Neuro Midterm Weeks 1 - 5
1/43
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
44 Terms
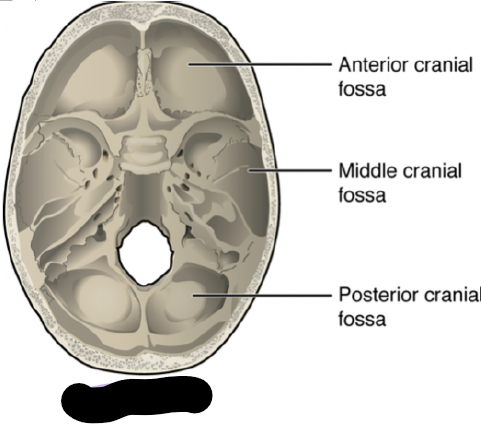
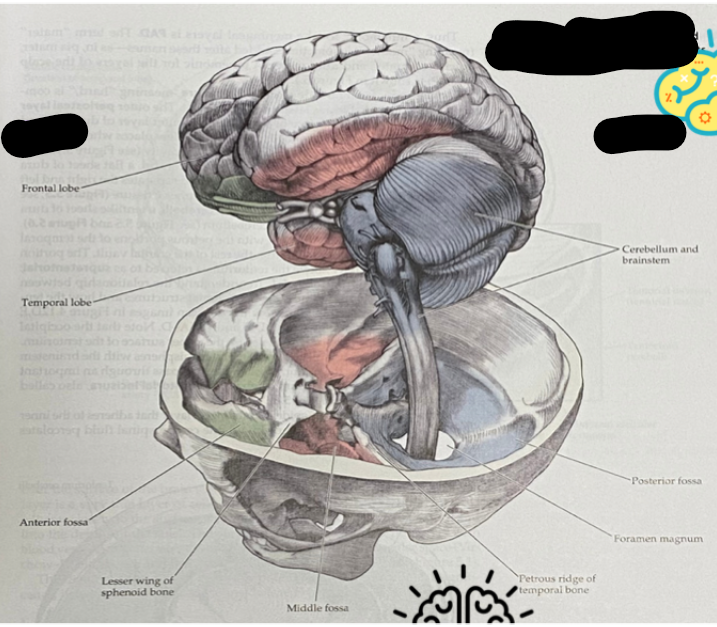
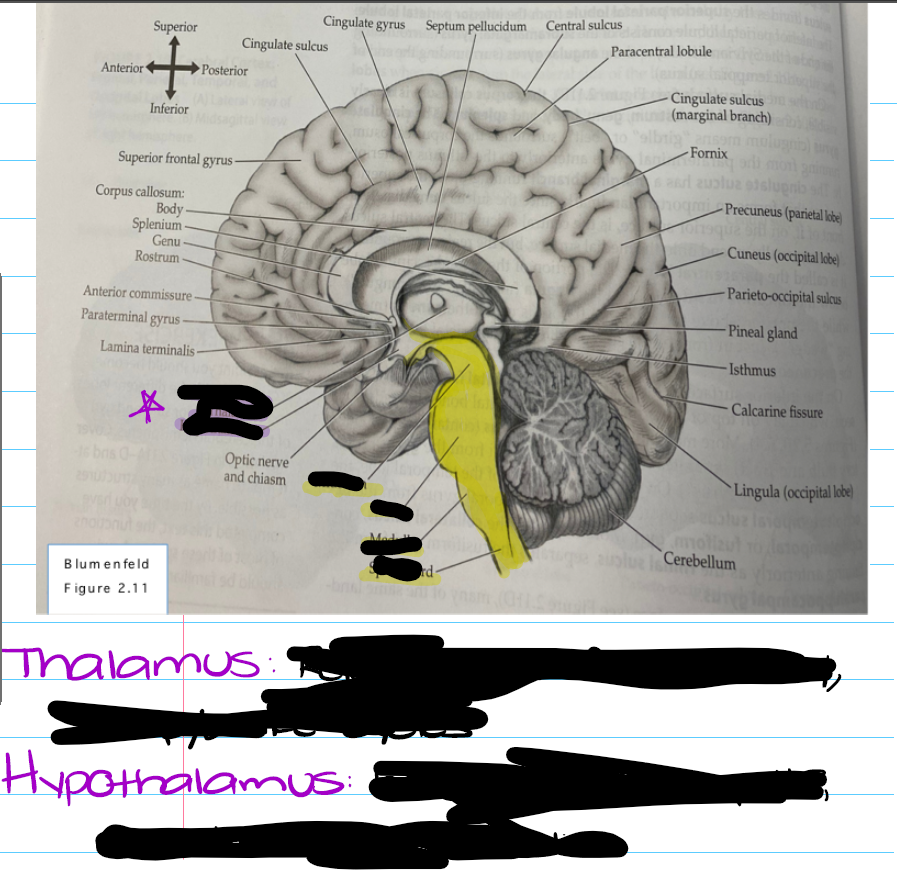
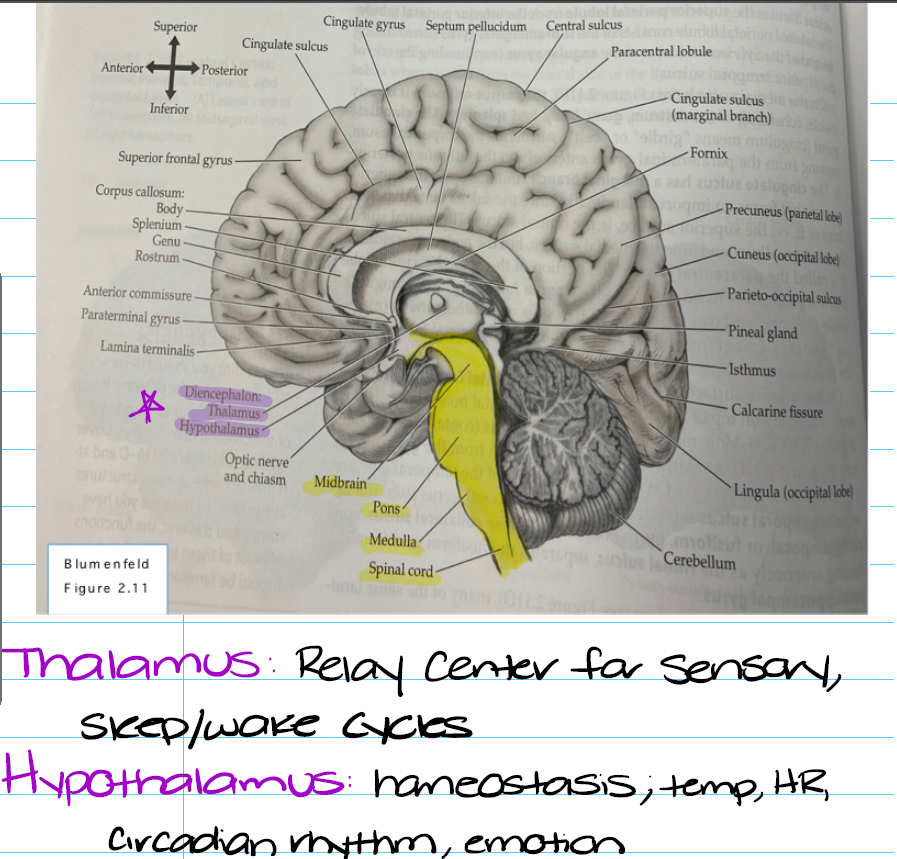
What are the three nervous systems and their individual subcategories?
Central
Consists of the cerebral cortex (cerebrum)
Subcortical structures
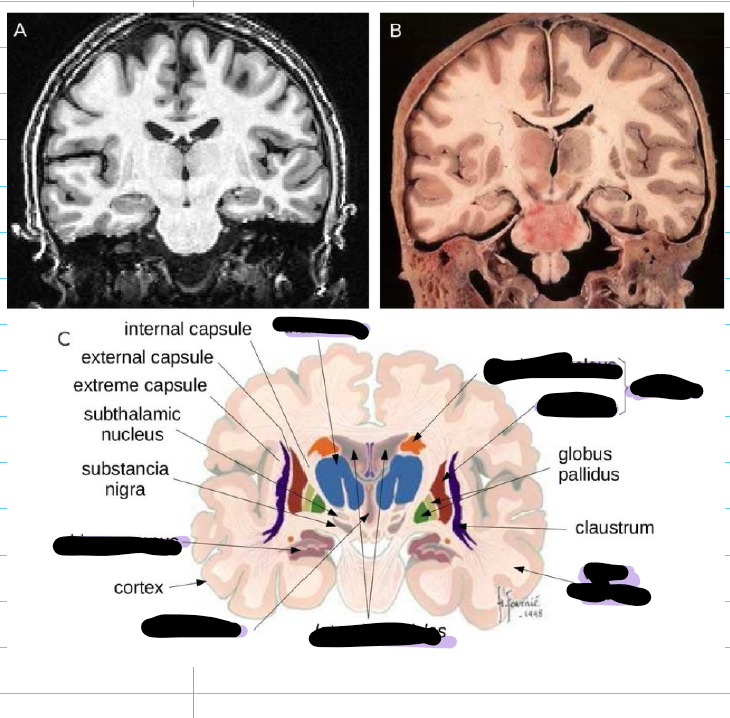
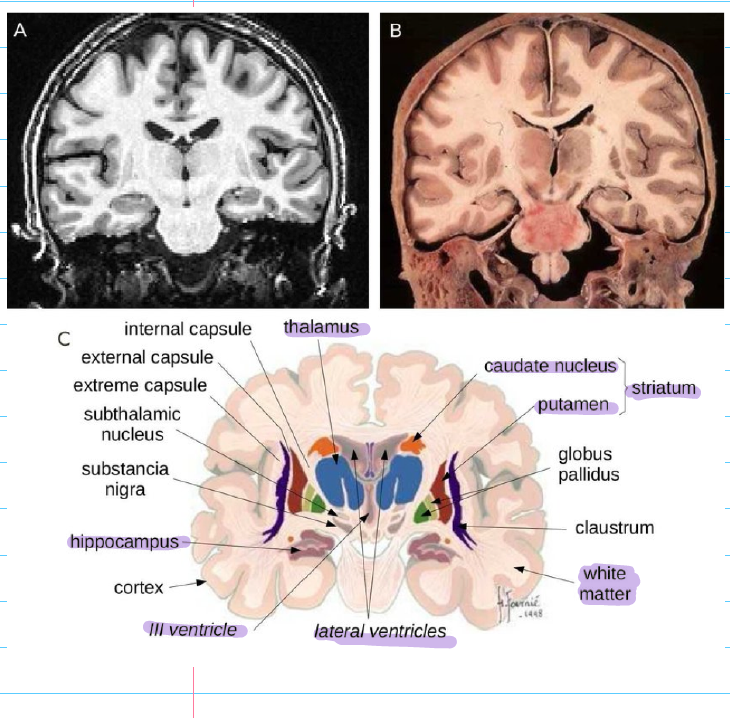
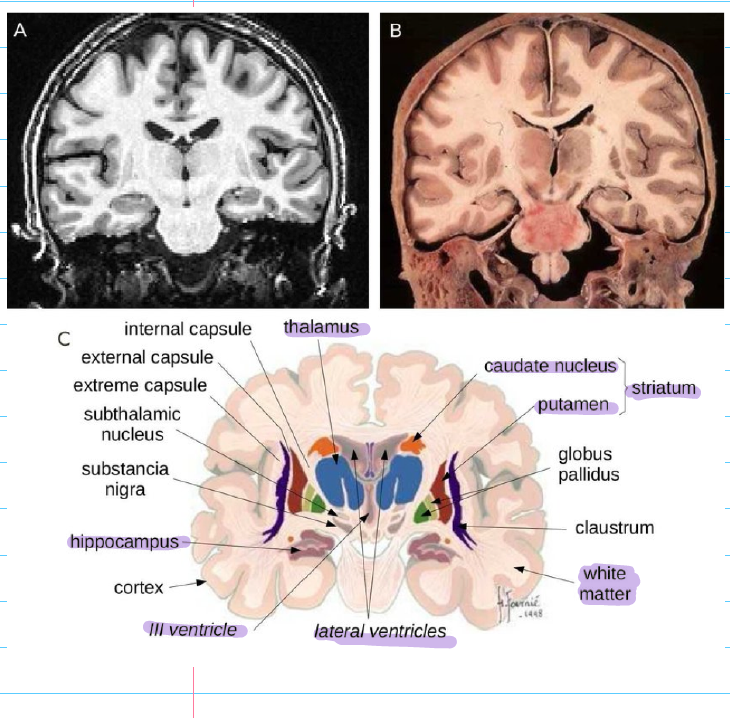
Basal Ganglia (Striatum, Subthalamic nucleus, Substantial nigra)
Diencephalon (Thalamus, Hypothalamus)
Brainstem (Midbrain, pons, medulla oblongata)
Cerebellum
Spinal Cord
Peripheral
Cranial nerves (Brainstem)
Spinal nerves (Peripheral)
Autonomic
Parasympathetic (Rest ad relax)
Cranial-sacral system
Conservation of metabolism
Sympathetic (Fight or flight)
Thoracic spinal cord
What are the 6 categories of neurological impairment? Treatment, neurophysiological rational/function (NPR/F) for each?
Weakness (Due to MSK injury or NM pathology. Over or under recruitment)
Treatment: Strengthening program, isometrics, Bands, weight, and more
NPR/F: Resetting the spindle, Reciprocal inhibition, Alpha and gamma neurons, UMN vs LMN vs motivation, Motor pathways involved
Abnormal tone (Increased or decreased, hypertonicity, rigidity vs abnormal tone)
Treatment: Relaxation, positioning, braces, strengthening
NPR/F: Supra-spinal control, Gamm overdrive, Neurotransmitters (medications), primitive reflexes
Sensory or perception dysfunction (Vestibular deficits, visual deficits, paresthesia)
Treatment: Vestibular rehab VOR, VCR. Gaze stabilization, Desensitization, approximation
NPR/F: Vestibular system, cranial nerves, thalamus and internal capsule, somatosensory systems, spinal cord
Lack of coordination (Loss of balance, dysmetria, altered RAM movements)
Treatment: Static vs dynamic activates, weighted utensils, proprioceptive training, equilibrium reaction
Cerebellum, basal ganglia pathologies
Balance dysfunctions (Center of gravity, base of support, peripheral vs central)
Treatment: External vs internal control and feedback, corrective vs compensatory mechanism
NPR/F: Vestibular vs visual vs perceptual ,Cerebellar vs cerebrum (central), NM vs MSK, peripheral control
Embryological development of the CNS (Not on study guide)
Where does it arise from? When go limbs generate and bud?
What are the 4 sections
Arises from a sheet of ectodermal cells that folds over to form the neural tube. Limbs generate and bud close to 5 - 6 weeks.
Prosencephalon (Forebrain)
Telencephalon
Diencephalon
Mesencephalon (Midbrain)
Rhombencephalon (Hindbrain)
Mesencephalon
Myellencephalon
Spinal chord
What are the anatomical planes of section?
Horizontal, Coronal, Sagittal
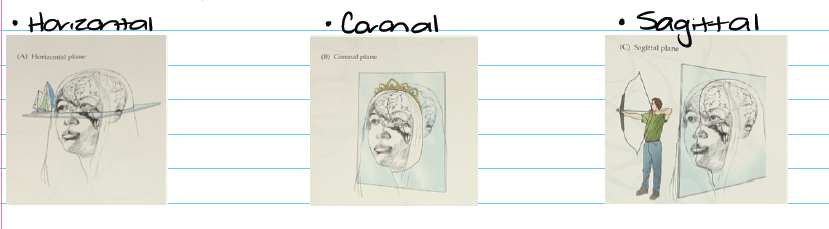
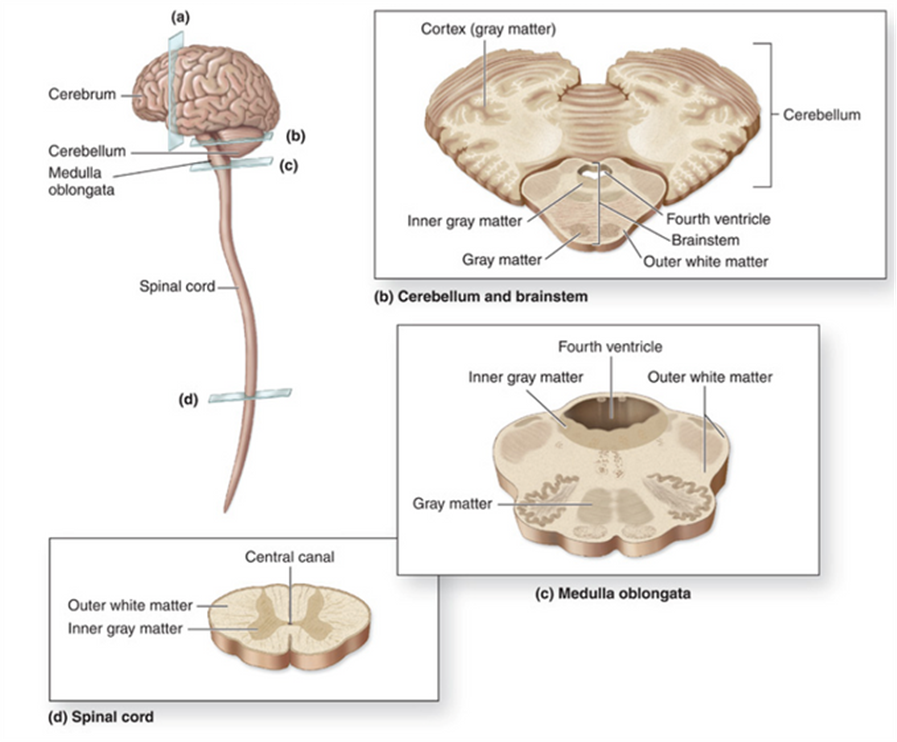
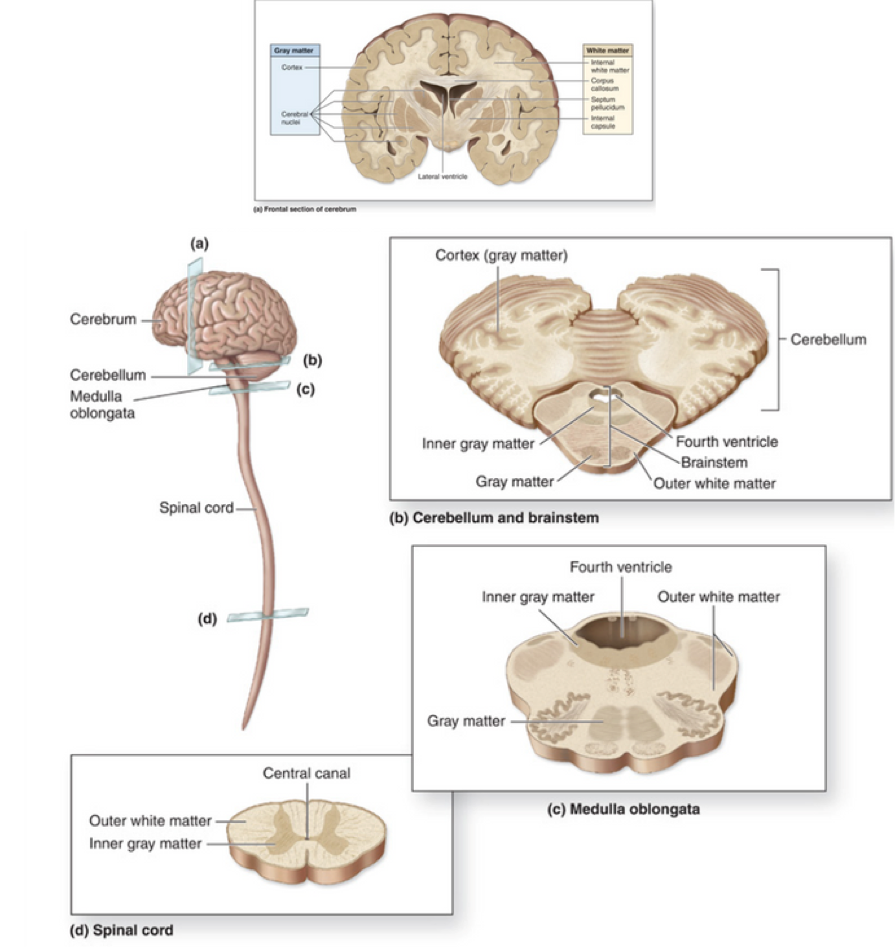
In the image below, name the anatomical plane of section for A B C and D
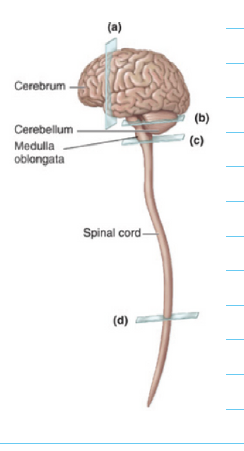
A: Coronal view, Frontal section of cerebrum
Ventricles are visible

B: Horizontal view, cerebellum and brainstem
cerebellum is physically connected to the rest of the NS at the level of the brainstem
C: Horizontal view, Medulla oblongata
D:Horizontal view, spinal cord.
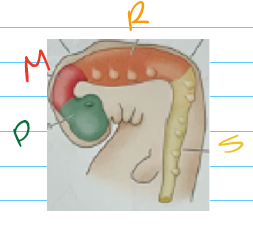
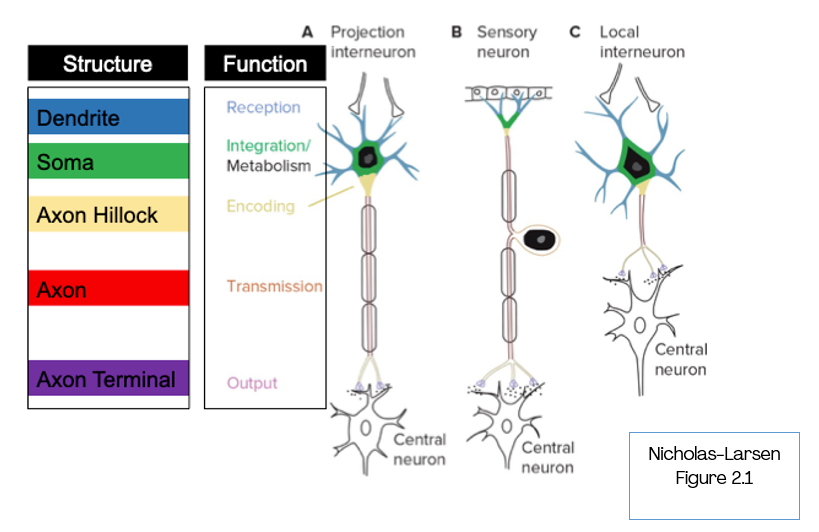
In the image bellow label the numbers and what each does
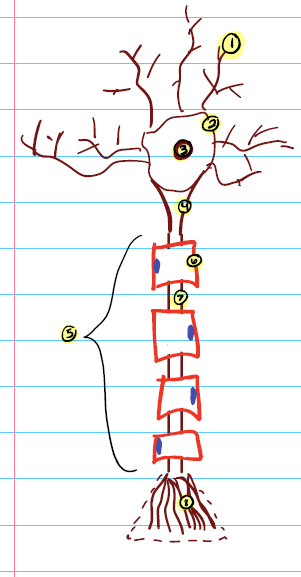
Dendrites → Reception
Receives signals
2 and 3. Cell body and nucleus → Integration/metabolism
Combines info. Cell metabolism, and houses nucleus
Axon hillock → Encoding
Maintains membrane potential and is the action potential site. Cone shaped.
Axon → Transmission
Transits electrical signals (action potential). May or may not be myelinated
Myelin sheath → Protection
Protects, isolates, and helps increase transmission speed. Composed of proteins and lipids
In the CNS myelin is produced in oligodendrocytes ; PNS myelin is produced by Schwann cells. BOTH are glial cells
Node of Ranvier → Optimization
Optimizes energy consumption and impulse transmissions; increases speed, facilitates movements and ensures signal does not get lost (nerve impulse jump conduction). Gap/spaces between myelin sheaths.
Axon terminal → output
Creates synapse and links to other neurons. Neurotransmitters are stores here in the synaptic vesicles
What are the three types of neurons and what does each do? How does each look?
Sensory neuron
Dendrites = receptors
Cell body = housed in dorsal root ganglion
activates with sensory mechanisms
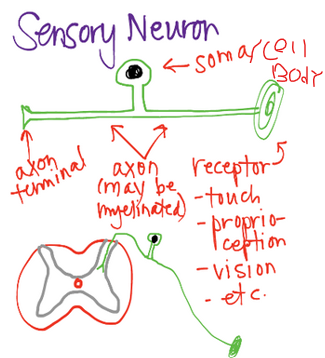
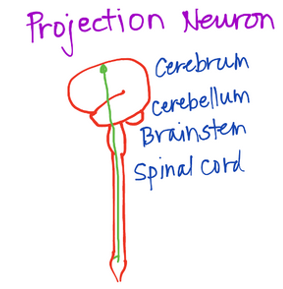
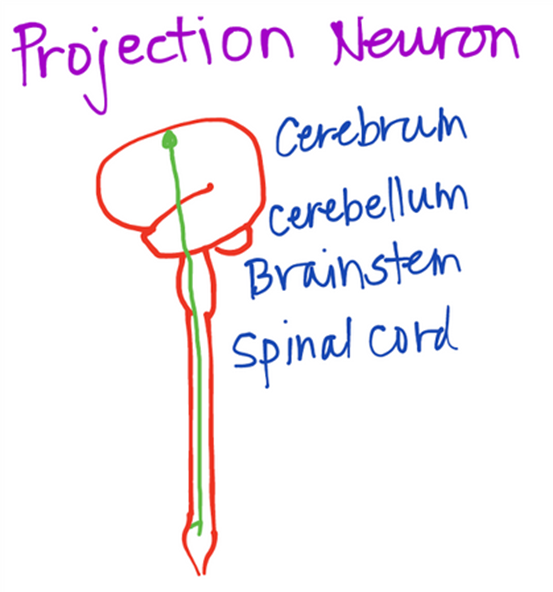
Projection neuron
Travels long distances. Myelinated axons
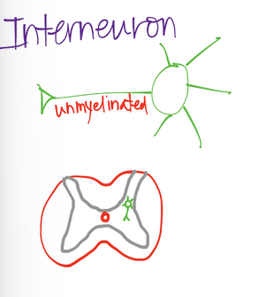
Interneuron or local interneuron
Travels short distances
Unmyelinated axons
Changes synergistic muscle activity
Pic of all:
What does glial cells do? What are the 5 types and what does each do?
Glial cells are support cells that help maintain homeostasis in the CNS + PNS
Ependymal cell
Makes up thin membrane lining in central spinal cord + ventricles. Also makes up CSF fluid and has a big role in the blood brain barrier
Astrocytes
Facilitates nutrition. Helps maintain normal signaling. Also has connections to both neurons and vasculature.
Microglia
The clean up crew (the immune cells of the CNS), works with macrophages and limits ecotoxicity. Has a role in promoting plasticity
Oligodendrocytes
Produces myelin sheath around axons. acts as insulation and increases speed of conduction. Myelinates in CNS.
Schwann Cells
Produce myelin sheath around axons. Acts as insulation and increases speed of conduction. Nerve regeneration after injury → metabolic support. Myelinates in PNS
What is the blood brain barrier BBB?
BBB
is a filtration system for the brain. Carries blood to brain spinal cord tissue while blocking certain substances. Vital.
selective semi-permeable border composed of endothelial cells.
Protective barrier to CNS from unwanted substances in blood
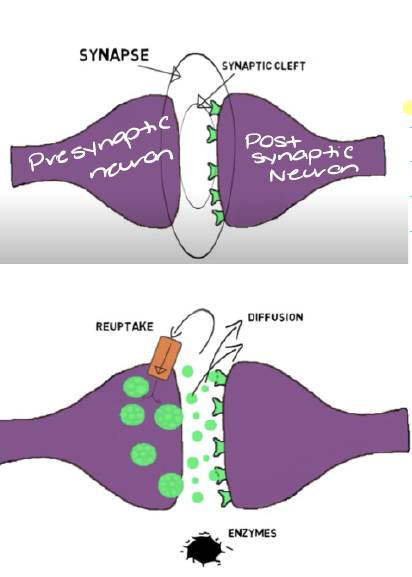
What is synaptic transmission and how does it work?
This is when neurotransmitters are released from the axon terminal of the presynaptic neuron and bind to receptors in the post synaptic neuron.
Pre synaptic neuron houses the vesicles (NTs) and gets released in the synaptic cleft.
Post synaptic neurons accepts the NTs necessary to either excite or inhibit the signal to get relayed.
Excess NTs in the cleft get reduced, reused or recycles via reuptake, diffusion or enzymes degradation
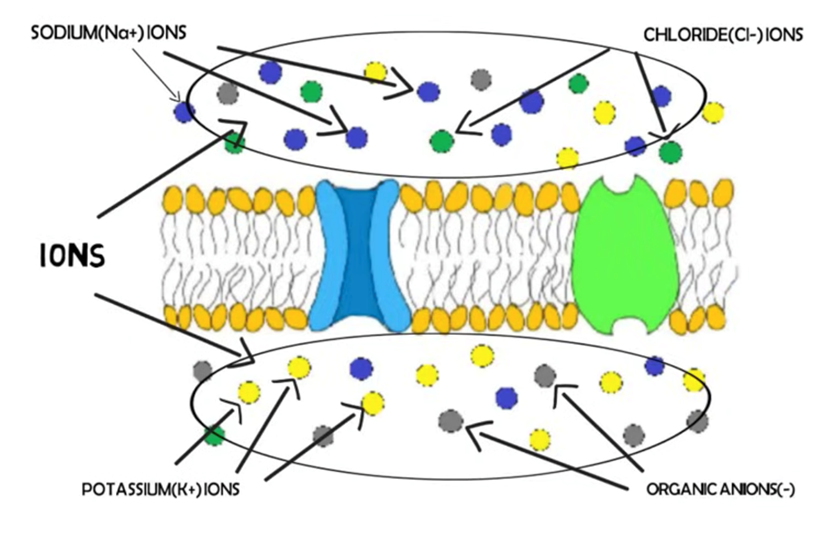
Membrane potentials are established because? Where are K+, Na+, and Cl-?
What is the resting potential of a neuron?
established because ion concentration gradients across the cell membrane phospholipid bilayer.
K+ (Potassium ion) Inside neuron
Na+ (Sodium ion) Outside the neuron
Cl- (chlorine ion)
Resting potential of the neuron is usually -65 to -70 mV. So the inside of the cell is slightly more negative than the outside.
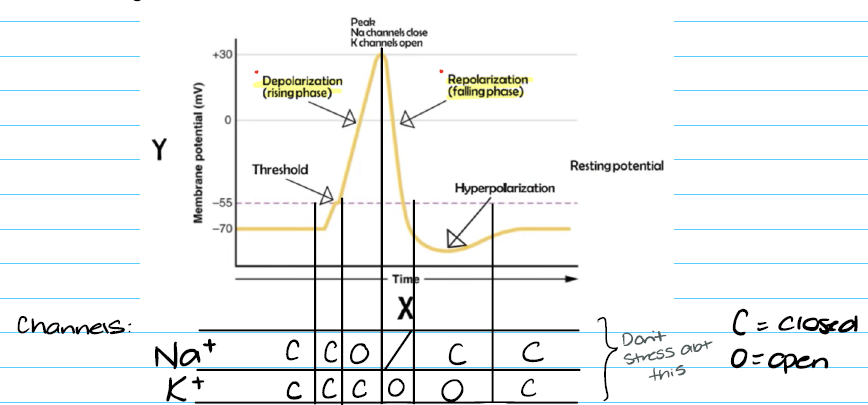
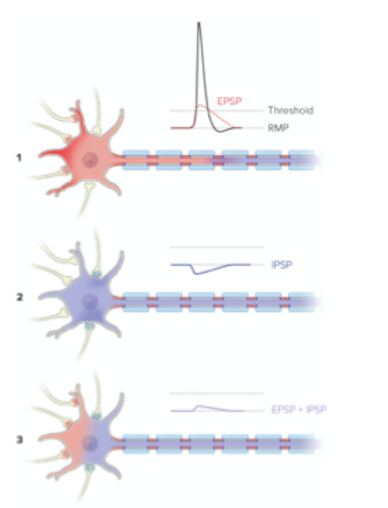
Pre synaptic neurons can deliver either what two inputs to the post-synaptic cell?
What is graded potentials and how does it relate to action potential?
Excitatory EPSP (+ potential)
Depolarization TO threshold
Inhibitory IPSP (- potential)
Hyperpolarization AWAY from threshold
Graded potential: Sum of both potentials
Action potential is the reaction to the sum, exceeding threshold
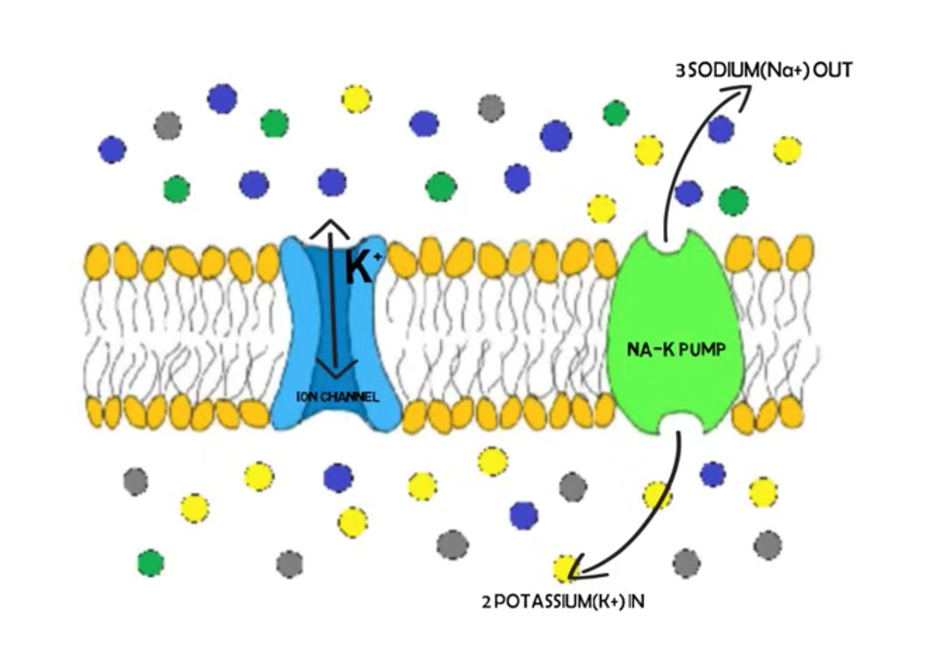
Active transport mechanism:
What is the sodium potassium pump? Potassium channel is always what?
Sodium potassium pump
For every 3 Nat+ out of the cell 2 K+ replace inside the cell.
The inside of the cell is slightly more negative than the outside. , If this is off balance then things like seizers or strokes can occur so this process is vital.
Potassium channel is always open
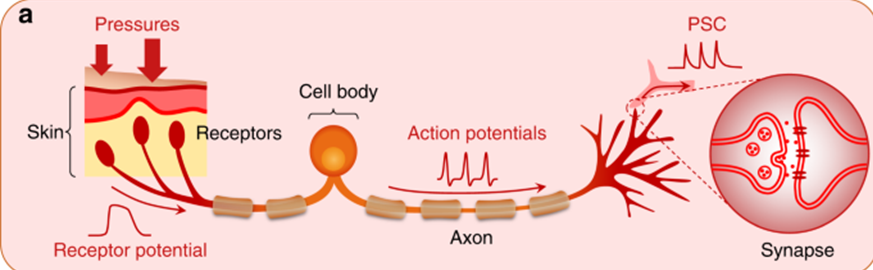
Sensory potentials
instead of NTs input to dendrites we get signals from tactile sensory modalities (such as pressure, stretch, etc) to the receptor. This is what causes the Stretch Reflex
What is neuroplasticity? Examples?
Neuroplasticity (Practice makes perfect)
Changes in synaptic efficacy, neuronal function/structure
Learning and memory; patients change their motor pattern
Examples:
Short term plasticity, reversible
Habituation: Decrease response to a repeated light stimulus
Habituation, getting use to the house smoke alarm going off eventually you don’t hear it.
Sensitization: Increase response to a repeated stimulus
Sensitive to stimulus, bruise starts to hurt/becomes sensitive in that area. Chronic pain
For example: PT should help desensitize a limb so the prosthetic isn’t a noxious stimuli
Long term, learning and memory plasticity
Active/experience dependent: Persistent, long lasting physiologic changes. Increase strength, sprouting and concentrations of neurons NTs.
Reinforcements of a specific pattern: Timing, sequence of movements → reward system, increases will to learn.
Use dependent movement therapies: Increase intensity, increase rep for motor learning. Re-training SCI patients; engages sensory neurons to reconnect communication between feet a brain. Another is body weighted supported treadmill training, constraint induced movement therapy.
Neurotransmitters:
What are ionotropic and metabotropic?
What is the NTs life cycle?
Ionotropic: Positive and negative synaptic inputs convey specific task related info to motoneurons.
Metabotropic: synaptic inputs dramatically impact motoneuron excitability to meet task demands.
Life cycle for NTs:
Synthesis: Location is dependent on specific neuron. fabricated in particular region of brain or presynaptic neuron
Synaptic action: Diffuses through synaptic cleft and binds to receptor on post-synaptic membrane → ionotropic/metabotropic effects in post synaptic neuron
Metabolism: reduce, reuse, and recycle
Diffusion → out of synaptic cleft (recycle)
Breakdown → inactivation by enzymes (reduce)
Reuptake → into pre-synaptic cell (reuse)
What are they types of NTs which associated charges?
Glutamate +
GABA and Glycine -
Acetylcholine AcH +-
Norepinephrine NE +
Serotonin 5-HT +-
Dopamine DA +-
Endorphins
Substance P
What is glutamate function with site of action, transmitters binding effects, and clinical application?
Glutamate +: Important for learning and memory, most common NT in synapse. Regulates development and creation of nerve contacts.
Site of action: Primary, fast, excitatory NT of CNS ~ 50% of synapses
Transmitters binding effects: General neuronal signaling. Facilitate learning and development, especially when binging to NMDA receptor in brain.
Clinical application: Increase levels can cause seizures. Glutamate excitotoxicity can occur in brain injury such as in the case with Tua. Increase concentration of glutamate remaining in synaptic cleft during an ischemic stroke, Post synaptic cell being to become exited to death so to speak. because of slowing energy (decrease O2/glucose)
What is GABA + Glycine function with site of action, transmitters binding effects, and clinical application?
Site of action: Principle inhibitory NT in CNS (GABA: widespread. Glycine: brainstem and spinal cord)
Transmitter binding effects: Inhibition of post-synaptic neuron (increase in Cl-). Sedation, anti anxiety, anti-seizure, sleep inducing (GABA). Important for shaping motor commands level of spinal cord
Clinical application: Baclofen, gabapentin, benzodiazepines, alcohol enhance effects of GABA. Typically given to CP and stroke patients because of the ischemic attacks, helps decrease glutamate action.
What is ACETYLCHOLINE function with site of action, transmitters binding effects, and clinical application?
ACETYLCHOLINE + (?): Major NT in PNS; muscle contraction
Site of action and → associated transmitter binding effects
Somatic: + in all NMJ → Skeletal contraction
Autonomic: Ionotropic effects at pre ganglionic receptors → facilitation of post ganglionic autonomic neurons
Autonomic: metabotropic effects at parasympathetic post ganglionic muscarinic receptors → increase parasympathetic actions; increase rest actions
Also present in CNS:
Cerebral cortex and ventral striatum (basal ganglia and reward system) → cognitive arousal and feelings of reward
Clinical application
Myasthenia gravis: Autoimmune destruction of AcH receptors at NMJ causing weakness
Botox: Inhibits AcH release at NMJ. Used for hypertonia
Nicotine binds to ACH receptors in ventral striatum causing the pleasurable and addictive feelings
Alzheimer’s: number of AcH receptors in cortex diminish
What is Norepinephrine function with site of action, transmitters binding effects, and clinical application?
Site of action
CNS: cerebral cortex, limbic system, spinal cord
PNS: sympathetic NS
Transmitter binding effects
Cortex, limbic system: control of mood
Spinal cord: increase excitability of alpha motor neuron and group ll sensory afferents
PNS: sympathetic effects (fight/flight)
Clinical application
Important in generation of spasticity and hyperreflexia after NS injury
May have vole in chronic pain / central sensitization (partial target of SNRIs drugs)
Role in Parkinson's disease
What is Serotonin function with site of action, transmitters binding effects, and clinical application?
Site of action
Brain and spinal cord (from raphe nuclei through cortex)
Transmitter binding effects
Brain: Control of mood, pain perception, increase arousal
Spinal cord: increase excitability of ventral horn; decrease excitability of dorsal horn
Clinical application
Alpha motor neuron w metabotropic effects, important in amplifying the effect of ionotropic input → motor command
Important in generation of spasticity hyperreflexia after NS injury
Lack of 5 HT after Spinal cord injury results in spasms due to adaptive hyperactivity of receptors on alpha motor neuron
May have role in chronic pain/central sensitization (partial target of SNRI drugs)
Role in Parkinson's disease (Increase in 5-HT can help move and groove on ischemic stroke patients
What is Dopamine function with site of action, transmitters binding effects, and clinical application?
Site of action
Basal ganglia, limbic system, frontal lobe
Transmitter binding effects
Control movements, feelings of pleasure, reinforcement of behaviors (including addiction), decision making, planning
Clinical application
Parkinson’s disease: Loss of dopaminergic neurons (primarily where they are synthesized in substatia nigra of brainstem) is major contributor to motor deficits (tremors). L-DOPA drug increase dopamine. If too high dose, lead to involuntary movements. Too high may also lead to addictive behaviors.
Amphetamines and cocaine increase/prolong release
What is Endorphins function with site of action, transmitters binding effects, and clinical application?
Site of action
CNS and spinal cord
Transmitter binding effects
Inhibition of pain signaling (Endogenous opioids)
Clinical application
Decrease signaling and pain perception
Descending pain modulation system
Pharmacologic agonists; morphine, heroin, oxycodone, etc
What is Substance P function with site of action, transmitters binding effects, and clinical application?
Site of action
PNS: Released by nerve endings in skin, muscles, joints
CNS: Brainstem, cortex, hypothalamus, amygdala
Transmitter binding effects
Produce pain sensation
Involved with mood, cortical perception of pain
Clinical application
Levels of substance P are excessive in some pathological pain conditions
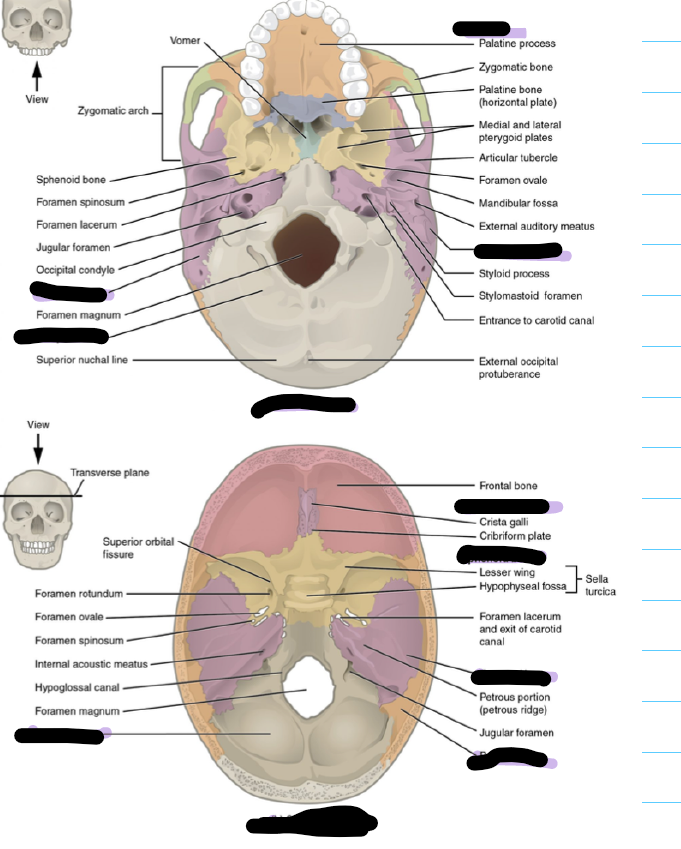
What view is this?
Superior
What view is on the left and right?
Anterior and posterior
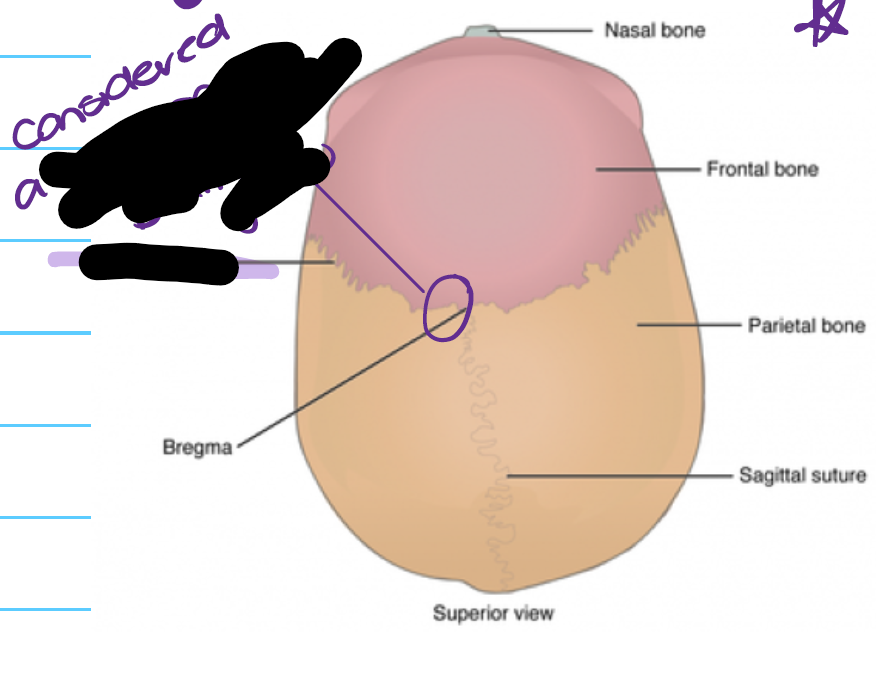
Label. This is considered what for babies?
Coronal suture. Considered a soft spot in babies to allow brain to grow
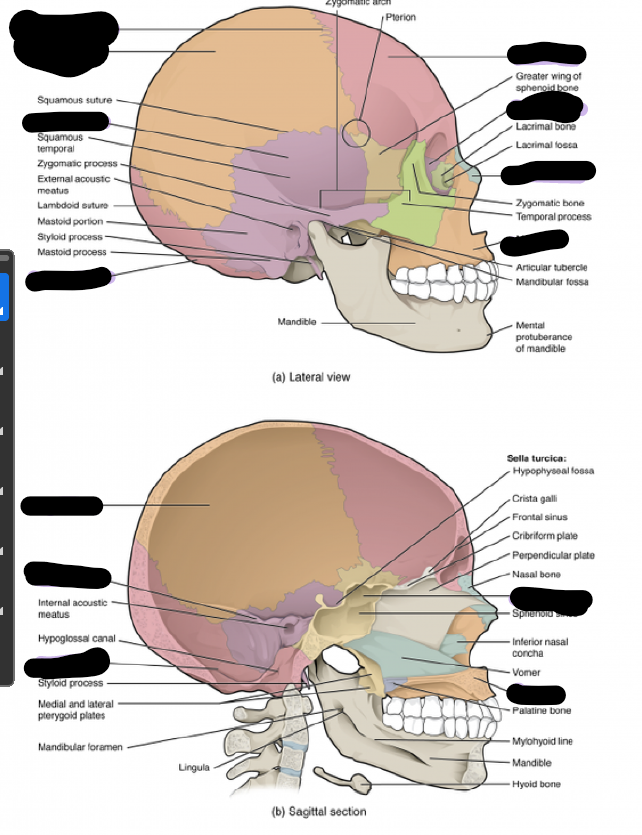
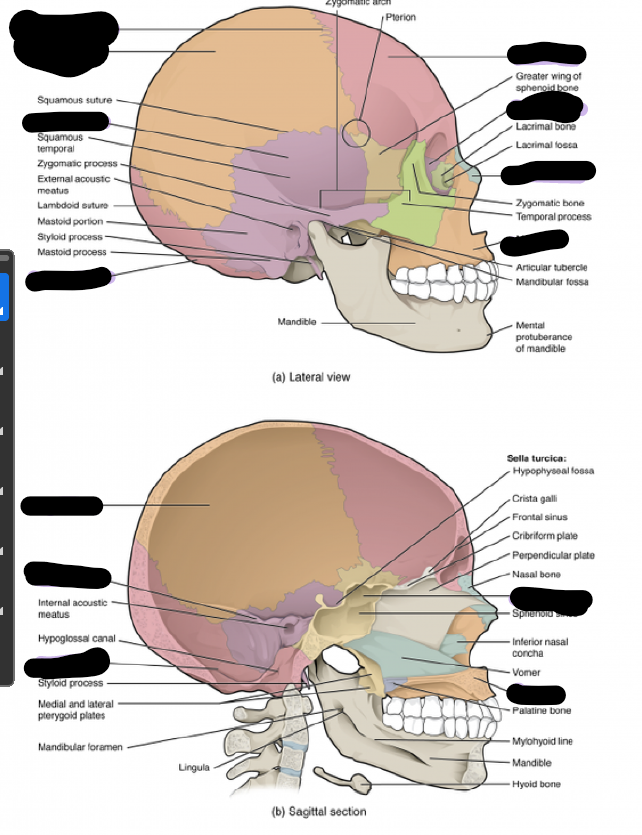
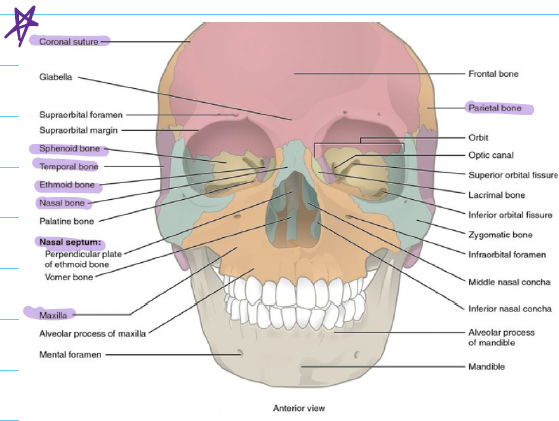
Fill in the blanks.
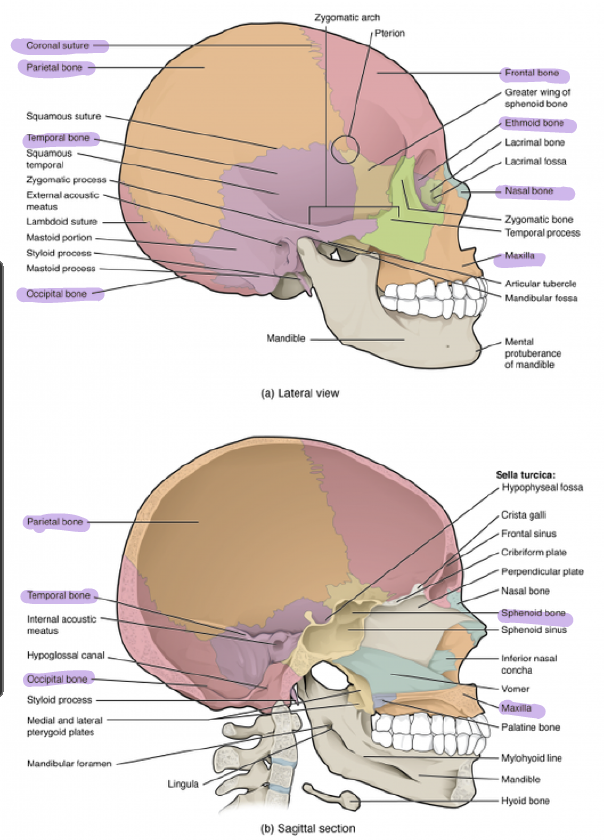
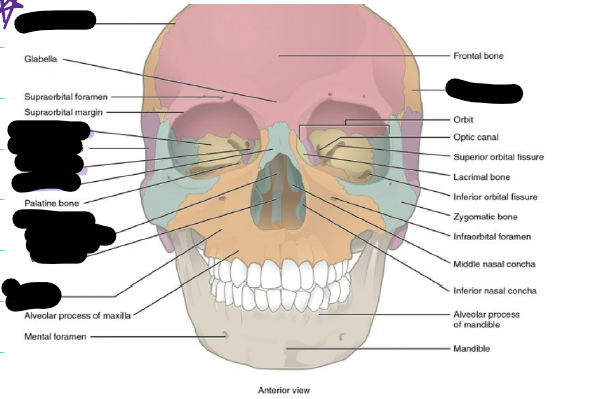
Label
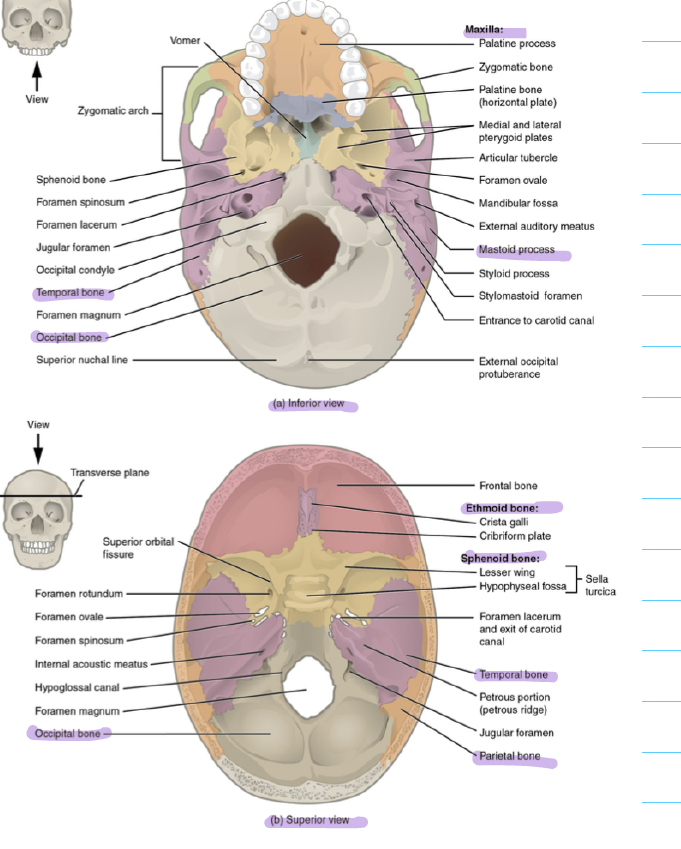
Label and state which view is this
Coronal
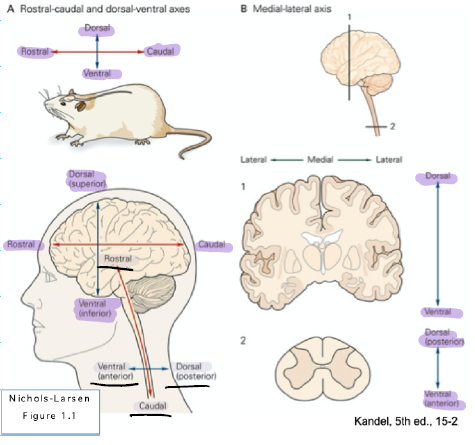
Orientation of direction in brain vs spinal cord
Rostral vs caudal
How does dorsal and ventral differ for the brainstem/spinal cord vs the actual brain
Rostral: towards the nose
Caudal: towards the tail
In the human brainstem/spinal cord
Dorsal = posterior
Ventral = anterior
In the human brain
Dorsal = superior
Ventral = inferior
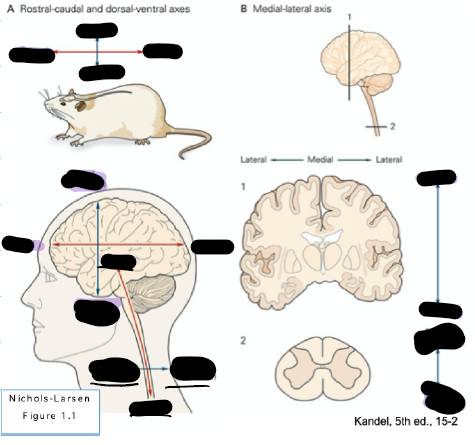
Label each based on the correct axis (dorsal, ventral, rostral, caudal)
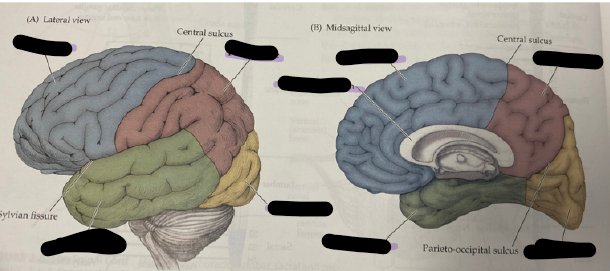
label the lobes
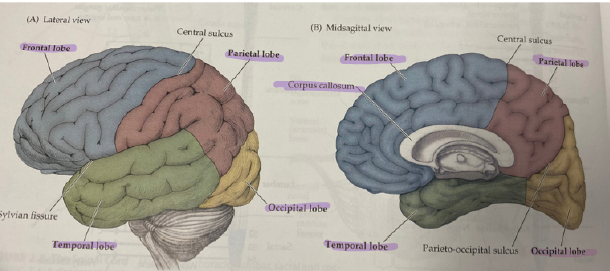
For each of the four lobes state what they do
Frontal
Function: Executive functioning, decision making
Impairment: Ataxia, impulse control
Parietal lobe
Function: Temperature regulation, touch sensation/pain, proprioception/spatial awareness
Impairment: Fall risk
Occipital lobe
Function: vision, perception
Temporal lobe
Auditory processing
Broca’s (actually talking) and Wernicke’s (understanding speech)
Memory storage
Tailors to motion and motivation
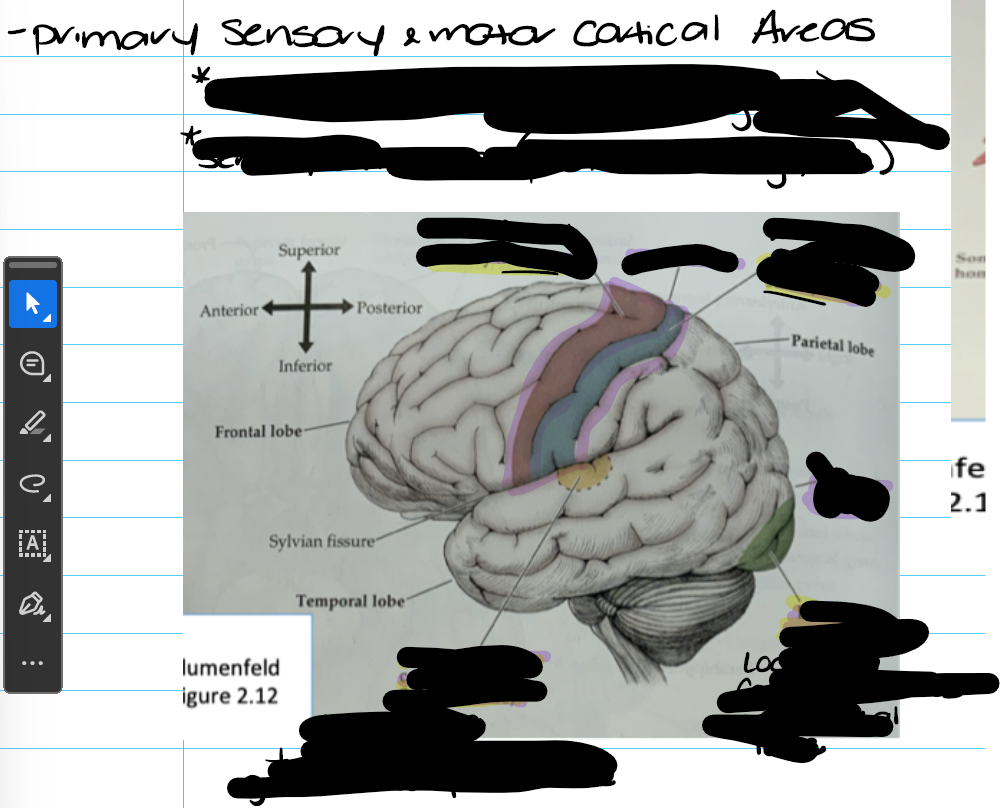
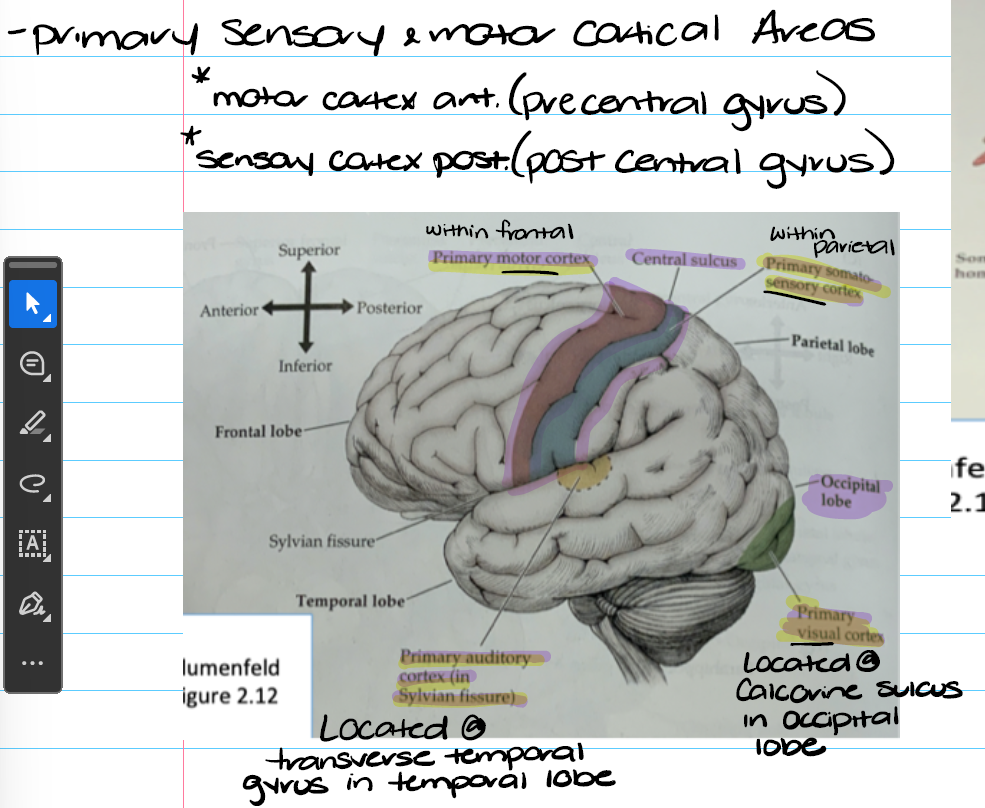
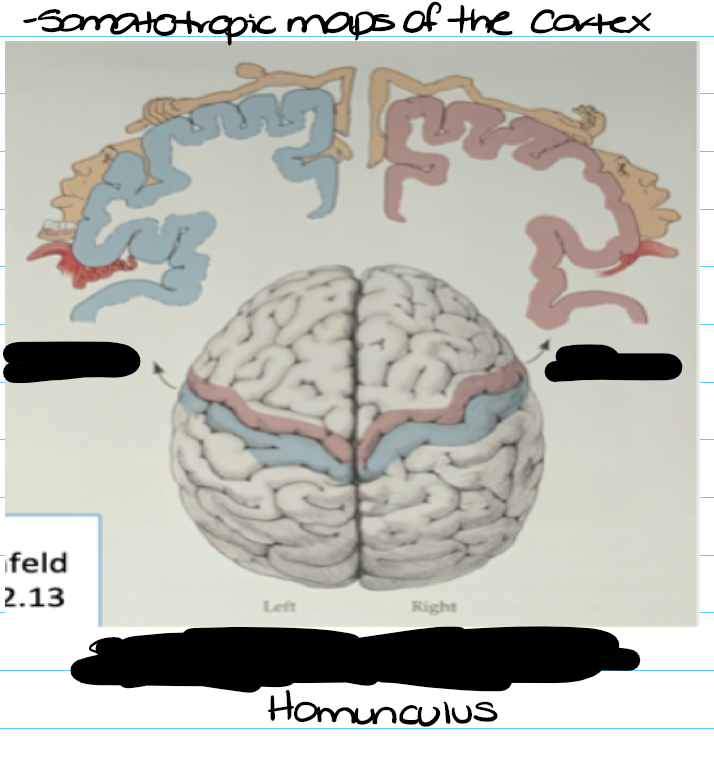
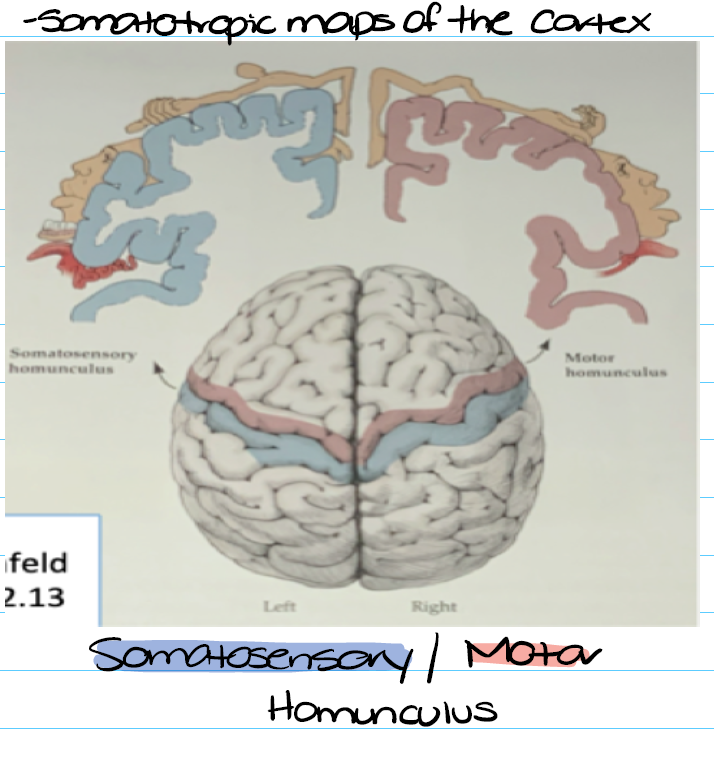
Primary motor is in the precentral gyrus in the frontal lobe: Motor control ect
Primary sensory is in the postcentral gyrus and in the parietal lobe: Processes sensation
Primary visual cortex: Located in the calcarine sulcus in the occipital lobe: vision
Primary auditory cortex located in the Transverse temporal gyrus in the temporal lobe: auditory interpretation
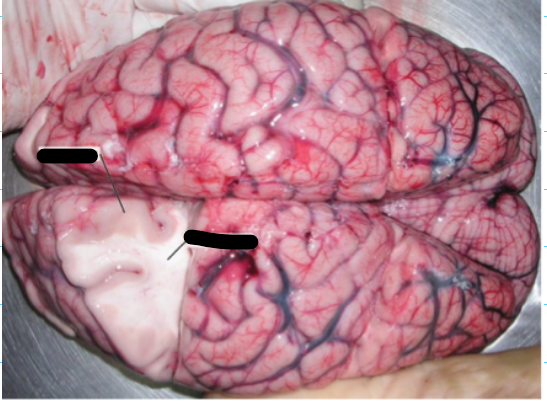
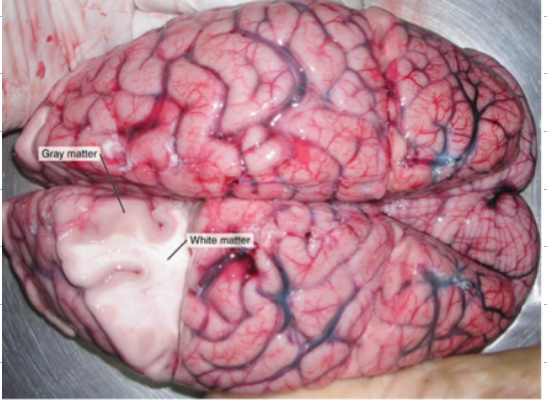
What is grey matter and what is its cortical and subcortical structures?
Grey matter
Neuron cell bodies
Synapses where white matter axons connect with other neurons at the nucleus
Glial cells (support cells)
Cortical structures
Lobes
Specific gyri within lobes
Subcotial structures
Diencephalon (Thalamus and hypothalamus)
Limbic system
Basal ganglia (In telencephalon; motor)
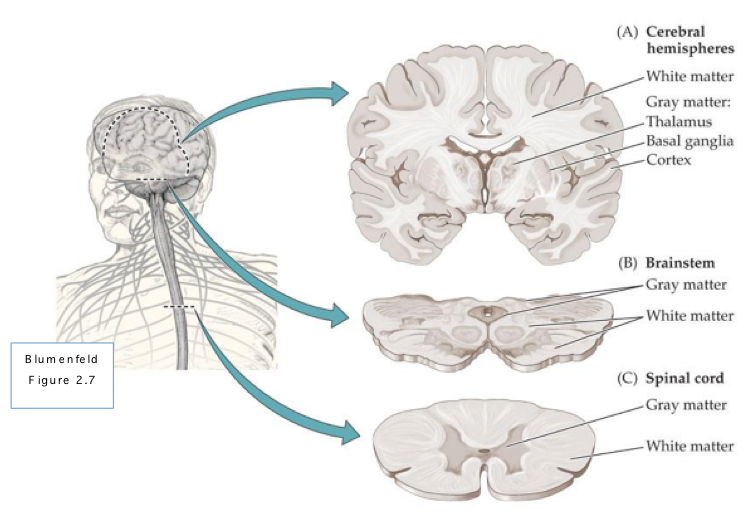
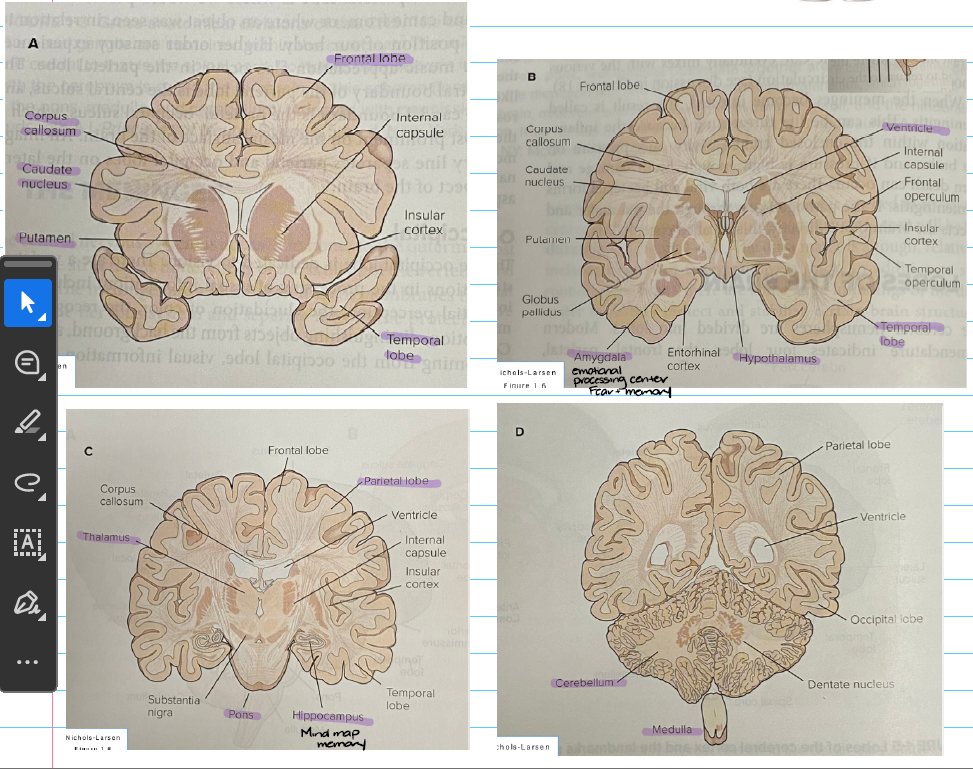
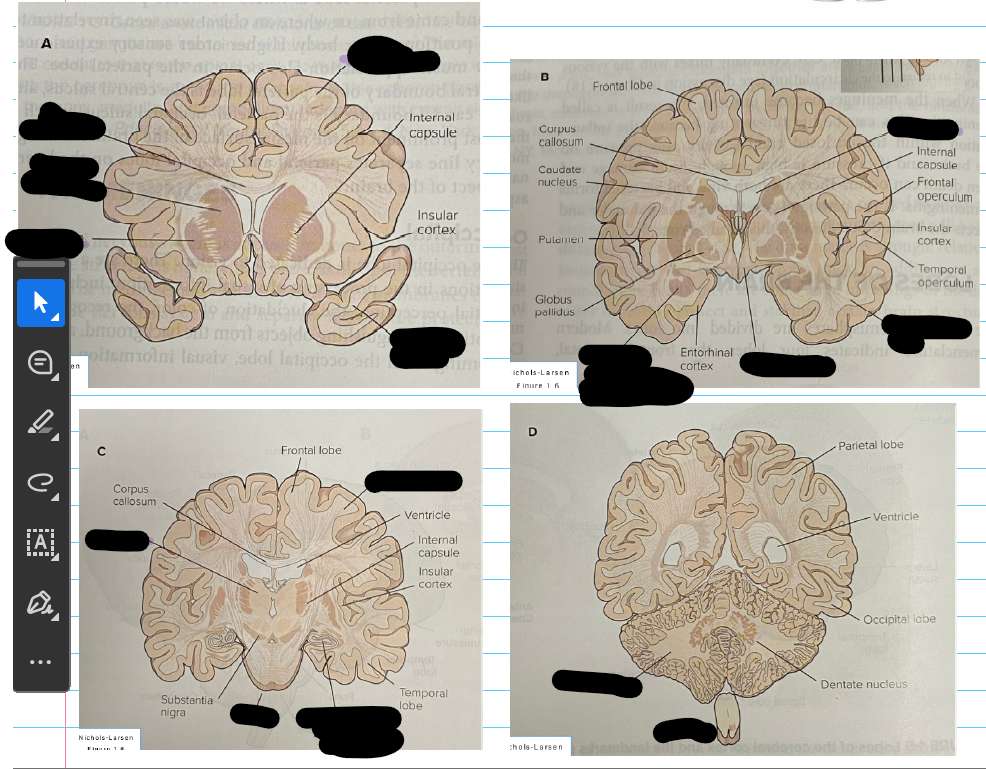
Amygdala: emotional processing center, regulates fear and memories associated with emotions
Hippocampus: critical for memories
What is white matter and its categories of fibers ( (Understand where they connect)?
White matter: Neuron axons surrounded by myelin
Categories of fibers
Projection fibers: Connect cortical, subcortical/brainstem/spinal structure
Ascend from spinal cord and subcortical structures to cortex (Green)
Descend from cortex to spinal cord, brainstem, basal ganglia, thalamus (Red)
Travels through internal capsule
Travels long distances
Commissural fibers (Between hemispheres): Connect same area between hemispheres like sticky give