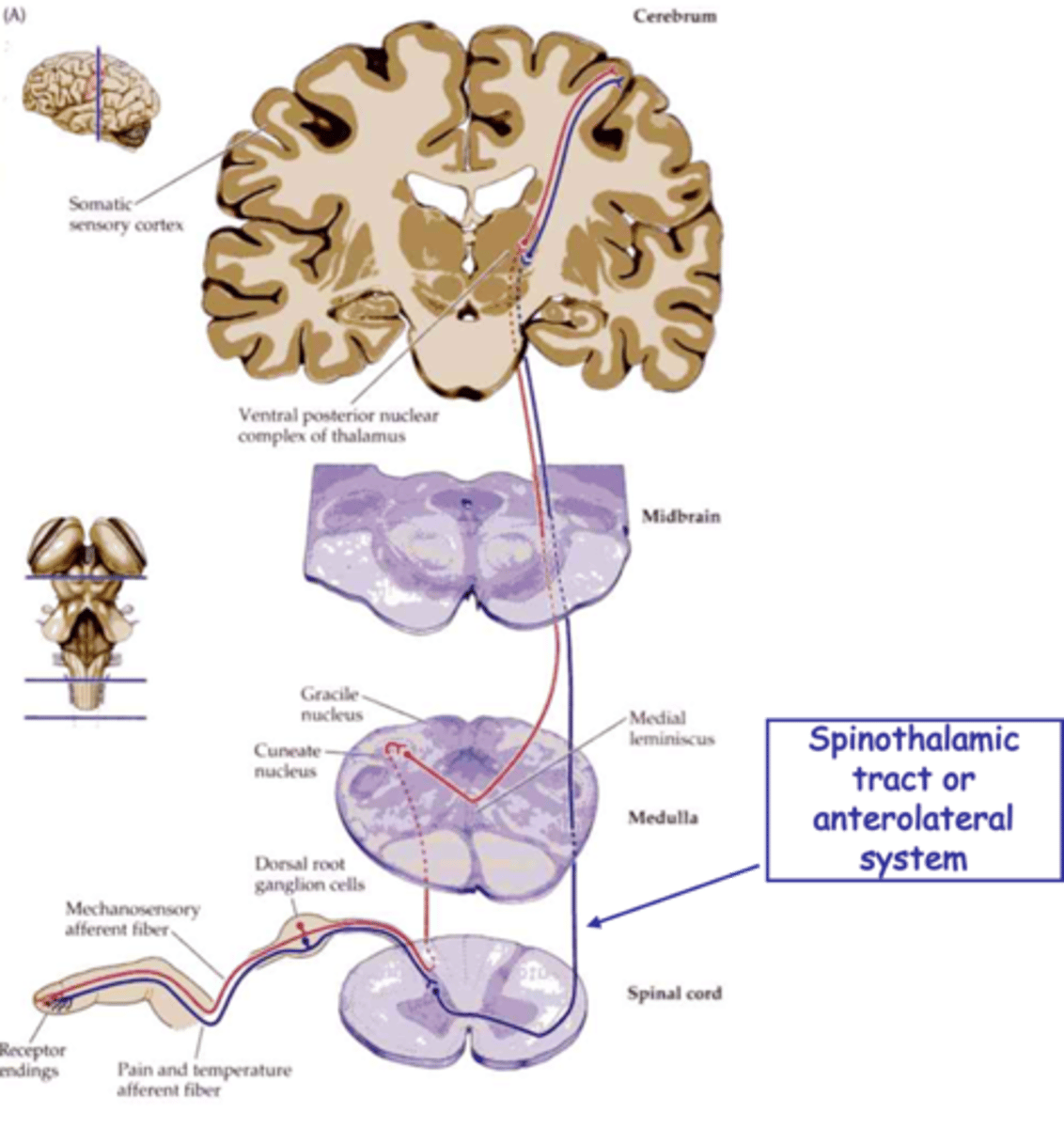
Topology
What do spinothalamic projections preserve?
That this region does indeed respond to painful stimuli and that response correlated to intensity of pain
That this is spatially mapped can be shown experimentally
What 2 things does measurement of activity in the somatosensory cortex indicate?
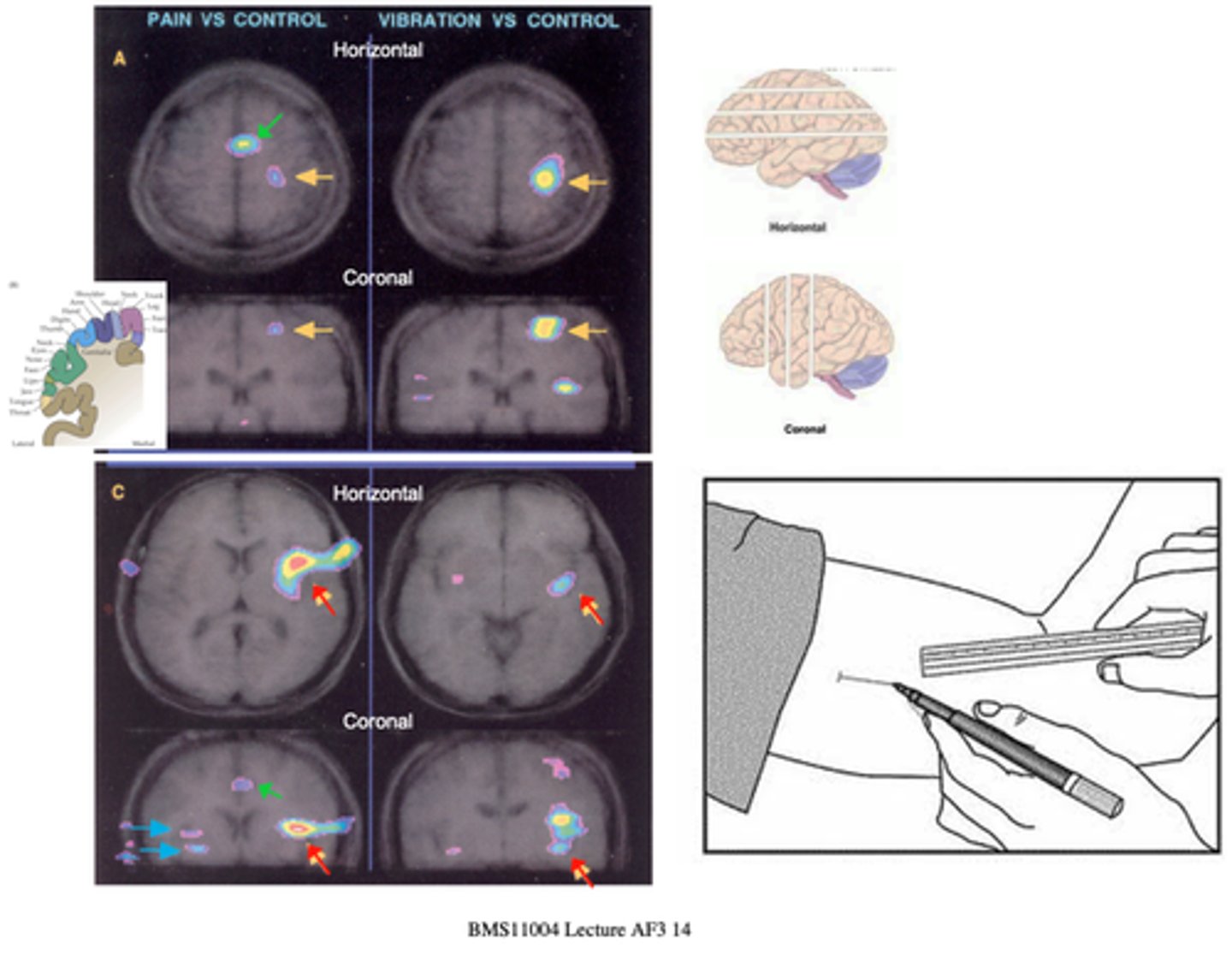
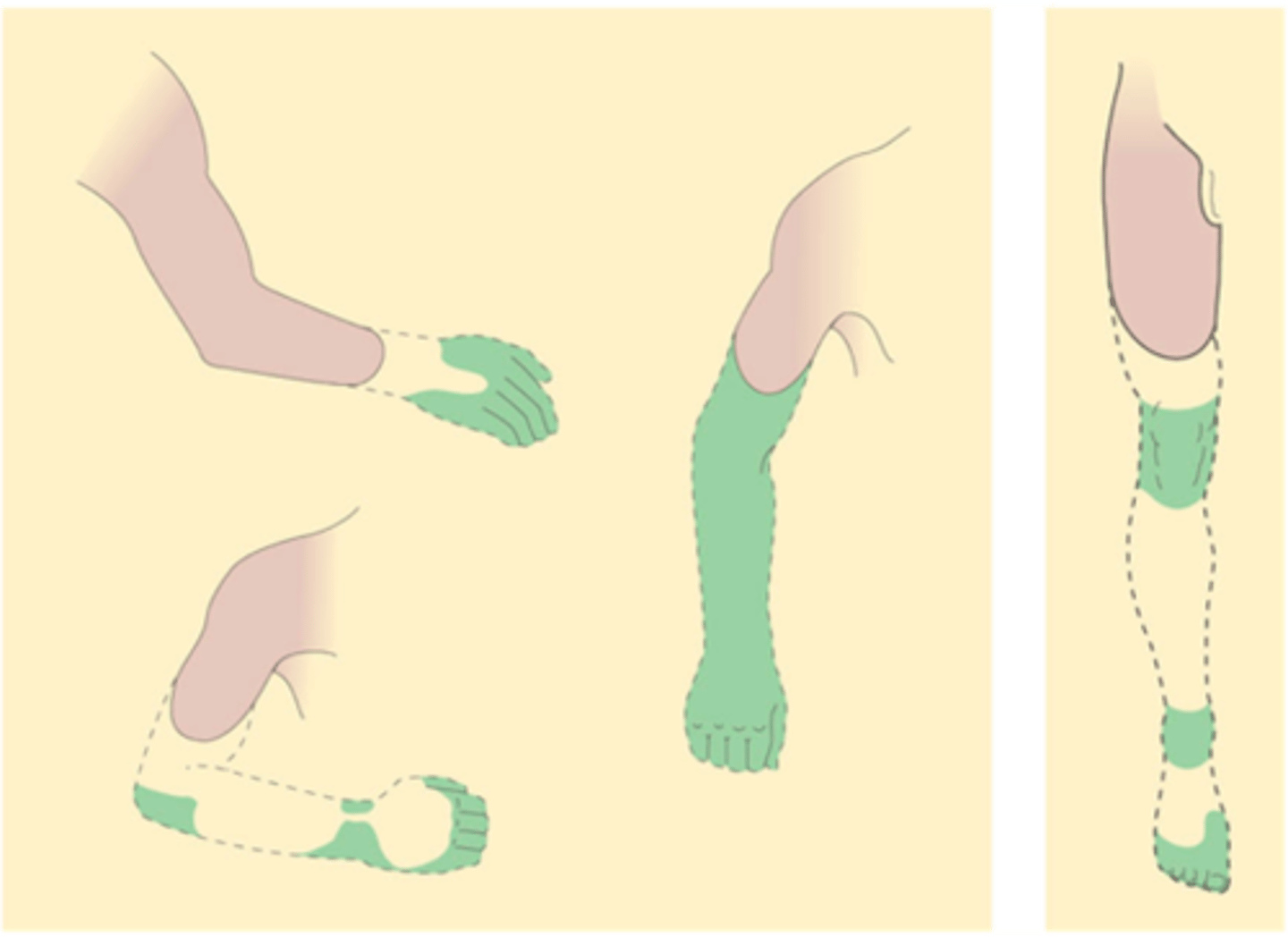
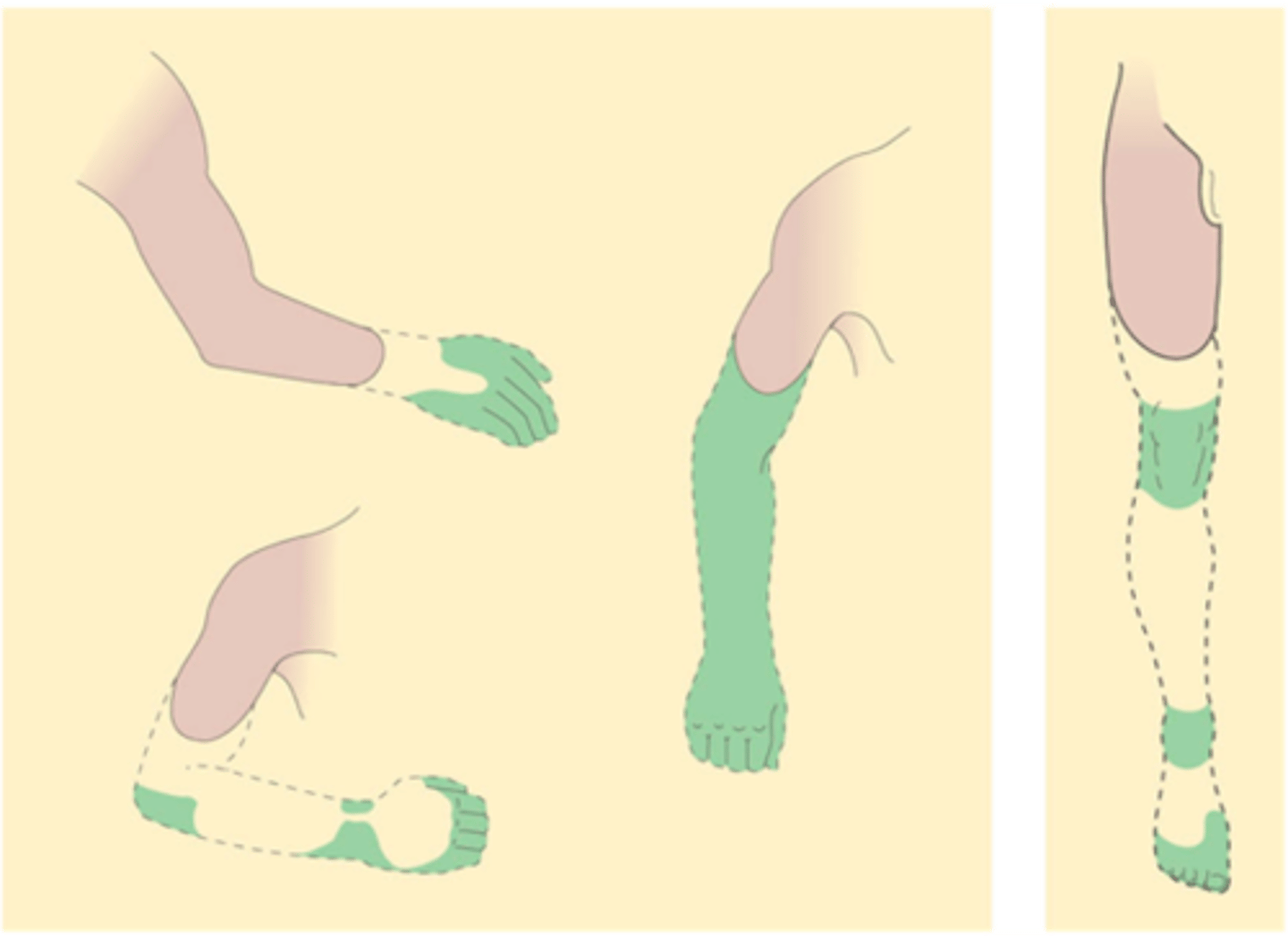
Somatosensory mapping for pain
What does the top panel show?
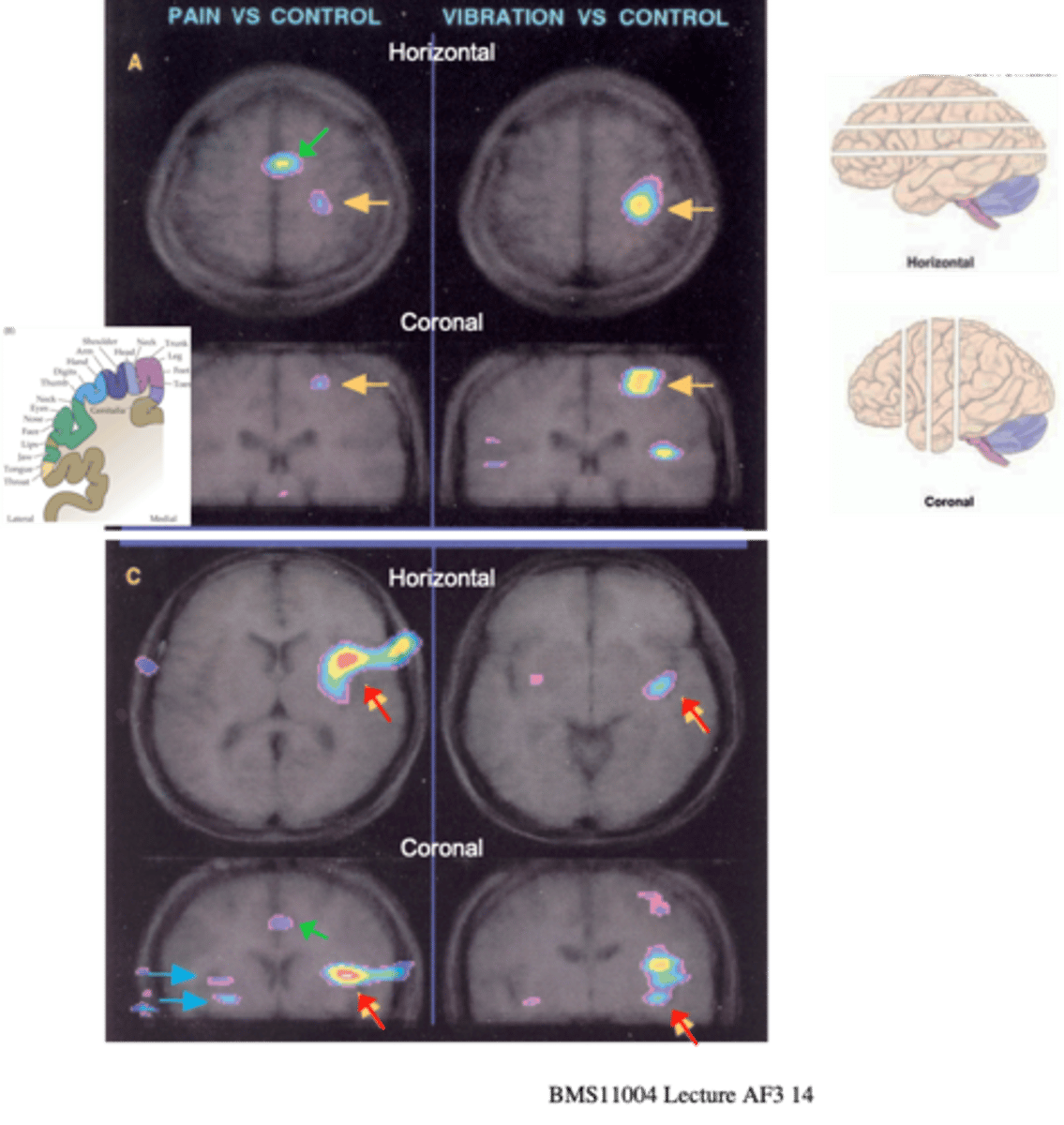
Other regions activated
What does the bottom panel show?
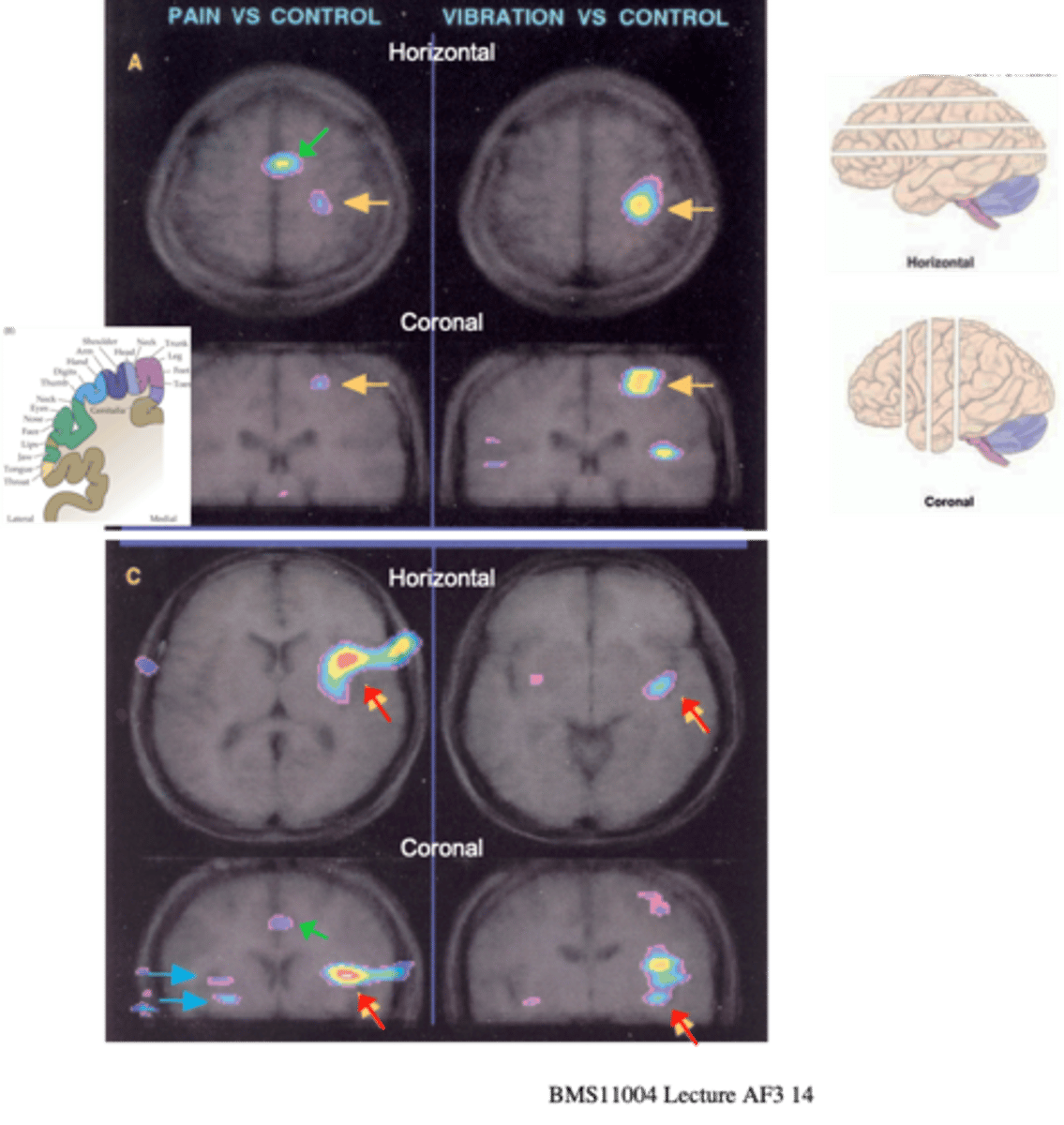
That painful stimuli activate the same region of the somatosensory cortex as the non-painful mechanical stimulation applied to the same region of skin (yellow arrows in A)
What does comparison (MRI) of cortical activation by painful (C fibre) or innocuous mechanical (vibration: Aβ fibre) stimuli to skin demonstrate?
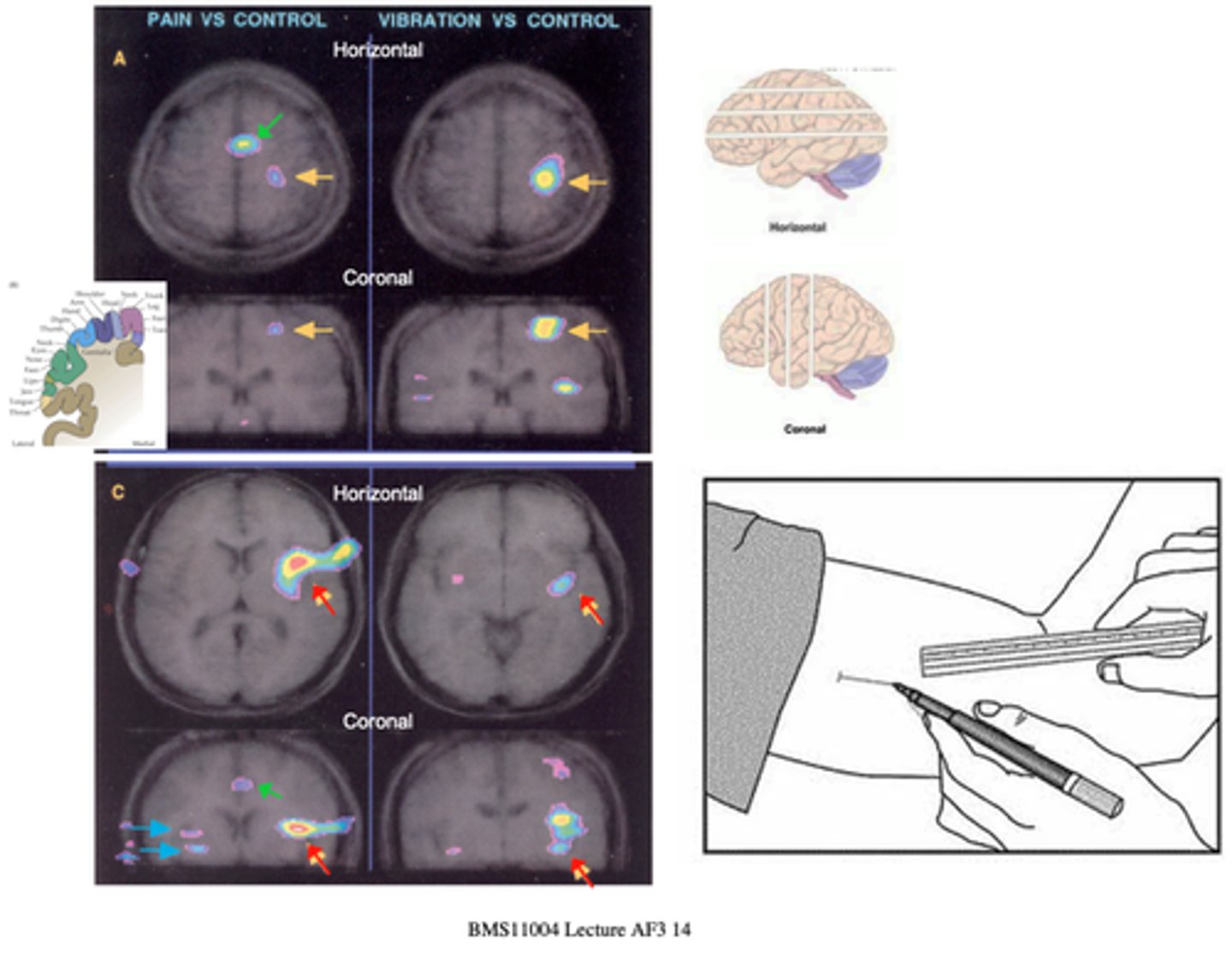
Connected to the limbic system and known to be involved in the activation of emotional responses
Pain activates a distinct response that includes other regions - notably is the activation of the insula (red) and the cingulate cortex (green), what are these regions connected to and involve?
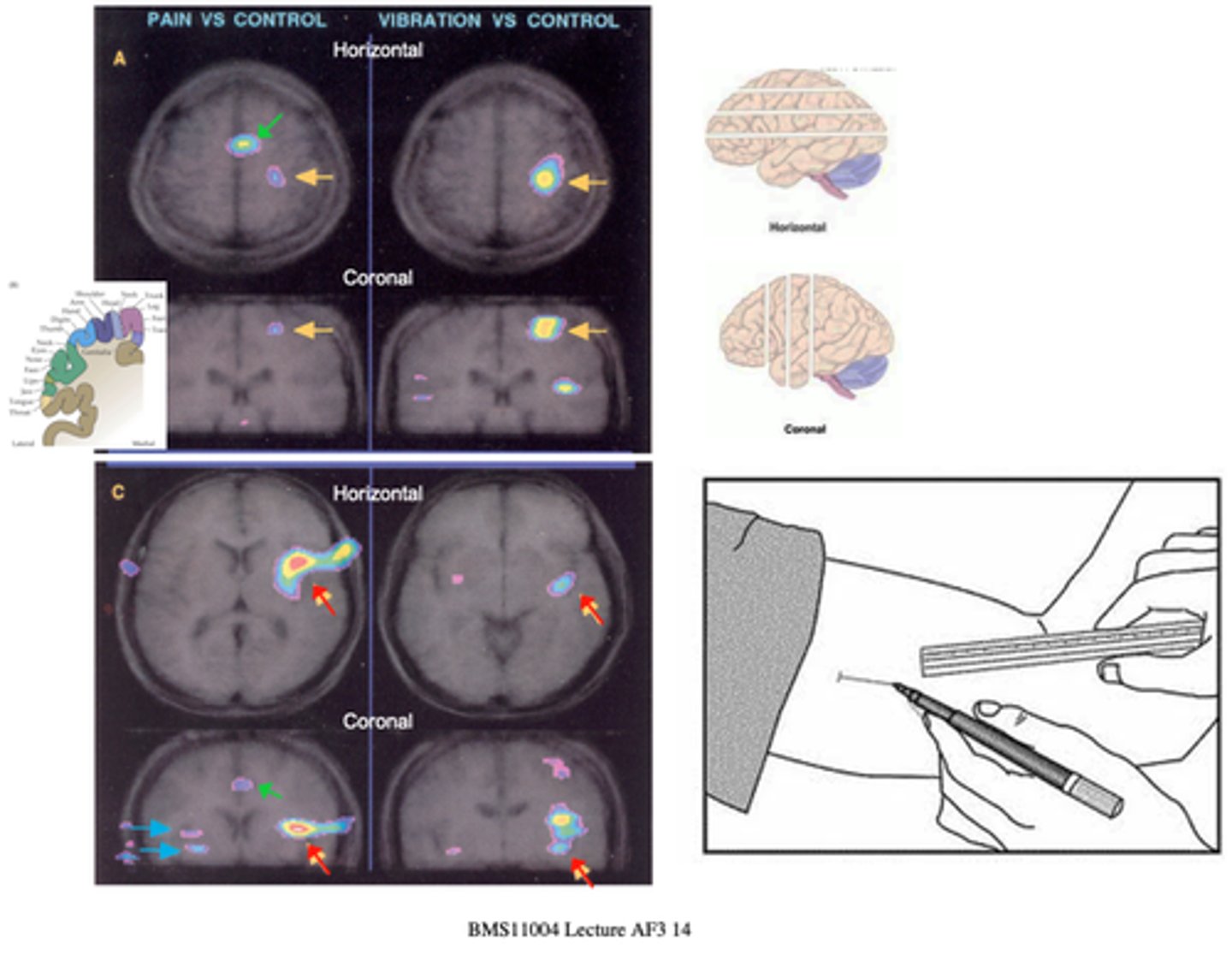
Affective-motivational
Which response to pain is this a part of?
Anterolateral
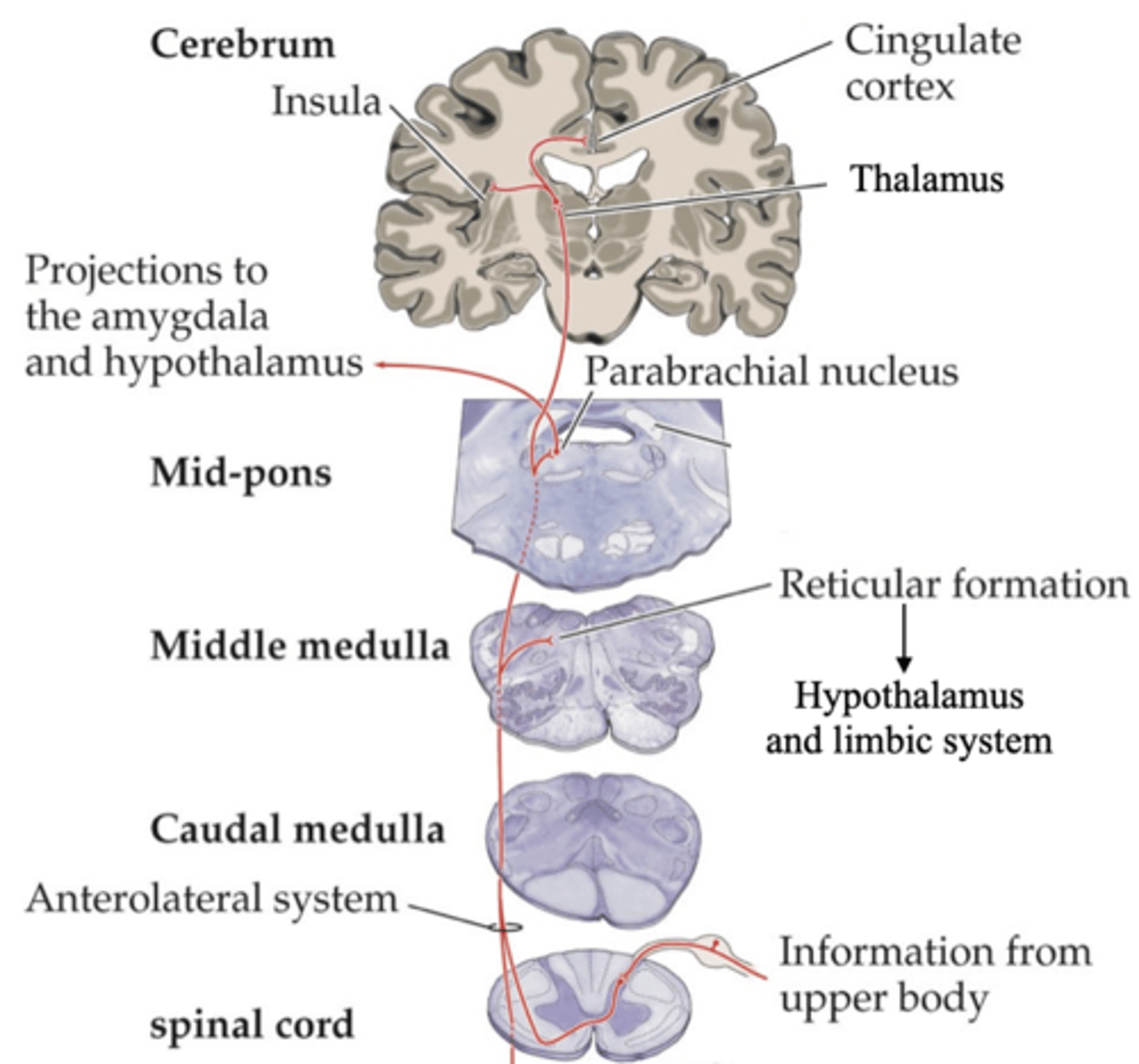
Affective-motivational pathways shares some paths with which system?
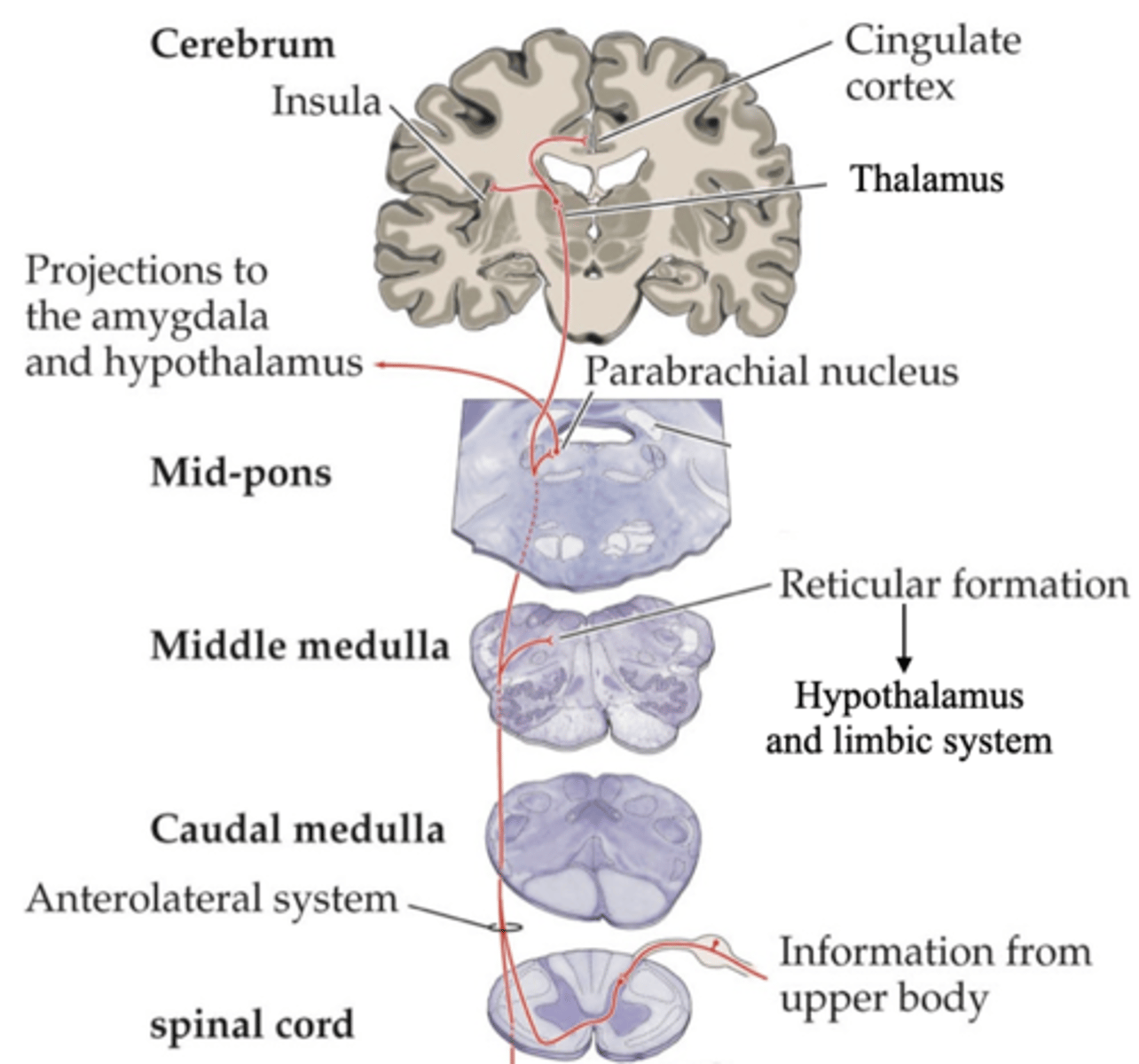
Parabrachial nucleus
There is little or no topographic mapping in affective-motivation pathways
-> Neurons in ____________ ________ can respond to painful stimuli from anywhere on the body's surface
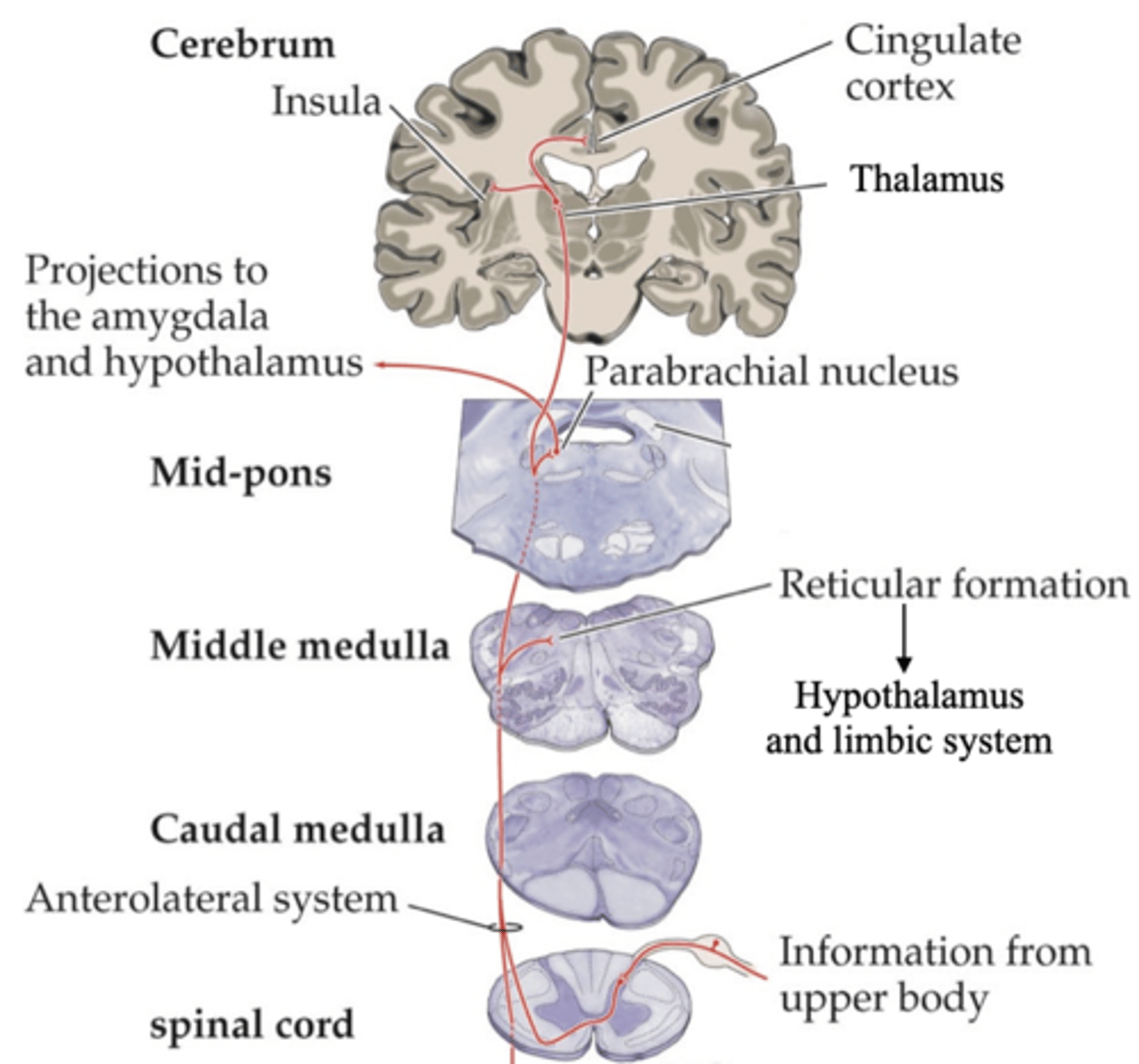
Emotional, homeostatic
Number of points of input to the ____________ (limbic) and _____________ (hypothalamic) systems
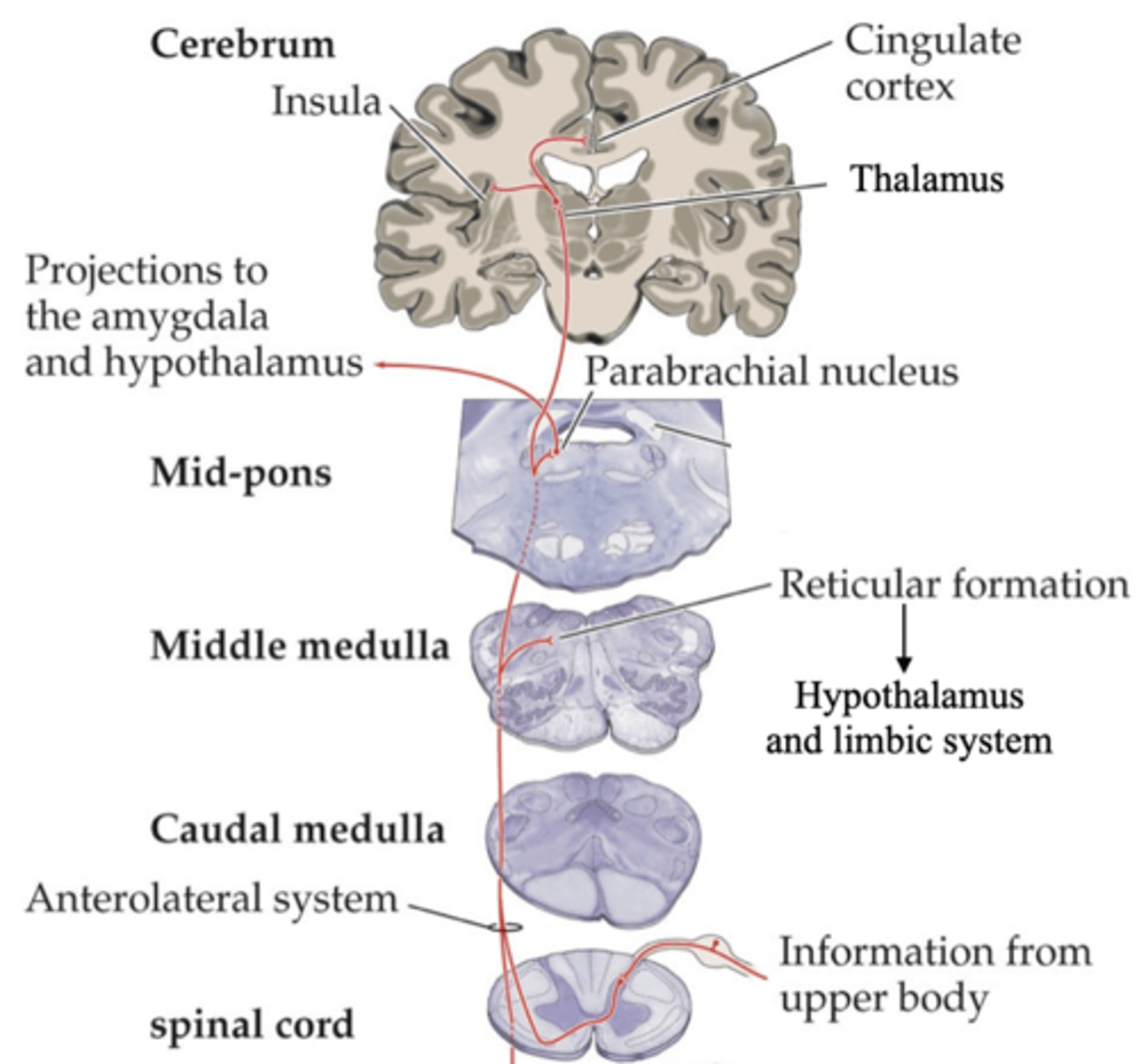
Cingulate cortex
Strong correlation of painful 'experience' (e.g. unpleasantness) with activity in ___________ ________

Somatosensory, discriminative
This is not the intensity of pain - intensity activates the _________________ cortex via the ______________ pathway
There are receptors, both cellular and molecular, that respond specifically to pain (a subset of Aδ and C fibres; TRPV1)
There are specific pathways that convey pain messages
There are regions of the CNS that are specifically and distinctly activated in response to pain
What are some tenets of the specificity theory that has been satisfied?
Pain perceived is not always proportional to intensity of stimulus
Modulation by other stimuli (e.g. acupuncture)
Perception of pain in severed limbs (phantom limbs)
Referral of pain from viscera to skin
Placebo effect
What are the phenomena that appear not to fit with the specificity theory?
Increased response to a painful stimulus (hypersensitivity of damaged skin to a normally tolerable painful stimulus e.g. light skin prick)
What is hyperalgesia?
Painful response to a normally innocuous stimulus (painful sensitivity of sunburnt skin to gentle mechanical stimulus (e.g. light brushing) or mild temperature)
What is allodynia?
Inflammatory substances, nerve, mast cells, neutrophils, blood flow
Peripherally, tissue damage releases a 'soup' of _______________ ___________ which affect _______ function, recruit ______ ______ and _____________ and increase local _______ _______
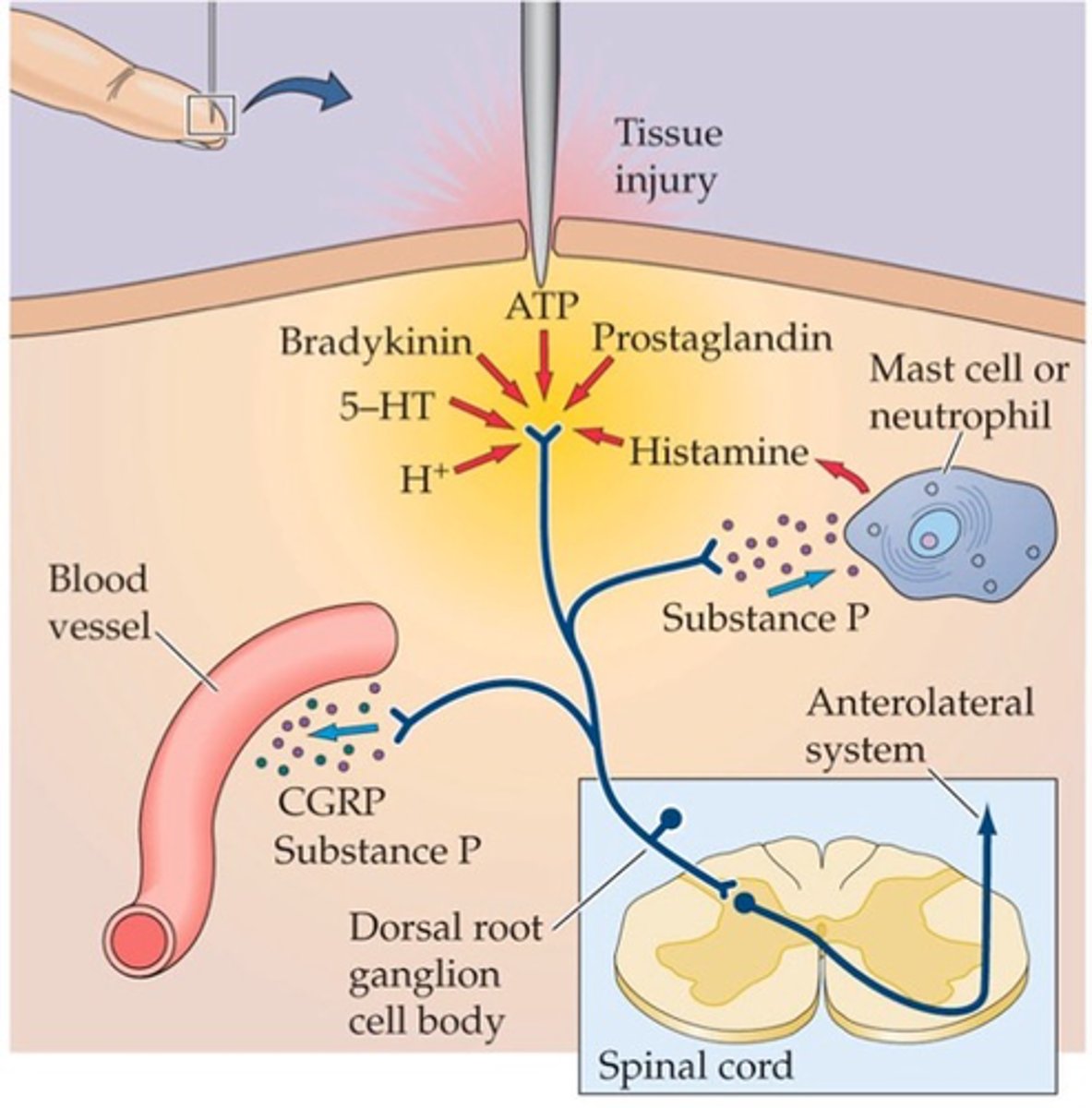
Directly affects the function of nociceptive molecular receptors such as TRPV1
What does bradykinin do?
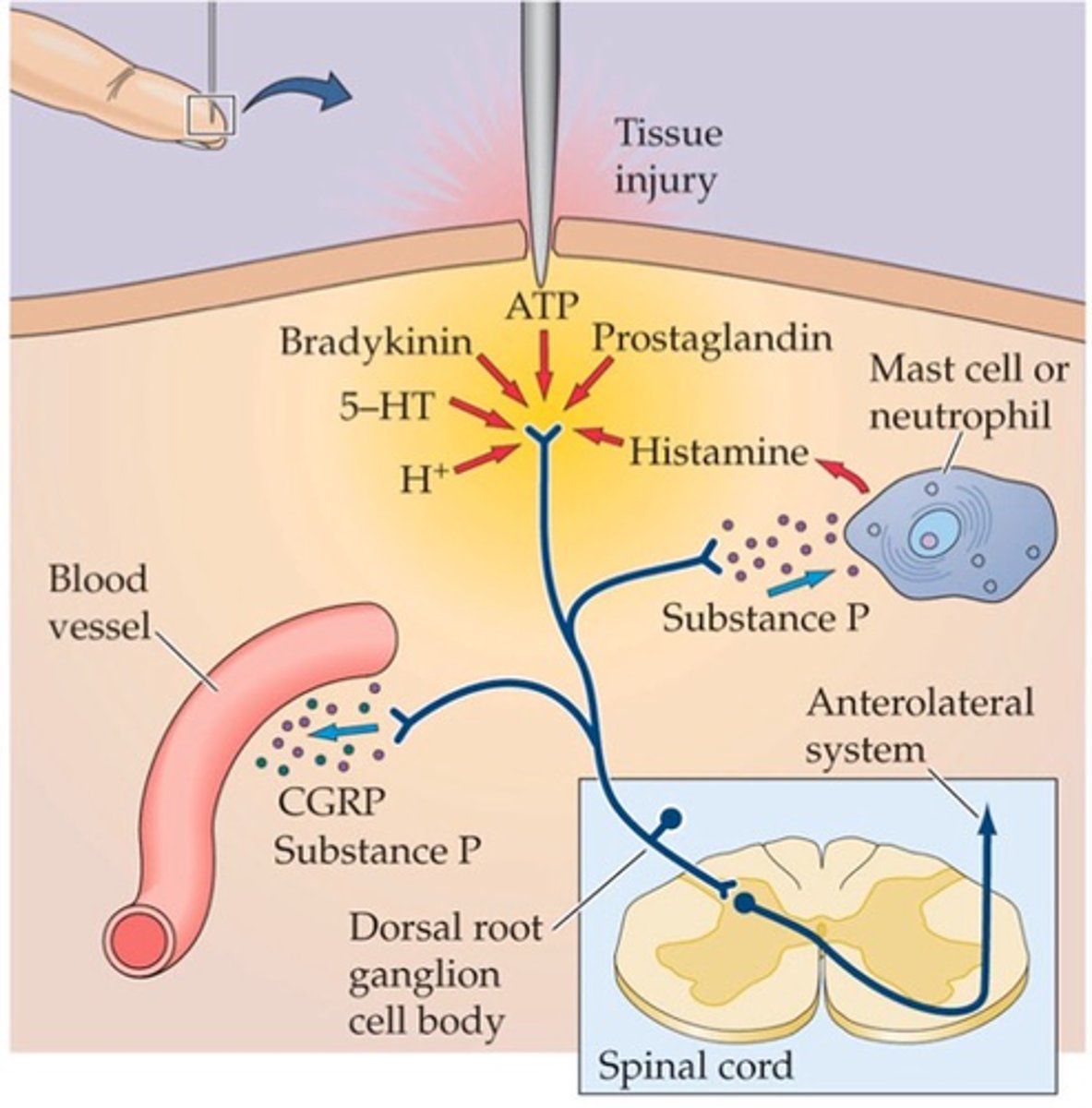
Lower the threshold for axon potential generation
What do prostaglandins do?
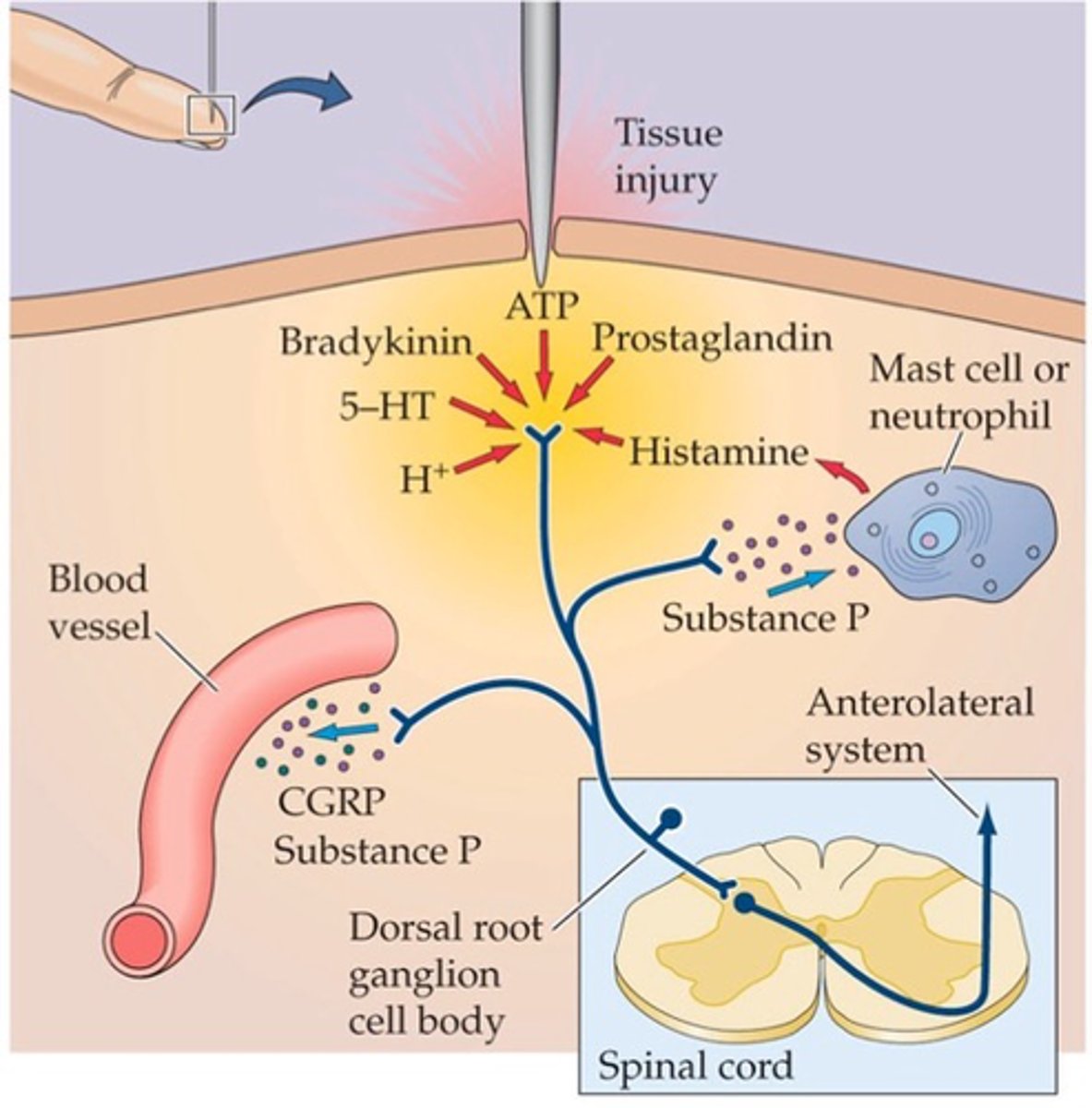
Analgesics, prostaglandin biosynthesis
Some painkillers (____________) notably aspirin and ibuprofen, act on cyclooxygenase (COX) an enzyme important in ________________ ______________
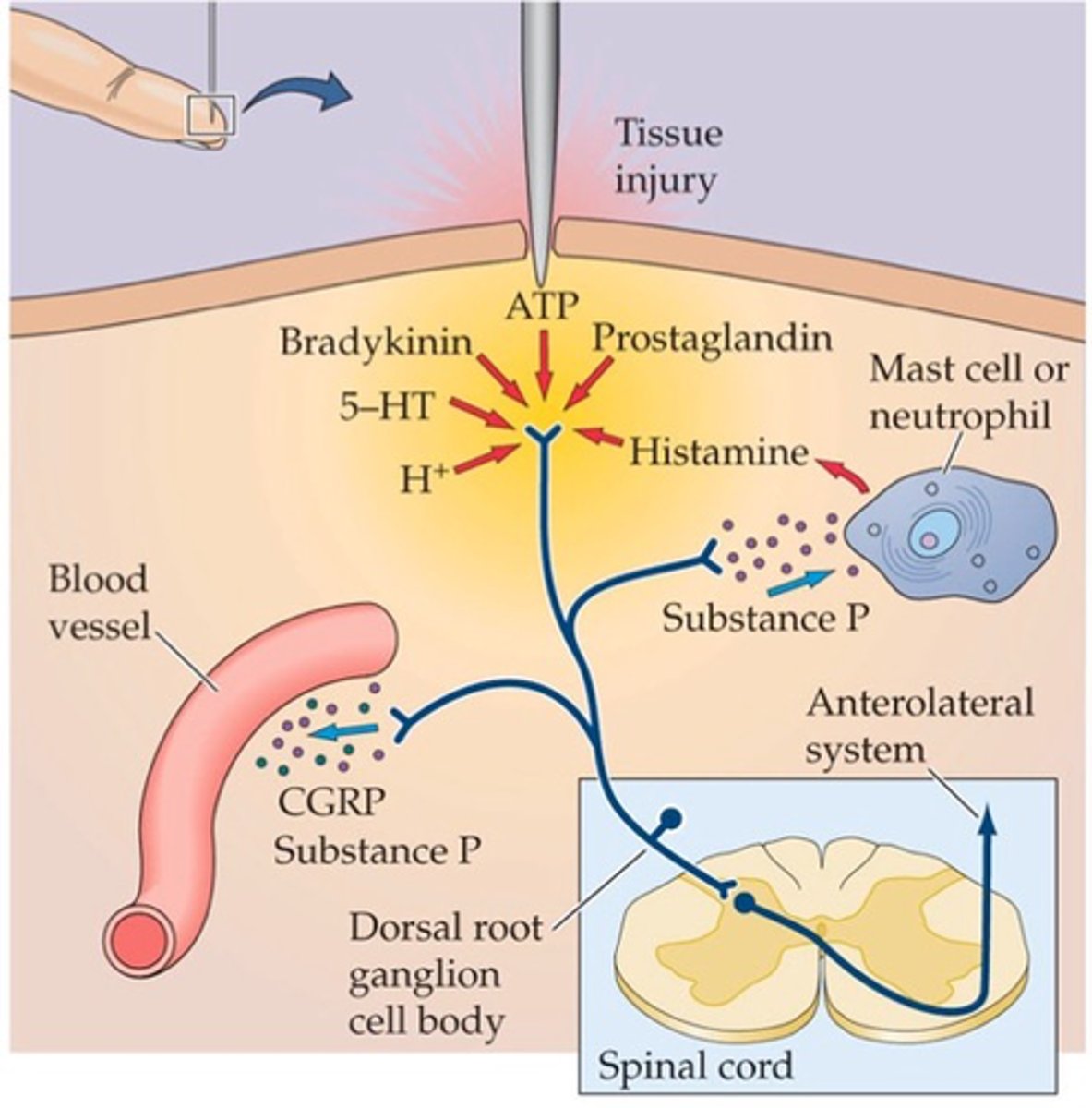
Hyperalgesia - result of lowered nociceptor thresholds which heightens pain response
What does the inflammatory response lead to?
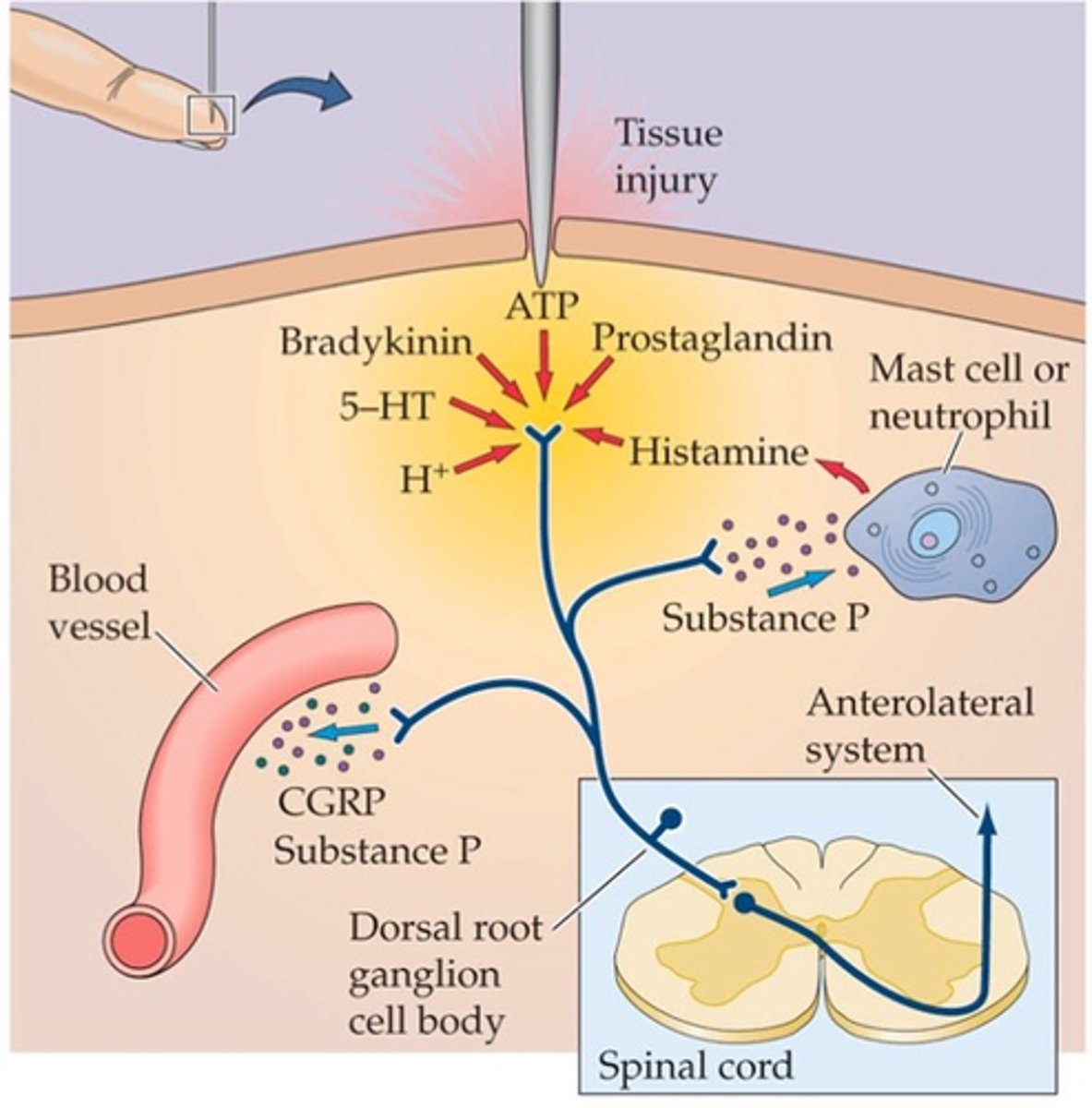
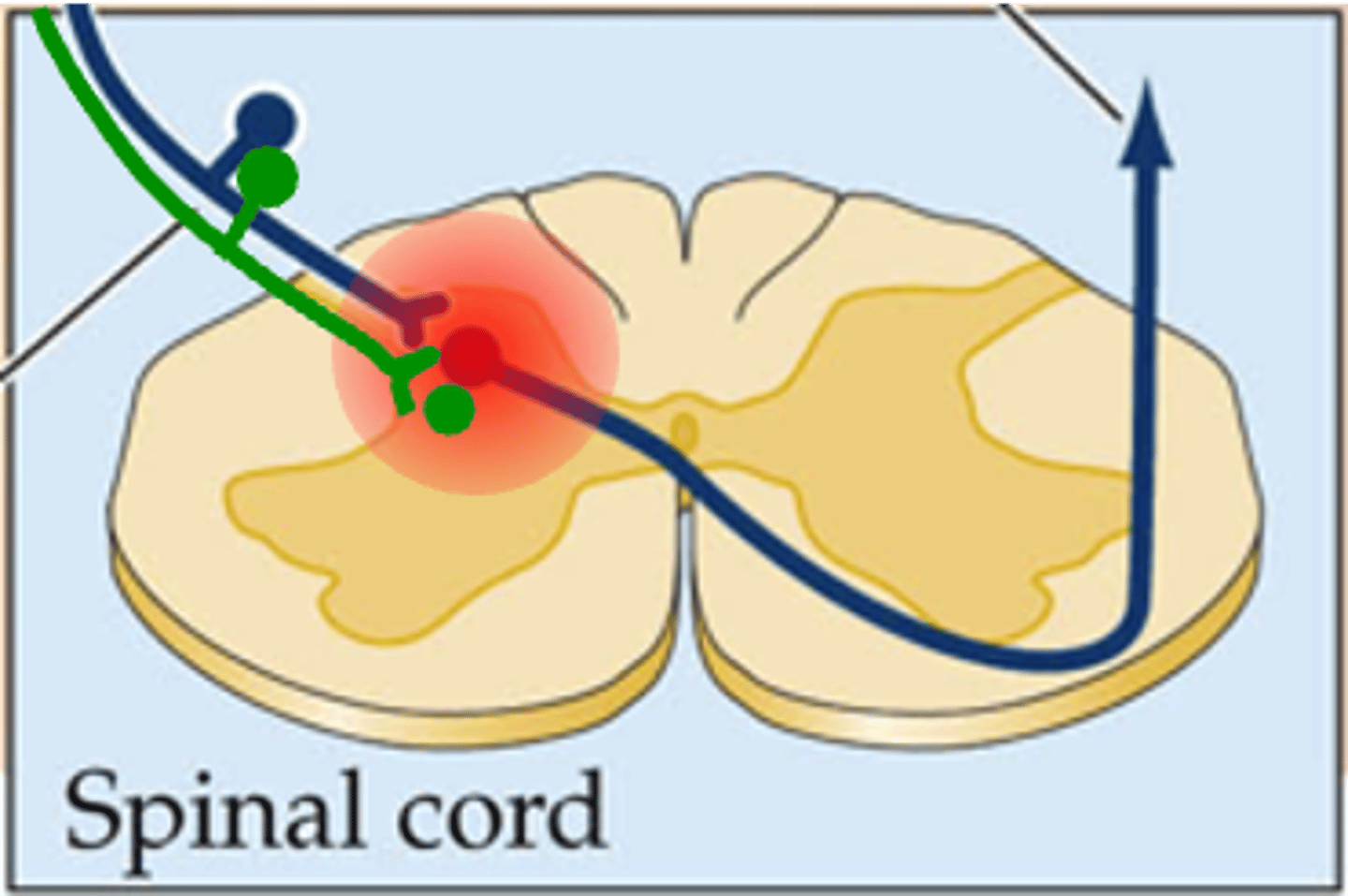
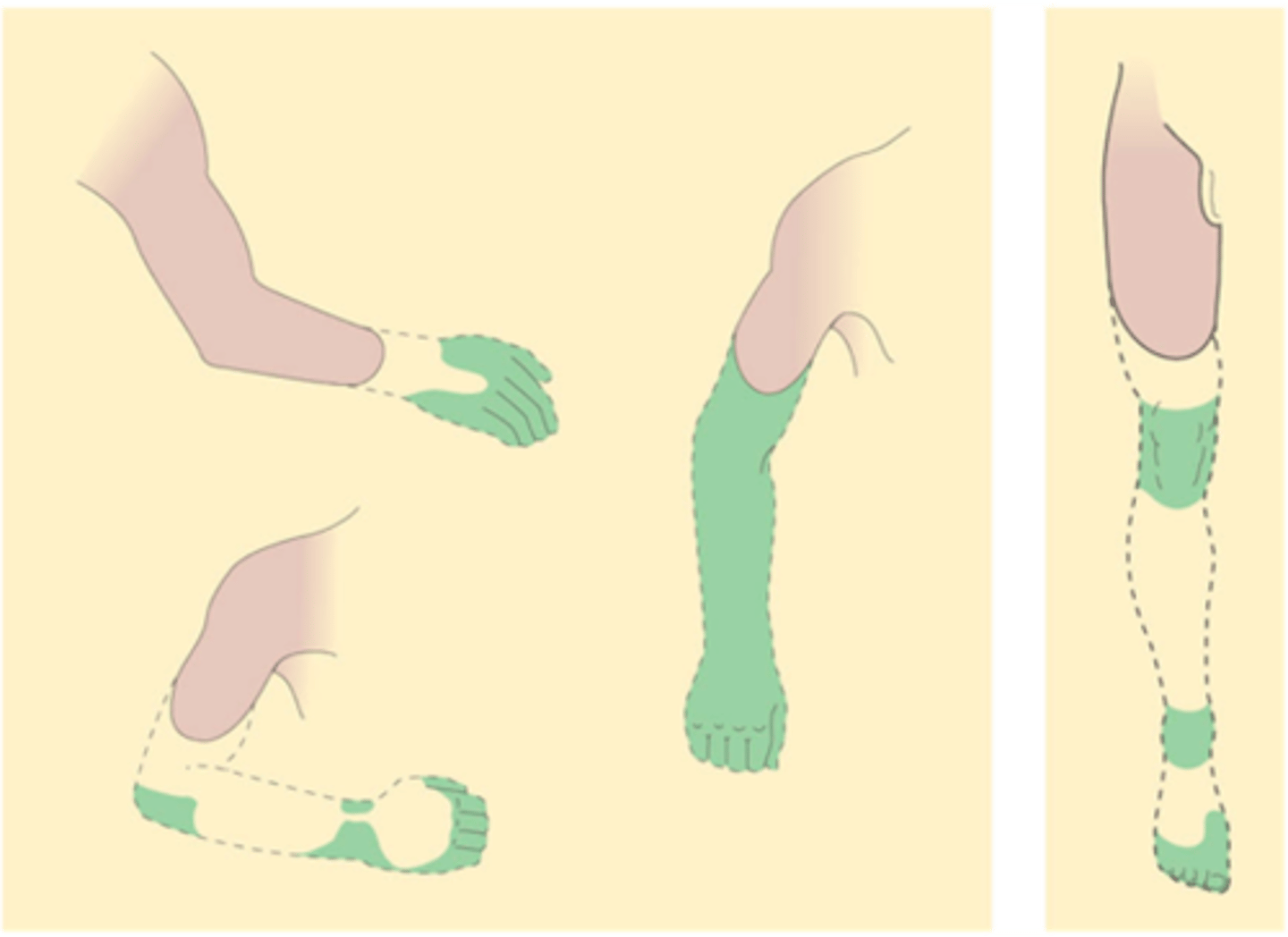
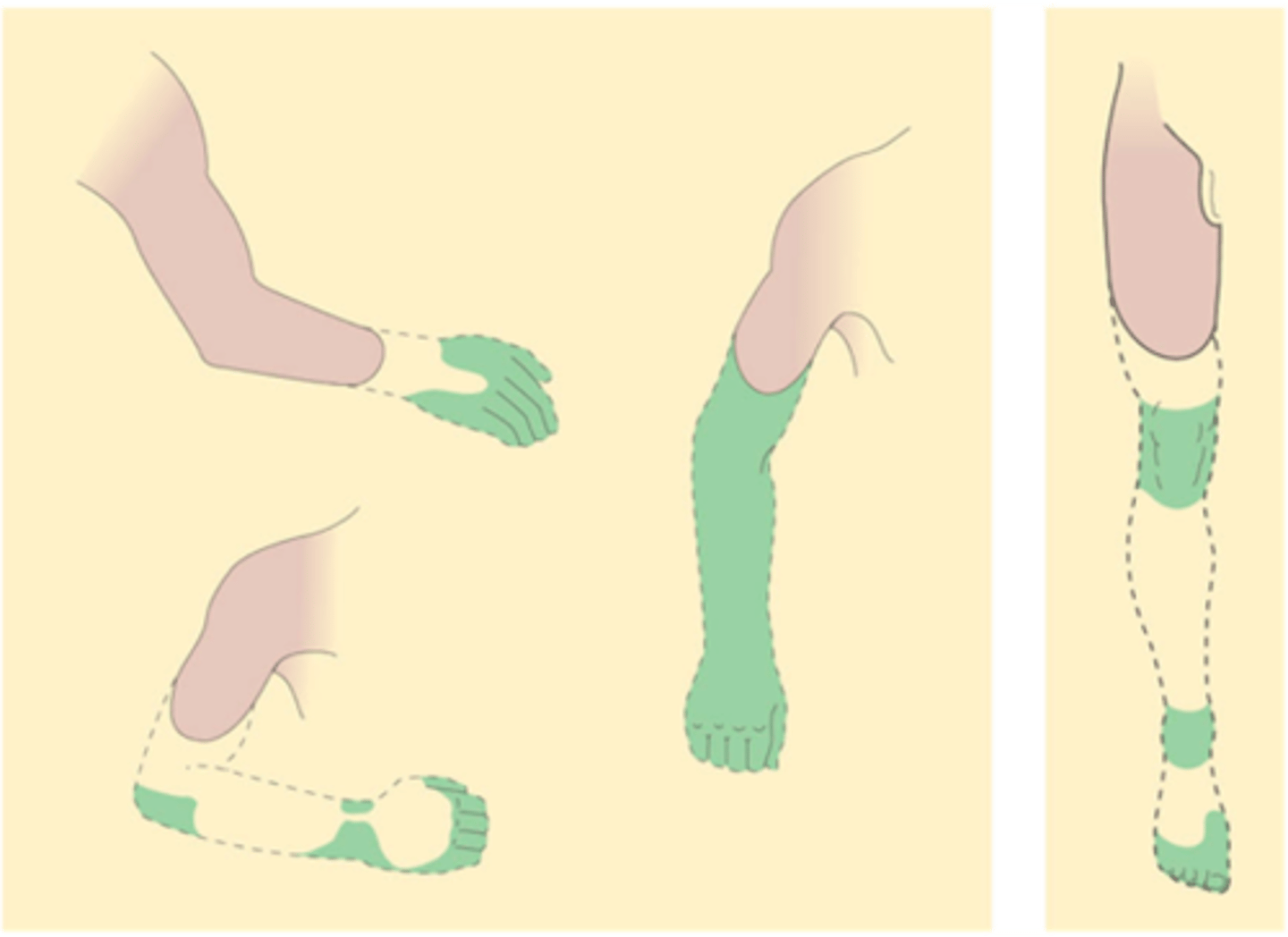
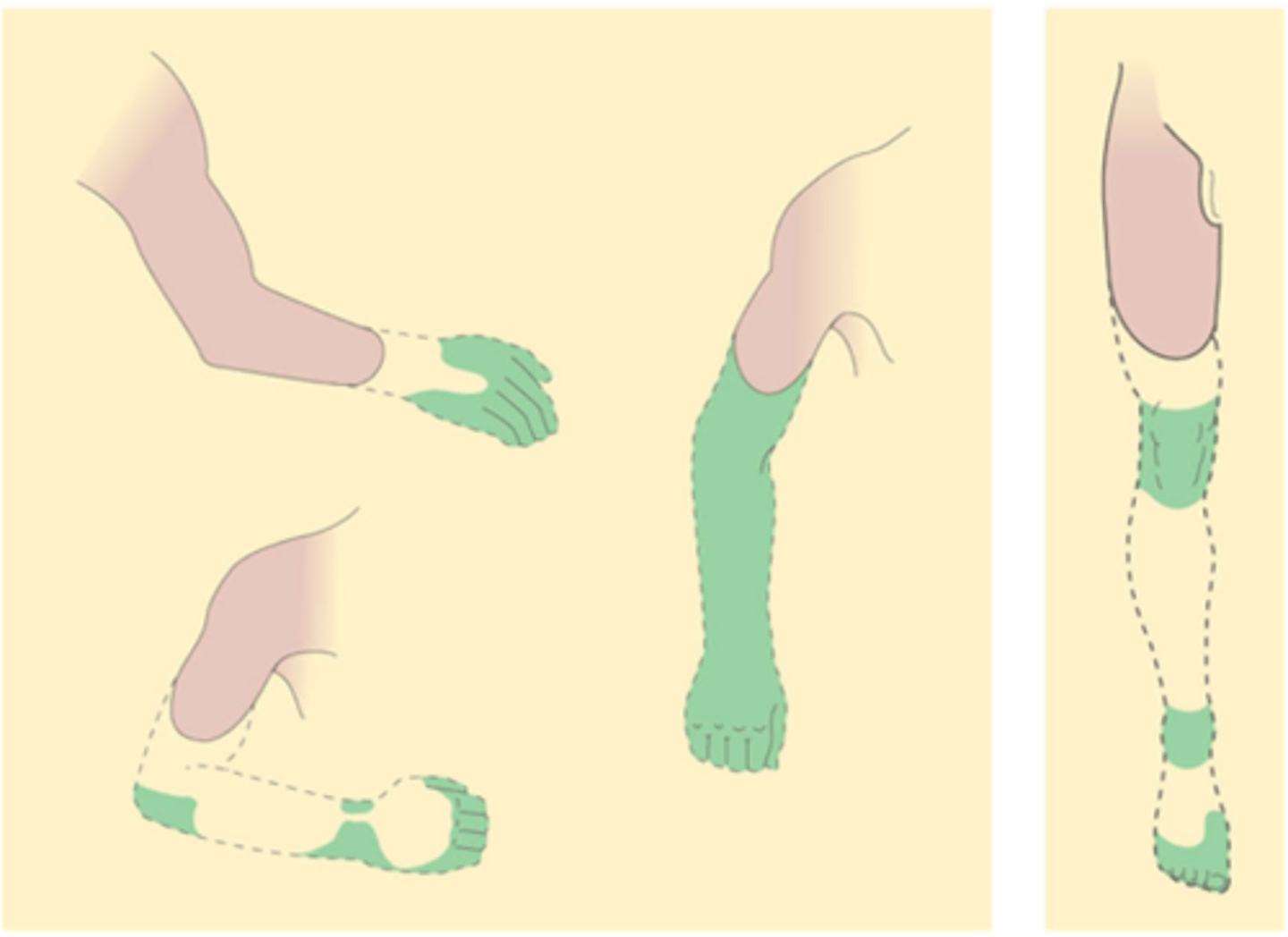
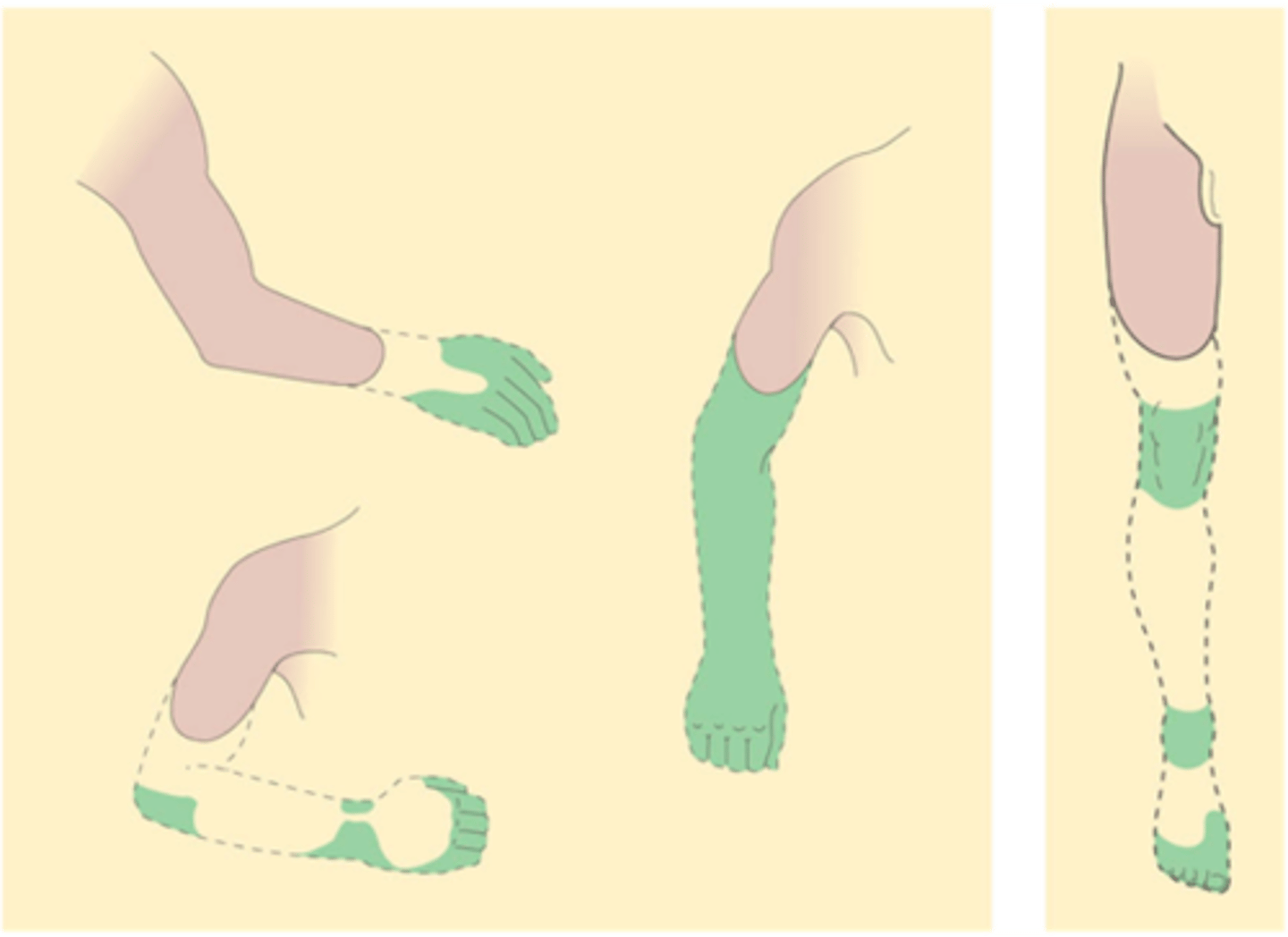
Prostaglandins, dorsal horn neurons
Centrally, sensitisation can also result from the activity-dependent local release of substances like _________________ (red in image) from nociceptive ________ _______ ___________
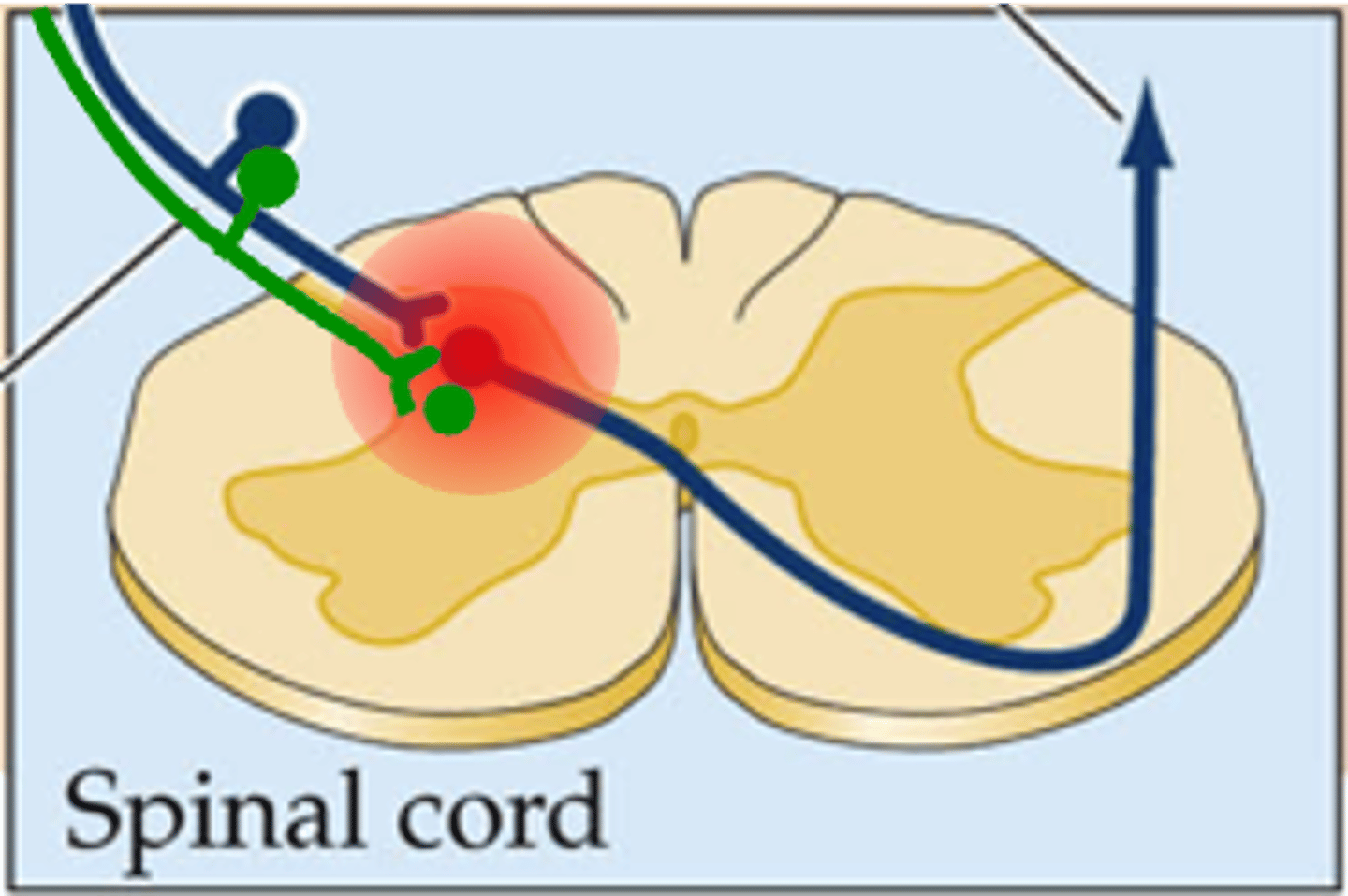
Lowering the threshold for action potential generation for neurons relaying nociceptive information, also giving rise to hyperalgesia
What can sensitisation (resulted from the activity-dependent local release of substances like prostaglandins) cause centrally which is the same in the periphery?
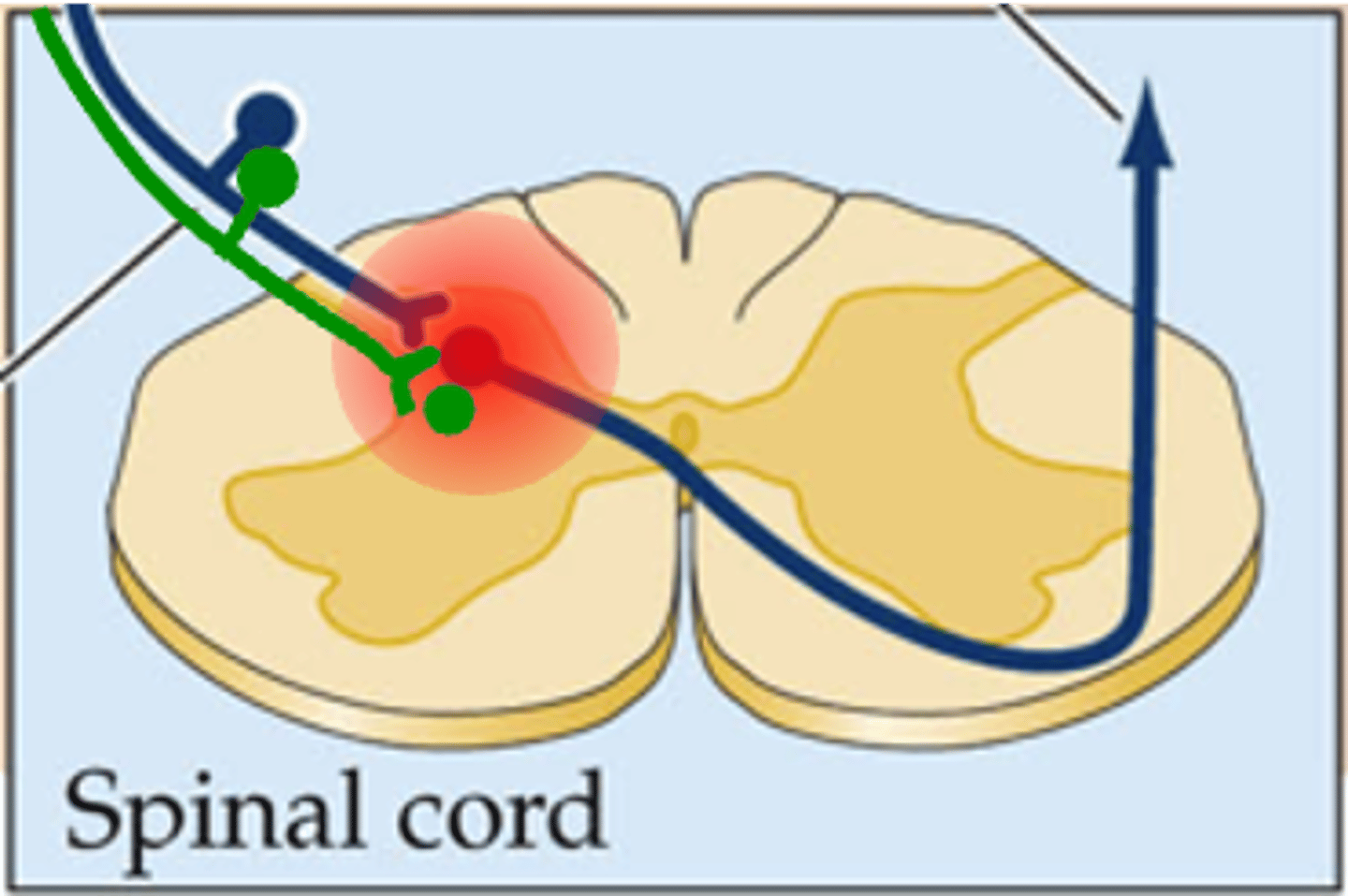
They also become sensitive to nearby non-nociceptive inputs (e.g. mechanoceptors)
What is another consequence of the lowering the threshold for action potential generation for neurons relaying nociceptive information?
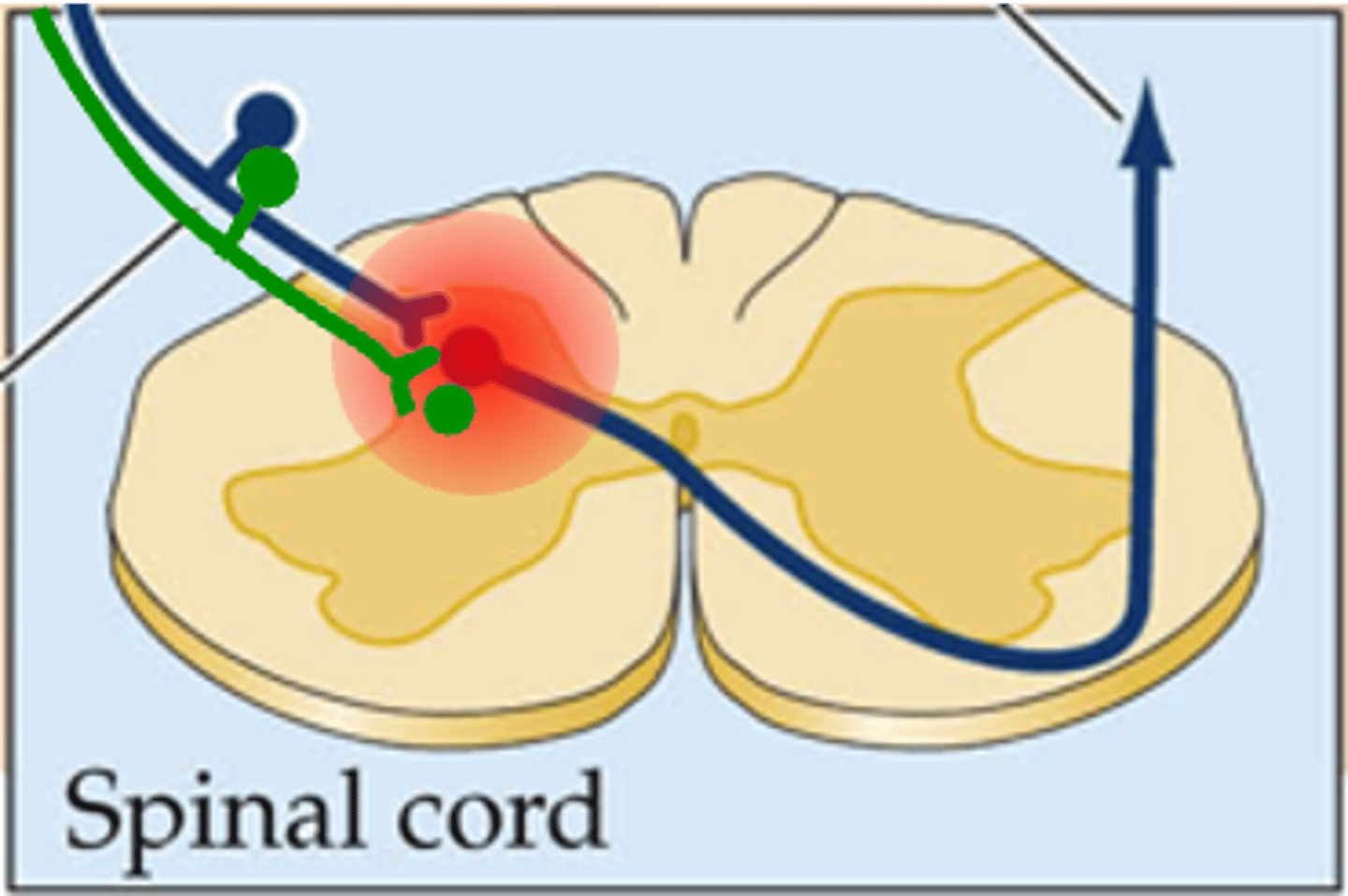
Innocuous stimuli, allodynia
The result of this is that normally _____________ _________ (e.g. gentle brushing of the skin) can be perceived as painful => ____________
Hyperalgesia and allodynia
What is hyperpathia a variant of?
When there is fibre/axonal loss/damage (either centrally or peripherally) that results in a raising of the detection threshold (i.e. you need a greater level of stimulation before the stimulus is detected)
When does hyperpathia result?
Explosive pain
When the detection threshold is exceeded, the subsequent excitability is much greater and patients report ___________ ______
When the central pathways themselves are damaged, for instance in diabetes, shingles, multiple sclerosis or after stroke
When can central sensitisation also occur?
Limb amputation
Such neuropathic pain is also sometimes experienced after ...?
After amputation
When are phantom limbs experienced?
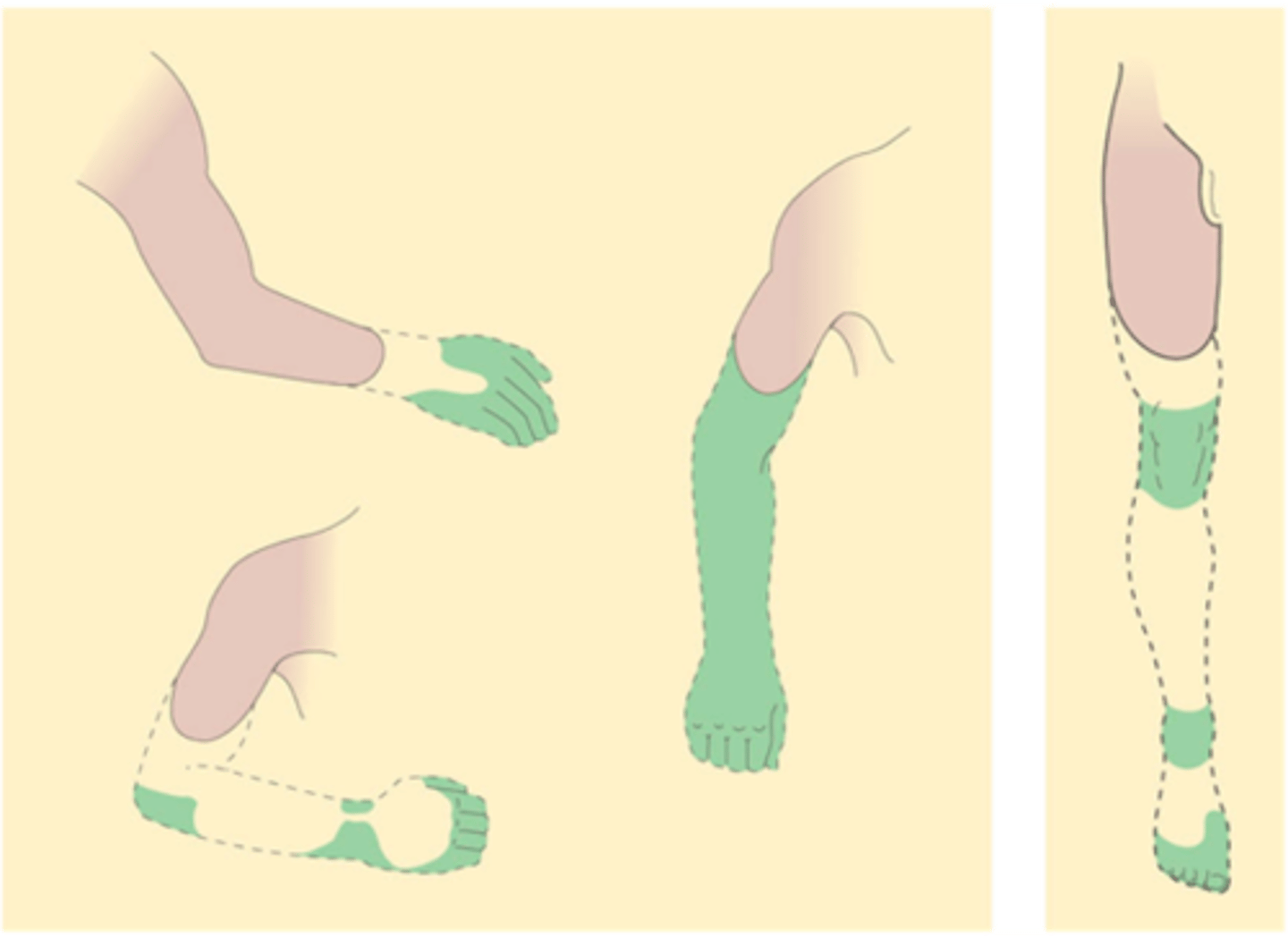
The illusion that the limb is still present
What are phantom limbs?
That central representation of the body is not passive - i.e. that it persists in the absence of peripheral input
What do phantom limbs indicate?
That central maps may be partly pre-formed
Children born without limbs can also have phantoms, what does this suggest?
That this pain may also be centrally represented
Amputees also experience pain from phantoms and attempts to block known pain pathways usually fail, what does this suggest?
Expect
Phantom limb pain suggests that the pain we experience may, in part, be a central representation of what we __________ pain to be
Specificity theory
Phantom limb pain clearly does not fit simply with _____________ _______
Pain due to damage in the viscera is often perceived as coming from specific locations in the skin according to what organ is affected (e.g. heart attack is often preceded by pain in the left shoulder and arm)
What is referred pain?
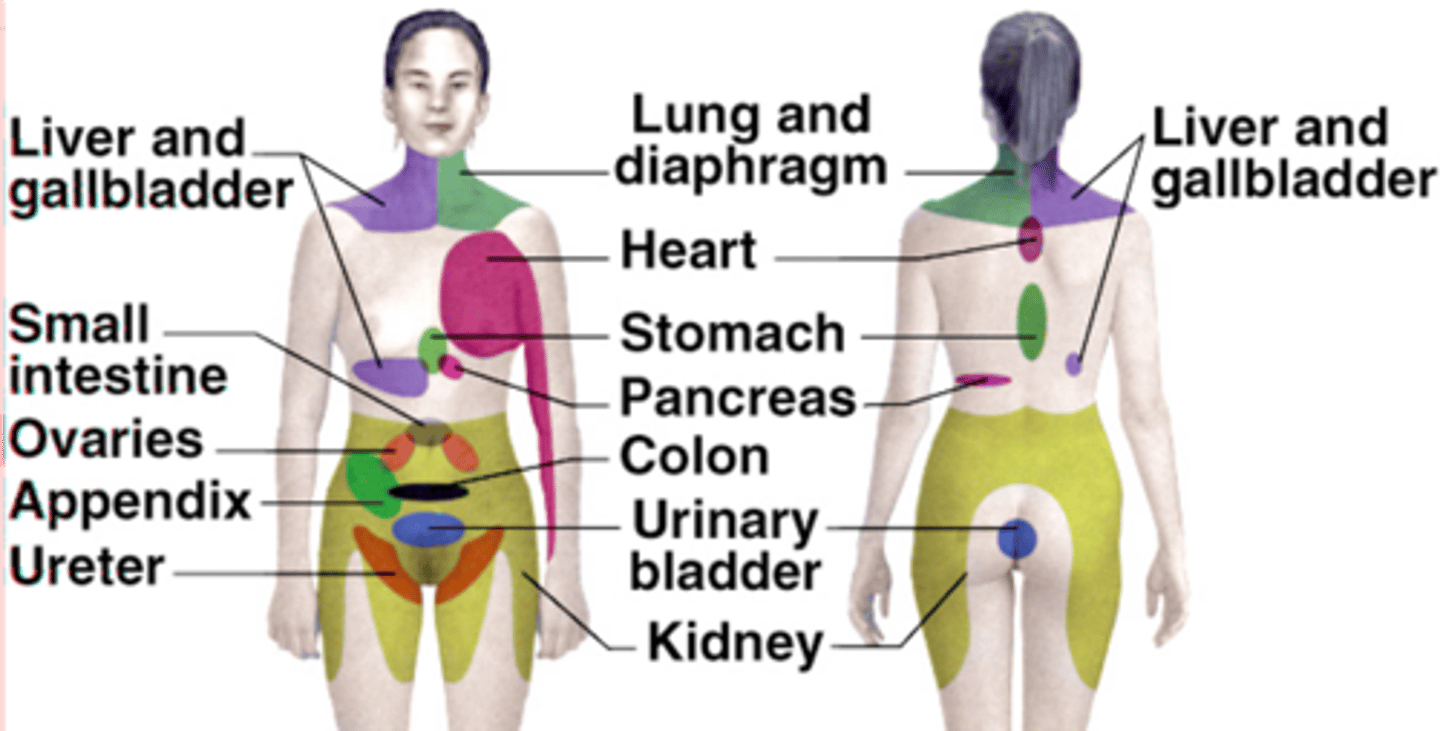
Convergence of visceral afferents onto the same pathways as cutaneous afferents in the CNS
Referred pain is not well understood but what is it thought to reflect?
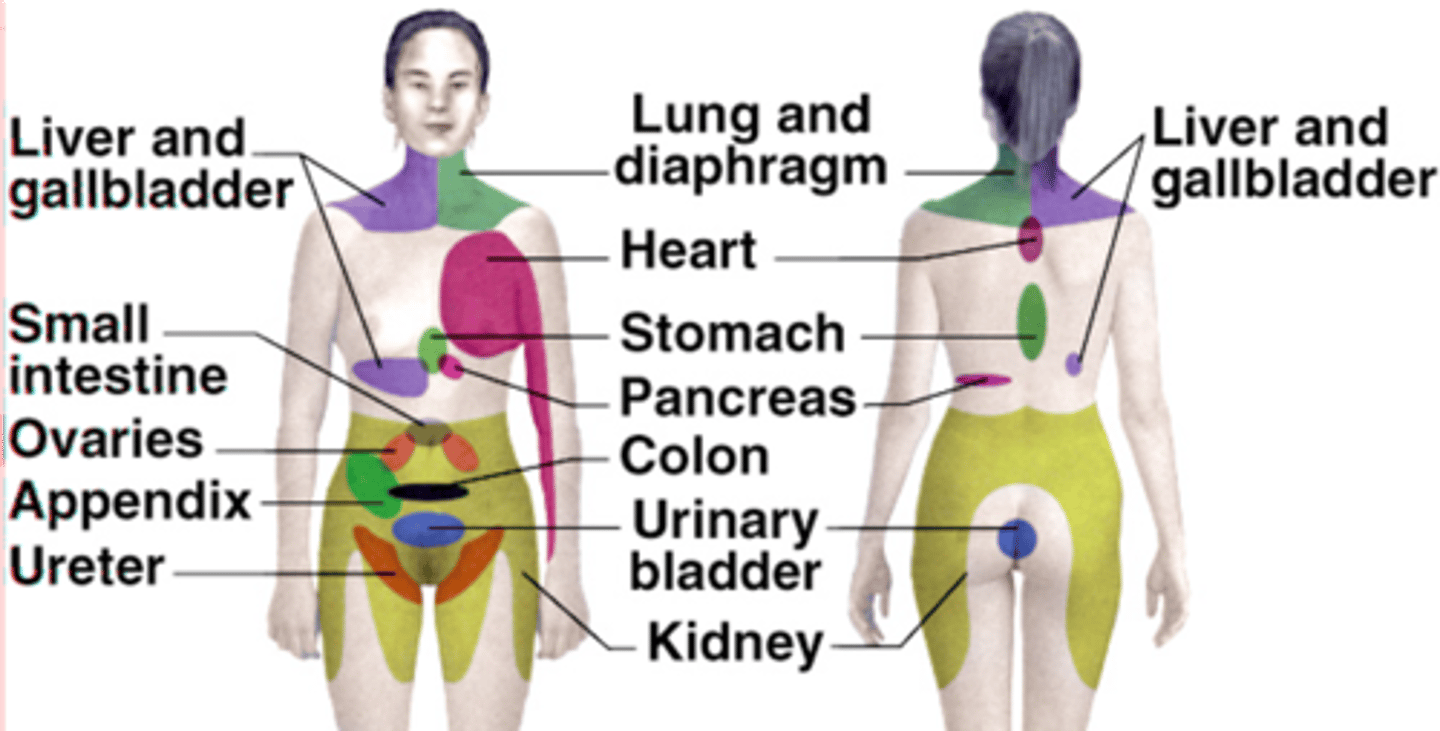
Aiding clinical diagnosis of organ dysfunction
What is referred pain extremely useful in?
Its context
Our perception of pain varies according to what?
That soldiers with severe battle wounds often experienced little or no pain
What did Henry Beecher during WWII find?
That 'mind over matter' really counts when walking on fire
What do Indian fakirs (or even tourists) demonstrate?
Placebo effect
The mere suggestion that pain will be relieved can result in real pain relief, even when no drug is actually administered, what is this phenomena known as?
When experiments stimulating certain regions of the midbrain produced pain relief
How was the physiological basis of pain modulation discovered?
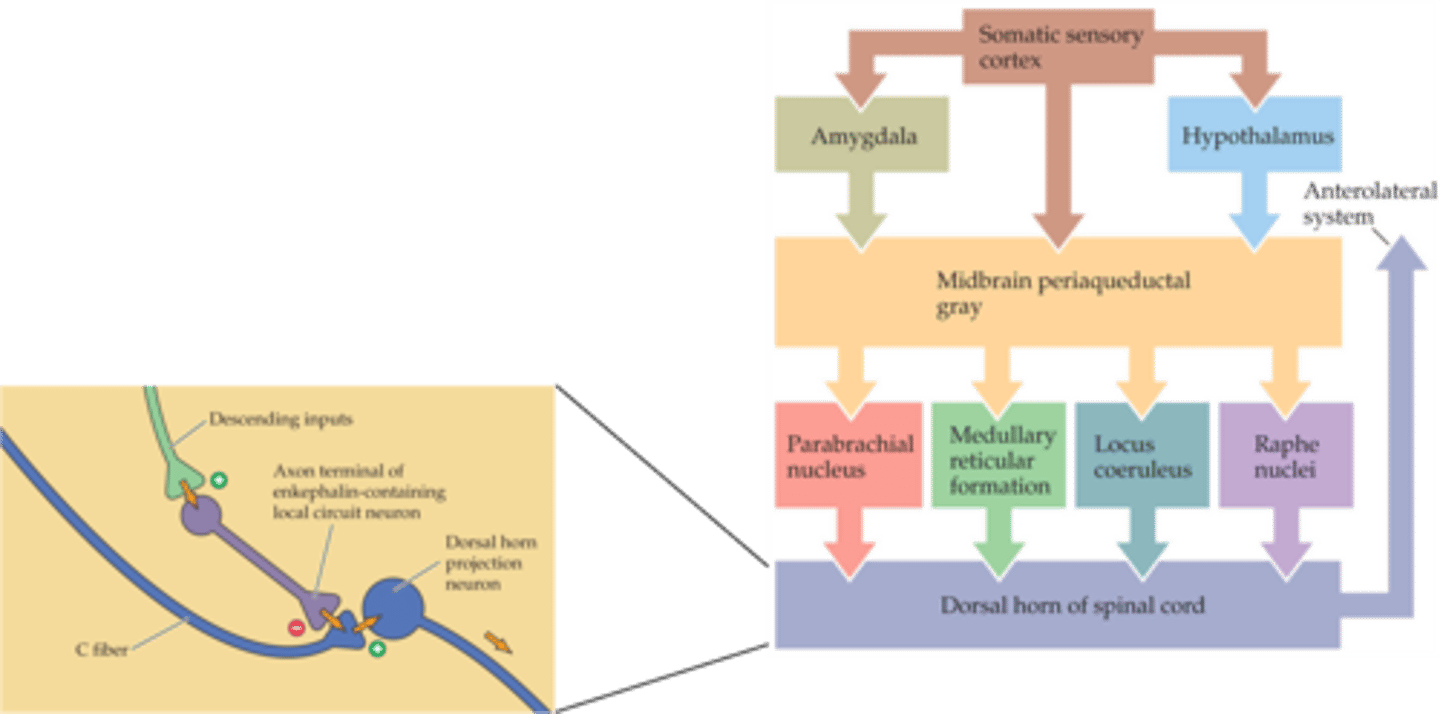
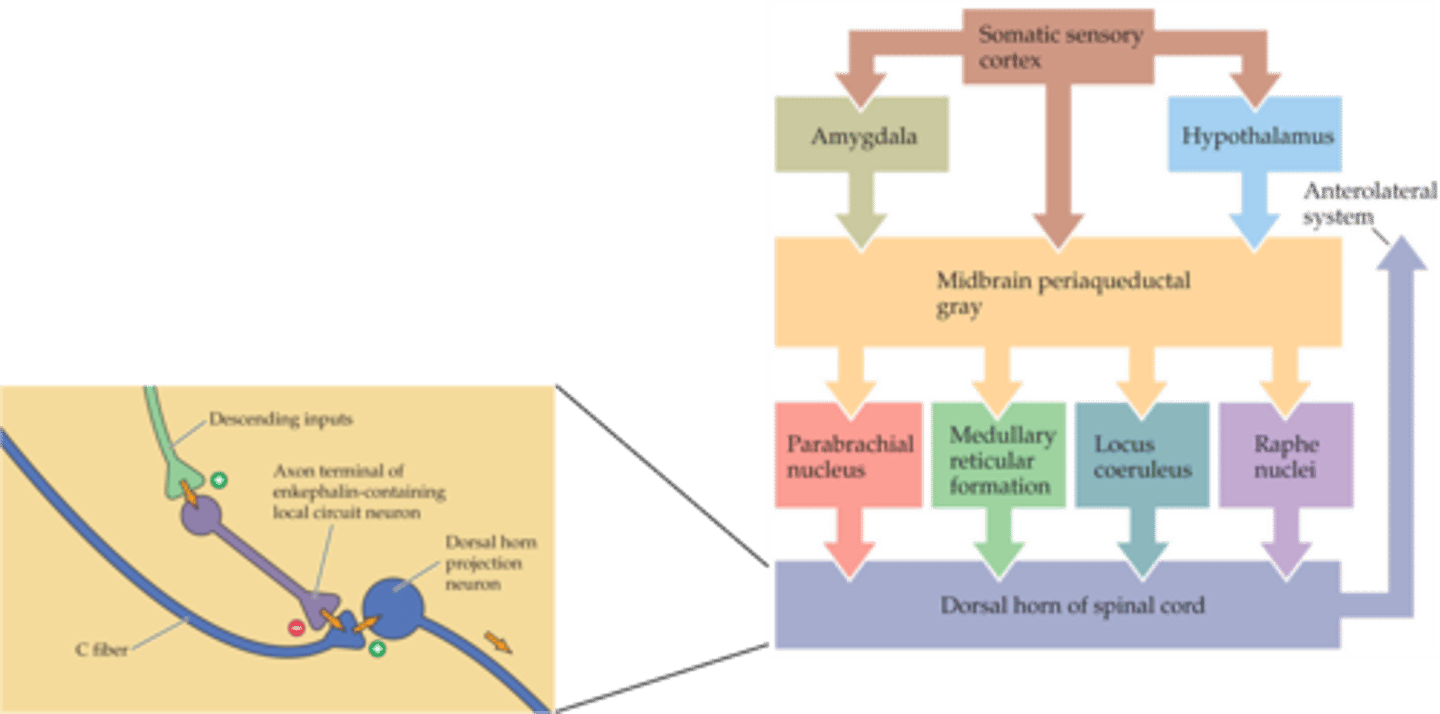
Periadqueductal grey
Stimulation of the ________________ ______ activates brainstem nuclei that modulate the activity of the dorsal horn neurones
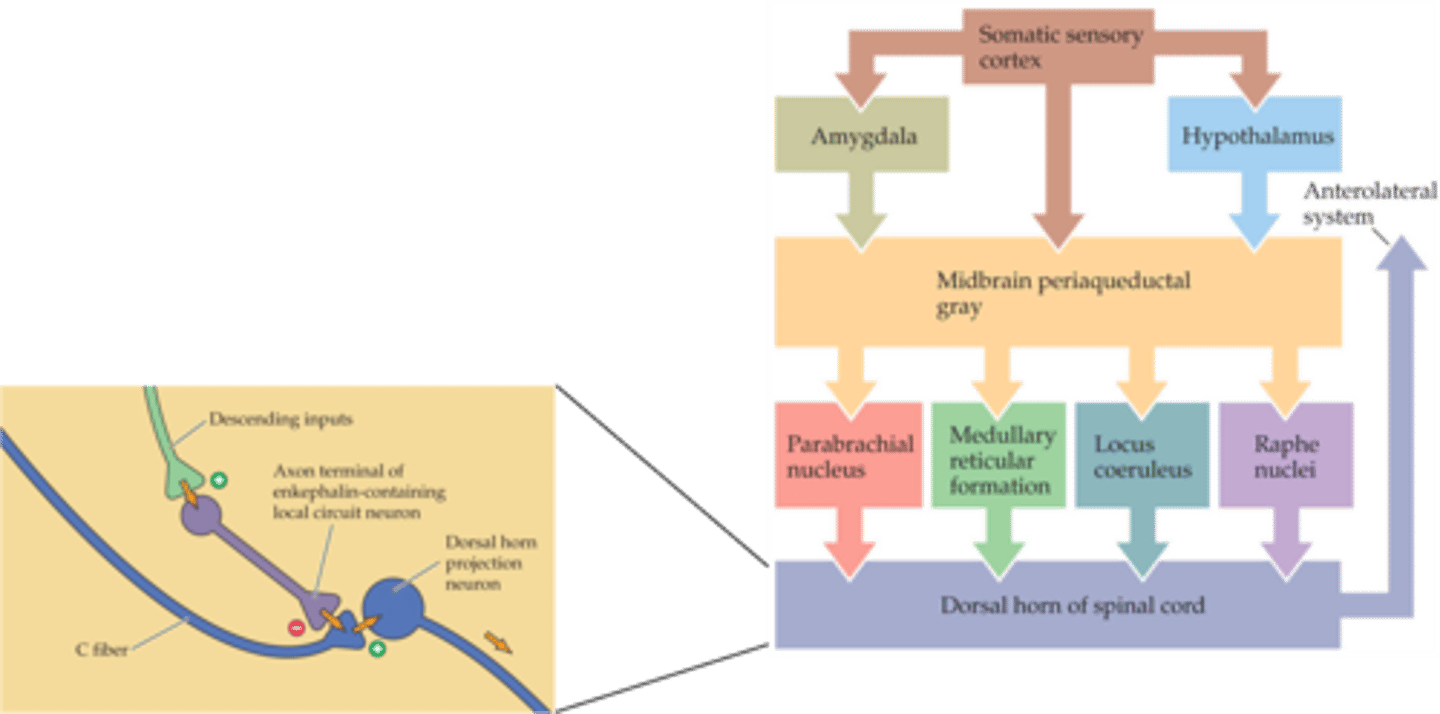
Enkephalin, nociceptive
In the dorsal horn, descending inputs activate ______________ - releasing interneurons which presynaptically inhibit __________ fibres
Endogenous opioid peptides (that also include endorphins and dynorphins)
What family do enkephalins belong to?
Local inhibition, Aβ, C
Rubbing an injury often relieves the pain - this is thought to be due to ________ ______________ by mechanoceptors (__ fibres) of nociceptive (_ fibre) inputs in the spinal cord
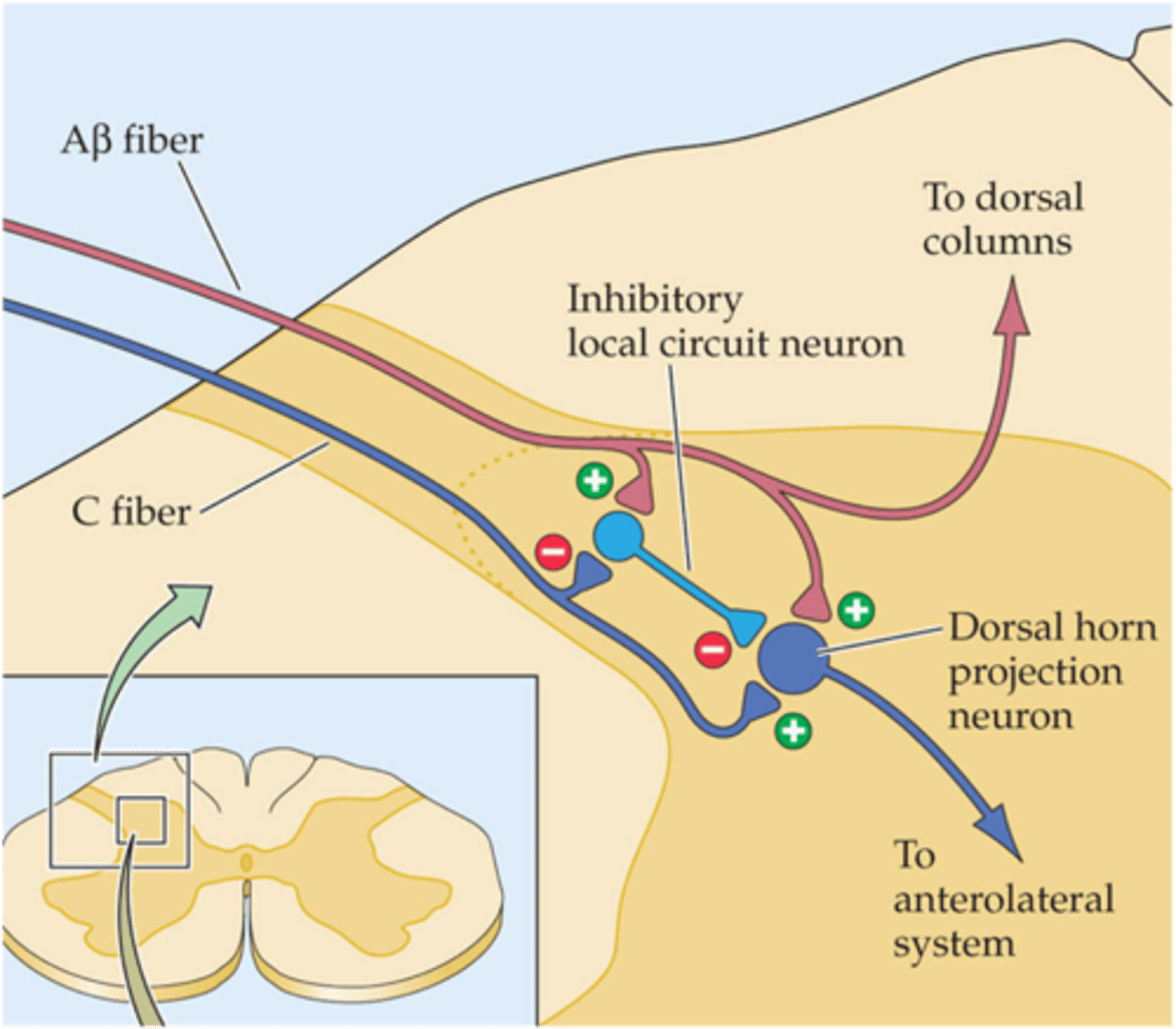
"Gate" or "Sensory Interaction" theory of pain
What did Melzack and Wall propose in 1965?
Pain perception to be the result of integration of convergent sensory information
What did Melzack and Wall's theory of pain suggest?
Warning, motivator
The complexity of our response to pain fits with its enigmatic role in our lives wherein it plays the role of both a ___________ and a ___________