Pathology flashcards
1/91
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
92 Terms

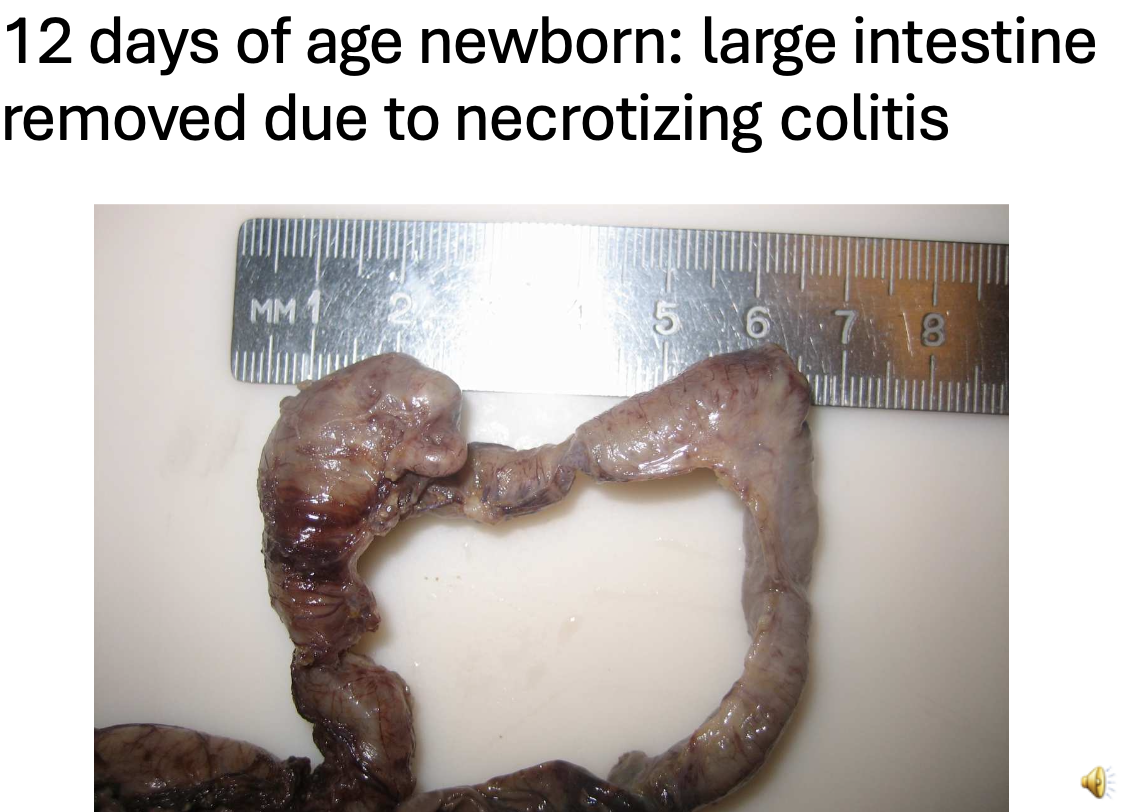
Congenital small intestinal atresia with enlargement, purulent inflammation and necrosis
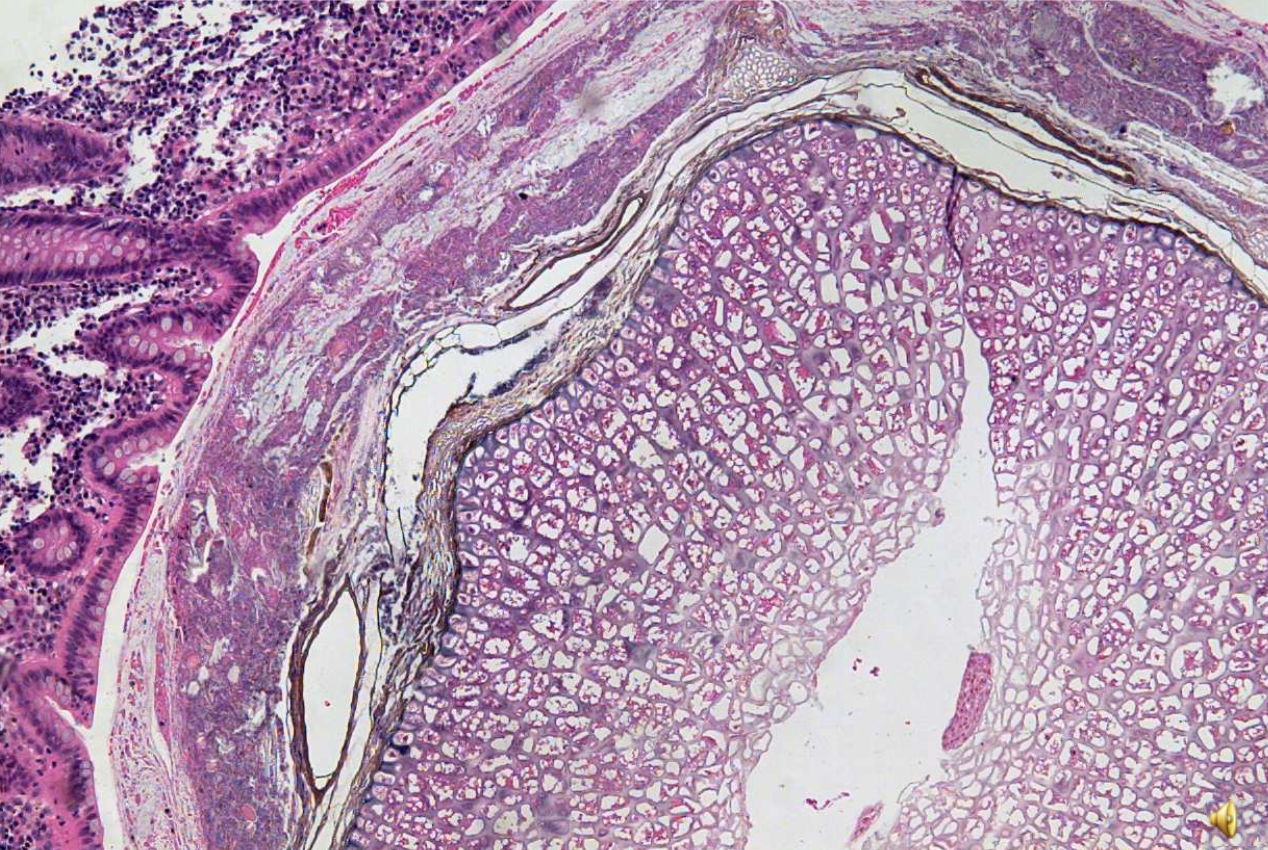
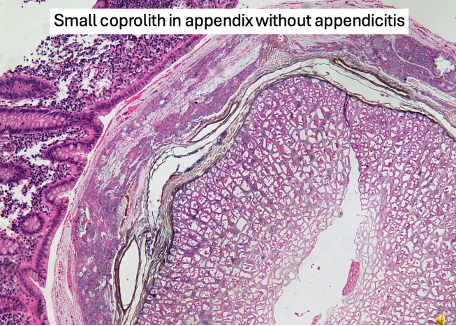
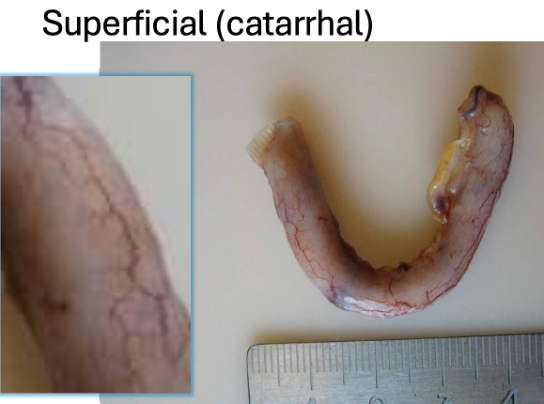
Epithelium is intact and no inflammatory cells intraepithelial
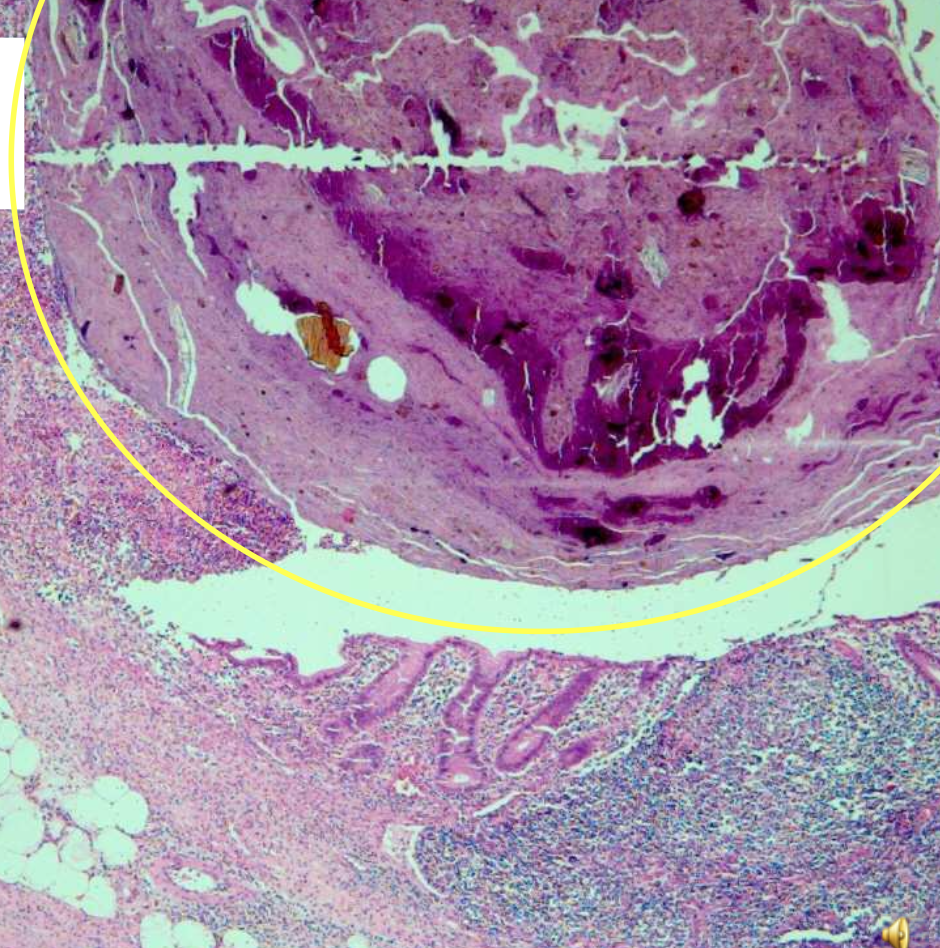
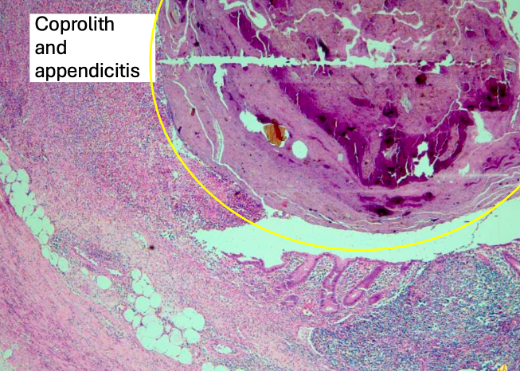
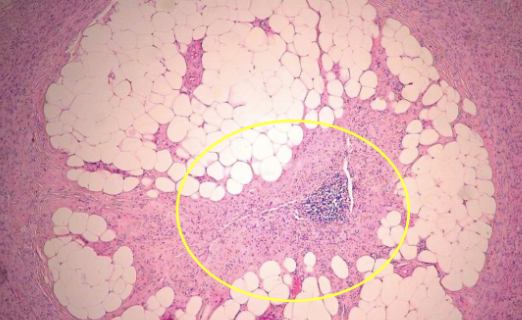
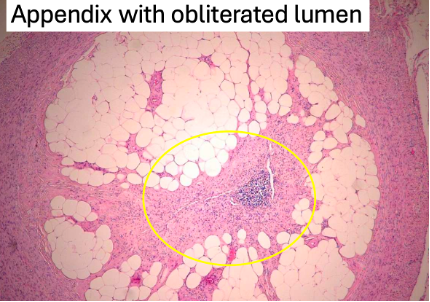
Inflammation started due to large coprolith → ischemia, epithelium disclamation and inflammation in deep layers of appendix

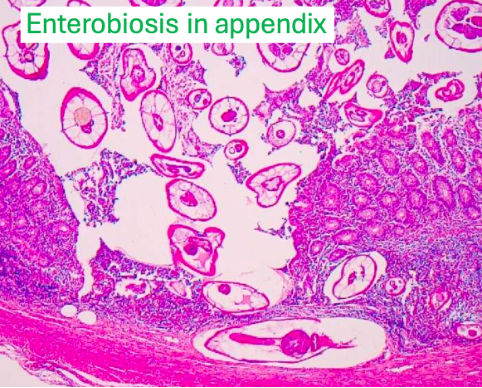
Enterobiosis vermicularis penetrate through mucosa into deep layers → cause inflammation
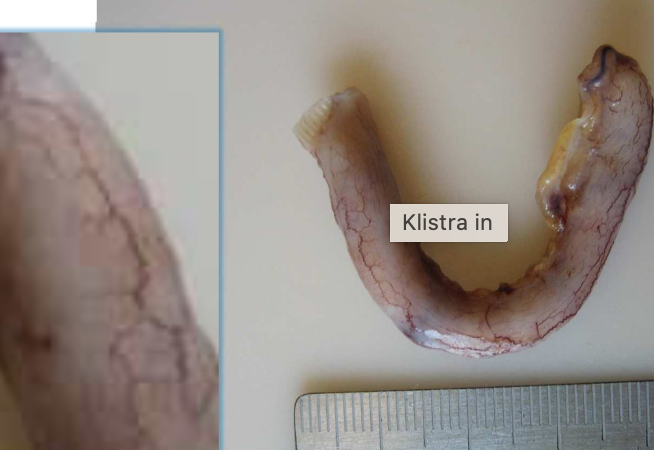
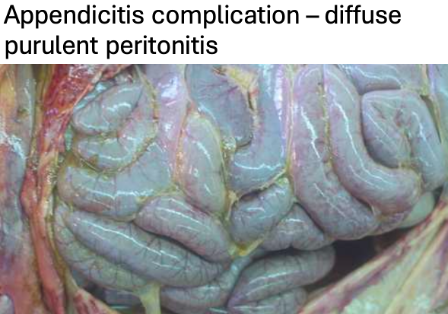
Hyperaemic vessels

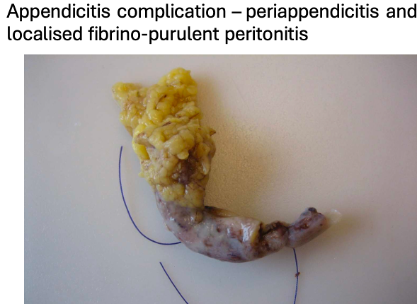
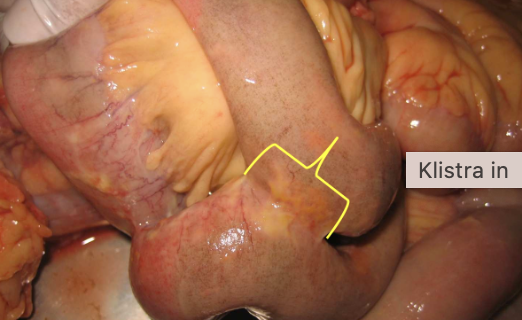
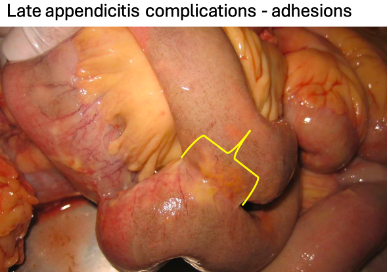
Purulent exudate on surface of appendix + inflammation
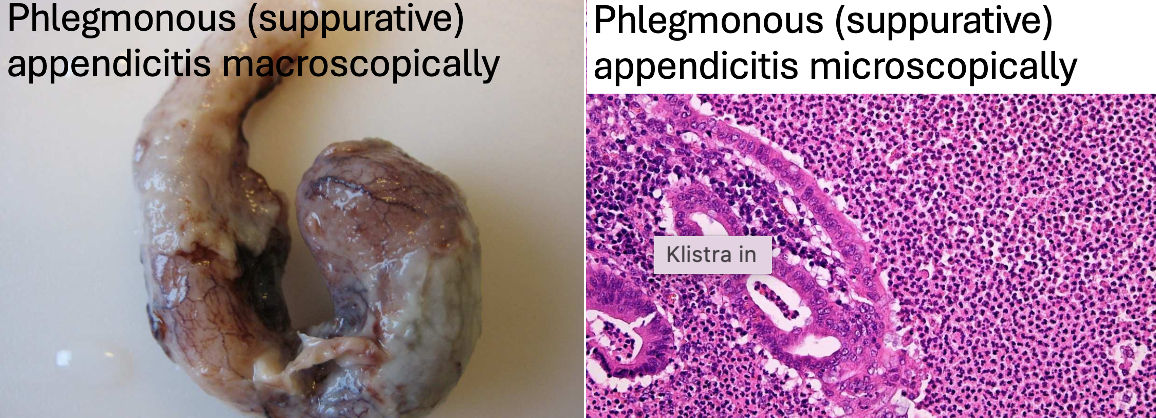
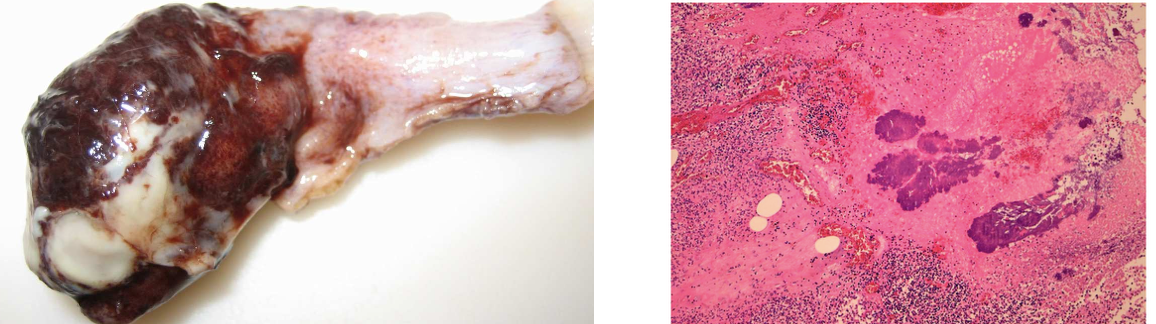
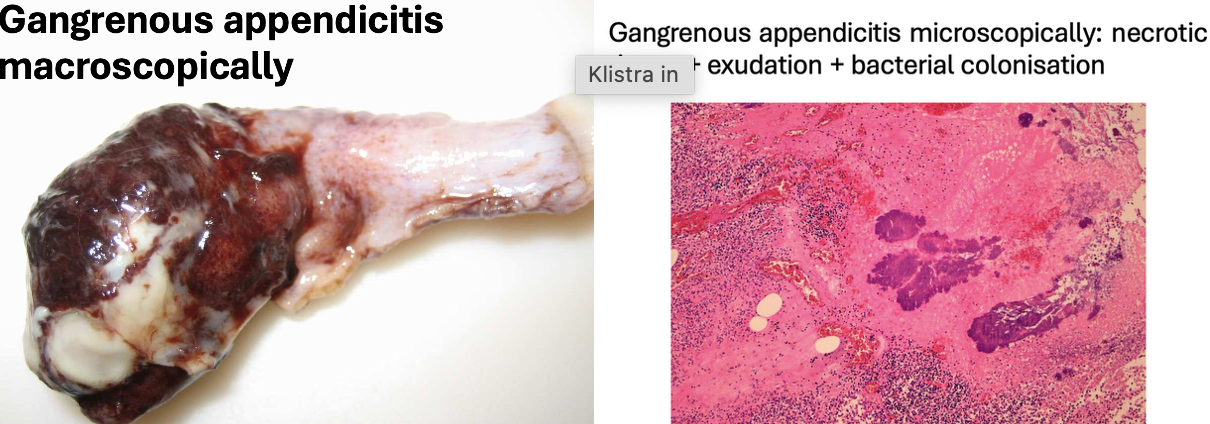
Discoloration of appendix and purulent exudate around and inside appendix.
No muscular or submucosal layer is visible → only necrosis


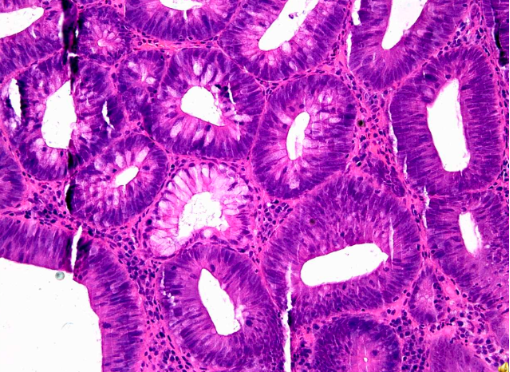
Adenomas – tubular structure of neoplasm
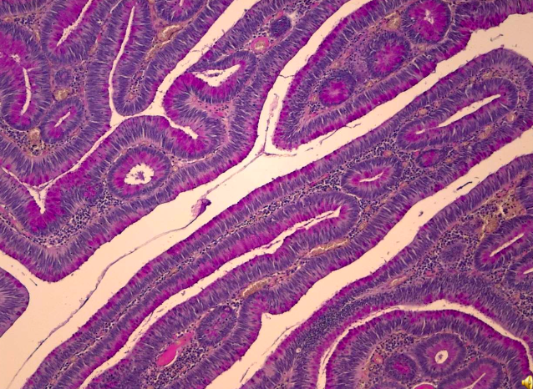
Tubular papillary carcinoma
Tubular and papillary structures formed from neoplastic epithelial cells from GI tract
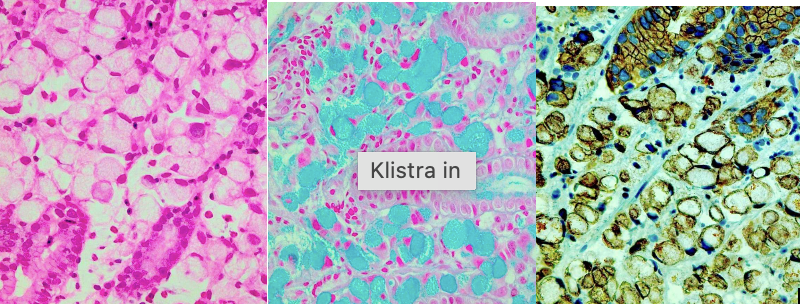
Explain all three pictures
Cyanate ring carcinoma
Ø Formed of neoplastic cells from GI tract.
Ø Alcion blue in the middle where we see mucus inside cells.
Ø Immunohistochemical reaction (right) – positive for cytokeratin’s → shows that they are carcinoma epithelial origin.
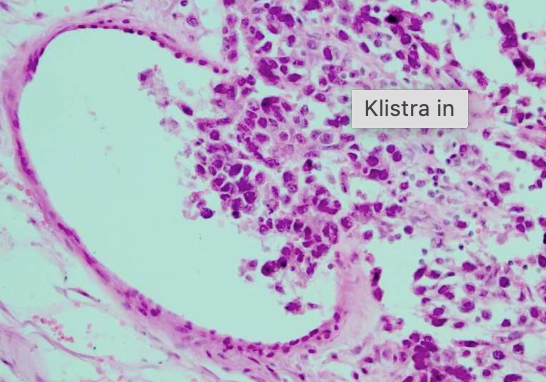
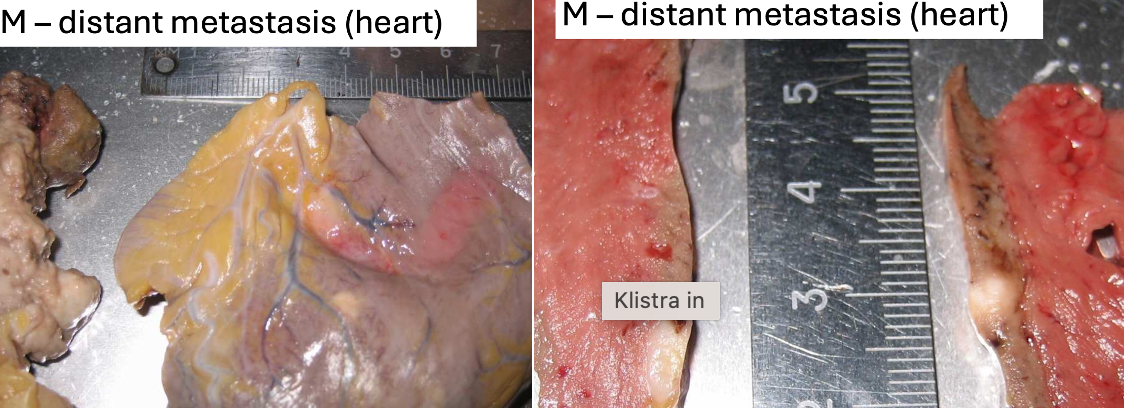
Ø Whitish region near coronary artery – metastasis:
1. Caused obstruction of BV → infarction.

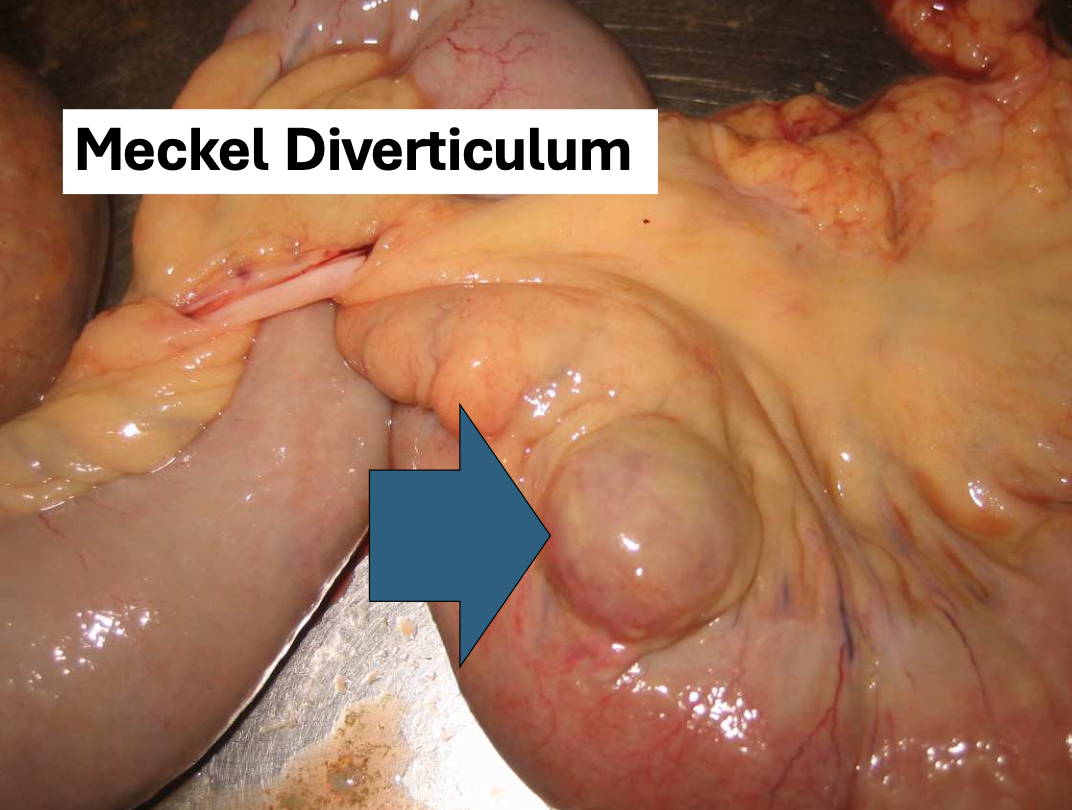
Ø Congenital outpouching in the small intestine.
1. Usually located in the ileum, that results from a failure of the omphalomesenteric duct (also known as the vitelline duct) to fully close during foetal development.

Mucosa is red, ulcerated due to UC
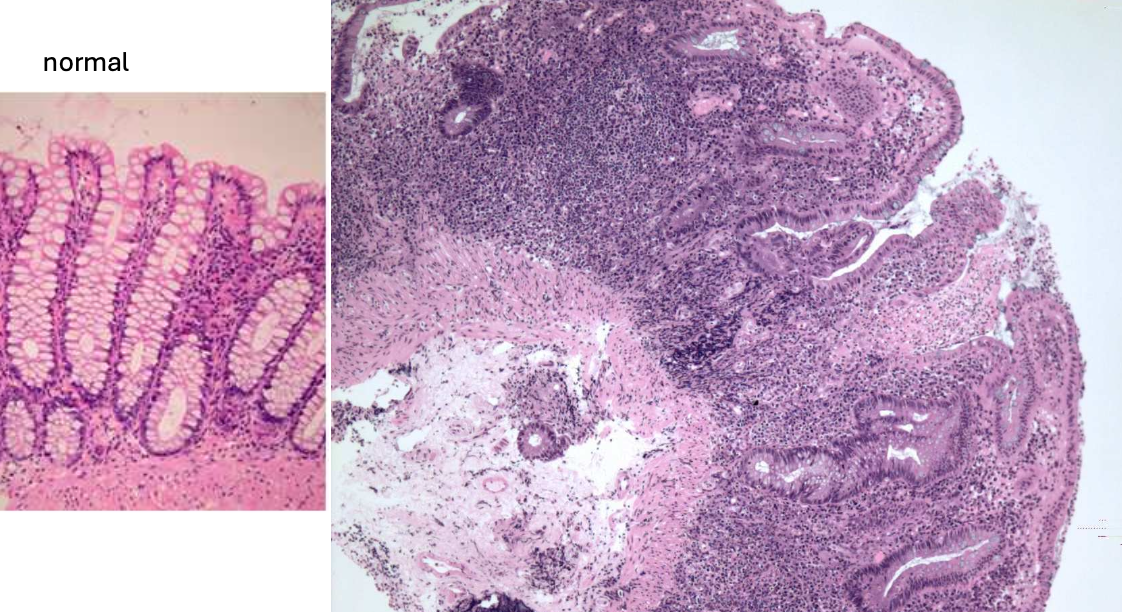
Ulcerative colitis
1. Architecture of mucous gland is distorted, branched, deformed.
2. Infiltration of leukocytes.
3. Centre with ulceration.
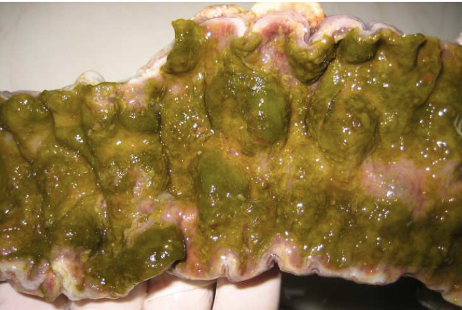
Pseudomembranous colitis:
Damaged mucosa covered with exudate with greenish colour.
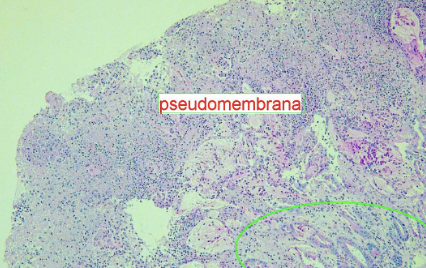
Pseudomembranous colitis:
1. Green – rest of mucous glands.
Other regions with necrotic debris due to inflammation and exudate