PANCE Blueprint Neurology - All Smarty PANCE neurology flashcard lesson sets combined (Smarty PANCE)
1/395
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
396 Terms
What is a concussion?
Injury to the body or head that results in a force to the brain, it can be accompanied by transient loss of consciousness; but not always.
Concussion vs. Mild TBI
The term "concussion" is often used in the medical literature as a synonym for mild traumatic brain injury (mild TBI or mTBI). Mild TBI, or concussion has a GCS of 13 to 15
What are the symptoms of a concussion?
Headache, dizziness (feeling off balance), confusion, retrograde/antegrade amnesia, and blurred vision. Symptoms typically resolve within 7 to 10 days postinjury.
What are the indications for CT scan of the head in a patient with a suspected concussion?
Use validated clinical decision rules (such as the PECARN decision tool) to determine if imaging is warranted - No routine imaging of pediatric patients with mTBI. Indications for CT scan include prolonged loss of consciousness (>1 minute), persistent headache, altered mental status, repeated episodes of vomiting postinjury, history of repeated head injury/severe mechanism, or signs on physical examination of basilar skull fracture.
What percent of CT scans in mild TBI are abnormal?
Approximately 10 percent of CT scans in mild TBI are abnormal, showing mild subarachnoid hemorrhage, subdural hemorrhage, or contusions. MRI is more sensitive than CT scan, showing abnormalities in approximately 30 percent of patients with normal CT scans
What is the acute management of patients with concussion?
Rest, symptomatic treatment (for headaches and nausea), no contact sports, and decreased exposure to technology (television, cellular phones, computers, and electronic games). Athletes should be symptom free while at rest and exercise before returning to sports activities. Many states have laws requiring the patient be reevaluated and cleared before starting sports activities, and at times a stepwise progress for returning to activities is followed.
Athletes who suffer a concussion during their activity ______________ resume their activity the same day after normal physical exam and imaging findings?
Any child or adolescent with a suspected sport-related concussion should be removed from further competition that day. If a concussion is diagnosed, the athlete should not return to play until a full recovery is evident.
Patients with concussion should be admitted to the hospital if their Glasgow coma scale is less than ____?
Patients with concussion should be admitted to the hospital if their Glasgow coma scale is less than 15.
What is post concussion syndrome?
Symptoms of headache, dizziness, difficulty concentrating, and fatigue that begins days to weeks after a head injury and can last weeks to several months
What percent of patients with mild traumatic brain injury (TBI) will experience some symptoms of PCS?
30 to 80 percent of patients with mild traumatic brain injury (TBI) will experience some symptoms of PCS
Which patients with PCS should have an MRI?
Patient with PCS who have not had an MRI and have disabling complaints should have a brain MRI to exclude more serious pathology that would identify either a worse prognosis or an alternative cause for their symptoms.
For patients with post concussion syndrome complaining of headache and dizziness, what is the first-line treatment?
Treatment is symptomatic treat headaches like migraines with PRN analgesics, psychotherapy
Recovery time from post concussion syndrome?
Most patients recover quickly, within several weeks. A minority have prolonged disability
A GCS of 13 to 15 indicates what
Mild TBI, or concussion has a GCS of 13 to 15
A GCS of 9-12 indicates what?
Moderate TBI has a GCS of 9 to 12
A GCS of 8 or less indicates what?
Severe TBI has a GCS of 8 or less.
When is a brain CT indicated for TBI?
The brain CT is done for moderate and severe TBI, as well as in mild TBI where the individual has a worsening headache, persistent confusion, a focal neurological deficit, or is on anticoagulation therapy like warfarin
Treatment of traumatic brain injury?
General measures for treating TBI include lowering the ICP by elevating the head of the bed to 30 degrees, sedation, intubation and hyperventilation in order to achieve a partial pressure of carbon dioxide or PaCO2 between 35 and 45 millimeters of mercury, osmotic diuresis with mannitol or hypertonic saline, and finally if all else fails, a decompressive craniectomy. Specific lesions identified on CT scan such as epidural and subdural hematomas should be identified and evacuated
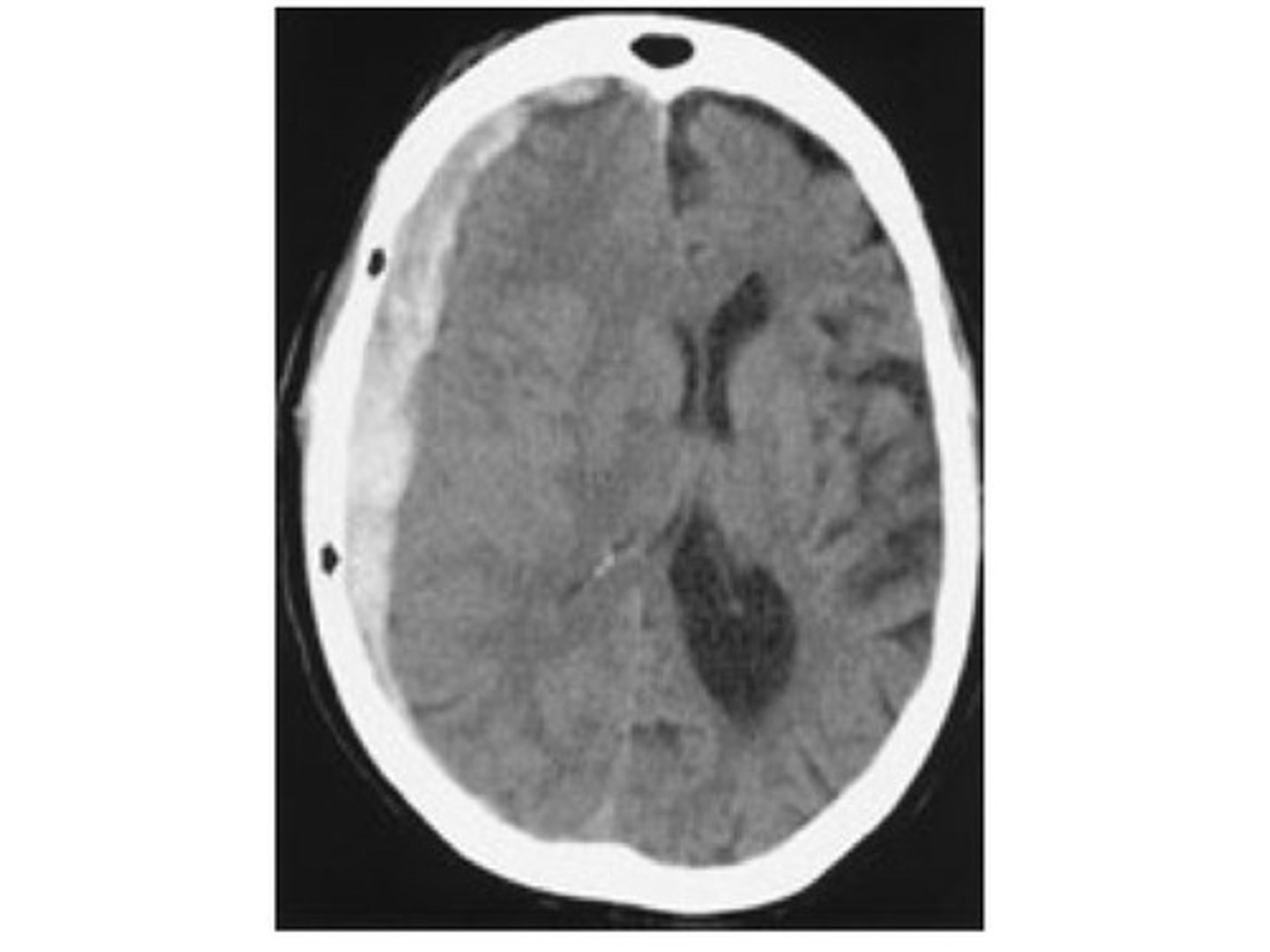
On CT appear as a convex, “lens-shaped” hyperdense collection of blood that does not cross the suture lines.
Epidural hematomas appear as a convex, "lens-shaped" hyperdense collection of blood that does not cross the suture lines.
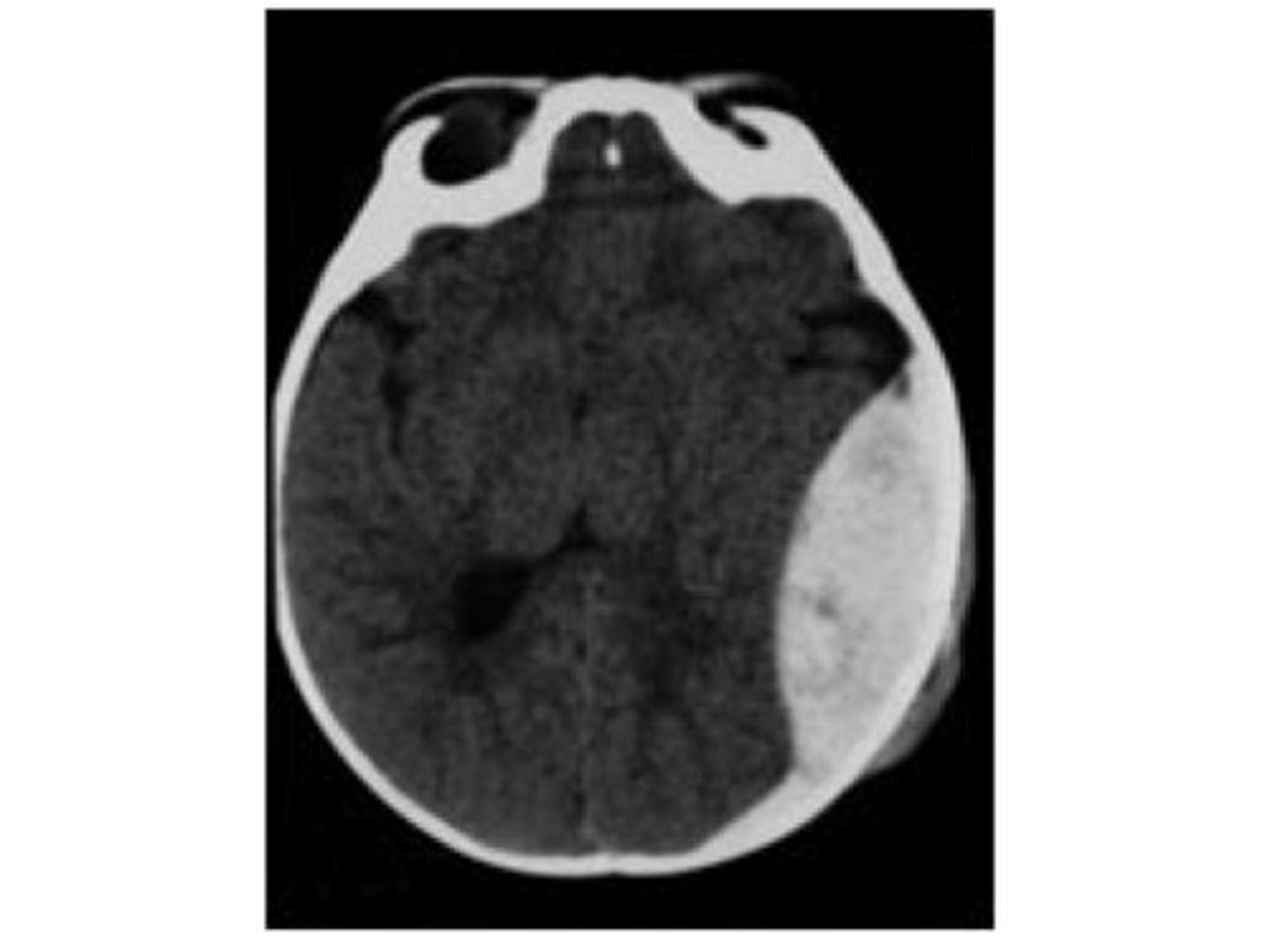
On CT appear as a concave, "crescent-shaped" density that crosses the suture lines.
Subdural hematomas appear as a concave, "crescent-shaped" density that crosses the suture lines.
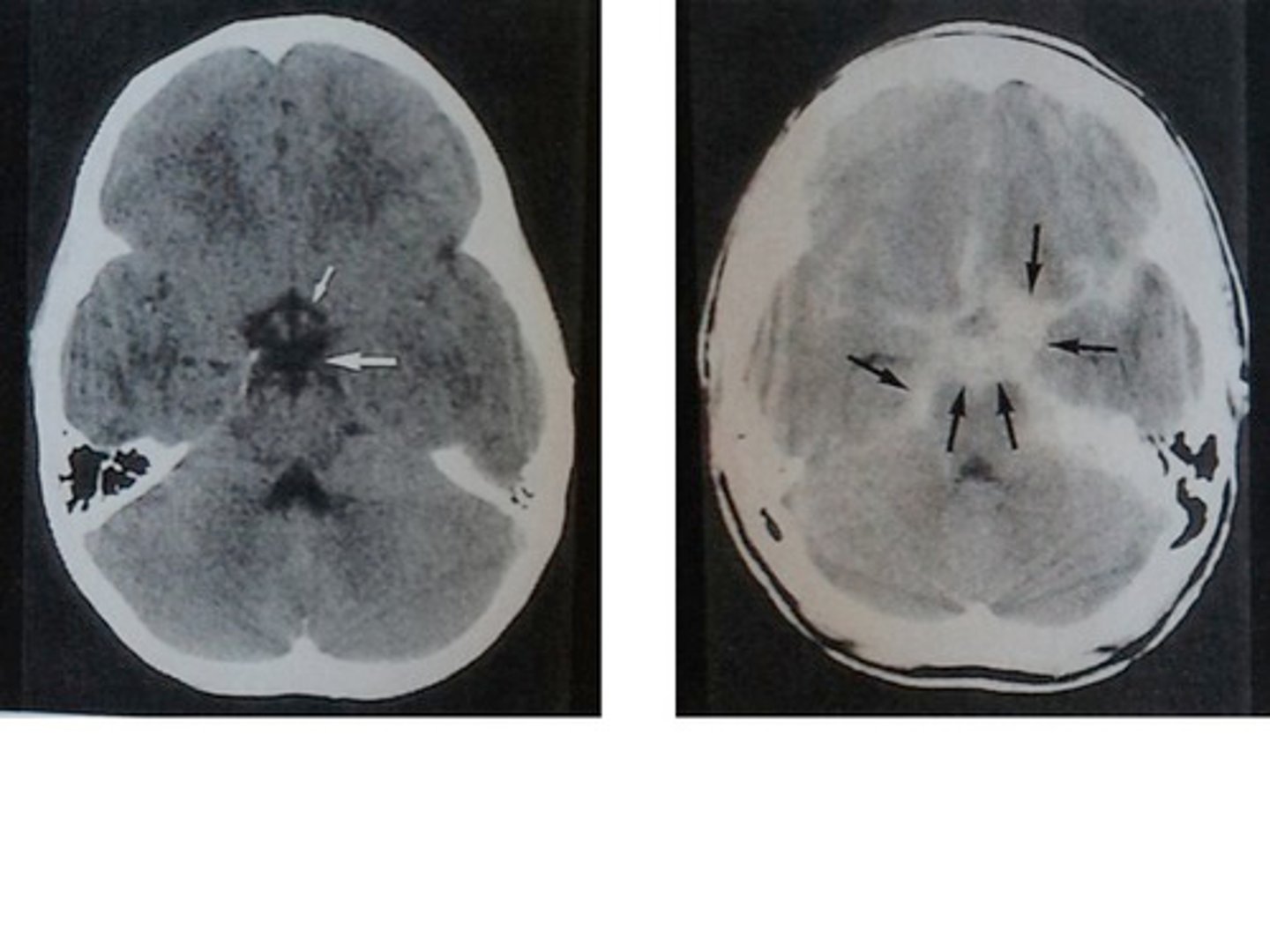
On CT is seen as blood in the ventricular cisterns, interhemispheric fissures and within the sulci.
Subarachnoid hemorrhage is seen as blood in the ventricular cisterns, interhemispheric fissures and within the sulci.
What two pre-hospital factors dramatically increase the mortality of patients suffering a mild or moderate traumatic brain injury (TBI)?
Hyperventilation and poorly performed intubation
What are the clinical indicators for performing pre-hospital or emergency department hyperventilation, before invasive ICP monitoring, in a patient experiencing a traumatic brain injury (TBI)?
Development of signs or symptoms of herniation; unilateral dilated pupil, asymmetric motor examination, or a declining GCS.
How does cranial nerve I deficit present?
Loss of smell - CN I = Olfactory nerve
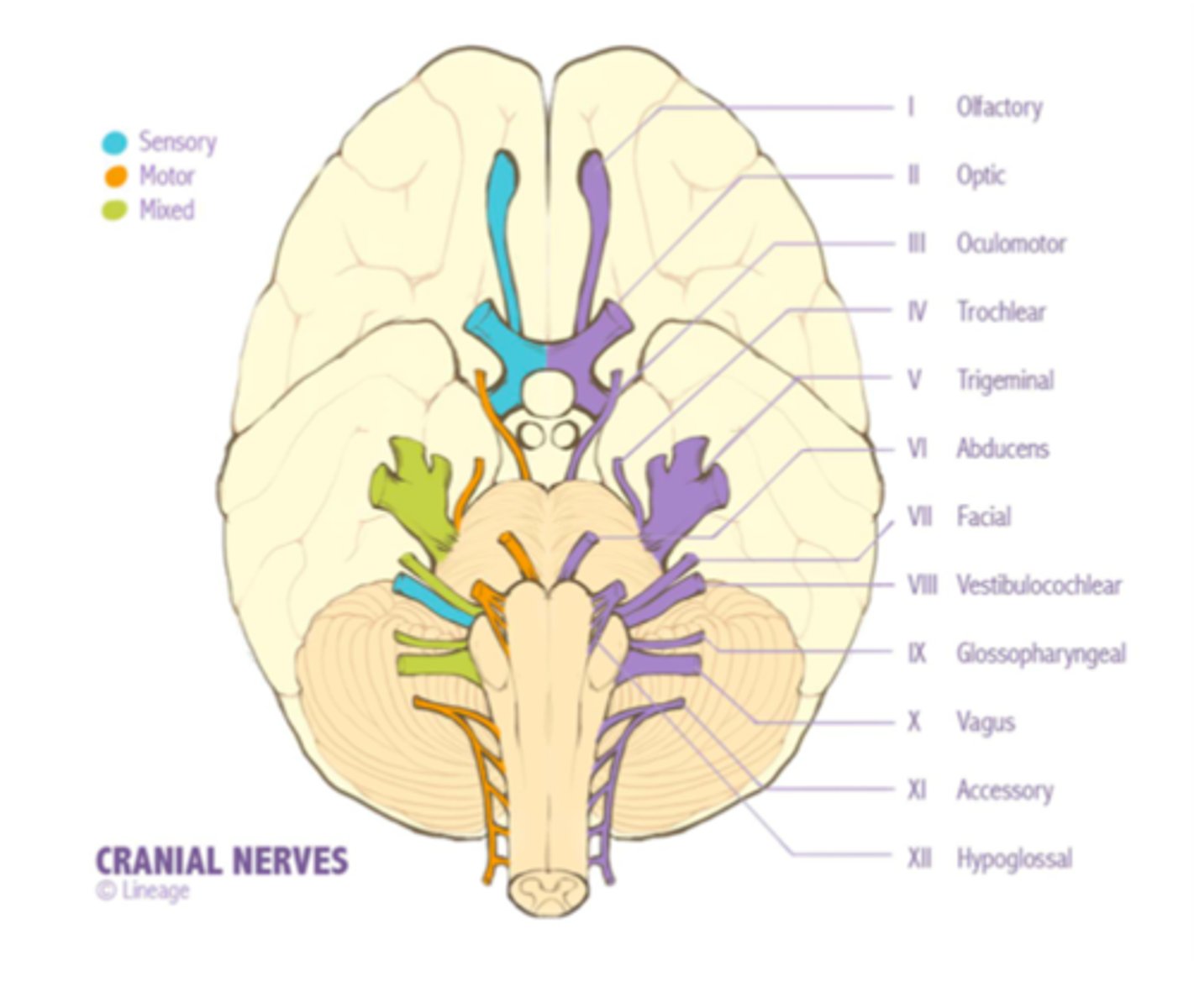
How does cranial nerve II deficit present?
Partial or complete blindness - CN II = Optic nerve
How does cranial nerve III deficit present?
Outward and downward deviation of the eye - Ptosis of the eyelid - Dilation of the ipsilateral pupil in complete palsy -CN III - Oculomotor nerve
How does cranial nerve IV deficit present?
Vertical diplopia - CN IV = Trochlear nerve
How does cranial nerve V deficit present?
Anesthesia of the forehead - Corneal drying - Decreased salivation - CN V = Trigeminal nerve
How does cranial nerve VI deficit present?
Medial turning of affected eye - CN VI = Abducens nerve
How does cranial nerve VII deficit present?
Complete or partial paralysis of the face - CN VII = Facial nerve
How does cranial nerve VIII deficit present?
Positional vertigo - Tinnitus - Rarely hearing loss - CN VIII = Vestibulocochlear nerve
How does cranial nerve IX deficit present?
Dysphagia and dysarthria - CN IX = Glossopharyngeal nerve
How does cranial nerve X deficit present?
Focal: Aphonia dysphagia dysarthria - Systemic: (cardiac and GI most affected) - CN X = Vagus nerve
How does cranial nerve XI deficit present?
Weakness with turning of head - CN XI = Spinal accessory nerve
How does cranial nerve XII deficit present?
Weakness on the ipsilateral side and protrusion of the tongue toward the affected side - CN XII = Hypoglossal nerve
A group of progressive, invariably fatal, conditions that affect the brain are caused by the accumulation of misfolded prion proteins giving the brain a "spongy" appearance?
Spongiform encephalopathy
Diagnosis of spongiform encephalopathy?
Lumbar puncture ↑ levels of 14-3-3 protein. Definitive diagnosis with brain biopsy
What is Creutzfeldt-Jakob disease (CJD)?
CJD is classified as a transmissible spongiform encephalopathy (TSE) along with other prion diseases that occur in humans and animals.
How does bovine spongiform encephalopathy (mad cow disease) relate to humans?
Bovine spongiform encephalopathy (BSE), commonly known as mad cow disease, is an incurable and invariably fatal neurodegenerative disease of cattle. Symptoms include abnormal behavior, trouble walking, and weight loss. Later in the course of the disease the cow becomes unable to function normally. The time between infection and onset of symptoms is generally four to five years. Time from onset of symptoms to death is generally weeks to months. Spread to humans is believed to result in variant Creutzfeldt-Jakob disease (vCJD)
Syndrome of acute or subacute encephalopathy that is associated with elevated anti-thyroid antibody titers?
Hashimoto encephalopathy (HE)
Diagnosis of Hashimoto encephalopathy?
The presence of elevated antithyroid antibody titers and the exclusion of other causes of encephalopathy support the diagnosis of HE
Treatment of Hashimoto encephalopathy?
Treated with corticosteroids
A neurological disorder induced by thiamine, vitamin B1, deficiency. This is the most important encephalopathy due to a single vitamin deficiency and presents with the classic triad of ocular findings, cerebellar dysfunction, and confusion.
Wernicke encephalopathy (WE)
Treatment of Wernicke encephalopathy?
This is a medical emergency and requires infusion of thiamine over a few days to normalized thiamine levels
Occurs in individuals with chronic liver disease such as cirrhosis or hepatitis. Early symptoms include forgetfulness, confusion, and breath with a sweet or musty odor. Advanced symptoms include shaking of the hands or arms (asterixis), disorientation, slurred speech, and coma?
Hepatic encephalopathy
Treatment of hepatic encephalopathy?
Treatment includes removing toxic substances from the intestine. Lactulose (to increase NH4 generation) and rifaximin (decrease intraluminal NH3 production)
A 21-y/o F presents with several episodes of throbbing left temporal pain that lasts for 2–3 hours. Prior to its onset, she sees flashes of light in her right visual field and feels weakness and numbness on the right side of her body for a few minutes. Headaches are often associated with nausea and vomiting. She has a family history of migraine. What's the diagnosis?
Migraine Headache
A 26-y/o M presents with terrible right temporal headaches associated with ipsilateral rhinorrhea and eye tearing and redness. Episodes have occurred at the same time every night for the past week and last for 45 minutes. What's the diagnosis?
Cluster Headaches
A 65-y/o F presents with severe, intermittent right temporal headache, fever, blurred vision in her right eye, and pain in her jaw when chewing. What's the diagnosis?
Temporal arteritis
A 30-y/o F presents with frontal headache, fever, and nasal discharge. There is pain on palpation of the frontal and maxillary sinuses. She has a history of sinusitis. What's the diagnosis?
Sinusitis
A 50-y/o F presents with recurrent episodes of bilateral squeezing headaches that occur 3–4 times a week. She is experiencing significant stress in her life. What's the diagnosis?
Tension headaches
A 35-y/o M presents with sudden severe headache, vomiting, confusion, left hemiplegia, and nuchal rigidity. What's the diagnosis?
Subarachnoid hemorrhage
A 25-y/o M presents with high fever, severe headache, confusion, photophobia, and nuchal rigidity. Kernig’s and Brudzinski’s signs are positive. What's the diagnosis?
Meningitis
An 18-y/o obese F presents with headache, vomiting, and blurred vision for the past 2–3 weeks. She is taking OCPs. What's the diagnosis?
Pseudotumor cerebri
A 47-y/o M c/o daily pain in the right cheek over the past month. The pain is electric in character and occurs while he is shaving. Each episode lasts 2–4 minutes. What's the diagnosis?
Trigeminal neuralgia
A female > 50, jaw claudication with chewing, visual disturbances (secondary to anterior ischemic optic neuritis), and constitutional symptoms - fever, anorexia, weight loss. What's the diagnosis?
Temporal arteritis
A 39-year-old man presents with intermittent episodes of severe headaches around the left eye and temple. His symptoms typically last less than an hour and resolve on their own. The headaches awaken him nightly for several days in a row then he is headache-free for a couple of months before another "round" begins. What is the most likely diagnosis?
Cluster headaches present with severe nonthrobbing headaches that typically occur at the same location and the same time each day. Headaches generally last for a few minutes up to a couple of hours. The headaches occur daily for weeks to months before they spontaneously resolve; patients may be pain-free for months to years.
How do cluster headaches classically present?
Multiple attacks of unilateral, excruciating, sharp, searing, or piercing pain that awaken patients at night. Typically localized in the periorbital area and temple accompanied by signs of ipsilateral autonomic features.
Cluster headaches are unilateral or bilateral?
Unilateral
What are the associated signs and symptoms seen with cluster headaches?
Conjunctival injection, tearing, and nasal congestion ipsilateral to the headache. Horner syndrome (anhidrosis, miosis, and ptosis) can also be seen on the affected side.
How are cluster headaches diagnosed?
Diagnosis is based on the distinctive symptom pattern and exclusion of intracranial abnormalities
What are the abortive therapy options to treat cluster headaches?
100% oxygen, sumatriptan, or dihydroergotamine.
What is the role of corticosteroids in the treatment of cluster headaches?
Prednisone can be initiated at the beginning of a cluster cycle to effectively eliminate the patient's symptoms; most patients will be pain-free within 2 days.
Long-term prophylaxis of cluster headaches?
Verapamil is often used to prevent attacks in patients with chronic or episodic disease. Think of lithium next if verapamil isn't an option or isn't enough - requires monitoring of kidney and thyroid function, lithium levels, etc.
What are some typical features of migraine without aura (formerly "common" migraine)?
Unilateral, pulsating/throbbing, nausea/ vomiting, photophobia/phonophobia, worse with activity, headache lasting 4-72 hours, and positive family history
What is the usual age of onset of migraine?
School-age or teenage years
What distinguishes migraine with aura (formerly "classic" migraine)?
Typical features of migraine plus gradual development of 1 or more transient focal neurologic symptoms, often preceding peak head pain and lasting <60 minutes
What are some common auras associated with migraine?
Ophthalmic (most common), hemiparesthetic, aphasic, and hemiplegic (formerly "complicated" migraine)
Can someone have a migraine aura without head pain?
Yes. These are termed "migraine equivalents" and are usually a diagnosis of exclusion.
What are some typical migraine triggers?
Stress, sleep deprivation, exertion or trauma, menses, bright lights, certain odors such as perfumes, and food or drink with nitrates, glutamate, aspartame, or tyramine
What are some common abortive medicines for migraine?
Triptans, ergotamine derivatives, anti-inflammatories such as high-dose NSAIDs or glucocorticoids, mixed analgesics (i.e., Midrin, Excedrin, Fiorinal), and certain antiemetics (i.e., prochlorperazine, metoclopramide)
When should abortive therapies be administered for maximum benefit?
At the onset of aura or as early in the headache as possible; earlier administration improves efficacy.
What is the therapeutic mechanism of action for triptans?
5-HT1b/d (serotonin) agonist
What are the 3 contraindications to the use of triptans and ergotamines?
Coronary artery disease, peripheral vascular disease, or hemiplegic/basilar migraine variants
Why is it important to know about butalbital in Fiorinal or Fioricet?
Because it is a habit-forming barbiturate
What 5 prophylactic drug therapies prevent or reduce the frequency of migraine?
1. β-Adrenergic blockers such as propranolol
2. Calcium-channel blockers such as verapamil
3. Tricyclic antidepressants such as amitriptyline
4. Valproic acid
5. Topiramate
What constitutes chronic migraine?
Migraine attacks >15 days per month for >3 months
How do you "PIN" the migraine diagnosis?
"PIN" the migraine diagnosis
During the last three months, have you had the following with your headaches?
P hotophopia - light bothered you more than when you don't have headaches
I mpairment - headaches limit the ability to work, study or do what you need to do
N ausea - felt nauseated or sick to the stomach
2/3 Yes = migraine (93% predictive in primary care setting)
Where in the head are the usual locations of tension headache?
Bilateral occipital, nuchal, frontal, or encircling the head with bandlike tightness
What is the presumed cause of pain in tension headache?
Episodic tension headaches are usually associated with stress, and chronic tension headaches are usually associated with contracted muscles
Tension headaches usually lead to constant pain for a duration greater than ______ minutes?
Tension headaches usually lead to constant pain for a duration greater than 30 minutes
Are photophobia and phonophobia or nausea common in tension headache?
No. Patients suffering from tension headaches usually do not have photophobia, phonophobia, or nausea
Tension headaches are usually unilateral or bilateral?
Tension headaches are usually bilateral
What 2 problems often accompany tension headache?
Psychologic stress and musculoskeletal strain
What medications are useful for treating acute tension headache?
1. Analgesics - NSAIDs, acetaminophen
3. The combination of caffeine with the simple analgesics acetaminophen, aspirin, or ibuprofen is more effective than simple analgesic monotherapy
4. Additional treatment options include parenteral chlorpromazine, metoclopramide, the combination of metoclopramide plus diphenhydramine, or intramuscular ketorolac
What prophylactic medications are useful for treating chronic tension headache?
Antidepressants: Tricyclics (amitriptyline, nortriptyline), Mirtazapine/venlafaxine
Anticonvulsants: Topiramate/gabapentin
What is another approach for patients with tension headache who fail pharmacologic therapy?
Behavioral medicine (including biofeedback, relaxation, meditation)
What is the difference between encephalitis and meningitis?
Impaired mental status in encephalitis
What is the classic triad of meningitis?
The classic triad of meningitis is:
1. Fever often greater than 38° C
2. Nuchal rigidity
3. Headache
It may also cause photophobia and phonophobia. May have petechiae (especially N. meningitidis)
What are the most common symptoms of encephalitis?
Fever - Headache - Nausea - Vomiting + Altered mental status
What is the most common cause of sporadic encephalitis in the United States.?
Herpes simplex virus type 1 is the most common; arboviruses (West Nile Virus. St. Louis, eastern equine, western equine) can also cause encephalitis.
Most common severe complication of measles?
Encephalitis
Viral meningitis is associated with predominance of what cell in the CSF?
10 to 1000 white blood cells, > 50% lymphocytes and <20% PMNs (bacterial meningitis will have > 90% PMNs)
In bacterial meningitis is there an increase or decrease of glucose in cerebrospinal fluid?
In bacterial meningitis, there is decreased glucose in cerebrospinal fluid (bacteria love to eat suga
How is protein in CSF affected in bacterial meningitis?
In bacterial meningitis, there is increased protein in cerebrospinal fluid.
What is the CSF composition of fungal meningitis?
In most fungal cases, there'll be 10-500 white blood cells, with over being 50% lymphocytes
What will CSF studies show in patients with encephalitis?
CSF findings will be similar to findings seen with aseptic meningitis. There will be increased WBCs (<250/mm3) of predominantly lymphocytes; CSF glucose will be normal and CSF protein levels can be normal or slightly elevated.
Name the sign: Inability to allow full extension of knee when hip is flexed 90 degrees
Kernig's sign. (Kernig" starts with a "K", like "knee)
Name the sign: Flexion of hips on passive neck flexion
Brudzinski's sign (Brudzinski starts with a "B", like "back of the head")
What disorder are fever, headache, neck stiffness with initially normal brain function most concerning for?
Meningitis